Abstract
Summary
The risk of subsequent major osteoporotic and hip fracture following an initial fracture was increased in both sexes over 25 years, with modest time-dependent attenuation. This risk was highest in men, underscoring the importance of targeted treatment strategies particularly in this under-treated population.
Introduction
The risk of subsequent fractures is increased following an index fracture, and declines over time. We aimed to determine whether this risk was sustained over 25 years and evolved similarly in men and women.
Methods
Using population-based databases, we performed a matched cohort study in 16,876 men and 39,230 women ≥ 50 years who sustained an index fracture during 1989–2006. Rates of subsequent major osteoporotic fractures (MOF) and hip fractures until 2016 were compared to rates for matched controls (n = 160,983). Age- and sex-stratified cumulative incidences to 25 years were estimated in the presence of competing mortality. Hazard ratios (HRs) with 95% confidence intervals (CI) for subsequent fractures were estimated for each on the first 15 years of follow-up with a final category ≥ 15 years, adjusted for comorbidities.
Results
Risk for MOF and hip fractures remained elevated up to 25 years in both sexes. The cumulative incidence of fractures was higher in cases vs controls in both sexes and across all age categories except in those > 90 years. Crude rate ratios for subsequent MOF were 2.5 (95% CI 2.3–2.7) in men and 1.6 (95% CI 1.6–1.7) in women and were higher in the younger age groups. Adjusted HRs (aHRs) for subsequent MOF were higher in men than in women in the first year (men aHR 2.6, 95% CI 2.1–3.3; women aHR 1.6, 95% CI 1.4–1.7).
Conclusions
The risk of subsequent fractures following an initial fracture was increased over 25 years and the magnitude of risk was initially greater in men than in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals with a previous fracture are twice as likely to sustain subsequent fractures compared to those who are fracture-free [1, 2]. Age at the time of the initial fracture, skeletal site at which it occurred, and time elapsed since the fracture impact on subsequent fracture risk [3,4,5], following a hip fracture, von Friesendorff et al. observed a residual lifetime risk of recurrent fracture of 33% in men and of 45% in women [6, 7]. Those younger than 75 years of age at the time of fracture were at greater risk of subsequent fractures. The risk of a subsequent fracture has also been shown to be highest immediately following an index fracture at major osteoporotic sites (hip, spine, forearm, or humerus), declining progressively, but remaining higher than that of the general population [2, 4, 8,9,10,11,12]. The FRAX fracture risk assessment tool considers previous fracture, notwithstanding its timing, as an important clinical risk factor for future fracture. It is important to quantify whether this risk of subsequent fracture is sustained over the long term for accurate fracture risk assessment in older men and women who would have sustained fractures in the distant past.
Our objective was to determine the long-term risk of subsequent major osteoporotic fractures (MOF) and hip fractures following an initial fracture, in men and women separately, and to examine the change in risk over a 25-year period.
Methods
Study design and population
Using the linked comprehensive healthcare databases of the Manitoba Centre for Health Policy Data Repository (Canada), we performed a matched historical cohort study of men and women 50 years and older who sustained a first fracture between fiscal years 1989 and 2006. The Manitoba Centre for Health Policy Data Repository includes the population-based computerized databases of hospitalization discharge summaries, physician claims for services (billings), and vital statistics, which can all be linked through an anonymous personal identifier. Virtually all residents of the Province of Manitoba, Canada (population 1.3 million, 2016), receive health coverage through a publicly funded system and every encounter with the healthcare system is recorded in these databases. The accuracy and completeness of these databases for fracture outcomes have been described elsewhere [13, 14]. This study was approved by the Health Research Ethics Board of the University of Manitoba and data access was granted by the Health Information Privacy Committee of Manitoba.
We identified as cases all men and women aged 50 years and older who sustained a first fracture between April 1, 1989, and March 31, 2006. The entry date of an individual in the cohort was the date of a first fracture (index fracture) after age 50 years, on the condition of having had medical coverage from Manitoba Health for at least 5 years prior to the index fracture and continuous coverage after the index date.
Hospital discharge abstracts and physician claims databases were examined for the presence of fracture diagnostic codes at any skeletal site (categorized as hip, forearm, clinical spine, humerus, and other sites; excluding skull, hands, and feet fractures) using previously validated algorithms based on ICD-9-CM (prior to 2004) and ICD-10-CA codes [15, 16]. In addition, hip and forearm fractures were required to have concurrent site-specific physician claims for fixation, reduction, or casting to enhance specificity for an acute fracture event. Traumatic fractures (1677 fractures) were identified as such using trauma diagnostic codes and were excluded from the analyses.
Three controls for each case were selected and matched on a fiscal year basis by sex and age (within 5 years) and assigned the same index date as the matched case. Controls were required to have continuous health coverage for at least 5 years prior to their case’s index date and their records be free of fracture diagnosis codes during that period. Using a wider caliper for age matching (5 years) allowed us to identify 3 controls for each case.
Cases and controls living in a long-term care facility at the index date were included in the cohort (but were not matched on residential status). Control selection was done without replacement within a fiscal year and with replacement for each new fiscal year.
Subsequent fracture outcomes
We assessed longitudinal records for the presence of non-traumatic hip and major osteoporotic fracture (MOF: hip, clinical spine, forearm, and proximal humerus) diagnostic codes, as previously described, following the index date up to March 31, 2016, allowing for at least 10 years and up to 25 years of follow-up.
To minimize misclassification of incident and subsequent fractures, a 15-day washout period was applied to cases and their controls for subsequent fractures at any sites to avoid double counting. Furthermore, a 12-month washout was applied for a subsequent non-hip fracture affecting the same site (e.g., forearm fracture after forearm fracture) and a 3-month washout was applied for a subsequent hip fracture after a previous hip fracture. All individuals were followed until the occurrence of subsequent fractures, death, termination of provincial healthcare coverage due to relocation, or the study end date of March 31, 2016.
Covariates
The John Hopkins Ambulatory Care Group (ACG) system (version 9) was used to develop a comorbidity index for cases and controls [17]. Ambulatory diagnostic groups (ADGs) represent 32 comorbidity clusters. The number of ADGs for each subject at the time of entry into the cohort was documented from the hospital and physician medical records and categorized as none, 1–2, 3–5, and 6 or more.
Statistical analysis
Continuous variables were reported as means with standard deviations (SDs), and counts with percentages. Annual crude rates in cases and in controls per 1000 person-years of observation and cumulative incidence for subsequent MOF or hip fractures were estimated, accounting for competing risk of mortality [18], and stratified by sex and age groups (50–59, 60–69, 70–79, 80–89, and 90+ years). Crude relative rate ratios (RRs; cases/controls) for subsequent MOF or hip fracture were generated separately for men and women, by index fracture site. Unadjusted and comorbidity-adjusted hazard ratios (HRs) with 95% confidence intervals (CI) for subsequent MOF and hip fractures (cases versus controls) following an initial fracture were estimated for men and women from Cox proportional hazard models for each on the first 15 years of follow-up with a final category for > 15 years. Number of ADG comorbidities was entered into the model as a time-fixed covariate. All analyses were conducted using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC).
Results
During the study period, there were 16,876 initial fractures in men and 39,230 (70%) in women, for a total of 56,106 cases to whom we matched 160,983 controls. Initial fractures were identified at the following skeletal sites: 11,028 (20%) forearm, 9313 (17%) hip, 5799 (10%) humerus, 3554 clinical spine (6%), and 28,089 (50%) at other sites (Table 1). The cohort was followed for up to 25 years (cases: mean 9.9 [SD 7.1] years, range 0–27.0 years; controls: mean 11.0 [SD 7.0] years, range 0–27.0 years).
The overall annual rate, per 1000 person-years of observation, of subsequent MOF following an initial MOF among cases was 18.5 (95% CI: 17.3–19.8) in men and 29.6 (95% CI: 28.28.8–30.4) in women, and following an initial hip fracture was 26.2 (95% CI: 23.3–29.6) in men and 34.8 (95% CI: 32.9–36.7) in women. For subsequent hip fracture, the rate was 9.2 (95% CI: 8.4–10.0) in men and 13.8 (95% CI: 13.3–14.3) in women following a MOF, and 14.5 (95% CI: 12.5–16.8) in men and 18.3 (95% CI: 17.1–19.7) in women following a hip fracture. Subsequent fracture rates were highest in the older age groups (over the age of 70 years) following an initial fracture at all sites (Supplemental Table 1). Absolute risk differences in MOF and hip fractures in men and women, by age groups, are shown in Supplemental Table 2; in the older age groups (age 60 years and older), absolute differences in rates of MOF and hip fracture were higher in men than in women.
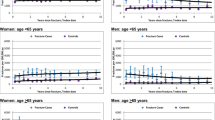
The cumulative incidence to 25 years of subsequent MOF and hip fractures following an initial MOF was higher in cases vs in controls for both sexes and across all age categories except for > 90 years where this relationship reversed due to competing mortality (Fig. 1). The highest cumulative incidence of subsequent fracture was observed in women in the age groups 60–69 years and 70–79 years for subsequent MOF and in age groups 70–79 years for subsequent hip fractures. The cumulative incidence of subsequent MOF and hip fractures was highest after a humerus, forearm, and spine fracture.
In general, the crude relative RRs of subsequent MOF and hip fractures in cases compared to controls over the entire study period of 25 years were higher in men and in younger age groups (Table 2). Over all ages, RRs were 2.5 (95% CI: 2.3–2.7) in men and 1.6 (95% CI: 1.6–1.7) in women for MOF following a MOF, and 2.1 (95% CI: 1.9–2.3) in men and 1.5 (95% CI: 1.5–1.6) in women for a hip fracture following a MOF. RRs were highest in younger men after a hip fracture (6.0 [95% CI: 3.4–10.6]), humerus fracture, and MOF, and were lowest in older men and women (over the age 80 years) following a fracture at most skeletal sites.
Unadjusted HRs (cases versus controls) for subsequent MOF or subsequent hip fracture following an initial MOF were higher in men than in women in the first year following the index fracture (MOF following MOF: HR 3.3, 95% CI: 2.6–4.1 in men and 1.8, 95% CI: 1.7–2.0 in women; hip fracture following MOF: HR 2.8, 95% CI: 2.1–3.8 in men and 2.0, 95% CI: 1.8–2.3 in women) (Figs. 2 and 3). Following adjustment for number of comorbidities, the risk in the first year was slightly attenuated, but retained a similar pattern for subsequent MOF following a MOF: aHR 2.62, 95% CI: 2.1–3.3 in men and 1.6, 95% CI: 1.4–1.7 in women; and for subsequent hip fracture following MOF: aHR 2.1, 95% CI: 1.7–3.2 in men and 1.7, 95% CI: 1.5–1.9 in women. The risk declined in both men and women over time but remained elevated even more than 15 years after the index fractures (MOF after initial MOF: aHR 1.7, 95% CI 1.2–2.2 in men; 1.4, 95% CI 1.3–1.6 in women; and hip fracture after MOF: aHR 1.7, 95% CI 1.2–2.4 in men; 1.5, 95% CI 1.3–1.7 in women). A similar pattern was seen for subsequent MOF following any low-trauma fracture (MOF + other sites) in men in the first year with an aHR 2.6 (95% CI: 2.2–3.1) and aHR 1.5 (95% CI: 1.3–1.9) for > 15 years, whereas in women, the aHR in the first year was 1.8 (95% CI: 1.7–1.9) and was 1.3 (95% CI: 1.2–1.4) for > 15 years.
Discussion
Following an initial fracture at any skeletal site, the risk of subsequent MOF and hip fracture was elevated compared to age- and sex-matched controls in both sexes over 25 years, with a modest time-dependent attenuation. The cumulative incidence over the study period of subsequent MOF and hip fractures was higher in cases vs in controls for both sexes and across all age categories even after accounting for the competing risk of mortality, with the exception of the very elderly group (> 90 years). This risk of subsequent fracture was higher in men, even after adjustment for number of comorbidities, particularly in the years immediately after the index fracture.
Low-trauma fractures have been linked to increased risk of subsequent fractures in previous studies, including our own [1, 9, 19]. The risk of subsequent fractures has been extensively researched, particularly in women, and observed in the first 10 years’ post-fracture [20, 21]. In the Dubbo Osteoporosis Epidemiology study (1989–2010, 343 initial fractures in men and 952 in women, 60 years and older), the relative risk of subsequent fracture was increased two- to four-fold following an initial fracture of the hip, the spine, or a non-vertebral-non-hip skeletal site [22]. Furthermore, the risks were particularly elevated in the younger age groups (60 to 74 years) and in men following a hip and spine fracture (relative risk [RR] 4.01; 95% CI, 1.48–10.87, and RR 6.95; 95% CI, 3.64–13.25, respectively). In the Study for Osteoporotic Fractures of 8049 women (mean age 73, SD 5 years), a proximal humerus fracture was associated with an 83% increase in the risk of subsequent fracture, compared with women without a humerus fracture, over an average period of observation of 10 years [11]. In a study among 377,561 US women 65 years and older, 10%, 18%, and 31% of women fractured again within 1, 2, and 5 years following their initial fracture, regardless of the initial fracture site [23]. Finally, Soreskog and colleagues documented a 3-fold risk of subsequent MOF following an index hip fracture over a 60-month period in a cohort of 231,769 Swedish women aged 50 years and older, with a time-attenuation effect similar to what we have presented [24].
The time dependency of fracture risk has drawn attention, since the early phase of highest risk might create an opportunity for early intervention [25,26,27]. Time interval since the initial fracture has been documented to impact the risk of subsequent fracture conveying a higher immediate risk in those who have sustained a more recent fracture [4, 11, 28]. In the Funen County Hip Fracture Study, the risk of sustaining a second hip fracture was found to be highest in the first 12 months following a first hip fracture, with 50% of recurrent fracture occurring within 12 months in men and within 19 months in women [29]. In another population-based study of 4140 postmenopausal women (aged 50 to 90 years), subsequent fractures after an initial fracture were documented: the relative risk of re-fracture was 5.3 (95% CI: 4.0–6.6) within 1 year following the initial fracture, 2.8 (95% CI: 2.0–3.6) within 2–5 years, 1.4 (95% CI: 1.0–1.8) within 6–10 years, and 0.41 (95% CI: 0.29–0.53) after > 10 years [30]. The Reykjavik Study fracture registration study provides insight into the time dependency of the recurrent fracture risk in a larger population of 18, 872 Icelandic men and women with a sentinel fracture, assessed over a period of 27 years [5]. In those who experienced a subsequent fracture, at least 30% of these fractures occurred within the first year. As in our study, the annual incidence of subsequent fracture was higher in women than in men and increased with age. The risk for MOF was highest immediately after the first fracture and decreased over time but remained higher than that of the population at risk throughout follow-up, similarly to what we have documented. Though the pattern of fracture risk over time was similar to what we report in this study, the risks for any subsequent osteoporotic fracture were up to two-fold higher than those we computed, specifically in men. These differences could be in part due to population-specific characteristics (for example, in our models, we adjusted for comorbidities) and baseline fracture risk, ascertainment of fracture events including methods, and time windows used to avoid double counting of subsequent fractures.
The reasons behind the increased risk in fracture are many and include loss of muscle strength and impaired balance, increased risk of falls, change in cognition, presence of comorbidities, and bone loss following in the period following the fracture [25, 31]. Higher complication rates and mortality have been documented in men following fractures, even after adjusting for the presence of comorbidities [32, 33].
The strengths of this study include the use of a population-based comprehensive registry that includes virtually the entire population of the Manitoba and many fracture outcomes in men and in women allowing for robust sex- and age-stratified analyses, a period of follow-up that spans over two decades, and consideration of the presence of comorbidities and of competing risk of mortality in the analyses. There are limitations to observational studies such as outcome ascertainment leading to misclassification of some fractures, particularly vertebral fractures. To minimize this bias, we have used fracture definitions that have previously been validated [16, 34]. Furthermore, to avoid double counting of fractures in the short time frame, we have used a period of 6 months (washout) before counting a second fracture at the same site. Similarly, all comorbidities may not be captured by claims coding or may be miscoded. We did not have access to anti-osteoporosis medication use in cases and controls, and could not account for their potential protective effect on subsequent fracture risk. However, in a similar population-based study in Manitoba in fiscal years 2000–2014, we have documented that only 14.3% of men and women who had sustained a major osteoporotic fracture received anti-osteoporosis medication in the 14 months following the fracture, making it unlikely that medication use would have a significant impact on our results [35].
The risk of subsequent MOF and hip fracture following an initial MOF was increased in both sexes over a 25-year period. Our results support the importance of a previous fracture in fracture risk assessment, even if sustained in the distant past. As others have also shown, the risk for subsequent fractures was highest in men and in the younger age groups. These results underscore the importance of timely recognition of fracture events and effective interventions that reduce fracture risk, especially in men, a population in whom secondary prevention is under-implemented.
References
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA III, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. JBone MinerRes 15:721–739
Morin SN, Lix LM, Leslie WD (2014) The importance of previous fracture site on osteoporosis diagnosis and incident fractures in women. J Bone Miner Res 29:1675–1680
Giangregorio LM, Leslie WD, Manitoba Bone Density P (2010) Time since prior fracture is a risk modifier for 10-year osteoporotic fractures. J Bone Miner Res 25:1400–1405
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
von Friesendorff M, Besjakov J, Akesson K (2008) Long-term survival and fracture risk after hip fracture: a 22-year follow-up in women. J Bone Miner Res 23:1832–1841
von Friesendorff M, McGuigan FE, Besjakov J, Akesson K (2011) Hip fracture in men-survival and subsequent fractures: a cohort study with 22-year follow-up. J Am Geriatr Soc 59:806–813
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res 24:1299–1307
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394
Huntjens KM, Kosar S, van Geel TA, Geusens PP, Willems P, Kessels A, Winkens B, Brink P, van Helden S (2010) Risk of subsequent fracture and mortality within 5 years after a non-vertebral fracture. Osteoporos Int 21:2075–2082
Clinton J, Franta A, Polissar NL, Neradilek B, Mounce D, Fink HA, Schousboe JT, Matsen FA 3rd (2009) Proximal humeral fracture as a risk factor for subsequent hip fractures. J Bone Joint Surg Am 91:503–511
Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K, Lorentzon M, Liu E, Vandenput L, McCloskey EV (2021) The effect on subsequent fracture risk of age, sex, and prior fracture site by recency of prior fracture. Osteoporos Int
Roos LL, Mustard CA, Nicol JP, McLerran DF, Malenka DJ, Young TK, Cohen MM (1993) Registries and administrative data: organization and accuracy. MedCare 31:201–212
Roos LL, Walld RK, Romano PS, Roberecki S (1996) Short-term mortality after repair of hip fracture. Do Manitoba elderly do worse? MedCare 34:310–326
Roos NP, Shapiro E (1999) Revisiting the Manitoba Centre for Health Policy and Evaluation and its population-based health information system. Med Care 37:JS10–JS14
O’Donnell S, Canadian Chronic Disease Surveillance System Osteoporosis Working G (2013) Use of administrative data for national surveillance of osteoporosis and related fractures in Canada: results from a feasibility study. Arch Osteoporos 8:143
Smith NS, Weiner JP (1994) Applying population-based case mix adjustment in managed care: the Johns Hopkins Ambulatory Care Group system. ManagCare Q 2:21–34
Leslie WD, Lix LM, Wu X, Manitoba Bone Density P (2013) Competing mortality and fracture risk assessment. Osteoporos Int 24:681–688
Langsetmo L, Goltzman D, Kovacs CS, Adachi JD, Hanley DA, Kreiger N, Josse R, Papaioannou A, Olszynski WP, Jamal SA (2009) Repeat low-trauma fractures occur frequently among men and women who have osteopenic BMD. J Bone Miner Res 24:1515–1522
Hansen L, Petersen KD, Eriksen SA, Langdahl BL, Eiken PA, Brixen K, Abrahamsen B, Jensen JE, Harslof T, Vestergaard P (2015) Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int 26:513–519
Gehlbach S, Saag KG, Adachi JD, Hooven FH, Flahive J, Boonen S, Chapurlat RD, Compston JE, Cooper C, Díez-Perez A, Greenspan SL, LaCroix AZ, Netelenbos JC, Pfeilschifter J, Rossini M, Roux C, Sambrook PN, Silverman S, Siris ES, Watts NB, Lindsay R (2012) Previous fractures at multiple sites increase the risk for subsequent fractures: the Global Longitudinal Study of Osteoporosis in Women. J Bone Min Res : the official journal of the American Society for Bone and Mineral Research 27:645–653
Bliuc D, Nguyen TV, Eisman JA, Center JR (2014) The impact of nonhip nonvertebral fractures in elderly women and men. J Clin Endocrinol Metab 99:415–423
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30:79–92
Söreskog E, Ström O, Spångéus A, Åkesson KE, Borgström F, Banefelt J, Toth E, Libanati C, Charokopou M (2020) Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 134:115286
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28:1765–1769
Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N, Lorentzon M, Cooper C, Rizzoli R, Adib G, al-Daghri N, Campusano C, Chandran M, Dawson-Hughes B, Javaid K, Jiwa F, Johansson H, Lee JK, Liu E, Messina D, Mkinsi O, Pinto D, Prieto-Alhambra D, Saag K, Xia W, Zakraoui L, Reginster JY (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12
Compston JE, Drake MT (2020) Defining very high fracture risk: is FRAX fit for purpose? J Bone Miner Res 35:1399–1403
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Nymark T, Lauritsen JM, Ovesen O, Röck ND, Jeune B (2006) Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int 17:1353–1357
van Geel TA, van Helden S, Geusens PP, Winkens B, Dinant GJ (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22:2439–2448
Morin S, Lix LM, Azimaee M, Metge C, Majumdar SR, Leslie WD (2012) Institutionalization following incident non-traumatic fractures in community-dwelling men and women. Osteoporos Int 23:2381–2386
Lix L, Azimaee M, Osman B, Caetano P, Morin S, Metge C, Goltzman D, Kreiger N, Prior J, Leslie W (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Cui Y, Lix LM, Yang S, Morin SN, Leslie WD (2019) A population-based study of postfracture care in Manitoba, Canada 2000/2001–2014/2015. Osteoporos Int 30:2119–2127
Acknowledgements
We are indebted to Manitoba Health for providing data (HIPC No. 2008/2009-16, Theme 2). SNM is a scholar of the Fonds de Recherche du Québec en Santé and LML is supported by a Tier 1 Canada Research Chair.
Author information
Authors and Affiliations
Contributions
All authors substantially contributed to the conception (WDL) and design (WDL, LML), or analysis (WDL, LML, LY, and SNM) and interpretation of data (all); drafting the article (SNM) or revising it critically for important intellectual content (all); and final approval of the version to be published (all). WDL accepts full responsibility for the work and/or the conduct of the study, had full access to all the data, and controlled the decision to publish.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Disclaimer
The results and conclusions are those of the authors, and no official endorsement by Manitoba Health is intended or should be inferred.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 105 kb)
Rights and permissions
About this article
Cite this article
Morin, S.N., Yan, L., Lix, L.M. et al. Long-term risk of subsequent major osteoporotic fracture and hip fracture in men and women: a population-based observational study with a 25-year follow-up. Osteoporos Int 32, 2525–2532 (2021). https://doi.org/10.1007/s00198-021-06028-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06028-9