Abstract
Summary
Failure to account for competing mortality gave higher estimates of 10-year fracture probability than if appropriate adjustment is made for competing mortality, particularly among subgroups with higher mortality. A modified Kaplan–Meier method is easy to implement and provides an alternative approach to existing methods for competing mortality risk adjustment.
Introduction
A unique feature of FRAX® is that 10-year fracture probability accounts for mortality as a competing risk. We compared the effect of competing mortality adjustment on nonparametric and parametric methods of fracture probability estimation.
Methods
The Manitoba Bone Mineral Density (BMD) database was used to identify men and women age ≥50 years with FRAX probabilities calculated using femoral neck BMD (N = 39,063). Fractures were assessed from administrative data (N = 2,543 with a major osteoporotic fracture, N = 549 with a hip fracture during mean 5.3 years follow-up).
Results
The following subgroups with higher mortality were identified: men, age >80 years, high fracture probability, and presence of diabetes. Failure to account for competing mortality in these subgroups overestimated fracture probability by 16–56 % with the standard nonparametric (Kaplan–Meier) method and 15–29 % with the standard parametric (Cox) model. When the outcome was hip fractures, failure to account for competing mortality overestimated hip fracture probability by 18–36 % and 17–35 %, respectively. A simple modified Kaplan–Meier method showed very close agreement with methods that adjusted for competing mortality (within 2 %).
Conclusions
Failure to account for competing mortality risk gives considerably higher estimates of 10-year fracture probability than if adjustment is made for this competing risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of clinical risk factors has been shown to enhance the performance of bone mineral density (BMD) in the prediction of hip and major osteoporotic fractures [1]. Important clinical risk factors include age, sex, body mass index, prior fragility fracture, prolonged use of glucocorticoids, rheumatoid arthritis, parental history of hip fracture, current smoking, high alcohol intake, secondary osteoporosis, and (optionally) femoral neck BMD [2]. These elements are integrated in the WHO fracture risk assessment tool (FRAX®) for estimation of individual 10-year major osteoporotic and hip fracture probabilities [2].
Survival methods are widely used to study time-to-event (such as fracture). The standard Kaplan–Meier (product limit) and Cox proportional hazard models are nonparametric and parametric survival methods, respectively, that consider only two endpoints: the outcome of interest (event) and loss to follow-up (censoring). For example, in order to estimate the risk of hip fracture among osteoporotic patients, subjects are followed from a baseline date (such as date of diagnosis) until the date of hip fracture, death, or study closing date. A patient who is alive and fracture-free at final follow-up is considered to be censored. These various states are shown schematically in Fig. 1. The importance of competing endpoints is increasingly recognized when estimating cause-specific incidences [3–8]. A patient who dies without hip fracture during the study period is considered to have a “competing event” at their date of death. Treating the competing event as “censored” at the time of occurrence is inappropriate because after a competing event has occurred, fracture is no longer possible. A unique feature of FRAX, which distinguishes it from other absolute fracture risk assessment systems [9–12], is that fracture probability estimates account for the risk of death (“competing mortality”) [13, 14].
Commonly employed methods for computing incidence adjusted for competing risk of mortality typically involve two steps [15, 16]. In step 1, the overall survival probability of being “event-free” is determined, where all events—the event of interest or the competing risk event(s)—are considered (e.g., death or fracture). In step 2, cause-specific cumulative incidence functions (e.g., fracture) are constructed by cumulatively summing the event-specific incidence for each time interval multiplied by the survival probability up to the start of that time interval (e.g., the joint probability of experiencing a fracture in this time interval given that the individual survived fracture-free through all prior intervals). The cumulative incidence functions correctly partition the probability of any event into the probability corresponding to each competing event. That is, at any point in time, the cumulative overall event probability is equal to the sum of the cumulative incidence functions for each individual type of event.
If competing mortality is not appropriately considered, this can result in biased estimates of fracture probability [15]. Since many of the risk factors for fracture are also risk factors for death (e.g., older age, prior fracture, and medical comorbidities) [2], failure to consider competing mortality may result in an overestimate of fracture probability. The Kaplan–Meier method is implemented in many statistical software packages and provides the basis for simple comparisons of the survival curves using the log rank test but does not consider competing endpoints. In contrast, only a few statistical software packages have specific function for survival analysis that considers competing outcomes (e.g., stccreg in STATA, StataCorp LP, College Station, TX; R, Comprehensive R Archive Network, TU Wien, Austria [16]).
We describe a simple nonparametric approach to estimate cumulative fracture incidence that incorporates competing mortality using a modified Kaplan–Meier method. We compare this approach with nonparametric and parametric methods that do and do not account for competing mortality risk [15]. Results are compared for population strata where competing mortality is expected to exert the greatest effect: men, elderly individuals (age 80 years and older), those with high major osteoporotic fracture probability (>20 %), and one selected comorbidity (diabetes).
Methods
Subjects and setting
In the Province of Manitoba, Canada, health services are provided to virtually all residents through a single public health care system. Bone density testing with dual-energy X-ray absorptiometry (DXA) has been managed as an integrated program since 1997; criteria and testing rates for this program have been published [17]. The program maintains a database of all DXA results which can be linked with other population-based computerized health databases through an anonymous personal identifier. The DXA database has been previously described with completeness and accuracy in excess of 99 % [18].
For this retrospective study, we identified all individuals age 50 years and older with valid FRAX probability estimates calculated using femoral neck BMD. Subjects were required to have medical coverage from Manitoba Health during the observation period ending on March 31 2008. For those with more than one eligible set of measurements, only the first record was included. The study was approved by the Research Ethics Board for the University of Manitoba and access to the data was granted by the Health Information Privacy Committee of Manitoba.
Bone density measurements
DXA scans were performed and analyzed in accordance with the manufacturer’s recommendations. Femoral neck hip T-scores (number of SDs above or below young adult mean BMD) were calculated from the Third National Health and Nutrition Examination Survey White female reference values (Prodigy version 8.8) [19, 20]. Prior to 2000, DXA measurements were performed with a pencil-beam instrument (Lunar DPX, GE Lunar, Madison WI) and after this date a fan-beam instrument was used (Lunar Prodigy, GE Lunar, Madison WI). Instruments were cross-calibrated using anthropomorphic phantoms, and 59 volunteers and no clinically significant differences were identified. Densitometers showed stable long-term performance (coefficient of variation (CV) < 0.5 %) and satisfactory in vivo precision (CV 1.7 % for L1-4 and 1.1 % for the total hip) [21]. Weight and height were recorded at the time of the DXA examination (prior to 2000 this was by self-report and starting in 2000 height was assessed with a wall-mounted stadiometer and weight was assessed without shoes using a standard floor scale). BMI (in kilograms per square meter) was calculated as weight (in kilograms) divided by height squared (in meters).
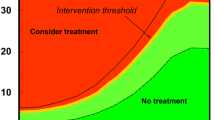
Fracture probability calculations
Clinical risk factors (or proxies) required for calculating fracture probability with FRAX were assessed through a combination of hospital discharge abstracts (diagnoses and procedures coded using the ICD-9-CM prior to 2004 and ICD-10-CA thereafter) and physician billing claims (coded using ICD-9-CM) with adjustment for the effect of missing parental hip fracture information as previously described [22]. Ten-year probability of a major osteoporotic fracture or hip fracture using BMD was calculated for each subject by the WHO Collaborating Center based on the Canadian FRAX tool (version 3.1). Discrimination and calibration of the Canadian FRAX tool used in this analysis have been previously validated in large Canadian cohorts [23, 24]. Major osteoporotic fracture probability was categorized as low (<10 %), moderate (10–19 %), and high (>20 %) in accordance with published Canadian guidelines [25].
Incident fractures
Manitoba Health physician claims and hospital databases record all health care utilization in the province. Each subject’s longitudinal health record was assessed from the date of bone density measurement to March 31 2008 for the presence of hip, clinically diagnosed spine, forearm, or proximal humerus fracture codes that were not associated with codes indicating high trauma. The accuracy of these data and fracture codes has been established for a number of clinical disorders, including osteoporotic fractures [26, 27].
Analysis
Estimates of 10-year fracture probability for major osteoporotic fractures and hip fractures were initially obtained without considering competing mortality using nonparametric (Kaplan–Meier) and parametric (Cox proportional hazards) methods. The fracture probability estimates were recalculated using nonparametric and parametric methods that considered competing mortality. The nonparametric method was implemented using the two-step procedure [15, 16]. In step 1, the overall survival probability of being alive without fracture was determined. In step 2, the fracture-specific cumulative incidence function was constructed by cumulatively summing the fracture incidence for each time interval multiplied by the survival probability at the start of that time interval from step 1. The overall survival function considered migration (i.e., moving out of province) as a censoring event. The cumulative incidence function for fracture was then constructed by cumulatively summing the fracture-specific incidence for each time interval multiplied by the survival probability up to the start of that time interval. The parametric method was implemented according to the methodology described by Allison using SAS software [28, 29]. A modified Kaplan–Meier method was also implemented. In the modified Kaplan–Meier method, individuals who died before a defining fracture endpoint were not censored at the time of death. Instead, these individuals were assigned a final follow-up date of March 31, 2008 (i.e., the end of the observation period) and assumed to remain fracture-free up to and including that date (dotted line for “Death without fracture” in Fig. 1). Censoring of observations only occurred when individuals were lost to follow-up from migration. The proportional hazards assumption was evaluated and confirmed to apply using graphical methods (i.e., plot of log(time) versus log (−log(survival))).
Results
Baseline characteristics of the population are summarized in Table 1. As expected, the vast majority (92.7 %) of the individuals referred for BMD testing were women, tended to be in younger age groups, were nondiabetic, and had major osteoporotic fracture probability in the low-risk range. Despite this, there were sufficient numbers of men, older individuals (age 80 years and above), individuals with high risk fracture probability, and diabetics for robust analysis.
During the mean 5.3 years of observation, almost 90 % of the cohort was still alive and living within the province. A relatively small number (8.0 %) died before March 31, 2008 and an even smaller number (3.0 %) had left the province. A total of 2,543 (6.4 %) sustained one or more major osteoporotic fractures including 549 (1.4 %) with a hip fracture. Table 2 confirms that there was significantly higher mortality in the subgroups of particular interest: men, individuals age 80 years and older, high major osteoporotic fracture probability, and diagnosed diabetes.
Estimated major osteoporotic fracture probabilities at 10 years are summarized in Table 3. Without adjusting for competing mortality, estimates from the nonparametric (Kaplan–Meier) and parametric (Cox proportional hazards model) methods were generally very close (maximum difference 9 % for men, all others within 5 %). When competing mortality risk was considered, nonparametric and parametric methods again showed good agreement (maximum difference 14 % for men, all others within 4 %). Estimation of fracture probability that did not include competing mortality gave consistently higher results than when competing mortality risk was considered in the estimation process. The magnitude of the effect of adjusting for competing mortality risk was greater for men (versus women), diabetics (versus nondiabetics), high FRAX probability (versus low and moderate risk), and individuals aged 80 years and older (versus younger groups). A Ten-year major osteoporotic fracture probability was greater for men than women when estimated without competing mortality (Kaplan–Meier 0.146 versus 0.125; Cox model 0.134 versus 0.124). When estimated with competing mortality, this was reversed with lower 10-year fracture probability in men than women (Kaplan–Meier 0.094 versus 0.117; Cox model 0.109 versus 0.117). In the subgroups where competing mortality was expected to exert the greatest effect (men, diabetics, high FRAX probability, and age 80 years and older), failure to account for competing mortality overestimated fracture risk by 16 to 56 % with the Kaplan–Meier model and 15 to 29 % by the Cox model. Generally similar findings were seen when analysis was limited to hip fractures (Table 4). Failure to account for competing mortality overestimated hip fracture probability in the high mortality groups by 18 to 36 % using the Kaplan–Meier model and by 17 to 35 % in the Cox model.
The modified Kaplan–Meier approach for estimation of 10-year major fracture probability (Table 3) and hip fracture probability (Table 4) showed very close agreement with the parametric and nonparametric models that accounted for competing mortality. The difference was within 2 % in all subgroups. Figure 2 compares the nonparametric cumulative incidence of major osteoporotic fractures in the four high mortality groups. Results from the cumulative incidence function and modified Kaplan–Meier methods, both of which adjusted for competing mortality, were virtually indistinguishable whereas failure to account for competing mortality gave consistently higher fracture predictions.
Cumulative major osteoporotic fracture incidence to 10 years estimated with three different nonparametric methods: standard Kaplan–Meier (which does not consider competing mortality), cumulative incidence function (with two-step competing mortality adjustment), modified Kaplan–Meier (with competing mortality adjustment). These last two curves show substantial overlap
Discussion
This analysis shows the large effect of competing mortality on estimation of fracture probability, particularly among individuals where mortality rates are elevated. As hypothesized, failure to account for competing mortality significantly overestimated major osteoporotic and hip fracture probability in all groups but most particularly among men, individuals age 80 years and older, those with major osteoporotic FRAX probability >20 %, and diagnosed diabetics. We also found that a modified Kaplan–Meier approach could be used to accurately account for competing mortality as a relatively simple procedure that allowed for estimation of fracture-free survival.
Although the parametric model that accounts for competing mortality risk will give unbiased estimates, assuming that model assumptions are satisfied and the data do not contain measurement error, there are advantages to the modified nonparametric approach that we propose. Specifically, implementation of the parametric models requires programming skills in statistical software that may not be straightforward for clinicians. The modified Kaplan–Meier method can use functions for survival analysis readily available in most statistical software packages since the adjusted cumulative incidence function is simply the complement of the survival curve (i.e., one minus survival). Therefore, statistical tests for comparison of fracture-free survival curves adjusted for competing mortality can use standard functions available within the software package (e.g., log rank test). In addition, estimation of error (variance) in the probability estimates is immediately available from the statistical software, whereas this could be a nontrivial issue, depending on the software adopted, for the parametric model. We found that fracture probability estimates for the modified Kaplan–Meier approach showed close agreement with the nonparametric model that accounted for competing risk (within 2 %).
However, the limitations of the study should be noted. The comparison of the procedures was limited to a single numeric example; our conclusions about performance of the modified Kaplan–Meier approach may not generalize to other datasets. Given the low rate of censoring for non-death reasons (migration out of province), it would be interesting to see whether the same findings are observed where there are much higher rates of loss to follow-up. As well, both the parametric and nonparametric models were simple models; only a single categorical covariate was included in each model for the comparisons that were undertaken. This was done to highlight the independent effect of individual variables. However, the modified Kaplan–Meier method cannot be applied in instances where the researcher is interested in simultaneously investigating the effect of multiple continuous covariates on the estimates of fracture probability. Limitations to our modified Kaplan–Meier approach to account for competing mortality are acknowledged. It would therefore be important to compare these approaches in other datasets and clinical contexts before the modified Kaplan–Meier approach is assumed to give equivalent results to more conventional approaches for competing mortality risk adjustment.
In conclusion, we have shown that failure to account for competing mortality gives considerably higher estimates of 10-year fracture probability than if adjustment is made for competing mortality. This effect is most clearly evident among subgroups with higher mortality. A modified Kaplan–Meier approach, relatively easy for clinicians to implement, provides an alternative approach to existing parametric and nonparametric methods for competing mortality risk adjustment.
References
Kanis JA, Oden A, Johnell O et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Kanis JA, Oden A, Johansson H et al (2009) FRAX and its applications to clinical practice. Bone 44:734–743
Aus G, Pileblad E, Hugosson J (1995) Impact of competing mortality on the cancer-related mortality in localized prostate cancer. Urology 46:672–675
Goldie SJ, O’Shea M, Campos NG et al (2008) Health and economic outcomes of HPV 16,18 vaccination in 72 GAVI-eligible countries. Vaccine 26:4080–4093
Kim WR, Poterucha JJ, Benson JT et al (2004) The impact of competing risks on the observed rate of chronic hepatitis C progression. Gastroenterology 127:749–755
Mell LK, Jeong JH, Nichols MA et al (2010) Predictors of competing mortality in early breast cancer. Cancer 116:5365–5373
Mell LK, Dignam JJ, Salama JK et al (2010) Predictors of competing mortality in advanced head and neck cancer. J Clin Oncol 28:15–20
Simard EP, Pfeiffer RM, Engels EA (2011) Cumulative incidence of cancer among individuals with acquired immunodeficiency syndrome in the United States. Cancer 117:1089–1096
Nguyen ND, Frost SA, Center JR et al (2007) Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int 18:1109–1117
Nguyen ND, Frost SA, Center JR et al (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1444
Henry MJ, Pasco JA, Sanders KM et al (2006) Fracture risk (FRISK) score: Geelong osteoporosis study. Radiology 241:190–196
Pluijm SM, Koes B, de Laet C et al (2009) A simple risk score for the assessment of absolute fracture risk in general practice based on two longitudinal studies. J Bone Miner Res 24:768–774
Bolland MJ, Siu AT, Mason BH et al (2011) Evaluation of the FRAX and Garvan fracture risk calculators in older women. J Bone Miner Res 26:420–427
Henry MJ, Pasco JA, Merriman EN et al (2011) Fracture risk score and absolute risk of fracture. Radiology 259:495–501
Satagopan JM, Ben-Porat L, Berwick M et al (2004) A note on competing risks in survival data analysis. Br J Cancer 91:1229–1235
Scrucca L, Santucci A, Aversa F (2007) Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transpl 40:381–387
Leslie WD, MacWilliam L, Lix L et al (2005) A population-based study of osteoporosis testing and treatment following introduction of a new bone densitometry service. Osteoporos Int 16:773–782
Leslie WD, Caetano PA, MacWilliam LR et al (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8:25–30
Binkley N, Kiebzak GM, Lewiecki EM et al (2005) Recalculation of the NHANES database SD improves T-score agreement and reduces osteoporosis prevalence. J Bone Miner Res 20:195–201
Kanis JA, McCloskey EV, Johansson H et al (2008) A reference standard for the description of osteoporosis. Bone 42:467–475
Leslie WD (2006) The importance of spectrum bias on bone density monitoring in clinical practice. Bone 39:361–368
Leslie WD, Lix LM, Johansson H et al (2010) Independent clinical validation of a Canadian FRAX® tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358
Leslie WD, Berger C, Langsetmo L et al (2010) Construction and validation of a simplified fracture risk assessment tool for Canadian women and men: results from the CaMos and Manitoba cohorts. Osteoporos Int 22(6):1873–1883
Fraser LA, Langsetmo L, Berger C et al (2011) Fracture prediction and calibration of a Canadian FRAX® tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837
Papaioannou A, Morin S, Cheung AM et al (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 182:1864–1873
Leslie WD, Tsang JF, Caetano PA et al (2007) Effectiveness of bone density measurement for predicting osteoporotic fractures in clinical practice. J Clin Endocrinol Metab 92:77–81
Roos LL, Sharp SM, Wajda A (1989) Assessing data quality: a computerized approach. Soc Sci Med 28:175–182
Allison P (2005) Survival analysis using the SAS® system: a practical guide. SAS Institute Inc
Klein JP, Gerster M, Andersen PK et al (2008) SAS and R functions to compute pseudo-values for censored data regression. Comput Methods Programs Biomed 89:289–300
Acknowledgments
The authors are indebted to Manitoba Health for the provision of data (HIPC file no. 2007/2008-49). The results and conclusions are those of the authors, and no official endorsement by Manitoba Health is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee. We would like to thank Ms. Helena Johansson and Dr. John Kanis for generating the FRAX results for the Manitoba cohort. LML is supported by a Centennial Research Chair at the University of Saskatchewan.
Conflicts of interest
William D. Leslie received speaker fees and unrestricted research grants from Merck Frosst Canada Ltd; unrestricted research grants from Sanofi-Aventis, Procter & Gamble Pharmaceuticals, Novartis, Amgen Pharmaceuticals, Genzyme; and advisory boards for Genzyme, Novartis, and Amgen Pharmaceuticals. Lisa M. Lix received unrestricted research grants from Amgen Pharmaceuticals.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Leslie, W.D., Lix, L.M., Wu, X. et al. Competing mortality and fracture risk assessment. Osteoporos Int 24, 681–688 (2013). https://doi.org/10.1007/s00198-012-2051-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2051-5