Abstract
Summary
The risk of major osteoporotic fracture (MOF) after a first MOF is increased over the whole duration of follow-up, but the imminent risk is even higher. If the acute increment in risk in the few years following MOF is amenable to therapeutic intervention, then immediate short-term treatments may provide worthwhile clinical dividends in a very cost-effective manner.
Introduction
A history of fracture is a strong risk factor for future fractures. The aim of the present study was to determine whether the predictive value of a past MOF for future MOF changed with time.
Methods
The study was based on a population-based cohort of 18,872 men and women born between 1907 and 1935. Fractures were documented over 510,265 person-years. An extension of Poisson regression was used to investigate the relationship between the first MOF and the second. All associations were adjusted for age and time since baseline.
Results
Five thousand thirty-nine individuals sustained one or more MOFs, of whom 1919 experienced a second MOF. The risk of a second MOF after a first increased by 4% for each year of age (95% CI 1.02–1.06) and was 41% higher for women than men (95% CI 1.25–1.59). The risk of a second MOF was highest immediately after the first fracture and thereafter decreased with time though remained higher than the population risk throughout follow-up. For example, 1 year after the first MOF, the risk of a second fracture was 2.7 (2.4–3.0) fold higher than the population risk. After 10 years, this risk ratio was 1.4 (1.2–1.6). The effect was more marked with increasing age.
Conclusions
The risk of MOF after a first MOF is increased over the whole follow-up, but the imminent risk is even higher. If the acute increment in risk in the few years following MOF is amenable to therapeutic intervention, then immediate short-term treatments may provide worthwhile clinical dividends in a very cost-effective manner, particularly in the elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well established that fragility fractures increase the risk of a further fracture [1–4]. In a meta-analysis performed by Klotzbuecher et al. [5], the relative risk of having a hip fracture or a vertebral fracture was approximately twofold higher for most types of prior fracture. For a prior vertebral fracture, however, the risk of a further vertebral fracture was increased more than fourfold. Most studies suffer from heterogeneous and incomplete retrieval of fracture outcomes, a relatively short follow-up and scant information on men so that risk estimates lack accuracy.
Additionally, and importantly, the increase in relative risk may not be constant with time or age. For example, a large meta-analysis showed that a prior fracture history was a significant risk factor for hip fracture at all ages but was highest at younger ages and decreased progressively with age [3]. Several studies have examined the time course of second fractures by site following an index fracture [1, 6–11]. Fracture at the hip, forearm, spine or humerus (collectively termed major osteoporotic fractures) have been less frequently studied but (apart from rib fractures) comprise approximately 90% of the morbidity due to fracture [12, 13]. In a small study of patients in Malmo over 5 years, prior fractures of the proximal humerus, spine or hip were associated with higher subsequent fracture risks at the hip, forearm, spine or humerus that were most marked in the year following the index fracture [1]. A large study from Manitoba showed a similar phenomenon when these fracture sites were combined [6]. There are no studies that have examined the age-dependency of the immediate increase in fracture risk.
The time since prior fracture and age-dependency have clinical implications. An acute increase in risk following an index fracture argues that treatment should be optimally targeted as soon as possible after a fragility fracture. Age-dependency may help target such strategies to the more vulnerable sections of the community at high risk. The aim of the present study was to determine the pattern of risk of major osteoporotic fractures (MOF) in the years following a MOF. The patterns of interest included the time course of risk, effects of gender and dependency on age.
Methods
The study cohort consists of 30,795 men and women, comprising all residents in the greater Reykjavik area on 1 December 1967 who were born between 1907 and 1935 (both years included); this sample represented 55% percent of the total Icelandic population in this age range [14, 15]. Participants were selected at random from the Icelandic National Register. The current study was based on 18,872 participants who enrolled during the recruitment period in 1967–1991, with 9116 men and 9756 women, resulting in a 71.8% recruitment rate. Individuals were followed up for a median time of 28 years until death, emigration or December 31, 2012, a total of 510,265 person-years.
The study was approved by the National Bioethics Committee and the Data Protection Authority in Iceland. All participants gave informed written consent.
Assessment of fractures
The Reykjavik Study fracture registration collected all fractures of the participants from entry into the study up to December 31, 2008 [14–16]. All residents of Iceland have a unique personal identification number allocated at birth or when taking up residence in the country, which facilitates identity and examination of hospital records. Fractures treated on an outpatient basis in Reykjavik were always referred to the only outpatient trauma clinic at the Landspitalinn University Hospital. Both inpatient and outpatient reports, from all hospitals in Reykjavik, including different departments, e.g. the trauma, radiography and outpatient departments, were manually examined and verified for fractures until 1983. Beginning in 1983, hospitals and the private radiology clinics used by the general practitioners in the Reykjavik area introduced a computerized registration system, including fracture diagnostic codes. All medical records for the participants, including referral letters if needed, were manually examined and verified. The medical records from the main hospitals outside Reykjavik (Akureyri and Akranes) were searched in the same way. The same two orthopaedic surgeons were consulted if any doubt arose about the fracture diagnosis. All fractures were registered according to the International Classification of Diseases (ICD version 10 or ICD version 9). Avulsions less than 5 × 6 mm were excluded. The Reykjavik Study fracture registration has been shown to have a capture rate of about 97% for hip, forearm and clinical vertebral fractures [16]. The circumstances of the trauma leading to the fracture were assessed as well as the date of the fracture. However, all fractures were counted regardless of trauma. If reports for a participant contained records of two identical fractures on the same day, only the first fracture was included, and 30 days had to pass between fractures at the same site for the second event to be included in the calculation as a separate fracture.
Cases with major osteoporotic fractures comprised vertebral fracture (ICD 10 codes S12.0-S12.2, S12.7, S22.0-22.1, S32.0), humeral fractures (S42.2-42.3), distal forearm fracture (S52.5-52.6) and hip fracture (S72.0-S72.2) which were identified throughout the follow-up. Any participant who experienced one or more incident MOFs was eligible for inclusion in the analysis of a second MOF.
In order to eliminate any risk of double counting, we reanalysed the data where the second MOF was excluded if it occurred at the same site as the first fracture. For example, if the index fracture was a forearm fracture, only fractures at the hip, spine and humerus were counted as a second MOF.
Statistical methods
We calculated the incidence of the first major osteoporotic fracture, in order to compare this with the incidence of the second fracture. A modification of the Poisson regression model was used to study the relationship between sex, age and the time since previous fracture on the one hand and on the other hand the risk of the first fracture (n = 18,872) and the second (n = 5039) [17]. Note that the model determines the hazard function for fracture and not fracture probability. Follow-up was measured in person-years, and the observation period of each participant was divided in intervals of 1 month. In the case of recurrent fractures, the first recurrent MOF was counted. The hazard function was assumed to be exp(β 0 + β 1 · sex + β2 · current time from fracture + β3 · current age). The beta coefficients reflect the importance of the variables, and β x = 0 denotes that the corresponding variable does not contribute to fracture risk. All associations were thus adjusted for age and time since baseline. The fracture risk with the time after previous fracture was investigated both with linear, with piecewise linear and with spline functions. Time since previous fracture was investigated as a continuous variable and examples given at specific times. When analysing time to fracture (second or first), only the first fracture after baseline was counted. The association between risk of a second fracture and the time since first fracture, spline functions were fitted using knots at 0.5, 2.5 and 15 years after the first fracture. The splines were second-order functions between the breakpoints and linear functions at the tails resulting in a smooth curve. The final model assessed the dependence of the spline functions with age and sex to determine if the time to subsequent fracture was affected in the presence of these variables.
Results
During follow-up, a total of 6895 major osteoporotic fractures occurred, comprising 1365 single or multiple clinical vertebral fractures, 2074 hip fractures, 2364 forearm fractures and 1092 humeral fractures. These fractures occurred in 5039 individuals (Table 1). For MOF, the risk of a first fracture was two- to threefold higher for women than for men and the fracture risk increased progressively with age in both men and women (Table 2).
Of the 5039 men and women sustaining at least one incident MOF, 1919 individuals went on to sustain a second fracture (Table 1). Women were more likely to sustain first and subsequent fractures. During follow-up, the number of individuals who sustained two or more clinical vertebral fractures was 289. For hip, distal forearm and humerus, the numbers were 352, 489 and 138, respectively. The pattern of major fractures was very similar to the pattern for the first MOF. For example, clinical vertebral fractures accounted for 19% of fracture cases in the case of first MOF and 21% in the case of second fracture (Table 1).
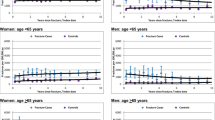
The risk of a second MOF after a first increased by 5% for each year of age (95% CI 2–7%) and was 25% more likely for women than men (95% CI 9–44%). The incidence of a second MOF was highest immediately after the first fracture and decreased with time though remained higher than the population risk throughout follow-up (Fig. 1). For example, 1 year after the first MOF, the risk of a second fracture was 2.7 (2.4–3.0) fold higher than the population risk. After 10 years, the risk ratio was 1.4 (1.2–1.6) and remained above unity for the subsequent 15 years. In individuals with an incident fracture that was examined over a 10-year time horizon, 20% of 1311 cases re-fractured within 1 year and 34% within 2 years.
Risk per 100,000 (95% CI) of a second MOF after a first MOF for a woman at the age of 75 years at her first fracture. Knots for the spline function are set at 0.5, 2.5 and 15 years of follow-up after the first fracture. The dashed line is the risk of first MOF in whole population (n = 18,872) for a woman 75 years at baseline
When the second MOF fracture was not allowed to be at the same site as the first MOF, the imminent risk was still higher than after 5–10 years, although as expected, the magnitude of the effect was less. Extending the 30-day window (during which second fractures were excluded) up to 2 years had little effect on the pattern with time (data not shown).
There were statistically significant interactions between age and the spline functions for time since first fracture (p < 0.004), i.e. the pattern of a second MOF with time from first fracture was age-dependent. The immediate incremental risk appeared remarkably similar across all age groups, but the incremental risk remained elevated over time for those with baseline age 60 years whereas it declined sharply with increasing follow-up time for those with baseline age 80 or 90 years (Fig. 2).
The effect of age on the risk of subsequent major osteoporotic fracture at 6, 24 and 60 months following a first major osteoporotic fracture. The hazard ratio (HR with 95% confidence intervals) compares the risk against that of the general population when allowing the population to age with time (e.g. the 80-year-old individual after 60 months is compared with the population age 85 years)
The time-dependent shape of the curve was similar when only counting second fractures if they occurred at a separate skeletal site than the first fracture. The interaction, however, fell short of statistical significance (p = 0.11), likely related to the lower number of fractures in the secondary analysis (1381 vs 1919) and the associated loss of power.
There were no statistically significant interactions between sex and the spline functions for time since first MOF (p > 0.30), i.e. the pattern of a second MOF with time was the same in men as in women.
Discussion
The present study confirms many observations, summarized in meta-analyses, that the risk of fracture is approximately doubled after a first fracture [3, 5]. For all prior fractures combined, the relative risk of any subsequent fracture was 2.2 (95% CI 1.9–2.6) in the meta-analysis of Klotzbeucher [5]. This estimate is very consistent with the long-term observations in the present study.
The principal aim of the present study was to document the change in risk after MOF with time. Our findings suggest that the risk is initially high and declines thereafter, though not to the levels of the general population with a follow-up of up to 25 years. The same relative risks were found in men and women, though the absolute risk was higher in women. This transient phenomenon will be missed in long-term follow-up studies where the pattern of risk with time is not studied [2, 18–20]. Several previous studies have found that a recent occurrence of fracture was a greater risk factor for subsequent fracture than a history of earlier fracture, demonstrated for vertebral fracture [6, 10], hip, humeral and forearm fractures [3, 6] and all fractures combined [11].
A novel finding was that the high risk in the immediate post-fracture interval was age-dependent in that the marked transient increase in risk was not found at the age of 60 years and became progressively evident with advancing age. Many randomised studies have shown the early onset of effectiveness of pharmaceutical intervention for spine fractures and in some cases for appendicular fractures [21]. These benefits are particularly well documented in individuals with one or more prior vertebral fractures. If the same holds true for appendicular fractures, then our findings suggest that treatment should be commenced immediately after the occurrence of a fracture, in order to reduce the high immediate risk of further fracture. Moreover, the dividends of early intervention are particularly marked in the elderly, so that physicians should be encouraged to treat the very old with fracture prevention medication immediately after a fracture.
The reason for the transient marked increase in risk is not known, but immobilisation and impaired coordination are potential factors [22–24]. Indeed, a recent study of US claim databases identified fall-related factors such as age, poor mobility, neurological comorbidity and psychoactive medication use as associated with increased risk of first fracture over 12–24 months [24]. Since the study did not examine relationships over longer timescales (or from first to second fracture), it is impossible to evaluate whether the short-term relationships were of greater magnitude than they would have been long-term associations or whether the associations documented over 1–2 years simply demonstrated markers of generally increased fracture risk. A further complication of such analyses is that many risk factors will persist over time, for example the propensity to fall is usually a long-term attribute. Whilst dissecting out true risk factors for imminent as opposed to long-term risk presents an investigative challenge, our demonstration of an increased fracture risk in the first year after an index fracture suggests a relatively straightforward requirement for the targeting of assessment and therapy immediately following such an event.
One of the strengths in this study was the random sampling of a large population and the detail placed on fracture ascertainment and the long duration of observation. As participants were identified from nationwide registers representing 34% of the midlife Icelandic population born between 1907 and 1935 [14, 15], selection bias seems unlikely. However, there were also some limitations to this study. First, the fracture ascertainment was collected retrospectively but was based on all available records and X-rays from the main hospitals in Iceland. Second, there are known to be substantial differences in age- and sex-specific fracture incidence across Europe, with rates in northern Europe greater than those in the south. Although the absolute incidence values we observed may not be representative of other populations, there is no reason to suppose that there would be any difference in the age and temporal relationships. Third, we were not able to include radiographically defined vertebral fractures. This would have increased the rates, but we aimed to assess clinical fractures, and temporal evaluation of radiographic vertebral fractures would have required multiple sequential radiographs. Fourth, as with all such studies, the possibility of under-ascertainment and misclassification exists, but as both capture and classification of fractures have been shown to be highly reliable in this cohort [16], it is unlikely that this would alter the results materially.
A problem that potentially confounds most studies of incident fractures is the risk of double counting, and this can be of major relevance in studies examining rates of re-fracture within short timeframes. This is particularly problematic for vertebral fractures since the diagnosis is confirmed by radiography and the deformities are persistent over time, at least in adults. In the present study, we used a 30-day window before counting a second fracture at the same site which would diminish but not eliminate the risk that it was the same fracture. Extending the window further up to 2 years had little effect on the pattern with time. The most robust sensitivity analysis was to only count the second MOF when the site of the second fracture differed from the site of the first MOF. The imminent risk was still higher than after 5–10 years. These findings indicate that the concept of imminent risk is a reality rather than an artifact of double counting.
The risk of MOF after a first MOF is increased over the whole follow-up, but the imminent risk is even higher. Many randomised studies have shown the early onset of effectiveness of pharmaceutical intervention for spine fractures and in some cases for appendicular fractures [21]. These benefits are particularly well documented in individuals with one or more prior vertebral fractures. If the same holds true for appendicular fractures, then our findings suggest that treatment should be commenced immediately after fractures to reduce the high immediate risk of further fracture. Moreover, the finding that the imminent risk increases with age has several important implications in developing treatment strategies. In this regard, it will be of value to determine the pattern of fracture events with time following a sentinel fracture at the hip, spine, forearm or humerus to determine the potential gains in fractures avoided and cost-effectiveness of early treatment.
References
Johnell O, Kanis JA, Oden A et al (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Hansen L, Petersen KD, Eriksen SA et al (2015) Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int 26:513–519
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Haentjens P, Johnell O, Kanis JA et al (2004) Gender-related differences in short and long-term absolute risk of hip fracture after Colles’ or spine fracture: Colles’ fracture as an early and sensitive marker of skeletal fragility in men. J Bone Miner Res 19:1933–1944
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Johnell O, Oden A, Caulin F, Kanis JA (2001) Acute and long term increase in fracture risk after hospitalization for vertebral fracture. Osteoporos Int 12:207–214
Giangregorio LM, Leslie WD (2010) Manitoba bone density program. Time since prior fracture is a risk modifier for 10-year osteoporotic fractures. J Bone Miner Res 25:1400–1405
Dretakis KE, Dretakis EK, Papakitsou EF, Psarakis S, Steriopoulos K (1998) Possible predisposing factors for the second hip fracture. Calcif Tissue Int 62:366–369
Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B (2006) Short timeframe from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int 17:1353–1357
Lindsay R, Silverman SL, Cooper C et al (2001) Risk for new vertebral fracture in the year following a fracture. JAMA 285:320–323
van Geel TA, van Helden S, Geusens PP, Winkens B, Dinant GJ (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Bjornsson G, Bjornsson OJ, Davidsson D et al (1982) Report abc XXIV. Health survey in the Reykjavik area—women. Stages I-III, 1968–1969, 1971–1972 and 1976–1978. Participants, invitation, response etc. The Icelandic Heart Association, Reykjavík
Bjornsson OJ, Davidsson D., Olafsson H et al. (1979) Report XVIII. Health survey in the Reykjavik area—men. Stages I–III, 1967–1968, 1970–1971 and 1974–1975. Participants, invitation, response etc. The Icelandic Heart Association, Reykjavík
Siggeirsdottir K, Aspelund T, Sigurdsson G et al (2007) Inaccuracy in self-report of fractures may underestimate association with health outcomes when compared with medical record based fracture registry. Eur J Epidemiol 22:631–639
Breslow NE, Day NE (1987) Statistical methods in cancer research. IARC Scientific Publications No 32 II:131–135
Ismail AA, Cockerill W, Cooper C et al (2001) Prevalent vertebral deformity predicts incident hip though not distal forearm fracture: results from the European Prospective Osteoporosis Study. Osteoporos Int 12:85–90
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res 24:1299–1307
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation ( IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Bischoff Ferrari HA, Dawson Hughes B, Willett WC et al (2004) Effect of vitamin D on falls: a meta-analysis. JAMA 291:1999–2006
Helden van S, Wyers CE, Dagnelie PC et al (2007) Risk of falling in patients with a recent fracture. BMC Musculoskelet Disord 8:55
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26. doi:10.1007/s11657-016-0280-5
Acknowledgements
We thank the participants in the Reykjavik Study for their valuable contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the National Bioethics Committee and the Data Protection Authority in Iceland. All participants gave informed written consent.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Johansson, H., Siggeirsdóttir, K., Harvey, N.C. et al. Imminent risk of fracture after fracture. Osteoporos Int 28, 775–780 (2017). https://doi.org/10.1007/s00198-016-3868-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3868-0