Abstract
Summary
Fractures after the age of 50 are frequently observed in Denmark, and many of these may be osteoporotic. This study examined the incidence of all and subsequent fractures in a 10-year period from 2001 to 2011. The incidence of subsequent fractures was high, especially following hip fracture.
Introduction
The purpose of this study is to examine patterns of subsequent fractures and mortality rates over a 10-year period in patients already suffering from fracture.
Methods
The study was designed as a nationwide, register-based follow-up study. Patients were included if diagnosed with an index fracture (ICD-10 codes: S22.x, S32.x, S42.x, S52.x, S62.x, S72.x, S82.x, S92.x, T02.x, T08.x, T10.x and T12.x) between January 1st, 2001 and December 31st, 2001 and if older than 50 years at time of fracture. The patients were investigated for future subsequent fractures from January 1st, 2002 to December 31st, 2011.
Results
In this study, we demonstrated that patients with fractures (especially hip fractures) have a high risk of subsequent fractures, especially hip fracture. Other fractures, which are not commonly considered as osteoporotic fractures, such as lower leg, were frequently observed in the 10 years following index fracture. The cumulative incidence proportion (CIP) of subsequent fractures during the 10-year follow-up period was high for all recurrent fractures (9–46 %). Subsequent hip fracture, regardless of index fracture, had the highest CIP across the study period, ranging from 9 to 40 %. Appendicular fractures were often followed by a recurrent fracture, or subsequent fractures at a more proximal location in the same limb, i.e. forearm fractures were followed by humerus fractures. These results have not been previously demonstrated to this extent, and according to our knowledge, no previous studies have estimated cumulative 10-year subsequent fracture incidences for any non-hip fractures.
Conclusion
Patients suffering a fracture (and especially a hip fracture) have a high incidence of subsequent fracture. Fractures after the age of 50 may be considered an early warning of increased risk for future fractures in many patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures have typically been characterized as fractures of the hip, spine and forearm resulting from low energy trauma, although proximal humerus fractures may also be considered as osteoporotic fractures [1–3]. Clinically, osteoporosis is defined by a low bone mineral density (BMD), which is closely associated with increased risk of low energy trauma fractures [1, 4]. Thus, a diagnosis of osteoporosis can be made based on dual X-ray absorptiometry or in the presence of low energy fractures. In the latter case, fractures serve as a marker of low BMD or impaired bone quality. However, previous studies have shown that only the minority of fracture patients receive anti-osteoporotic medication [5, 6].
Osteoporotic fractures and hip fractures in particular have immediate consequences for patients such as increased mortality [7, 8] and transiently or permanently decreased health-related quality of life [9]. Furthermore, these fractures, of which a large part is preventable, entail substantial costs for society [5].
Fracture risk assessment tools [10, 11] have been used to primarily identify the risk of future hip fracture and of other major osteoporotic fractures (MOF) in order to predict a 10-year fracture probability. Fracture prevention programmes [12] have focused on identifying patients at risk of secondary low energy trauma fractures. Both fracture risk assessment tools and fracture prevention programmes apply risk factors for assessment. The most important risk factors include age and gender, which are associated with both increased risk of falling and decreased bone strength [13, 14] and, thus, increased risk of hip fracture [15–18]. Furthermore, fracture patients have an increased risk of future fractures. Studies have shown that within the first month following a hip fracture, the risk of a second hip fracture is increased by 11.8 (relative risk: RR), then decreases to 2.2 (RR) after 1 year [8], but remains increased for up to 15 years [8]. Similarly increased risks have been reported following all index fractures regardless of subsequent fracture site [18].
When identifying a low energy trauma fracture, doctors need information on the future risk of fractures, especially for major osteoporotic fractures, in order to guide patients properly in choosing treatment regiments. The aim of the present study is to examine patterns of subsequent fracture and mortality rates in a 10-year time span.
Subjects and methods
In Denmark, the extensive use of registers covering contacts to the health sector offers the possibility of reliable studies on the occurrence of fractures [19]. The National Hospital Discharge Register (NHDR) has a nationwide coverage of public hospitals with an almost 100 % completeness of records and a high precision of diagnoses [20, 21] including fracture diagnoses [22]. NHDR has covered both inpatient and outpatient contacts since 1995; thus, all diagnosed fractures are presumed to be captured in this register. The validity of fracture reports in NHDR compared with patient files has previously been reported at 97 % [22]. NHDR includes information on the civil registration number, date of discharge and discharge diagnoses assigned by the physician according to the Danish version of the International Classification of Diseases (ICD). Since 1993, the ICD 10th revision has been used in Denmark. Danish registers can be linked by Statistics Denmark due to the civil registration number, which is unique to each individual in Denmark and enables broader epidemiological studies.
The study was approved by the National Board of Health and the Danish Data Protection Agency. The study is reported in accordance with STROBE guidelines [23].
Study design
The study was designed as a nationwide, register-based follow-up study. Patients were included if diagnosed with an index fracture (ICD-10 codes: S22.x, S32.x, S42.x, S52.x, S62.x, S72.x, S82.x, S92.x, T02.x, T08.x, T10.x and T12.x) between January 1st, 2001 and December 31st, 2001 and if older than 50 years at time of fracture. For this study, some fracture types (such as skull, patella, foot and others) were not included. The patients were investigated for future subsequent fractures from January 1st, 2002 to December 31st, 2011. Subsequent fractures were defined as either recurrent fracture, where index and subsequent fractures were of the same type, or second fracture, where index and subsequent fractures were of different types. The number of fractures and deaths was calculated per calendar year, only allowing each patient one fracture per group per calendar year to avoid double counting. Fractures were aggregated in the following groups, of which MOF sites are the hip, forearm and vertebra:
-
Lower leg (S82.2–8)
-
Femur (non-hip) (S72.3–9)
-
Hip (S72.0–2)
-
Pelvis (S32.3–5)
-
Vertebral (S22.0–S22.1, S32.0–S32.2, S32.7, S32.8, T08.x)
-
Forearm (S52.x)
-
Humerus (S42.x)
From the Danish Civil Registration System, migrations or date of death during the study period were retrieved, and these patients were censored as these were considered lost to follow-up. To account for deaths during the study period, we used the actuarial method, assuming that the number of deaths were constant during a period of time.
Furthermore, incidence rates for all fracture groups are reported from 2001 to 2011, for individuals aged 50 years at time of fracture.
Statistics
Data from the different registers were merged at Statistics Denmark. For each subject, their unique personal civil registration number was substituted by a unique anonymous case number. Data were reported as mean ± standard deviation (SD) and percentages (%). Mortality was accounted for by use of actuarial method, and chi-square test was used to test difference in mortality between groups. All analyses were performed using Stata MP 13 (StataCorp, College Station, TX, USA) and SPSS 20.0 (SPSS Inc., Chicago IL).
Results
From 2001 to 2011, the crude number of fractures in the included groups in Denmark rose from 45,691 to 49,050. Indeed, the incidence of all but hip fractures increased during the study period, Table 1. For MOF, the annual number of hip fractures decreased (from 11,103 to 9,310), whereas wrist and vertebral fractures increased (from 9,418 to 11,383 and from 2,322 to 2,814, respectively), in the same period of time.
The average annual incidence of any fracture from January 1st, 2001 to December 31st, 2011, for individuals older than 50 years at the time of fracture, was highest for forearm and hip fractures (6.3 and 5.4 per 1,000 persons, respectively) and was lowest for pelvic and femur (non-hip) fractures (both 0.7 per 1,000 persons). Considerably, more women than men experienced a fracture, as women accounted for 71.8 % of all fractures, p < 0.001. The average age at index fracture (for all fracture groups) was 72.1 years, with the lowest average age in patients with a lower leg fracture (65.7 ± 11.6 years) and highest in patients with a hip fracture (80.3 ± 9.9 years) (Table 1).
During the 10-year follow-up period, the incidence of any recurrent fracture, i.e. where index and subsequent fractures are of the same type, was high for all groups (9–34 % for men and 12–40 % for women, see Table 2). Subsequent hip fracture, regardless of index fracture, had the highest incidence across the study period, ranging from 9 to 40 %. For both men and women, the frequency of second pelvic, lower leg, femur (non-hip) or vertebral fracture was low (<8 %) (Table 2). A total of 11 % of patient with a forearm index fracture experienced a subsequent humerus fracture and 11 % of patients with a lower leg index fracture had a hip fracture within the follow-up period. The same tendencies were present when looking at the gender-stratified subsequent fracture rates (Table 2).
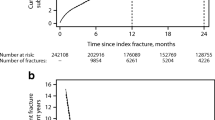
The mortality rate in the first year following a fracture was highest for femur (non-hip) fracture (26 % for men and 19 % for women, p < 0.001). Forearm fracture had the lowest 1-year mortality rate (4 % for both men and women, p value not significant). The 10-year mortality rate was highest for hip fractures (87 % for men and 85 % for women, p < 0.001) and lowest for forearm fractures in men and lower leg fractures in women (36 % for both, p value not significant). The cumulative survival rate curves in the 10-year period following any fracture type is illustrated in Fig. 1. Furthermore, the 10-year mortality rate for MOF divided into age groups (Fig. 2) showed that mortality was lower for women than men regarding all MOFs. Furthermore, hip fracture had the highest mortality of all MOFs across age groups. The 10-year mortality rates illustrated in this study following an index hip fracture for the age group 50–59 were 58 and 44 %, for men and women respectively. This is significantly higher than the equivalent 10-year mortality rate for the entire Danish population, which was 11 and 7 % for men and women, respectively [24] (p < 0.001 for both). For patients in the age group 80+ years, the 10-year mortality rate for hip fractures was 98 % for men and 95 % for women. This is significantly higher than the equivalent 10-year mortality rate for the entire Danish population in this age group for the same period, which was 86 and 80 % for men and women, respectively [24] (p < 0.001 for both). In the Supplementary material, mortality life tables are presented.
Discussion
In this nationwide cohort study, we demonstrated that patients who suffered a fracture have a high risk of subsequent fractures, especially for hip fracture. Other fractures, which are not commonly considered as osteoporotic fractures, such as lower leg, were frequently observed in the 10 years following index fractures. Appendicular fractures were often followed by a recurrent fracture, or subsequent fractures at a more proximal location in the same limb, i.e. forearm fractures were followed by humerus fractures. These results have not been previously demonstrated to this extent, and according to our knowledge, no previous studies have estimated cumulative 10-year subsequent fracture incidences for any non-hip fractures.
The 10-year mortality rates found in this study were considerably higher than the equivalent 10-year mortality rate for the entire Danish population. These findings are supported by other studies [7, 25–27]. Mortality following fracture was higher for men than women regardless of age, which underlines the need for early prevention of fractures and diagnosis of osteoporosis in men. This result is supported by previous studies on Danish fracture patients [7, 8].
Studies have shown that, amongst patients with hip fracture, 20–50 % have suffered a previous fracture [8, 28, 29]. A large proportion of patients may, potentially, be identified prior to hip fracture. Results from this study showed that patients with a fracture, regardless of type, had a high rate of subsequent forearm, humerus and hip fractures within the following 10 years, which for men were 5–15, 8–24 and 9–34 %, respectively (Table 2). The equivalent rates for women were 11–25, 9–27 and 13–40 %, respectively. Furthermore, this study showed that within 10 years, 3–47 % fracture patients will experience a MOF and that an index MOF will result in recurrent fracture for 11–40 % of patients, which is supported by a previous study [26]. Fracture prevention programmes targeting patients with any type of low energy trauma fractures could, therefore, be anticipated to prevent especially hip, humerus and forearm subsequent fractures as these are the most frequent [3, 30].
The mean age for patients at the time of index fracture in this study was 72.1 years, and the mean age at the initiation of anti-osteoporotic treatment is 73 year in Denmark; thus, many patients would be expected to receive treatment at the time of fracture, both index and subsequent fractures. Previous studies have shown that only the minority of fracture patients receive anti-osteoporotic medication [5, 6]. Approximately 85 % of hip fracture patients have previously been shown to have osteoporosis [31] and are, thus, ideal candidates for anti-osteoporotic treatment. Hence, it is important to initiate treatment if a low energy fracture has occurred, both to prevent future fractures and to decrease the high mortality due to osteoporotic fractures [32–34].
One of the strengths in this study was the study design. As data were collected from nationwide registers with a generally excellent fracture registration, selection bias seems unlikely [22]. However, there were also some limitations to this study, including the observed study population, time span and furthermore the use of registries in relation to vertebral fractures. For the observed study population, incidence rates for forearm and hip fractures varied substantially between 2001 and 2011, which is consistent with other studies [35]. Regarding hip fractures, this could be due to improved awareness on prevention, both concerning pharmaceutical treatment and lifestyle changes [36]. This study had a 10-year perspective, from which fracture risks were estimated. This was chosen in order to produce results comparable to those of fracture risk assessment tools and fracture prevention programmes. However, this length of time may not capture the true risk between index and subsequent fractures, as some subsequent fractures may occur more than 10 years after the index fracture. In this study, distal fractures (e.g. lower leg) occurred earlier in life (mean age around 66 years) and proximal fractures (e.g. hip) occurred on average more than 10 years later (mean age around 80 years). Use of registries for diagnosis have previously shown a high accuracy in fracture diagnosis [22]; however, other studies find that only a minority of vertebral fractures are diagnosed and registered [31, 37]. Registries may, therefore, may be insufficient for identification of the true vertebral fracture incidence rate and these rates may, thus, not be comparable to other fracture incidence rates. In this study, low and high energy fractures have not been differentiated. It would be expected that the number of subsequent fractures would be substantially higher following low energy fracture compared to high energy fractures. However, due to the study design, it was not possible to distinguish between these.
In conclusion, patients suffering a fracture (and especially a hip fracture) have a high incidence of a subsequent fracture. Fractures after the age of 50 may be considered an early warning of increased risk for future fractures in many patients, and this actualizes the discussion for implementing fracture risk assessment tools and fracture prevention programmes.
References
Melton LJ III (1995) Epidemiology of fractures. In: Riggs B, Melton LJ III (eds) Osteoporosis: etiology, diagnosis, and management, Second edn. Lippincott-Raven, Philadelphia, pp 225–247
Kanis JA, Johnell O, Oden A et al (2002) Ten-year risk of osteoporotic fracture and the effect of risk factors on screening strategies. Bone 30:251–258
Warriner AH, Patkar NM, Curtis JR et al (2011) Which fractures are most attributable to osteoporosis? J Clin Epidemiol 64:46–53
Marshall DA, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254
Hansen L, Mathiesen AS, Vestergaard P et al (2013) A health economic analysis of osteoporotic fractures: who carries the burden? Arch Osteoporos 8:126
Abrahamsen B, Eiken P, Eastell R (2009) Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res 24:1095–1102
Vestergaard P, Rejnmark L, Mosekilde L (2007) Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int 18:1583–1593
Ryg J, Rejnmark L, Overgaard S et al (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977–2001. J Bone Miner Res 24:1299–1307
Borgström F, Zethraeus N, Johnell O et al (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650. doi:10.1007/s00198-005-0015-8
World Health Organization Collaborating Centre for Metabolic Bone Diseases (2013) FRAX ® WHO fracture risk assessment tool. http://www.shef.ac.uk/FRAX/index.aspx. Accessed 14 Aug 2013
Garvan Institute (2013) Fracture risk calculator. http://www.garvan.org.au/bone-fracture-risk/. Accessed 22 Aug 2013
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Brixen K, Overgaard S, Gram J et al (2012) Systematisk forebyggelse og behandling af knogleskørhed hos patienter med hoftebrud – en medicinsk teknologi vurdering
Chari S, McRae P, Varghese P et al (2013) Predictors of fracture from falls reported in hospital and residential care facilities: a cross-sectional study. BMJ 3:1–7
Bischoff-Ferrari HA (2011) The role of falls in fracture prediction. Curr Osteoporos Rep 9:116–121
Johansson C, Mellstrom D (1996) An earlier fracture as a risk factor for new fracture and its association with smoking and menopausal age in women. Maturitas 24:97–106
Gunnes M, Mellstrom D, Johnell O (1998) How well can a previous fracture indicate a new fracture? A questionnaire study of 29,802 postmenopausal women. Acta Orthop Scand 69:508–512
Klotzbuecher CM, Ross PD, Landsman PB et al (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Frank L (2000) When an entire country is a cohort. Science 287(80-):2398–2399
Andersen T, Madsen M, Jørgensen J et al (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull J Health Sci 46:263–268
Mosbech J, Jørgensen J, Madsen M et al (1995) The national patient registry. Evaluation of data quality. Ugeskr Laeger 157:3741–3745
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16, 416 patients in Denmark. Am J Epidemiol 156:8–10
Von Elm E, Altman DG, Egger M et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
Statistics Denmark (2013) StatBank Denmark. Population and elections
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39:203–209
Hodsman AB, Leslie WD, Tsang JF, Gamble GD (2008) 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort. Arch Intern Med 168:2261–2267
Omsland TK, Emaus N, Tell GS et al (2013) Ten-year risk of second hip fracture. A NOREPOS study. Bone 52:493–497
Port L, Center J, Briffa NK et al (2003) Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int 14:780–784
Edwards B, Bunta A, Simonelli C et al (2007) Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res 461:226–230
Eisman JA, Bogoch ER, Dell R et al (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046
Ryg J (2009) Ph.d. Thesis: osteoporose og hoftebrud – en klinisk, økonomisk og epidemiologisk undersøgelse
Harris ST, Watts NB, Genant HK et al (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. J Am Med Assoc 282:1344–1352
Chesnut CH III, Skag A, Christiansen C et al (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Reginster JY, Seeman E, De Vernejoul MC et al (2005) Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab 90:2816–2822
Amin S, Achenbach SJ, Atkinson EJ et al (2014) Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res 29:581–589. doi:10.1002/jbmr.2072
Abrahamsen B, Vestergaard P (2010) Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int 21:373–380
Ankjaer-Jensen A, Johnell O (1996) Prevention of osteoporosis: cost-effectiveness of different pharmaceutical treatments. Osteoporos Int 6:265–275
Funding
This study was supported by a grant from the Danish Bone Society.
Conflicts of interest
LH has received research grants from MSD Danmark ApS and honoraria from Eli Lilly and MSD Danmark.
KDP and SAE have no conflicts of interest.
BLL has received research grants from Eli Lilly and Axellus; served on advisory boards for Eli Lilly, Merck, Sharp & Dohme and Amgen and received honoraria from Eli Lilly, Merck, Sharp & Dohme and Amgen.
PE is an advisory board member of Eli Lilly, MSD and Amgen and has received lecture fees from Eli Lilly, Amgen and GlaxoSmithKline.
KB reports serving on the board for Osteologix, Servier, Amgen and Novartis; receiving payment for expert testimony on a patent for strontium maleate in the USA; consulting fees from Osteologix; lecture fees from Servier, Amgen, GlaxoSmithKline and Novartis and payment for travel accommodation from Amgen, Eli Lilly, Servier and Novartis.
KB further reports receiving grant support to his institution, Odense University Hospital, from Merck, Sharp & Dohme and Novartis and investigator payments from Merck, Sharp & Dohme, Osteologix, Servier, Amgen, Natural Product Sciences Pharmaceuticals and Eli Lilly.
BA received grants from or conducted trials for Novartis, Nycomed/Takeda and Amgen and served as an advisory board member for Nycomed/Takeda, Merck and Amgen.
JEBJ received honoraria from and is an advisory board member for Eli Lilly, Merck, Sharp & Dohme and Amgen.
TH received speaker’s honorarium from Amgen.
PV received unrestricted research grants from Servier and MSD and travel grants from Amgen, MSD, Eli Lilly, Novartis and Servier.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material - Tables A-H
(DOCX 45 kb)
Rights and permissions
About this article
Cite this article
Hansen, L., Petersen, K.D., Eriksen, S.A. et al. Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int 26, 513–519 (2015). https://doi.org/10.1007/s00198-014-2875-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2875-2