Abstract
Long-term outcome after closure of isolated congenital coronary artery fistula (ICCAF) is poorly documented. To assess late outcome after ICCAF closure, a 1983–2013 retrospective study included all patients who attempted an ICCAF closure and whose follow-up was ≥1 year. ICCAF was diagnosed in 23 patients [median age 6.9 years (0.1–70.5 years), 13 children]. ICCAF was symptomatic in 12 patients (52.2 %). First intervention was either a transcatheter embolization (n = 19 patients, 82.6 %) or a surgical ligation (n = 4 patients, 17.4 %). After a follow-up of 9.0 years (2.8–33.5), neither death nor late ischemic event occurred but one patient was transplanted, because of postoperative myocardial infarction. Late ICCAF recanalization occurred in eight patients, leading to successful embolization of the shunt in all patients after a delay of 9.8 years (5.7–13.8 years) from the first intervention. Re-intervention occurred later in children (p = 0.0027), with a 50 and 37.5 % freedom from re-intervention in adults compared to a 100 and 89.0 % in children, respectively, at 1 and 6 years of follow-up. At last follow-up, coronary artery diameter had decreased from a mean z score of 12.0 ± 7.7 to a mean z score of 6.0 ± 6.0 (p = 0.002). Long-term outcome after ICCAF closure is excellent, with neither death nor late ischemic event, and a significant decrease in coronary artery diameter with time. Late follow-up is of paramount importance, as one-third of patients will require a re-intervention for late shunt recanalization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Isolated congenital coronary artery fistula is a rare anomaly, defined as a direct abnormal connection of a coronary artery with one of the four cardiac chambers or any vessel. Considered as a major coronary artery malformation by Odgen’s classification, it represents 0.4 % of all cardiac malformations, with 0.002 % reported prevalence in the general population [9]. While congenital coronary artery fistula can be associated with another congenital heart disease like pulmonary atresia with intact ventricular septum or tetralogy of Fallot, isolated congenital CAF (ICCAF) accounts for up to 80 % of cases, occurring in structurally normal hearts [25]. ICCAF management remains not consensual in asymptomatic patients, as both spontaneous regression and life-threatening complications have been described [2, 26, 29].
From an interventional standpoint, with growing experience and technical developments, feasibility and safety of both surgical ligation and percutaneous embolization have been reported in most cases in experienced centers [11, 21, 28]. Although data regarding technical considerations and early post-procedural outcomes have been largely reported, long-term outcomes after ICCAF closure are still poorly documented. We report here the late follow-up of 23 patients who underwent ICCAF closure at our tertiary institution.
Materials and Methods
We conducted an observational longitudinal monocentric retrospective study. All adult and pediatric patients (1) who had ICCAF, (2) who attempted fistula closure from 1983 to 2013 and (3) whose follow-up duration was ≥1 year were included. Patients with a short follow-up <1 year and those who were lost to follow-up were not included in the study. Children were defined as aged less than 15 years old. Indication for ICCAF closure was either symptoms or fistula-related significant shunt, assessed by ventricular dilation on echocardiography and confirmed by Qp/Qs ratio at cardiac catheterization. Twenty-three patients were identified and classified into two groups: the group A (n = 19 patients, 82.6 %) included patients who first underwent a transcatheter closure and the group B (n = 4 patients, 17.4 %) included those who first had a surgical ligation. Medical files were reviewed to collect demographic, clinical, 12-lead electrocardiograms and echocardiographic data as well as technical characteristics of the percutaneous procedure or the surgery and early clinical outcomes. All imaging modalities (transthoracic echocardiography, coronary angiography and computed tomography) were analyzed for all patients by two investigators in a blind manner, at the time of diagnosis, fistula closure and last follow-up. ICCAF anatomy was accurately described including its origin, course and exit site; coronary arteries diameters, cardiac chambers dimensions [left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD)] and systolic LV function data [ejection fraction (EF)] were collected. Coronary artery diameters, LVEDD and LVESD were compared to normal values according to both age and body surface area [8, 15]. At the last visit, for a given patient, coronary artery size was measured by the same imaging modality that the one performed at the time of diagnosis, to assess the evolution of diameters with time.
Percutaneous ICCAF closures were performed in the catheterization laboratory with biplane fluoroscopic guidance, under local anesthesia in adults and general anesthesia in children. All patients received intravenous unfractionated heparin. Various materials were used following the size and anatomy of the ICCAF: releasable balloons, coils, microparticles, Amplatzer occluder and plugs. Immediate success was defined as a total or subtotal occlusion of the given pedicle. Surgery consisted in an external plication of ICCAF or, under cardiopulmonary bypass, a closure of the intracardiac opening. A physical examination, 12-lead ECG and TTE were performed at 24 h, 3 months, and 1 year after the procedure. The referring cardiologists provided subsequent follow-up. Long-term outcomes were assessed by telephone interviews of referring cardiologists to obtain information on cardiac status, data at the last visit and any delayed complications. The study was reviewed and approved by the appropriate institutional ethics committee, and all patients or legal guardians gave their informed consent to be included in the database.
Statistical Analysis
Relevant variables were expressed either as numbers and percentages or as mean value ± standard deviation. Coronary diameters after and before ICCAF closure were compared by paired t test. Further re-interventions between adults and children were compared with log-rank test. Statistical analyses were performed using Statview software version 5. Results were considered as statistically significant for an alpha risk ≤0.05.
Results
A total of 34 patients underwent ICCAF closure at our institution during the study period. We subsequently excluded 11 patients because of loss of follow-up (n = 3 patients), short follow-up less than 1 year (n = 7) and patient decline to participate (n = 1 patient), leaving 23 patients in the final analysis.
ICCAF Characteristics
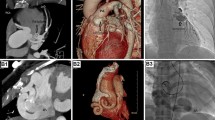
Patients and ICCAF characteristics are summarized in Table 1. ICCAF was symptomatic in 12 patients (52.2 %) who complained about chest pain (n = 4 patients) or exercise dyspnea (n = 8 patients). In 11 asymptomatic patients, a continuous systolic–diastolic murmur led to ICCAF diagnosis. ICCAF diagnosis was achieved by transthoracic echocardiography in 20 patients (86.9 %). In the 3 remaining patients, a coronary angiography was required: Two adults presented a poor echogenicity that not allowed an accurate diagnosis by echocardiography alone and 1 child had multiple drainage sites into the pulmonary artery. In 2 patients (8.7 %), the 12-lead ECG showed negative T waves in anterior leads assessing ischemic anomalies (Fig. 1).
ICCAF Closure and Early Outcome
The median age of ICCAF closure was 11.1 years (0.1–70.5 years) distributing into 13 children (median age 6.0 years, 0.1–12.5 years) and 10 adults (median age 56.6 years, 30.5–70.5 years).
In the group A, the transcatheter closure was performed in 11 children (median age 6.0 years, 0.8–12.5 years) and 8 adults (median age 57.8 years, 47.6–70.5 years). Different materials were used: releasable balloons (n = 4 patients, 21.1 %), plugs (n = 7 patients, 36.8 %), coils (n = 6, 31.6 %) (Fig. 2), and plugs and coils (n = 2 patients, 10.5 %). The approach was anterograde in 16 patients (84.2 %), retrograde in 2 (10.5 %) and both anterograde and retrograde in 1 patient (5.3 %) with a voluminous ICCAF. Two major peri-procedural complications occurred in two distinct patients consisting in one ventricular fibrillation efficiently treated with external defibrillation, and one coil migration into the distal pulmonary artery, percutaneous retrieved. In both cases, procedure was continued and fistula was closed. Early success rate was 100 % with either occlusion (n = 17, 89.5 %) or subocclusion (n = 2, 10.5 %).
In the group B, a surgical ligation was performed in 2 children (0.1 and 5.5 years) and 2 adults (30.5 and 57.8 years). Surgery was preferred because of the young age and low body weight in one 1-month-old, 3.5-kg infant, adjacent vessel at risk (superior vena cava, n = 1 patient; coronary sinus, n = 1 patient), and large fistula aneurysm with inadequate embolization material in 1 patient. Cardiopulmonary bypass was used in all patients due to anatomic considerations, and ICCAF drainage closure without CAF origin closure was performed in all patients. Cavity exposure was either right atrium (n = 3 patients) or right ventricle (n = 1 patient). Successful closure was achieved in all patients, but a 57.8-year-old woman experienced a major complication, presenting with a postoperative anterior ST-segment elevation myocardial infarction and further severe left ventricular systolic dysfunction (Table 2).
All patients received antiplatelet therapy from ICCAF closure to hospital discharge. After hospital discharge, medical treatment was led to the choice of referring cardiologist: Nine patients had an abrupt treatment discontinuation at hospital discharge, 8 received an antiplatelet agent for 3 months, 5 for 6 months, and the patient whose operation was complicated by a myocardial infarction had an antiplatelet therapy for long term.
Long-Term Outcomes
After a median follow-up of 9.0 years (2.8–33.5), neither death nor late ischemic event occurred. However, the patient who experienced postoperative myocardial infarction required a cardiac transplantation 5.7 years after the surgical ICCAF closure, because of subsequent severe ischemic cardiomyopathy with chronic heart failure. Late ICCAF recanalization occurred in 8 patients (34.8 %). Six of them were from group A (31.6 %; 1 retrievable balloon, 5 coils), 2 from group B (50 %). Ten re-interventions were needed in 8 patients (2 children) after a delay of 9.8 years (5.7–13.8 years) from the first intervention. Re-intervention was done later in children (p = 0.0027), with a 60, 50 and 37.5 % freedom from re-intervention in adults compared to a 100, 100 and 89.0 % in children, respectively, at 6 months, 2 years and 6 years of follow-up (Fig. 1). In 6 (75 %) patients, mostly adult patients [n = 5 (50 %) adults versus n = 1 (7.7 %) child, p < 0.05], late recanalization affected ICCAF draining into the pulmonary artery. In all ICCAF patients, the late recanalization was successfully treated by percutaneous embolization. Definite successful CAF closure was achieved after 2 procedures in 6 patients, 3 procedures in 2 patients.
At last follow-up, the mean z score of coronary artery diameter had decreased from 12.0 ± 7.7 to 6.0 ± 6.0 (p = 0.002).
Regarding ECG follow-up, one patient had negative T waves in inferior leads after his first percutaneous embolization. He required a second procedure because of late recanalization, with no ECG modification. In all other patients, except the one who had postoperative myocardial infarction, ECG was normal all along follow-up. Eighteen patients (78.3 %) had a regular exercise test during their follow-up, which was normal in all patients.
Discussion
Although technical considerations and early results of ICCAF closure have been evaluated, long-term outcomes are still poorly documented [3, 17, 20]. In our experience, late outcome is excellent, with no death, no late ischemic event and a significant decrease in coronary artery diameter with time. However, patients have to be carefully evaluated after ICCAF closure, as one-third of them will require a re-intervention for late shunt recanalization during follow-up.
Management of asymptomatic ICCAF is still not consensual, as its natural course may be variable. Both spontaneous closure and severe, life-threatening complications have been reported, including atrial fibrillation, ventricular arrhythmias, congestive heart failure, coronary artery aneurysm, cardiac tamponade due to spontaneous rupture of a coronary artery aneurysm, infective endocarditis [2, 5, 7, 14, 23, 24, 26, 29]. According to the American College of Cardiology/American Heart Association guidelines, ICCAF transcatheter occlusion should be considered in symptomatic patients (class I indication) and in patients with moderate or large coronary artery fistulae without clinical symptoms (class IIa indication) [10].
Our results add several novel insights compared to previous reports. Liang et al. [18, 19] have suggested a reduction in the involved coronary artery diameter in 4 patients with a mid-term follow-up, and our study confirms in a larger population and after a longer follow-up that involved coronary artery diameter significantly reduced after ICCAF closure.
Rate of recurrent fistula or residual shunt is variable among published series, whatever the occlusion method, ranging from apparently no recanalization to a 10–15 % incidence of recurrent fistula over time [1, 4, 6, 16, 22]. In another report, 30 % of patients had documented residual coronary artery fistula, but a re-intervention occurred in less than 1 % of them [13]. Our study provides information on one of the longest follow-up ever reported. We found a high proportion of fistula recanalization, up to 31 % after transcatheter closure and 50 % after surgical ligation, over a 10-year follow-up period. Although being in an acceptable range in children, freedom from re-intervention was as low as 37.5 % at 6 years in adult patients. In our study, distribution and characteristics of coronary artery fistula are concordant with what was previously published, ICCAF being unilateral in around two-third cases, and drainage site being mainly the right heart side [24, 25]. We found that fistulae were more complex in adults and pulmonary artery was more frequently the drainage site. This could explain the high rate of residual shunt in adults. Nevertheless, these data strongly support the need for a close, regular follow-up of patients after ICCAF closure, even in the long term.
Surprisingly, despite a high proportion of ICCAF recanalization, our long-term follow-up is uneventful, with no major complication. In the huge experience of the Boston’s group, major complications, including myocardial infarction, angina with coronary thrombosis and symptomatic cardiomyopathy, occurred in 15 % patients [27]. In their series, the sole angiographic feature that was predictive of adverse outcome was drainage of the ICCAF into the coronary sinus. Clinical predictors associated with adverse outcomes included older age at diagnosis, tobacco use, diabetes, systemic hypertension and hyperlipidemia. In another series, Cheung et al. [6] made coronary angiograms in 21 asymptomatic patients after ICCAF surgical ligation and found that the native coronary artery either remained dilated and tortuous, or more frequently had thromboses with a short proximal stump. Distal vessel was threadlike or completely occluded in 4 patients, and 2 patients had a thrombosed proximal artery with distal coronary artery filled by collaterals. More recently, in a series of 16 patients, Gowda and coworkers showed that post-ICCAF treatment sequelae include thrombosis and myocardial infarction, revascularization, persistent coronary dilatation, remodeling, and decrease in conduit coronary artery size toward normal [12]. The large size distal type of CAF may be at highest risk of coronary thrombosis post-closure. The authors proposed to prescribe both anticoagulation therapy and associated antiplatelet agent to treat CAF with high risk of thrombosis. In our series, despite no (or no long-term) treatment by antiplatelet agent, no ischemic clinical event occurred, and no electrical changes were observed at 12-lead electrocardiogram and/or during exercise test all along the follow-up. However, no recommendation can be done based on this observation on a little series. Given the risk of ischemic events reported by others, it makes sense that patients receive at least long-term treatment by an antiplatelet agent after ICCAF closure. Further collaborative prospective studies may be of interest to assess anticoagulation benefits after ICCAF closure.
Conclusion
Long-term outcome after ICCAF closure is excellent in our series, with neither death nor late ischemic event, and a significant decrease in involved coronary artery diameter with time. Late follow-up remains of paramount importance, as (1) thrombus formation and ischemic complications have been reported by other groups and (2) one-third of patients will require a re-intervention for late shunt recanalization.
References
Abdelmoneim SS, Mookadam F, Moustafa S et al (2007) Coronary artery fistula: single-center experience spanning 17 years. J Interv Cardiol 20:265–274
Alsara O, Kalavakunta JK, Hajjar V, Alsarah A, Cho N, Dhar G (2014) Surviving sudden cardiac death secondary to anomalous left coronary artery from the pulmonary artery: a case report and literature review. Heart Lung 43:476–480. doi:10.1016/j.hrtlng.2014.06.048
Armsby LR, Keane JF, Sherwood MC, Forbess JM, Perry SB, Lock JE (2002) Management of coronary artery fistulae. Patient selection and results of transcatheter closure. J Am Coll Cardiol 39:1026–1032
Brenot P, Riou J-Y, Losay J, Petit J, Lambert V, Angel C-Y (2007) Endovascular treatment of coronary arterial fistulae in children and adults. Arch Mal Coeur Vaiss 100:373–379
Chandra N, Sarkar A, Pande A (2015) Large congenital coronary arteriovenous fistula between the left main coronary artery and right superior vena cava, associated with aneurysmal dilatation of the left main coronary artery: rare case report. Cardiol Young 25:143–145. doi:10.1017/S1047951114001103
Cheung DL, Au WK, Cheung HH, Chiu CS, Lee WT (2001) Coronary artery fistulas: long-term results of surgical correction. Ann Thorac Surg 71:190–195
Corvaja N, Moses JW, Vogel FE et al (1999) Exercise-induced ventricular tachycardia associated with coronary arteriovenous fistula and correction by transcatheter coil embolization. Catheter Cardiovasc Interv 46:470–472
Dallaire F, Dahdah N (2011) New equations and a critical appraisal of coronary artery Z-scores in healthy children. J Am Soc Echocardiogr 24:60–74. doi:10.1016/j.echo.2010.10.004
Dodge-Khatami A, Mavroudis C, Backer CL (2000) Congenital heart surgery nomenclature and database project: anomalies of the coronary arteries. Ann Thorac Surg 69:S270–S297
Feltes TF, Bacha E, Beekman RH 3rd et al (2011) Indications for cardiac catheterization and intervention in pediatric cardiac disease: a scientific statement from the American Heart Association. Circulation 123:2607–2652. doi:10.1161/CIR.0b013e31821b1f10
Freund JE, Yuko-Jowi C, Freund MW (2015) Transcatheter embolization of a large aneurysm in a congenital coronary cameral fistula from the left coronary artery to the right ventricle. Catheter Cardiovasc Interv 85:435–439. doi:10.1002/ccd.25587
Gowda ST, Forbes TJ, Singh H et al (2013) Remodeling and thrombosis following closure of coronary artery fistula with review of management: large Distal Coronary Artery Fistula-To Close or Not to Close? Catheter Cardiovasc Interv 82:132–142. doi:10.1002/ccd.24699
Jama A, Barsoum M, Bjarnason H, Holmes DR Jr, Rihal CS (2011) Percutaneous closure of congenital coronary artery fistulae: results and angiographic follow-up. JACC Cardiovasc Interv 4:814–821
Jariwala U, Hasan RK, Thorn EM, Zakaria S (2015) An unusual case of infective endocarditis involving a right coronary artery to superior vena cava fistula. Catheter Cardiovasc Interv 85:620–624. doi:10.1002/ccd.25597
Kampmann C, Wiethoff C, Wenzel A et al (2000) Normal values of M-mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart 83:667–672
Kimura S, Miyamoto K, Ueno Y (2006) Cardiac tamponade due to spontaneous rupture of large coronary artery aneurysm. Asian Cardiovasc Thorac Ann 14:422–424
Latson LA (2007) Coronary artery fistulas: how to manage them. Catheter Cardiovasc Interv 70:110–116
Liang C-D, Ko SF (2006) Midterm outcome of percutaneous transcatheter coil occlusion of coronary artery fistula. Pediatr Cardiol 27:557–563
Liang C-D, Ko S-F, Huang C-F, Huang S-C (2005) Echocardiographic evaluation of coronary artery fistula in pediatric patients. Pediatr Cardiol 26:745–750
Mangukia CV (2012) Coronary artery fistula. Ann Thorac Surg 93:2084–2092. doi:10.1016/j.athoracsur.2012.01.114
Manoly I, Mahadevan VS, Hoschtitzky JA (2014) Hybrid approach to closure of an acquired coronary-cameral fistula. Ann Thorac Surg 98:e59–e61. doi:10.1016/j.athoracsur.2014.05.094
Oto A, Aytemir K, Çil B et al (2011) Percutaneous closure of coronary artery fistulae in adults with intermediate term follow-up results. J Interv Cardiol 24:216–222
Reinders S, Bogaard K, Reichert CL, Knol RJ (2014) A tortuous road for septic pulmonary emboli in left-sided endocarditis. Can J Cardiol 30(1462):e3–e5. doi:10.1016/j.cjca.2014.06.008
Said SA (2011) Current characteristics of congenital coronary artery fistulas in adults: a decade of global experience. World J Cardiol 3:267–277. doi:10.4330/wjc.v3.i8.267
Said SA, Lam J, van der Werf T (2006) Solitary coronary artery fistulas: a congenital anomaly in children and adults. A contemporary review. Congenit Heart Dis 1:63–76. doi:10.1111/j.1747-0803.2006.00012.x
Schleich JM, Rey C, Gewillig M, Bozio A (2001) Spontaneous closure of congenital coronary artery fistulas. Heart 85:E6
Valente AM, Lock JE, Gauvreau K et al (2010) Predictors of long-term adverse outcomes in patients with congenital coronary artery fistulae. Circ Cardiovasc Interv 3:134–139. doi:10.1161/CIRCINTERVENTIONS.109.883884
Wang C, Zhou K, Li Y et al (2014) Percutaneous transcatheter closure of congenital coronary artery fistulae with patent ductus arteriosus occluder in children: focus on patient selection and intermediate-term follow-up results. J Invasive Cardiol 26:339–346
Yilmazer MM, Demir F, Yolbaş I, Bilici M (2014) Spontaneous closure of a symptomatic coronary artery fistula just within a few days of newborn period. Congenit Heart Dis 9:E27–E30. doi:10.1111/chd.12060
Acknowledgments
We gratefully thank Benedicte Mennelet-Clouet for her kind assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The present study was approved by our institutional review board in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Ponthier, L., Brenot, P., Lambert, V. et al. Closure of Isolated Congenital Coronary Artery Fistula: Long-Term Outcomes and Rate of Re-intervention. Pediatr Cardiol 36, 1728–1734 (2015). https://doi.org/10.1007/s00246-015-1224-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1224-3