Abstract
Purpose of Review
Coronary artery fistulas (CAFs) are rare coronary anomalies that most often occur as congenital malformations in children. Although most children with CAFs are asymptomatic at the time of diagnosis, some present with symptoms of congestive heart failure in the setting of large left-to-right shunts. Others may develop additional complications including coronary artery ectasia and coronary thrombosis. Surgical and transcatheter closure techniques have been previously described. This review presents the classifications of CAFs in children and the short and long-term outcomes of CAF closure in children in the reported literature. We also summarize previously-reported angiographic findings and post-treatment remodeling characteristics in pediatric patients.
Recent Findings
With advancements in cross-sectional imaging technologies, anatomic delineation of CAFs via these modalities has become crucial in procedural planning. Recent reports of surgical and transcatheter closure of CAFs in children have reported good procedural success and low rates of short-term morbidity and mortality. Distal-type CAFs have elevated risk for long-term sequelae post-closure compared to proximal-type CAFs. A recent report of a multi-institutional cohort also describes post-closure remodeling classifications which may predict long-term outcomes in these patients as well as guide individualized anticoagulation management.
Summary
Invasive closure of significant CAFs via surgical or transcatheter techniques is feasible and safe in most children with good short and intermediate-term outcomes. However, close clinical and imaging follow-up is required to monitor for late complications even after successful closure. Antiplatelet and anticoagulation regimens remain important aspects of post-closure management, but the necessary intensity and duration of such therapy remains unknown.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
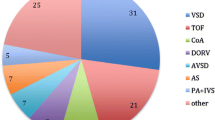
Coronary artery fistulas (CAFs) are rare coronary anomalies defined as an abnormal connection between a coronary artery and a cardiac chamber or other thoracic vessel without an interposed capillary bed [1]. The incidence of congenital CAFs in the general population has been estimated at 0.002% [1]. In series of 126,595 primarily adult patients undergoing invasive coronary angiography to assess for atherosclerotic lesions, coronary artery fistulas comprised 0.1–0.2% of isolated coronary artery anomalies with equal incidence in both sexes [2]. CAFs are noted in approximately 0.3% of patients with congenital heart disease that includes ventricular and atrial septal defects, patent ductus arteriosus, tetralogy of Fallot, and pulmonary atresia with intact ventricular septum [3]. Most CAFs in infants and children are congenital fistulas. Acquired fistulas are extremely rare in infants and children and are most often small, hemodynamically insignificant, and do not require intervention.
About 75% of CAFs found incidentally in infants and children are small and hemodynamically insignificant [4,5,6]. Neonates and infants with large size CAFs typically present with congestive heart failure symptoms. Older children with CAF are either asymptomatic or diagnosed with a CAF when they are referred for evaluation of heart murmur, recurrent respiratory infection, and/or exercise intolerance. Invasive treatment of isolated CAFs in asymptomatic neonates and infants is controversial. Symptoms and sequalae, when present, typically arise from significant left-to-right shunts, coronary artery ectasia, or coronary thrombosis. While medical therapy for congestive heart failure is first line treatment, early referral for surgical or transcatheter closure of large symptomatic CAFs has been the mainstay of treatment for infants and children.
Types of Coronary Artery Fistula
CAFs can occur either as a congenital malformation, thought to be due to persistence of sinusoidal-coronary arterial connections during fetal cardiac development, or acquired as a result of infective endocarditis, traumatic injury, such as a complication of penetrating chest injury or endomyocardial biopsies, or due to other cardiac surgery (e.g., right ventricular outflow tract resection tumor resection) [7]. Different CAF terminology is used based on the outlet of the fistulas. These abnormal coronary connections may terminate in a chamber of the heart, referred to as coronary-cameral fistula, or into a vein as a coronary arteriovenous fistula. Rarely, a coronary artery fistula may end in a pulmonary artery in a coronary-pulmonary artery fistula.
In 1966, Sakakibara and colleagues from Japan proposed the initial classification describing the three schema (Schema I, II and III) of CAF based on the site of origin of the fistulae [8]. Subsequently, the classification has been modified into two main types: Type A or the Proximal CAF and Type B or the Distal CAF [9, 10••]. Type A (Sakakibara Schema I) fistulae originate from the proximal third of the epicardial coronary artery (Fig. 1a). The fistula has no significant coronary branches supplying the myocardium, and the distal coronary artery, beyond the fistula origin, has normal caliber. Type B (Sakakibara Schema III) fistulae originate from or at the distal end of the epicardial coronary artery leading to a diffusely dilated and tortuous native coronary artery with normal coronary branches arising from this fistula (Fig. 1b). Maintaining blood flow in this dilated and tortuous epicardial coronary artery is critical for myocardial perfusion via the relatively smaller/normal branches supplying the myocardium. Schema II CAF of Sakakibara classification was noted when fistula was observed at the mid portion of the epicardial coronary artery, but this type is not specified in the modified Type A and B classifications.
Coronary artery fistula types A (proximal) and B (distal). a Type A or proximal-type coronary artery fistulas (CAFs) originate from a proximal portion of epicardial coronary artery without giving off coronary branches. b By contrast, type B or distal-type CAFs originate from the distal aspect of an epicardial coronary artery. The coronary artery proximal to the fistulous connection is dilated with normal coronary branching. RCA, right coronary artery; LCx, left circumflex artery; LAD, left anterior descending artery
CAFs can be present as single or multiple fistulas. In addition, CAFs can also be classified as simple versus complex fistulae: Simple CAFs typically are single origin arising from 1 epicardial feeding artery and have a single termination. Complex CAFs have more than one origin with multiple exit points into the same or different chambers/vessels. Based on the mode of termination noted on transcatheter angiography, patients can either have a macro-CAF, where a discrete fistulous connection is noted, or a micro-CAF, where a diffuse contrast blush is visible without a discrete fistulous connection.
The actual size of the fistula itself is not considered to be a reliable indicator of hemodynamic insignificance. Based on the angiographic dimensions of the fistulae in reference to the adjacent/distal vessel diameter, simple CAF can be further classified as “small” CAF if the fistula size is less than the distal coronary artery diameter, “medium” CAF if the fistula size is 1–2 times the distal coronary artery diameter, and “large” CAF if the fistula size is more than twice the distal coronary artery diameter [9, 11].
Clinical Presentation
The majority of patients with coronary artery fistulas are asymptomatic. In a review of 173 patients reported in the literature, Liberthson et al. found that patients less than the age of 20 years old were less likely to be symptomatic (19%) at the time of diagnosis than those older than 20 years of age (63%) [5]. In the younger patient group, the most common symptoms were dyspnea on exertion or fatigue followed by angina. Preoperative complications occurred in 11% of patients, primarily as congestive heart failure from a left-to-right shunt with a mean pulmonary-to-systemic flow ratio (Qp:Qs) of 1.6:1 [5]. Severe sequalae occur more frequently in adult patients, including myocardial infarction (9%), fistula thrombosis or aneurysm formation, or rupture (1%), endocarditis (4%), or death (14%) [5]. Physical examination often reveals a continuous murmur with diastolic accentuation, which stands in contrast to the systolic accentuation of the continuous murmur associated with a patent ductus arteriosus.
Diagnostic Studies
Initial diagnostic testing may reveal an abnormal electrocardiogram (ECG) with evidence of ventricular hypertrophy, ST changes suggestive of ischemic disease, or arrhythmias [12]. Chest radiographs may reveal cardiomegaly or pulmonary vascular plethora.
Echocardiography is often performed as part of work-up for an audible murmur or other cardiac indications. In a single center retrospective study on the use of echocardiography and the evaluation of coronary artery fistula, Vinograd et al. reported that CAFs were found incidentally on screening echocardiograms for indications such as prechemotherapy or evaluation of suspected genetic syndrome in 38% of patients with small CAFs and 5% in those with moderate-large CAFs [13]. Two-dimensional and color flow echocardiography may show dilation or ectasia of coronary arteries, an abnormal vessel with continuous or diastolic flow pattern, and/or abnormal drainage into a cardiac chamber or major thoracic vessel (Fig. 2) [13, 14]. When hemodynamically significant shunting is present, enlargement of cardiac chambers may also be seen. Secondary signs such as impaired ventricular or valvar function may also rarely be seen.
Echocardiographic view of dilated right coronary artery in setting of large coronary artery fistula. Parasternal short-axis echocardiographic view in two-dimensional and color mapping of patient with a distal-type right coronary artery fistula showing severely dilated proximal right coronary artery is seen highlighted by a star (*)
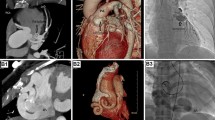
Coronary computed tomography (CCT) has emerged as a valuable non-invasive diagnostic tool for comprehensive evaluation of coronary arteries and CAFs. Coronary CT is the first-line diagnostic tool to evaluate hemodynamically significant or large CAFs [15•]. This non-invasive imaging modality offers several advantages in the assessment of CAF. It provides high spatial and temporal resolution, enabling precise visualization of the origin of the fistula, anatomic course and borders, and termination or drainage site/sites [15•]. With the aid of electrocardiogram (ECG)-gating protocols, CCT minimizes cardiac motion artifacts, ensuring clear and accurate depiction of the coronary artery tree and the features of the CAF (Fig. 3a). Three-dimensional (3D) volume rendering and post-processing techniques enhance the ability to examine CAF anatomy and course, which can be quite challenging with other imaging modalities (Fig. 3b). Beyond diagnosis, CCT plays a crucial role in pre-procedural planning by defining the exact location of the fistulous connection relative to the coronary artery tree, providing essential information for interventional decisions (transcatheter candidacy and transcatheter intervention approach and strategy) [16]. Additionally, it offers a valuable means of follow-up after transcatheter closure procedures, allowing for the assessment of fistula closure success and patency of coronary artery branches (Fig. 3c). In summary, CCT has become an indispensable tool for both the initial evaluation and long-term management of coronary artery fistulas, offering the cardiologist a comprehensive view of these complex vascular anomalies.
Coronary computed tomography showing a proximal right coronary artery fistula to the cavo-atrial junction before and after device closure. a Coronary CT showing proximal origin of a coronary artery fistula (black arrow) from the dilated right coronary artery (triangle). b Three-dimensional volume rendering of coronary CT showing course of large coronary artery fistula off the dilated right coronary artery (triangle) to the cavo-atrial (SVC-RA) junction (star *). c Follow-up coronary CT 6 months post-device closure (device not seen here) of right coronary artery fistula with remodeling without residual fistulous connection and decrease in right coronary luminal diameter (block arrows). Triangle: dilated proximal right coronary artery. Black arrow: coronary fistula, cross (+) coronary artery fistula termination site to SVC-RA junction. Block arrows: decreased coronary luminal diameter. RA, right atrium
While CCT is the mainstay non-invasive diagnostic tool for evaluating CAF, cardiac magnetic resonance (CMR) imaging can be used at times for further evaluation. The role of CMR is especially important when additional physiological and functional information are required. Cardiac MRI provides hemodynamics of CAF by measuring the Qp:Qs using phase-contrast imaging, offering insights into the significance and impact of the shunt [17]. Cardiac MRI is also capable of evaluating myocardial viability through techniques like late gadolinium enhancement, which can be particularly relevant in cases where CAF-related myocardial ischemia or scarring is suspected. These techniques, however, have largely been limited to the adult population and reliability in young children is likely limited [18, 19]. Additionally, CMR can assist in identifying large coronary artery fistulas and their impact on adjacent structures. Overall, CMR complements other imaging modalities by providing a comprehensive assessment of CAF, including both anatomic but more importantly functional data, making it an indispensable tool in the management and decision-making process for selected patients with coronary artery fistulas.
Coronary Angiography
The gold standard for diagnosis and categorization of CAFs remains selective coronary angiography [20,21,22]. Invasive angiography allows for detailed delineation of the fistula anatomy including fine vessels with a high degree of temporal and spatial resolution [11]. Temporal resolution is of particular importance in infants and young children, in whom faster heart rates may degrade image quality on cross-sectional modalities. Pre-existing luminal abnormalities such as thrombosis can be identified and delineated. Hemodynamic assessments including quantification of left-to-right shunt burden can also be performed when congestive heart failure is the primary indication for invasive evaluation. Importantly, transcatheter closure of CAFs can be performed at the time of diagnostic imaging. Conventional angiography does have limitations, however, including inherent procedural risks and complications. Moreover, conventional angiography produces two-dimensional (2D) projection images, which may limit delineation of particularly complex or tortuous anatomy [22]. Cross-sectional imaging therefore remains an important adjunctive tool in the complete evaluation of many CAFs. During follow-up testing for patients following transcatheter or surgical closure, conventional angiography remains an important tool in assessing for residual shunts or development of coronary artery complications.
Exercise/Stress Testing
The role of exercise stress testing in children with CAFs has not been well defined. Published case reports with positive exercise stress testing have been restricted to older adult patients with CAFs [23,24,25]. In these patients, exercise testing was positive for ischemic changes on stress ECG, myocardial ischemia on nuclear perfusion stress testing, or atrioventricular conduction abnormalities [23,24,25]. Given that most pediatric patients are asymptomatic and those with symptoms are primarily related to left-to-right shunt burden, the role of exercise stress testing on initial evaluation in the pediatric population appears limited. Nonetheless, given the risk of development of late coronary artery complications, physiologic stress testing may play an important role in long-term follow-up in these patients, particularly as they enter adulthood.
Management
Observation
Observation remains a viable treatment plan for patients of any age who are asymptomatic (no chest pain, no ventricular dysfunction, no heart failure or respiratory symptoms, normal exercise tolerance without EKG changes) and who have small, single outlet CAF with small volume shunts and no chamber enlargement [9, 26]. Most of these will not enlarge and a few will spontaneously close with time [6]. Young patients who are asymptomatic at the time of diagnosis, but who have moderate or even large shunts, can be observed for a period of time, but regular follow-up with repeat imaging is necessary to make informed decisions about intervention [21]. In asymptomatic patients with moderate-to-large type B fistulas, Gowda et al. suggest that antiplatelet therapy may be indicated for prevention of thrombosis of the fistula, although supporting data is limited [10••, 21]. Unlike small shunts, CAF with moderate to large shunts are unlikely to close spontaneously. They are more likely to become more hemodynamically significant over time as the patient ages and may progress to symptoms of chest pain or angina from coronary stenosis, thrombosis, or myocardial infarction or fistula rupture [27]. Moreover, the risk of intervention increases with comorbid conditions such as hypertension, diabetes, and smoking. Because of the unpredictable timing of serious complications and increased procedural risk over time, the traditional teachings has been to perform elective closure in adults patients, even in the absence of significant symptoms [27].
Transcatheter Closure
Transcatheter closure of CAFs is a less invasive alternative to surgical closure and is applicable to most patients, including infants [10••]. Risks of transcatheter closure are related to type of CAF, number of outlets, older age, and number of comorbidities.
Ideal candidates for transcatheter closure would be patients with type A coronary artery fistula. These vessels can typically be closed with a device in the proximal part of the fistula without significant risk of thrombosis extending into the normal coronary artery. These vessels can also be closed at the outlet (i.e. entrance into the right atrium, right ventricular, or pulmonary artery). Although thrombus may form in the dilated portion of the fistula, it only rarely will extend to the proximal origin of the fistulous vessel and compromise the normal coronary. Remodeling of this vessel typically leads to normal coronaries beyond the origin of the fistula. Figure 4 shows an example of transcatheter closure of a Type A fistula from the right coronary artery.
Transcatheter closure of a proximal (Type A) right coronary artery to right atrium fistula. Aortic root angiography in posteroanterior (a) and lateral (b) projections outlining a large proximal right coronary to right atrium fistula with normal caliber distal right coronary artery. Arrows point to large fistula arising from proximal right coronary artery. Selective balloon occlusion of the proximal fistula in the posteroanterior (c) and lateral (d) projections showing no right coronary branches arising from the fistula. After transcatheter closure with two Amplatzer Vascular Plug II devices, angiography in posteroanterior (e) and lateral (f) projections showing occlusion of fistulous tract with normal flow to remainder of right coronary artery branches. Single star (*), normal right coronary artery; double star (**), tortuous and dilated fistula
Patients with type B coronary fistula (Fig. 5) can also be closed using transcatheter devices but must be closed at their distal end, at the entrance into the chamber and away from the normal coronary branches, to prevent occlusion and thrombosis of normal vessels. Typically, small balloon wedge catheters are placed distally into the fistulous vessel, and balloon occlusion angiograms are performed to look for normal distal coronaries originating distally near the outlet site. Closure targets can then be selected beyond the origin of the normal coronaries and proximal to the outlet sites. Distal closure must address all outlet sites to prevent persistent shunting. Unfortunately, distal closure can lead to stasis of blood flow in the fistulous coronary artery, leading to thrombosis of the dilated vessel and occlusion of the normal coronary branches in that area. The larger the fistula and the larger the shunt, the higher the risk for a coronary event even at a young age. Anticoagulation and antiplatelet therapy are standard for these patients with distal transcatheter closure [10••].
Transcatheter closure of distal right coronary to right ventricle fistula. Selective right coronary angiography in posteroanterior (a) and lateral (b) projections outlining large distal right coronary to right ventricle fistula with minimal opacification of normal right coronary artery branches. Angiogram post-occlusion of fistulous connection with Amplatzer Vascular Plug IV device in posteroanterior (c) and lateral (d) projections showing increased opacification of right coronary branches. Star (*), normal right coronary branches. Double star (**), dilated fistula
Patients with very large and very tortuous coronary fistula or multiple outlet sights have the highest risk of complication and myocardial infarction, and transcatheter closure remains a controversial topic for this group [10••]. Older patients, who are high risk for observation or surgical closure, may be considered for transcatheter closure once the risks have been adequately explained to the patient.
Transcatheter closure can be achieved with many types of closure devices including coils, patent ductus arteriosus devices, and vascular plugs based on the size of the fistulous vessel and the need for distal outlet closure [10••, 20, 21, 28].
Surgical: Epicardial vs Endocardial Closure
Surgical closure of coronary fistula has been in place for more than 70 years and represents an excellent option for select patients [29, 30]. Certainly, patients with large symptomatic fistula with multiple communications, those with tortuous and aneurysmal arteries and those patients with need for simultaneous bypass surgery, are good candidates for surgical closure [22]. The simplest surgical treatment is the proximal epicardial ligation of the proximal fistula. But more complex fistulae require more complex closures. Complex fistulae with multiple outlet sites, or short tracks near important structures, such as the aortic valve or coronary sinus, may benefit from endocardial closure [31]. Other techniques employed have been to ligate the coronary arteries proximal and distal to the fistula and then construct a bypass for these vessels. Surgical closure has a low mortality rate, but careful follow-up is still needed [29, 32].
Follow-Up
Short-Term Outcomes
Reports of surgical closure, either via an epicardial or endocardial approach, of CAFs in children have shown excellent acute procedural success rates, with procedural success rates of 89–100% [10••, 33,34,35]. Surgical closure of CAFs in children has been reported to be very safe, with no acute surgical complications, no reoperations during the same hospitalization, and 100% survival to discharge in case series [10••, 12, 27, 33, 35, 36]. Reinterventions for residual shunts are reasonable common. Zhang et al. reported a 17% incidence of residual shunt in their series of 47 patients, five (10.6%) of which were found in the immediate postoperative period with an additional three (6.4%) found in the median follow-up period of 7.8 years [33]. Two of the patients with immediately detected postoperative shunts underwent transcatheter closure of the residual fistula, without additional reinterventions in the cohort [33]. Valente et al. reported a similar reintervention rate of 15% in their cohort of 20 patients who underwent surgical closure without any major procedural complications [27].
Transcatheter closure of CAFs has also been reported to be highly successful. In the same Boston cohort with 44 pediatric and adult patients undergoing transcatheter closure of CAFs, Valente et al. reported a 2.3% reintervention without procedural deaths, strokes, or infections [27]. They did report transient ST-T wave changes in 5 patients, atrial arrhythmia in 7 patients, 11 with device migration, and 2 cases of coronary dissection without acute or long-term sequelae [27]. Thakkar et al. reported 100% procedural success in 13 patients with 12 having complete occlusion of the CAF post-closure and 1 with trivial residual flow [34]. In a cohort of 48 neonates and infants who underwent CAF closure across 20 centers, Gowda et al. reported a 92% procedural success rate for transcatheter closure without acute deaths, strokes, or infections [10••]. There was one patient with a right coronary artery fistula who underwent coil occlusion which was complicated by immediate thrombosis extending into nearby coronary branches that was managed with anticoagulation and aspirin [10••]. An additional infant who underwent closure of a large distal right coronary artery fistula using a vascular plug was placed on aspirin monotherapy post-procedure and presented 1 week later with irritability, moderate right ventricular systolic dysfunction, and elevated troponin. This patient was medically managed with anticoagulation and beta-blockers for presumed coronary ischemia [10••]. The reported short-term complications of both surgical and transcatheter closure are therefore low but do occur, primarily related to coronary thrombosis.
Long-Term Outcomes
The long-term outcomes of patients undergoing CAF closure have been mixed, with some series of surgical patients reported no mortality or symptoms at median follow-up of 7.8 to 9.6 years [12, 33]. Despite favorable acute outcomes for both transcatheter and surgical closure of CAFs, there remains an important incidence of late major complications even following acutely successful procedures. In a series from patients at the Cleveland Clinic, 16 patients underwent CAF closure between 1997 and 2007 at median age of 1.6 years. Twelve patients underwent transcatheter closure, while four underwent surgical closure. The median follow-up period was 2.3 years with complete closure on follow-up in 12 patients, trivial leak in 2, and small-moderate leak in 1 patient. Three patients were confirmed or suspected to have coronary artery thrombosis and presented with myocardial infarction in their 50 s, all of whom had a distal-type CAF [12]. In the Boston series, of 44 patients who underwent transcatheter closure and 20 patients who underwent surgical closure, 11 patients (15%) had major complications: seven patients had myocardial infarctions, two patients presented with angina with documented intracoronary thrombus, and two developed cardiomyopathy and significant heart failure symptoms [27]. Thus, close clinical follow-up and high index of suspicion for coronary complications remains important over the long term in these rare patients.
Post-Closure Coronary Remodeling
Gowda et al. have previously described an angiographic classification system for post-treatment coronary fistula remodeling broadly divided into “optimal” and “suboptimal” remodeling [10••]. Optimal remodeling is defined as thrombus occluding the fistulous segment without extension into the epicardial artery of the more proximal CAF or to the nearest branch (Fig. 6). In a proximal CAF, this results in complete occlusion of the fistulous connection (Fig. 6a) without proximal extension into the main coronary artery. In a distal CAF, optimal remodeling is considered thrombosis of the fistulous connection followed by decrease in luminal diameter of the feeding artery with maintenance of patency and good flow into coronary branches (Fig. 6b). Figure 7 demonstrates follow-up coronary angiogram 6 months post-transcatheter closure on proximal CAF developing thrombus through the fistulous connection but without extension into the main right coronary artery. Figure 8 similarly shows follow-up coronary angiogram 2 years post-transcatheter closure of a distal CAF with maintained patency of right coronary branches.
Optimal post-closure coronary artery fistula remodeling. Optimal post-coronary artery fistula (CAF) closure remodeling with device location marked “X.” a Optimal remodeling of post-closure proximal CAF with thrombus completely occluding fistulous connection without encroaching into the proximal coronary artery or epicardial branches. b Optimal remodeling of post-closure distal CAF with complete thrombus occlusion of distal fistulous connection and decrease in luminal diameter of the dilated conduit artery with formation of layering thrombus. Epicardial branches from the conduit artery remain patent with preserved coronary flow. RCA, right coronary artery; LCx, left circumflex artery; LAD, left anterior descending artery
Optimal remodeling post-closure of proximal coronary artery fistula. Follow-up coronary angiography in posteroanterior (a) and lateral (b) projections 6 months after device closure of proximal RCA fistula showing optimal remodeling without residual fistula flow and widely patent “true” right coronary artery without luminal irregularity or stenosis. Star (*) showing unobstructed, normal right coronary branches
Transcatheter closure of distal coronary artery fistula with follow-up angiogram showing optimal remodeling. Posterior (a) and lateral (b) projections of selective angiogram of a severely dilated right coronary artery with a type B CAF that was subsequently closed with Amplatzer vascular plug IV devices. Posteroanterior (c) and lateral (d) projections of follow-up angiogram 2 years post-closure showing no residual fistula flow and no extension of thrombus into proximal normal right coronary branches. There is good opacification of the distal right coronary artery. Star (*) showing unobstructed, normal right coronary branches
In contrast, suboptimal remodeling refers to symptomatic coronary thrombosis with occlusion of adjacent coronary branches (Fig. 9), asymptomatic thrombosis with revascularization through thread-like collaterals, and partial thrombosis with a residual cul-de-sac fistula with vessel irregularity and/or stenosis [10••]. A third category has been described as persistent coronary dilation due to residual flow from incomplete fistula closure [10••]. In Gowda et al.’s series of 20 patients with available posttreatment coronary angiography, 10 patients had optimal remodeling, and 7 patients had suboptimal remodeling with 2 patients with symptomatic thrombosis including troponin leak. And additional four patients had residual CAF dilation in the setting of residual flow. Importantly, of the 7 patients with suboptimal remodeling, six patients did not receive anticoagulation and were on antiplatelet therapy alone [10••]. There was a tendency toward suboptimal modeling in patients with distal type CAFs compared to proximal type as well as larger CAFs with maximal caliber of 7.3 mm [10••].
Suboptimal remodeling after coronary artery fistula closure. Suboptimal post-coronary artery fistula (CAF) closure remodeling with device location marked “X.” Direction and propagation of post-closure thrombosis is shown by the yellow arrow. a Suboptimal remodeling of post-closure proximal CAF with thrombus extending and encroaching into the proximal coronary artery (star *), resulting in narrowing of the distal left main coronary artery. b Suboptimal remodeling of post-closure distal CAF with thrombus extending proximally with occlusion of coronary artery branches of the conduit left circumflex artery (star *). RCA, right coronary artery; LCx, left circumflex artery; LAD, left anterior descending artery
Post-Procedural Management
There is limited data supporting post-closure anticoagulation management decisions of CAFs. Gowda et al. reported that the use of antiplatelet agents only may have been associated with suboptimal post-closure remodeling [10••]. Given the higher relative risk of coronary events in patients with moderate-to-large distal-type coronary artery fistula compared to proximal-type coronary artery fistulas, their group recommends anticoagulation for 3–6 months and antiplatelet therapy for 6–12 months in this higher risk group. Anticoagulation is continued until follow-up anatomic evaluation is performed and the type of remodeling is identified. This approach seems to us to be reasonable, particularly given that major complications in the post-treatment period appear to be related to coronary thrombosis. In a series of 76 patients who underwent either transcatheter (61%) or surgical (26%) closure of CAFs, Valente et al. found that drainage of the CAF to the coronary sinus was significantly associated with major complications [27]. Thus, in higher risk groups, namely, patients older than 20 years old at the time of procedure, those with moderate-large distal-type fistulas, and those with coronary-to-coronary sinus fistulas, we agree that therapeutic anticoagulation for ~ 6 months with a longer period of antiplatelet therapy for 12 months would allow for coronary remodeling and development of chronic thrombus while mitigating risks of acute thrombotic events.
Other clinical risk factors associated with complications were older age at diagnosis, tobacco use, diabetes, systemic hypertension, and hyperlipidemia [27]. These same risk factors have been previously implicated in the development in coronary artery disease in adults [37]. These findings emphasize the need for long-term cardiology follow-up and aggressive management of these known coronary artery disease risk factors, particularly in this patient population.
Our Approach
We propose the following approach to the management of CAFs. In asymptomatic patients with small CAFs which may close spontaneously, close clinical and imaging follow-up is reasonable. In those with larger fistulas, closure should be pursued prior to adulthood, even in the absence of symptoms. This recommendation is based primarily on the observation that CAFs in patients older than 20 years of age are more likely to present with symptoms and may incur a higher rate of major sequelae from observation or closure compared to younger patients [5, 27, 35]. Following surgical or transcatheter closure, we recommend close clinical follow-up with interval coronary angiography, particularly in the first 6–12 months. Assessment in this posttreatment period for optimal vs. suboptimal remodeling may hold important clinical implications for longer-term anticoagulation and invasive imaging. Patients with distal CAFs, CAFs with maximal caliber > 7 mm, and CAFs that drain to the coronary sinus may have particularly high-risk profiles in the long-term. In these patients, as well as patients older than 20 years at time of intervention, we recommend therapeutic anticoagulation for at least 6 months and lifelong antiplatelet therapy to mitigate the risk of intermediate-term coronary artery thrombosis until remodeling trajectory is established on follow-up coronary angiography. Follow-up coronary angiography by CT or invasive angiography should be performed 6 months post-procedure to assess remodeling. If optimal remodeling is not established, anticoagulation should be continued. Even after demonstrated longitudinal stability of CAFs posttreatment, continued close follow-up is important due to some small risk of recurrence. Finally, the aggressive management of modifiable risk factors such as tobacco exposure, hyperlipidemia, hypertension, and diabetes is critical in mitigating increased risk of coronary artery disease. In keeping with guidelines from the American Heart Association and American Academy of Pediatrics for high-risk patients, we recommend lipid and blood pressure screening beginning between 7 and 9 years of age in order to identify these risk factors for intervention at an early age [38,39,40,41].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Loukas M, Germain AS, Gabriel A, John A, Tubbs RS, Spicer D. Coronary artery fistula: a review. Cardiovasc Pathol. 2015;24:141–8.
Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28–40.
McNamara JJ, Gross RE. Congenital coronary artery fistula. Surgery. 1969;65:59–69.
Said SM, Burkhart HM, Schaff HV, Connolly HM, Phillips SD, Suri RM, et al. Late outcome of repair of congenital coronary artery fistulas - a word of caution. J Thorac Cardiovasc Surg. 2013;145:455–60.
Liberthson RR, Sagar K, Berkoben JP, Weintraub RM, Levine FH. Congenital coronary arteriovenous fistula report of 13 patients, review of the literature and delineation of management. Circulation [Internet]. 1979;59:849–54. Available from: http://ahajournals.org.
Sherwood MC, Rockenmacher S, Colan SD, Geva T. prognostic significance of clinically silent coronary artery fistulas. Am J Cardiol. 1999;83:407–11.
Burch GH, Sahn DJ. Congenital coronary artery anomalies: the pediatric perspective. Coron Artery Dis [Internet]. 2001;12:605–16. Available from: http://journals.lww.com/coronary-artery.
Sakakibara S, Yokoyama M, Takao A, Nogi M, Gomi H. Coronary arteriovenous fistula Nine operated cases. Am Heart J. 1966;307–14.
Latson LA. Coronary artery fistulas: How to manage them. Catheterization and Cardiovascular Interventions. Wiley-Liss Inc.; 2007. p. 111–8.
•• Gowda ST, Latson L, Sivakumar K, Hiremath G, Crystal M, Law M, et al. Anatomical classification and posttreatment remodeling characteristics to guide management and follow-up of neonates and infants with coronary artery fistula: a multicenter study from the Coronary Artery Fistula Registry. Circ Cardiovasc Interv. 2021;14:E009750. This study presents multicenter outcomes data in children after CAF closure. The authors describe a post-closure remodeling classification system which may correlate with risk for long-term complications after invasive management of CAFs.
Reddy G, Davies JE, Holmes DR, Schaff HV, Singh SP, Alli OO. Coronary artery fistulae. Circ Cardiovasc Interv: Lippincott Williams and Wilkins; 2015.
Kamiya H, Yasuda T, Nagamine H, Sakakibara N, Nishida S, Kawasuji M, et al. Surgical treatment of congenital coronary artery fistulas: 27 Years’ experience and a review of the literature. J Card Surg. 2002;17:173–7.
Vinograd CA, Ostermayer S, Lytrivi ID, Ko HH, Parness I, Geiger M, et al. Prevalence and outcomes of coronary artery ectasia associated with isolated congenital coronary artery fistula. Am J Cardiol. 2014;114:111–6.
Pisesky A, Nield LE, Rosenthal J, Jaeggi ET, Hornberger LK. Comparison of pre- and postnatally diagnosed coronary artery fistulae: echocardiographic features and clinical outcomes. J Am Soc Echocardiogr. 2022;35:1322–35.
• Al-Hijji M, El Sabbagh A, El Hajj S, AlKhouli M, El Sabawi B, Cabalka A, et al. Coronary artery fistulas: indications, techniques, outcomes, and complications of transcatheter fistula closure. JACC Cardiovasc Interv. 2021;14:1393–406. This report describes a decision-making algorithm for the transcatheter closure of CAFs, closure techniques, and a summary of recent reported outcomes of transcatheter fistula closure.
Velasco Forte MN, Byrne N, Valverde Perez I, Bell A, Gómez-Ciriza G, Krasemann T, et al. 3D printed models in patients with coronary artery fistulae: anatomical assessment and interventional planning. EuroIntervention. 2017;13:e1080–3.
Arar Y, Hussain T, Abou Zahr R, Gooty V, Greer JS, Huang R, et al. Fick versus flow: a real-time invasive cardiovascular magnetic resonance (iCMR) reproducibility study. J Cardiovasc Magn Reson. 2021;23:95.
Tangcharoen T, Bell A, Hegde S, Hussain T, Beerbaum P, Schaeffter T, et al. Detection of coronary artery anomalies in infants and young children with congenital heart disease by using MR imaging. Radiology. 2011;259:240–7.
Detorakis EE, Foukarakis E, Karavolias G, Dermitzakis A. Cardiovascular magnetic resonance and computed tomography in the evaluation of aneurysmal coronary-cameral fistula. J Radiol Case Rep. 2015;9:10–21.
Christmann M, Hoop R, Dave H, Quandt D, Knirsch W, Kretschmar O. Closure of coronary artery fistula in childhood: treatment techniques and long-term follow-up. Clin Res Cardiol. 2017;106:211–8.
Gowda ST, Forbes TJ, Singh H, Kovach JA, Prieto L, Latson LA, et al. Remodeling and thrombosis following closure of coronary artery fistula with review of management: large distal coronary artery fistula - To close or not to close? Catheter Cardiovasc Interv. 2013;82:132–42.
Yun G, Nam TH, Chun EJ. Coronary artery fistulas: pathophysiology, imaging findings, and management. Radiographics. 2018;38:688–703.
Ito H, Kamiyama T, Nakamura W, Segawa K, Takahashi K, Iijima T, et al. Coronary artery-pulmonary artery fistula originating from three major coronary branches associated with exertional chest pain and tachycardia-dependent left bundle branch block. Jpn Heart J. 1998;39:247–53.
Chiu C-Z, Shyu K-G, Cheng J-J, Ling S-C, Lee S-H, Hung H-F, et al. Angiographic and clinical manifestations of coronary fistulas in chinese people- 15-year experience. Circ J. 2008;72:1242–8.
Nagpal P, Khandelwal A, Saboo SS, Garg G, Steigner ML. Symptomatic coronary cameral fistula Heart Views. 2015;16:65–7.
Welisch E, Norozi K, Burrill L, Rauch R. Small coronary artery fistulae in childhood: a 6-year experience of 31 cases in a tertiary paediatric cardiac centre. Cardiol Young. 2016;26:738–42.
Valente AM, Lock JE, Gauvreau K, Rodriguez-Huertas E, Joyce C, Armsby L, et al. Predictors of long-term adverse outcomes in patients with congenital coronary artery fistulae. Circ Cardiovasc Interv. 2010;3:134–9.
Armsby LR, Keane JF, Sherwood MC, Forbess JM, Perry SB, Lock JE. Management of coronary artery fistulae patient selection and results of transcatheter closure. J Am Coll Cardiol. 2002;39:1026–32.
Hou B, Ma WG, Zhang J, Du M, Sun HS, Xu JP, et al. Surgical management of left circumflex coronary artery fistula: A 25-year single-center experience in 29 patients. Ann Thorac Surg. 2014;97:530–6.
Cheng TO. Management of coronary artery fistulas: Percutaneous transcatheter embolization versus surgical closure. Catheterization and Cardiovascular Interventions. Wiley-Liss Inc.; 1999. p. 151–2.
Vaidya YP, Green GR. Coronary artery fistula. J Card Surg. Blackwell Publishing Inc.; 2019. p. 1608–16.
Said SAM, Lam J, van der Werf T. Solitary coronary artery fistulas: a congenital anomaly in children and adults. A contemporary review. Congenit Heart Dis. 2006. p. 63–76.
Zhang W, Hu R, Zhang L, Zhu H, Zhang H. Outcomes of surgical repair of pediatric coronary artery fistulas. J Thorac Cardiovasc Surg. 2016;152:1123-1130.e1.
Thakkar B, Patel N, Poptani V, Madan T, Saluja T, Shukla A, et al. Clinical and angiographic follow-up of coronary artery fistula interventions in children: techniques and classification revisited. Cardiol Young. 2015;25:670–80.
Gowda ST, Latson LA, Kutty S, Prieto LR. Intermediate to long-term outcome following congenital coronary artery fistulae closure with focus on thrombus formation. Am J Cardiol. 2011;107:302–8.
Hsieh KS, Huang TC, Lee CL. Coronary artery fistulas in neonates, infants, and children: Clinical findings and outcome. Pediatr Cardiol. 2002;23:415–9.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. NLM (Medline); 2019. p. e596–646.
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart L and BI. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128 Suppl 5:S213–56.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140.
Stewart J, McCallin T, Martinez J, Chacko S, Yusuf S. Hyperlipidemia. Pediatr Rev. 2020;41:393–402.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1046–81.
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, S., Fares, M., Zellers, T.M. et al. Diagnosis and Management of Congenital Coronary Artery Fistulas in Infants and Children. Curr Cardiol Rep 25, 1921–1932 (2023). https://doi.org/10.1007/s11886-023-02007-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-02007-0