Abstract
The management of pediatric patients with coronary artery fistula (CAF) remains controversial because the clinical course of CAF may vary greatly from spontaneous closure to severe complications. The purpose of our study was to report the outcome of CAF in pediatric patients by using echocardiography as an evaluation tool. Between January 1997 and July 2003, 17 patients (age range, 5 months to 14 years; mean, 3.8 years) with coronary angiographically proven CAF were recruited. We divided patients into two groups. Group 1 (n = 4) included patients with symptoms related to CAF (n = 3), persistent coronary artery dilatation for 6 months (n = 4), and/or a continuous waveform of the fistula detected by Doppler (n = 3). Group 2 (n = 13) included patients who were asymptomatic, with normal coronary artery size or coronary artery dilatation less than 6 months, and/or a noncontinuous waveform of the fistula detected by Doppler. Group 1 patients received interventional therapy, whereas group 2 patients were managed conservatively. There were 6 male and 11 female patients. The correlation coefficient of coronary artery diameter measured on echocardiography and angiography was 0.935 and 0.834 in groups 1 and 2, respectively. The diameter of the involved coronary artery was 5.8-9.2 mm (mean, 7.50 ± 1.85) and 1.7-3.8 mm (mean, 2.72 ± 0.59) in group 1 and group 2, respectively. After transcatheter coil embolization, group 1 patients became asymptomatic with no residual fistula and had decrement of the coronary artery diameter (p = 0.035). All group 2 patients remained asymptomatic with no significant change in coronary artery size (p = 0.846) and 3 of them showed spontaneous closure of CAF. Persistent dilatation of the diameter of proximal coronary artery may be a useful parameter for determining subsequent application of interventional therapy. In patients with nonsignificant CAF, conservative follow-up is strongly suggested and intervention procedures may be unnecessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Coronary artery fistula (CAF) is an uncommon anomaly with an incidence of 0.26-0.40% [9, 16]. CAF is usually asymptomatic in children. However, in some cases if CAFs are undetected or untreated, aneurysmal dilatation, infective endocarditis, congestive heart failure, fistula rupture, myocardial infarction, ventricular arrhythmia, or even death may occur [1, 3, 6, 15]. Surgical closure or percutaneous coil occlusion of the fistula have been the preferred treatment methods [4, 7, 12]. However, spontaneous closure of CAF has also been documented on echocardiography [11, 14]. Therefore, the management of patients with CAF is controversial, particularly in asymptomatic pediatric patients. Usually, the clinical decision of interventional or surgical treatment relies on angiographic findings or abnormal hemodynamic status. Echocardiographic evaluation and follow-up of CAF has been described, but the criteria for treatment planning have not been well addressed [14]. The purpose of our study was to report the clinical application of echocardiography in the assessment of CAF in pediatric patients.
Materials and Methods
Between January 1997 and July 2003, 17 patients with CAF were recruited in our institution. Their age ranged from 5 months to 14 years (mean, 3.8 years). Fifteen patients had heart murmur on auscultation and 2 patients had Kawasaki disease. Three patients were symptomatic; 2 had exertional dyspnea and one had infective endocarditis. The remaining 14 patients were asymptomatic. The diagnosis of Kawasaki disease in 2 patients was based on fever ≥5 days and at least four of the following criteria: bilateral conjunctivitis, fissured lips and strawberry tongue, cervical lymphadenopathy, polymorphous exanthem, erythema palms and soles, and periungual desquamation on the subacute stage. Coronary angiography was performed in all patients after informed consent was obtained from the patient’s parents. Patients with complex or cyanotic heart disease, such as pulmonary atresia with intact ventricular septum, were excluded from our study.
The 17 patients were divided into two groups according to clinical presentations and echocardiographic findings. Patients in group 1 had sustained “significant” CAF that indicated the presence of symptoms related to CAF, persistent coronary artery dilatation for 6 months, and/or a continuous flow pattern of the fistula delineated on echocardiography. Patients in group 2 had “nonsignificant” CAF that indicated the absence of symptom, normal coronary artery size or transient coronary artery dilatation less than 6 months with subsequent normalization on follow-up echocardiogram, and/or a noncontinuous pattern flow of the fistula detected on echocardiography. All patients were regularly followed by echocardiography every 3-6 months. Group 1 patients received interventional therapy, whereas group 2 patients were managed conservatively. Echocardiography was performed with a SONOS 5500 cardiac scanner (Philips, Andover, MA, USA). Five- to 8-MHz sector phased array transducers were used for this study. Two-dimensional echocardiography was performed to visualize the diameter of the right and left coronary arteries on the parasternal short-axis view of the aorta. The coronary artery size was defined as dilated when its diameter was >3 mm in patients ≤5 years old and >4 mm in patients >5 years old. Color Doppler was performed from the parasternal, apical, and subcostal approaches in order to identify a mosaic-colored flow in any of the four cardiac chambers or the pulmonary artery. Unusual flow pattern was further evaluated by pulse. Doppler to determine continuous or noncontinuous waveforms. The whole course of CAF from the origin to the drainage sites was carefully evaluated. Images and all measurements were analyzed and stored on VHS format videotape. The anatomic delineation of the fistula made by angiography was compared with echocardiography. The diameter of the coronary artery was estimated using magnification correction by comparing it with known angiographic catheter diameters.
Statistical Analysis
Measurements are expressed as mean values ± SD. We compared the clinical data of group 1 and 2 patients by Fisher’s exact test. The Pearson correlation coefficient was used to assess echocardiographic and angiographic variability. The unpaired t-test was used for age and the duration of follow-up. The paired t-test was used to compare the first and latest proximally involved coronary artery diameter by echocardiography. Statistical analysis was performed using the Statistics Package for Social Sciences (SPSS, Chicago, IL, USA). A p value < 0.05 was considered statistically significant.
Results
There were 6 male and 11 female patients. According to our criteria, there were 4 patients in group 1 and 13 patients in group 2. Table 1 summarized the clinical data, management, and follow-up status of both groups. There were no significant differences in age (p = 0.226), sex (p = 0.555), the presence of cardiomegaly (cardiothoracic ratio > 0.5 on chest x-ray) (p = 0.579), abnormal ECG (changes consistent with ischemia) (p = 0.219), associated anomalies (p = 0.675), and the duration of follow-up (p = 0.652) between groups 1 and 2. The only significant clinical factor was the presence of continuous heart murmur (p = 0.0061). Associated cardiac anomalies were found in 10 patients: 2 in group 1 and 8 in group 2. The anomalies included isolated mitral regurgitation (n = 2), patent ductus arteriosus (n = 2), patent ductus arteriosus and ventricular septal defect (n = 1), atrial septal defect (n = 3), pulmonary stenososis (n = 1), and mitral valve prolapse and mitral regurgitation (n = 1).
The diameter of the involved coronary arteries was 5.8-9.2 mm (7.50 ± 1.85) in group 1 and 1.7-3.8 mm (2.72 ± 0.59) in group 2. The correlation coefficients of echocardiography and angiography of coronary artery diameter were high in group 1 (7.50 ± 1.85 vs 8.10 ± 1.59 mm, p = 0.935) and group 2 (2.72 ± 0.59 vs 2.97 ± 0.61 mm, p = 0.834). During follow-up, the coronary artery diameter had decrement in size in group 1 patients after transcatheter occlusion, with statistical significance (diameter before vs after transcatheter occlusion, 7.50 ± 1.85 vs 5.33 ± 2.66 mm, p = 0.035), whereas the involved coronary artery size showed no significant change in group 2 (initial evaluation vs final follow-up, 2.72 ± 0.59 vs 2.94 ± 0.45 mm, p = 0.846).
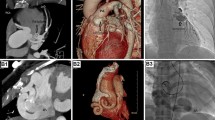
Twenty fistulae from 17 patients were identified by angiography. Eight fistulae (40%) originated from the right coronary artery, 11 (55%) from the left anterior descending coronary artery, and 1 (5%) from the left circumflex coronary artery. The pulmonary artery is the most common site of termination (15 fistulae, 75%). Two CAFs terminated at the right atrium and 3 at the right ventricle. Doppler color-flow mapping allowed precise definition of the site of the drainage of the fistula by revealing a mosaic flow in the receiving chamber except in 2 patients (1 with atrial septal defect and 1 with pulmonary stenosis). Three out of 4 group 1 patients had CAFs complicated with aneurysm formation (Fig. 1). Group 2 patients were characterized by normal size of the proximal coronary arteries and tortuous course of the fistula (Fig. 2). Three out of 13 group 2 patients had multiple CAFs.
(A) Echocardiogram in parasternal short-axis view shows a dilated right coronary with distal stenosis. The fistula can be traced into the right atrium (RA). (B) Right coronary angiogram (right anterior oblique projection) shows a large feeding artery that arises proximally from the fight coronary artery into the RA. (C) Complete occlusion following placement of two coils. (D) Repeat right coronary angiogram 1 year after coil occlusion shows the aneurysms had completely obturated. AO, aorta; PA, pulmonary artery.
(A) Color-flow mapping in parasternal short-axis view shows an abnormal antegrade flow (arrow) in the pulmonary artery. (B) An abnormal diastolic flow in the proximal artery by Doppler is noted. (C and D) Selective coronary angiograms show two fistulae (arrowheads) from the right and left coronary arteries to the pulmonary artery (P) respectively. Both coronary arteries are normal in size without dilatation.
Discussion
CAF is a rare cardiac anomaly. Although most CAF is congenital in origin, this anomaly is rarely diagnosed in infancy. In our study, the mean age of diagnosis was 3.8 years, and only two cases were detected by echocardiography within 1 year of age. It may reflect that CAFs in pediatric patients were usually asymptomatic or with nonspecific symptoms and thus easily overlooked by the physicians. The etiologies of acquired CAF include cardiac surgery, trauma, and myocardiac infarction [3]. Kawasaki disease complicated with CAF is very rare and, to our knowledge, only two cases have been reported [2]. In our study, CAF was noted in two patients on echocardiography after the presentation of Kawasaki disease. Both patients had fulfilled the criteria for the diagnosis of Kawasaki disease. They had no audible heart murmur in the acute stage of the disease and CAF was disclosed on the subacute stage. The pathophysiology may be related to acute coronary artery vasculitis with secondary revascularization.
Management of CAF patients depends on symptoms or complications of CAF. Consistent with prior reports [5, 7, 8, 10], we found that the presence of a continuous heart murmur in young patients may be a useful parameter to determine treatment methods. Three out of four group 1 patients who had continuous heart murmur also had persistent coronary artery dilatation and significant CAF on echocardiography. On the other hand, none of the group 2 patients had continuous heart murmur, and the diameters of the involved coronary arteries remained stable during follow-up.
Since precise demonstration of the origin, course, and site of drainage is needed for complete evaluation of CAF, angiography remains the gold standard. However, using angiography as a screening and routine follow-up modality is of doubtful practicality. Echocardiography is noninvasive and has several advantages in evaluating pediatric CAF patients. First, the sensitivity of echocardiography in the detection of CAF was good, and there were no false-positive cases in our studies. Second, the diameters of the involved proximal coronary arteries measured on echocardiography were well correlated with angiography.
Consistent with the results of Shakudo et al. [13], our study showed that the pulmonary artery is the most common site of drainage of CAF. In these patients, an antegrade flow can be detected in the main pulmonary artery during diastole by color Doppler (Fig. 2A). In the past, this kind of CAF was difficult to detect or was an incidental finding on angiography performed for other reasons. The differentiated diagnosis of abnormal flow in the pulmonary artery on echocardiography includes small patent ductus arteriosus (PDA), major aortopulmonary collateral arteries, and anomalous origin of the coronary artery. Small PDA may show abnormal diastolic flow in the pulmonary artery that is characterized by a high-velocity jet from the aorta to the pulmonary bifurcation in a retrograde manner. Color-flow mapping is helpful in distinguishing CAF from PDA by the flow direction and location. In this study, three CAFs associated with PDA could be clearly demonstrated on color Doppler. The major aortopulmonary collateral artery can also cause an abnormal flow in the pulmonary artery that is usually associated with cyanotic heart disease and pulmonary artery hypoplasia. Thus, it can easily be differentiated from isolated CAF. An anomalous origin of the left coronary artery from the pulmonary artery is rare, and this lesion always occurs with ventriculomegaly, myocardial dysfunction, and mitral regurgitation. Detailed evaluation of the origin of the coronary artery with antegrade flow allows differentiation of this lesion from CAF.
In our study, all group 2 patients were conservatively managed. Among these patients, 3 had spontaneous closure of CAF and the remaining 10 patients showed excellent prognosis without any symptoms on midterm follow-up (4-79 months; mean, 30). Echocardiography also revealed a regressive or stable condition of CAF. From our experience, for pediatric patients with nonsignificant CAF, conservative follow-up is strongly suggested and interventional procedures may be unnecessary.
On the other hand, all four patients in group 1 with persistent coronary artery dilatation were successfully treated with transcatheter coil embolization. Among them, three symptomatic patients became asymptomatic with regression of CAF. However, regarding the remaining asymptomatic patient, despite successful coil embolization, the application of interventional or conservative treatment in such patients remains controversial. Only after knowledge of the natural course of CAF with persistent coronary artery dilatation in the absence of treatment has been obtained can we address the issue of curability using interventional methods. However, our study is limited because there were only a small number of cases. Nevertheless, we believe that persistently dilated proximal diameter of the coronary arteries may be a useful parameter for determining treatment, but more cases must be collected before a definitive conclusion on using the coronary artery diameter as an absolute independent variable can be drawn.
In summary, persistent dilatation of the diameter of the proximal coronary artery may be a useful parameter for determining subsequent application of interventional therapy. In patients with nonsignificant CAF, conservative follow-up is strongly suggested and intervention procedures may be unnecessary.
References
N Corvaja JW Moses FE Vogel et al. (1999) ArticleTitleExercise-induced ventricular tachycardia associated with coronary arteriovenous fistula and correction by transcatheter coil embolization Cathet Cardiovasc Intervent 46 470–472 Occurrence Handle10.1002/(SICI)1522-726X(199904)46:4<470::AID-CCD20>3.0.CO;2-1 Occurrence Handle1:STN:280:DyaK1M3ivFyiuw%3D%3D
PR Koenig TR Kimball DC Schwartz (1993) ArticleTitleCoronary artery fistula complicating the evaluation of Kawasaki disease Pediatr Cardiol 14 179–180 Occurrence Handle10.1007/BF00795651 Occurrence Handle1:STN:280:ByuD387msV0%3D Occurrence Handle8415224
RR Liberthson K Sagar JP Berkoben RM Weintraub FH Levine (1979) ArticleTitleCongenital coronary arteriovenous fistula. Report of 13 patients, review of the literature and delineation of management Circulation 59 849–854 Occurrence Handle1:STN:280:CSaC2cjksVI%3D Occurrence Handle428095
C Mavroudis CL Backer AP Rocchini AJ Muster M Gevitz (1997) ArticleTitleCoronary artery fistulas in infants and children: a surgical review and discussion of coil embolization Ann Thorac Surg 63 1235–1242 Occurrence Handle10.1016/S0003-4975(97)00251-8 Occurrence Handle1:STN:280:ByiB1M7ns1w%3D Occurrence Handle9146308
CJ McMahon MR Nihill JP Kovalchin CE Mullins RG Grifka (2001) ArticleTitleCoronary artery fistula. Management and intermediate-term outcome after transcatheter coil occlusion Tex Heart Inst J 28 21–25 Occurrence Handle1:STN:280:DC%2BD3MvpsVarsw%3D%3D Occurrence Handle11330735
T Misumi K Nishikawa M Yasudo T Suzuki H Kumamaru (2001) ArticleTitleRupture of an aneurysm of a coronary arteriovenous fistula Ann Thorac Surg 71 2026–2027 Occurrence Handle1:STN:280:DC%2BD3Mzms1ajtw%3D%3D Occurrence Handle11426793
M Okubo D Nykanen LN Benson (2001) ArticleTitleOutcomes of transcatheter embolization in the treatment of coronary artery fistulas Cathet Cardiovasc Intervent 52 510–517 Occurrence Handle10.1002/ccd.1114 Occurrence Handle1:STN:280:DC%2BD3MzisVKksA%3D%3D
SB Perry J Rome JF Keane DS Baim JE Lock (1992) ArticleTitleTranscatheter closure of coronary artery fistulas J Am Coll Cardiol 20 205–209 Occurrence Handle1:STN:280:By2B1MbotlM%3D Occurrence Handle1607526
GS Reeder AJ Tajik HC Smith (1980) ArticleTitleVisualization of coronary artery fistula by two-dimensional echocardiography Mayo Clin Proc 55 185–189 Occurrence Handle1:STN:280:Bi%2BC3Mbht1c%3D Occurrence Handle7354655
JF Reidy RT Anjos SA Qureshi EJ Baker MJ Tynan (1991) ArticleTitleTranscatheter embolization in the treatment of coronary artery fistulas J Am Coll Cardiol 18 187–192 Occurrence Handle1:STN:280:By6B28fjvFw%3D Occurrence Handle2050921
JM Schleich C Rey M Gewillig A Bozio (2001) ArticleTitleSpontaneous closure of congenital coronary artery fistulas Heart 85 E6 Occurrence Handle10.1136/heart.85.4.e6 Occurrence Handle1:STN:280:DC%2BD3M3msFKhtQ%3D%3D Occurrence Handle11250983
G Schumacher A Roithmaier HP Lorenz et al. (1997) ArticleTitleCongenital coronary artery fistula in infancy and childhood: diagnostic and therapeutic aspects Thorac Cardiovasc Surg 45 287–294 Occurrence Handle1:STN:280:DyaK1c7jsl2nug%3D%3D Occurrence Handle9477461
M Shakudo J Yoshikawa K Yoshida Y Yamaura (1989) ArticleTitleNoninvasive diagnosis of coronary artery fistula by Doppler color flow mapping J Am Coll Cardiol 13 1572–1577 Occurrence Handle1:STN:280:BiaB2MnjsFU%3D Occurrence Handle2723269
MC Sherwood S Rockenmacher SD Colan T Geva (1999) ArticleTitlePrognostic significance of clinically silent coronary artery fistulas Am J Cardiol 83 407–411 Occurrence Handle10.1016/S0002-9149(98)00878-9 Occurrence Handle1:STN:280:DyaK1M7ntVCnuw%3D%3D Occurrence Handle10072233
MG St. John Sutton GA Miller IH Kerr TA Traill (1980) ArticleTitleCoronary artery steal via large coronary artery to bronchial artery anastomosis successfully treated by operation Br Heart J 44 460–463 Occurrence Handle1:STN:280:Bi6D3sbhvVc%3D Occurrence Handle7426209
M Vavuranakis CA Bush H Boudoulas (1995) ArticleTitleCoronary artery fistulas in adults: incidence, angiographic characteristics, natural history Cathet Cardiovasc Diagn 35 116–120 Occurrence Handle1:STN:280:ByqA1crgs1E%3D Occurrence Handle7656302
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liang, CD., Ko, SF., Huang, CF. et al. Echocardiographic Evaluation of Coronary Artery Fistula in Pediatric Patients. Pediatr Cardiol 26, 745–750 (2005). https://doi.org/10.1007/s00246-004-0889-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-004-0889-9