Abstract
Summary
Soluble CD14 (sCD14) is an inflammatory marker associated with osteoclasts. Using Cox proportional hazards models, we found a positive association between plasma levels of sCD14 and risk of incident fracture among participants in the Cardiovascular Health Study. sCD14 may be useful in identifying those at risk for fracture.
Introduction
Soluble CD14, a proinflammatory cytokine, is primarily derived from macrophages/monocytes that can differentiate into osteoclasts. The purpose of this study was to examine the relationship between sCD14 levels and osteoporotic fractures.
Methods
In the Cardiovascular Health Study, 5462 men and women had sCD14 levels measured at baseline. Incident hip fractures (median follow-up time 12.5 years) and incident composite fractures (defined as the first hip, pelvis, humerus, or distal radius fracture, median follow-up 8.6 years) were identified from hospital discharge summaries and/or Medicare claims data. Cox proportional hazards models were used to model the association between sCD14 levels and time to incident hip or composite fracture, overall and as a function of race and gender.
Results
In unadjusted models, there was a positive association between sCD14 levels (per 1 standard deviation increase, i.e., 361.6 ng/mL) and incident hip (HR, 1.26; 95 % CI, 1.17, 1.36) and composite (HR, 1.20; 95 % CI, 1.12, 1.28) fractures. When models were fully adjusted for demographics, lifestyle factors, and medication use, these associations were no longer significant. However, in whites, the association of sCD14 levels with hip fractures remained significant in fully adjusted models (HR, 1.11; 95 % CI, 1.01–1.23). Associations of sCD14 levels with hip and composite fracture did not differ between men and women.
Conclusions
In this large cohort of community-dwelling older adults, higher sCD14 levels were associated with an increased risk of incident hip fractures in whites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have demonstrated a link between increased levels of proinflammatory cytokines (e.g., interleukin-6 (IL-6) [1, 2], tumor necrosis factor-α (TNF-α)) [1], C-reactive protein (CRP) [1, 3]) and hip fracture risk. However, these associations may differ by race, as African-Americans have higher levels of IL-6 [4–8] and CRP [5, 8, 9] but lower fracture risk [10–12]. Soluble CD14 (sCD14), a coreceptor for bacterial lipopolysaccharide, is a proinflammatory cytokine that may be more directly connected to bone health. In humans, it is produced by both hepatocytes [13] and proteolytic cleavage of membrane-bound CD14 [14] on monocytes and macrophages, which are precursors to mature osteoclasts [15–17]. sCD14 acts as an acute phase reactant [18] and regulates T-lymphocyte activation and function [19] with decreases in interleukin -4 (IL-4) and interferon gamma production. Elevations in acute phase reactants [20] and lower levels of interferon gamma and IL-4 are associated with osteoporosis [19].
To our knowledge, no prior study has examined the relationship of sCD14 with osteoporotic fractures. We hypothesized that there would be a positive association between plasma sCD14 levels and incident fractures. Since African-Americans have higher levels of the inflammatory markers IL-6 and CRP than whites, yet a lower risk of fractures than whites, we decided a priori to further examine the impact of race on our outcomes.
Methods
Subjects
The Cardiovascular Health Study [21] is a longitudinal, community-based study of older men and women (age ≥65 years) designed to determine the factors that predict development and progression of cardiovascular disease. The main cohort of 5201 participants was enrolled between 10 June 1989 and 30 May 1990. To increase minority representation, an additional 687 participants, predominantly African-American, were recruited from 17 November 1992 through 11 June 1993. Participants were excluded if they were institutionalized, required a proxy, were unable to complete informed consent, were planning to move out of the area within 3 years of recruitment, required a wheelchair at home, were receiving hospice care, or were undergoing radiation or chemotherapy for cancer. In-person examinations were performed annually from 1989 to 1999 and again in 2005 to 2006. Telephone interviews were conducted semiannually from 1989 to 1999 and biannually thereafter. The institutional review board at each site approved the study methods, and all participants gave written informed consent.
sCD14 measurement
sCD14 levels were measured at the baseline visit. All CHS participants with an sCD14 measurement (n = 5462) were eligible for inclusion into this study. Blood samples were drawn on the morning of enrollment after an overnight fast. Plasma samples were stored at −70 °C, then thawed, and sCD14 levels were measured with a commercial enzyme-linked immunosorbent assay (ELISA, R&D Systems, Minneapolis, MN) [22]. The inter-assay coefficients of variation ranged from 5.32 to 12.36 % [22].
Fracture ascertainment
The primary outcome for this study was incident hip fractures. Incident hip fractures were defined by a hospital discharge International Classification of Diseases, Ninth Revision (ICD-9), code of 820.xx. CHS prospectively gathered all hospitalization data, including discharge summaries, from participants every 6 months. To ensure completeness of hospitalization records, data were checked against Medicare claims data to identify any hospitalizations not reported by participants. Follow-up for incident hip fracture occurred until a hip fracture event, death, loss to follow-up, or until 31 December 2011. Hip fractures caused by motor vehicle accidents or severe injury were excluded.
The secondary outcome, incident composite fracture, was identified from a merged CHS-CMS dataset based on hospitalization discharge ICD-9 codes for fractures of the hip (820.xx), pelvis (808.xx), humerus (812.xx), or distal forearm (813.4 or 813.5) and inpatient, outpatient, or physician service claims. Qualifying fractures identified from hospital discharge codes or other inpatient claims only required one of these ICD-9 diagnosis codes, while fractures identified from outpatient or physician claims also required a corresponding Current Procedural Terminology (CPT) procedure code consistent with treatment of this fracture type. Follow-up for incident composite fracture occurred until a composite fracture event, death, loss to follow-up, or until 30 July 2009. Follow-up for incident composite fractures was available for each participant in the composite fracture cohort only during the time in which the participant was enrolled within fee-for-service Medicare.
Covariates
We included as covariates factors associated with sCD14 levels or with osteoporosis. sCD14 levels are known to vary by age [22, 23], gender [22], race [22], BMI [24, 25], insulin levels and insulin sensitivity [26], smoking status [27], alcohol intake [28], and kidney function [29], all of which also are related to BMD and/or fracture risk. Walking pace (miles per hour (mph)) was included as a measure of physical activity [30]. Use of calcium supplements [31, 32] and health status [33] (excellent/very good/good/fair/poor), were also included. Additionally, the use of estrogen [34] and other medications known to modify bone mineral density or fracture risk (statins [35], loop diuretics [36], thiazides [37], thyroid hormones [38]), and corticosteroids [39]) were included. Participants who were using bisphosphonates or selective estrogen receptor modulators (SERMs) were excluded.
Statistical analysis
We compared baseline characteristics between CHS participants versus without sCD14 measures using t tests for continuous variables and chi-square tests for categorical variables. In participants with available sCD14 measures, we described and compared baseline participant characteristics across sCD14 quartiles using linear trend tests for continuous variables and chi-square tests for categorical variables.
Time to hip fracture was calculated as the interval from baseline visit to the earliest date of first incident hip fracture, death, loss to follow-up, or end of follow-up on 31 December 2011. Time to composite fracture was calculated as the interval from baseline to the earliest date of first incident composite fracture (i.e., hip, pelvis, humerus, or distal forearm), death, loss to follow-up, or end of follow-up on 30 July 2009, during fee-for-service Medicare enrollment.
Kaplan-Meier curves were generated to describe the association between sCD14 quartiles and time to incident hip and composite fracture. Log-rank tests were used to compare the curves across sCD14 quartiles.
For each of the two fracture outcomes, we used Cox proportional hazards models to estimate the hazard ratio (HR) of incident fracture, as associated with 1 standard deviation (SD) increase in sCD14 level (361.6 ng/mL). To examine the linearity of sCD14 in Cox regression, we used restricted cubic splines in Generalized Additive Modeling. We evaluated the validity of the proportional hazards assumption graphically and numerically using Schoenfeld residuals and found no meaningful departures.
Models were adjusted as follows: model 1, unadjusted; model 2, demographic variables (age, gender, race, BMI); model 3, factors in model 2 and smoking status (current versus former/never), alcohol use (for female ≥7 drinks/week, for male ≥14 drinks/week), presence of diabetes, estrogen use, and medication use (statins, loop diuretics, thiazides, thyroid hormones), and creatinine-based eGFR.
Interactions with race and gender were explored, and stratified analyses were performed. Insulin and insulin sensitivity also may affect sCD14 levels [26]. Additionally, the activity of sCD14 concentrations as an acute phase reactant differs in diabetic and nondiabetic subjects [40]; thus, we also performed post hoc analyses separately evaluating the association of sCD14 in participants with and without diabetes.
All analyses were conducted using R statistical analysis program [41].
Results
CHS cohorts 1 (enrolled in year 1989/1990) and 2 (enrolled in year 1992/1993) included 5888 total individuals. Of the 5888 CHS participants, 5462 (92.8 %) had sCD14 measurements on plasma obtained at baseline and provided hip fracture data. Among those with sCD14 measurements available, there were 4643 whites (85.0 %) and 819 African-Americans (15.0 %). Characteristics of individuals with and without sCD14 measurements are presented in the Appendix. Subjects who did not have sCD14 measurement at baseline were more likely to be African-American, have a greater BMI, and worse kidney function than those who did have an sCD14 measurement. Of the 5888 CHS participants, 4728 (80.3 %) were enrolled in CMS and provided composite fracture data (Fig. 1). Those not enrolled in CMS were more likely to be male, African-American, not use alcohol, and, among women, were more likely to have used estrogen (data not shown). There were no significant differences in the mean serum sCD14 measurements (p = 0.26) or incidence of hip fractures (p = 0.70) between those enrolled and not enrolled in CMS.
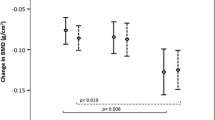
Baseline characteristics of the cohort with measured sCD14 levels, stratified by increasing quartiles of sCD14 levels, are shown in Table 1. There were significant differences in all demographic categories (age, gender, race, BMI) as well in health status, walking pace, alcohol use (yes or no), smoking status (yes or no), creatinine and GFR levels, presence of diabetes, estrogen use, and corticosteroid use across the quartiles of sCD14 levels. The highest quartile of sCD14 had the following characteristics: older age, more females, fewer African-Americans, lower BMI, a higher frequency of individuals reporting “fair” or “poor” health, fewer individuals that could walk 3 mph or faster, more current smokers, higher creatinine/lower GFR, more participants with diabetes, less estrogen use, but more frequent use of corticosteroids and calcium supplements. White females had the highest levels of sCD14, followed by White males, African-American females, and African-American males (Fig. 2). After adjusting for race, sCD14 levels in men were lower than in women by an average of 113. 5 ng/mL (95 % confidence interval (CI) [−132.5, −94.5], p < 0.01) (Fig. 2).
Incident hip fractures were identified in 672 (12.3 %) of the 5462 subjects with available sCD14 levels. Incident composite fractures occurred in 940 of the 4728 (19.9 %) subjects with data available for this outcome. Overall, there was a positive relationship between increasing sCD14 levels (per 1 SD) and hazard for incident fracture (log-rank test p value <0.01, Fig. 3). The unadjusted HR for hip fracture per 1‐SD increment increase in sCD14 levels was 1.26 (95 % CI, [1.17, 1.36]); in minimally adjusted models, the HR was 1.12 (95 % CI [1.03, 1.22], Table 2). Similarly, the unadjusted HR for composite fracture risk per 1‐SD sCD14 level was 1.20 (95 % CI [1.12, 1.28]); in minimally adjusted models, the HR was 1.076 (95 % CI [1.004, 1.154], Table 3). However, in fully adjusted models, all of these associations were no longer statistically significant (Tables 2 and 3). For incident hip fractures, there was evidence of a possible interaction for race (p = 0.08). Although in whites, HRs for hip fracture per 1-SD increment increase in sCD14 were significantly higher in unadjusted (HR 1.24, 95 % CI [1.14, 1.35]), minimally adjusted (HR 1.13, 95 % CI [1.04, 1.23]), and fully adjusted models (HR 1.11, 95 % CI [1.01, 1.23]) (Table 2); there was no association between sCD14 levels and incident hip fractures in African-Americans in any model (Table 2). No significant interactions for race (p = 0.92) or diabetes status (p = 0.97) were present in the composite fracture analysis, and no significant interactions were present for gender for either fracture outcome (p ≥ 0.53).
In a post hoc analysis, there was also was a suggestion of an interaction (p = 0.08) for the presence of diabetes. In participants without diabetes, there was a positive association of incident hip fractures per 1-SD increment increase in sCD14 in unadjusted (HR 1.30, 95 % CI [1.20, 1.40]) and fully adjusted models (HR 1.13, 95 % CI [1.02,1.25]) (Appendix Table 5). In subjects with diabetes, there was no association of sCD14 levels with incident hip fractures in any model (Appendix Table 5). No significant interactions were present for diabetes status in the composite fracture analysis (p = 0.97).
In the fully adjusted models for hip fracture, there was little to no attenuation of the HRs for each covariate when including and excluding sCD14 levels (Appendix, Table 6).
Discussion
In this cohort of older, community-dwelling men and women, increased sCD14 levels were associated with a heightened risk of incident hip fractures among White individuals. Though the sCD14-hip fracture associations did not differ by gender, they appeared significantly stronger in nondiabetic than in diabetic individuals in post hoc analyses.
There is limited prior data on sCD14 and bone metabolism. Prior animal and human data have suggested a potentially important link between CD14+ cells and bone mass. Mice with an inactivating mutation to the CD14 gene have a phenotype of increased bone mineral content [42]. In humans, CD14 mRNA expression is upregulated in osteoporotic bones compared to normal bones [43]. Circulating CD14+ cells are increased in those with osteoporosis compared with healthy controls [44]. In a 3-month study, the bisphosphonate risedronate reduced levels of circulating CD14+ cells in women with osteoporosis [45]. The current study adds to our understanding of sCD14 biology in a population of older, community-dwelling adults.
Our finding that White females had the highest levels of sCD14, followed by White males, African-American females, and lastly, African-American males, confirms the results of a previous study conducted in CHS [22]. Additionally, our findings that higher sCD14 levels are associated with older age [22], lower BMI [24, 25], smoking [27], alcohol use [28], poorer kidney function [29], and diabetes [26] are in agreement with published reports in other patient populations. To our knowledge, we are the first to report that high levels of sCD14 are associated with less estrogen use, although this finding is not surprising, since higher sCD14 levels are seen with rising age, and older females are less likely to use estrogen than younger females [46]. Similarly, this is the first report of a higher frequency of corticosteroid use among those with the highest sCD14 levels, although levels of membrane-bound CD14 have been reported to increase with corticosteroid use [47]. The observation of fewer individuals in the highest quartile of sCD14 able to walk 3 mph or faster is consistent with prior reports of an association between higher physical activity levels and lower levels of circulating CD14+ cells [48]. That higher sCD14 levels were associated with an increased frequency of self-reported “fair” or “poor” health status is consistent with it being a marker of increased inflammation. The reasons why more frequent use of calcium supplements were observed in the highest quartile of sCD14 are not clear.
Increased sCD14 levels likely reflect bone resorption due to its presence on cells of the osteoclast lineage. Bone turnover is higher in whites than in African-Americans [49–51], and hip fractures are associated with higher bone turnover [52, 53]. If sCD14 was simply reflective of bone turnover, one would have assumed, contrary to what we found, that the relationship between sCD14 and hip fractures would be independent of race or diabetes status. Our findings suggest that sCD14 may reflect more fundamental differences in bone health between African-Americans and Caucasians other than bone turnover.
Diabetes is a risk factor for fracture [54, 55], and in our study, the proportion of people with diabetes rose in each quartile of sCD14 level. This finding is in accord with a previously published report finding that decreased insulin sensitivity was associated with higher sCD14 levels [26]. However, our post hoc analyses indicated that sCD14 levels were only associated with hip fractures in nondiabetic individuals. The reasons for the lack of association in people with diabetes are not clear, but it is possible that alterations in the bone microstructure of diabetic individuals may play a more important role in hip fracture than inflammation. In support of this, Yu et al. recently reported that radial bone cortical porosity was significantly greater in African-American women with diabetes compared to those without, while areal and volumetric BMD was similar between the groups [56]. The lack of an association between sCD14 levels and hip fractures in those with diabetes is also consistent with a report that sCD14 behaves as an acute phase reactant in nondiabetic, but not diabetic, subjects [40].
The results reported here have similarities to other studies examining the role of inflammatory markers in nontraumatic fracture risk. Specifically, one report found significant elevations in the relative risk (RR) for fragility fractures among those with the highest serum levels of the soluble receptor for IL-2 (RR 1.52, 95 % CI [1.04–2.21]), TNF soluble receptor 1 (RR 1.73, 95 % CI [1.18–2.55]), and TNF soluble receptor 2 (RR 1.48, 95 % CI [1.01–2.20]) [1]. Unlike the results reported in the current study, the risks remained significantly elevated when adjusting for race and diabetes status. In women in the Women’s Health Initiative, higher levels of three cytokine-soluble receptors: interleukin-6 (IL-6), soluble receptor (SR), and TNF SR1 and SR2 were significantly associated with hip fractures [2].Others reported significantly elevated HRs for hip fractures among older White females with the highest levels of IL-6 (HR 1.64, 95 % CI [1.09–2.48]) and TNF soluble receptor 1 (HR 2.05, 95 % CI [1.35–3.12]) [57]. Interestingly, that report identified kidney function and BMD as potential mediators of this effect [57], while in the current study, including sCD14 did not significantly alter the HRs for hip fracture when adjusting for kidney function (Appendix Table 6). We did not include BMD in our models due the unequal time gap between the blood collection for the sCD14 measurement and the DEXA scan acquisition between the two cohorts (5 years for cohort 1, 2 years for cohort 2). This study has several strengths. Our study is the first to examine the association between the sCD14 inflammatory marker and incident fractures. The large sample sizes in this study allow for a more precise estimate of the risk of fracture associated with sCD14. We adjusted the analytic models with a comprehensive set of potentially confounding variables.
This study also has several limitations. First, sCD14 levels were not available in all CHS participants though the characteristics of those with and the <8 % without sCD14 measurements were similar. Importantly, hip fracture incidence was not significantly different between those with and without sCD14 measurement. Second, data on composite fractures were only available in the subset of CHS subjects enrolled in CMS (83 % of the cohort); there was no difference in sCD14 levels (p = 0.26) or number of hip fractures (p = 0.70) between those enrolled and those not enrolled in CMS. Third, because markers of bone turnover were not measured in CHS, we could not evaluate to what extent associations between sCD14 levels and hip fracture may have been accounted for by levels of bone resorption markers such as NTX. Fourth, CHS is an observational study, and although analyses accounted for multiple potential confounding variables, the possibility of residual confounding remains. Last, analyses examining the association of sCD14 with hip fractures by diabetes status were post hoc, and observed results could have been attributable to chance.
In conclusion, we found that increased sCD14 levels were associated with a heightened risk of incident hip fractures among White individuals. Further, the association between sCD14 and hip fracture was stronger in those without diabetes than in those with diabetes. More research is needed to elucidate the role of sCD14 in inflammation and bone metabolism; however, these findings suggest that sCD14, alone or in combination with other inflammatory markers, may help identify those individuals most at risk of fracture.
References
Cauley JA, Danielson ME, Boudreau RM, Forrest KYZ, Zmuda JM, Pahor M et al (2007) Inflammatory markers and incident fracture risk in older men and women: the health aging and body composition study. J Bone Miner Res 22(7):1088–1095
Barbour KE, Boudreau R, Danielson ME, Youk AO, Wactawski-Wende J, Greep NC et al (2012) Inflammatory markers and the risk of hip fracture: the women’s health initiative. J Bone Miner Res 27(5):1167–1176
Ishii S, Cauley JA, Greendale GA, Crandall CJ, Danielson ME, Ouchi Y et al (2013) C‐Reactive protein, bone strength, and nine‐year fracture risk: data from the study of Women’s Health Across the Nation (SWAN). J Bone Miner Res 28(7):1688–1698
Feairheller DL, Park JY, Sturgeon KM, Williamson ST, Diaz KM, Veerabhadrappa P et al (2011) Racial differences in oxidative stress and inflammation: in vitro and in vivo. Clin Transl Sci 4(1):32–37
Paalani M, Lee JW, Haddad E, Tonstad S (2011) Determinants of inflammatory markers in a bi-ethnic population. Ethn Dis 21(2):142
Park N-J, Kang D-H (eds) (2013) Inflammatory cytokine levels and breast cancer risk factors: racial differences of healthy Caucasian and African American women. Onc Nurs Soc
Veeranna V, Zalawadiya SK, Niraj A, Kumar A, Ference B, Afonso L (2013) Association of novel biomarkers with future cardiovascular events is influenced by ethnicity: results from a multi-ethnic cohort. Int J Cardiol 166(2):487–493
Morimoto Y, Conroy SM, Ollberding NJ, Kim Y, Lim U, Cooney RV et al (2014) Ethnic differences in serum adipokine and C-reactive protein levels: the multiethnic cohort. Int J Obes 38(11):1416–1422
Nazmi A, Victora CG (2007) Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies. BMC Public Health 7(1):212
Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA (1990) Hip fracture incidence among the old and very old: a population-based study of 745,435 cases. Am J Public Health 80(7):871–873
Bohannon AD (1999) Osteoporosis and African American women. J Womens Health Gend Based Med 8(5):609
Burge R, Dawson‐Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis‐related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475
Meuleman P, Steyaert S, Libbrecht L, Couvent S, Van Houtte F, Clinckspoor F et al (2006) Human hepatocytes secrete soluble CD14, a process not directly influenced by HBV and HCV infection. Clin Chim Acta 366(1):156–162
Bažil V, Baudyš M, Hilgert I, Štefanová I, Low MG, Zbrožek J et al (1989) Structural relationship between the soluble and membrane-bound forms of human monocyte surface glycoprotein CD 14. Mol Immunol 26(7):657
Massey HM, Flanagan AM (1999) Human osteoclasts derive from CD14-positive monocytes. Br J Haematol 106(1):167
Sørensen MG, Henriksen K, Schaller S, Henriksen DB, Nielsen FC, Dziegiel MH et al (2007) Characterization of osteoclasts derived from CD14+ monocytes isolated from peripheral blood. J Bone Miner Metab 25(1):36–45
Nicholson GC, Malakellis M, Collier FM, Cameron PU, Holloway WR, Gough TJ et al (2000) Induction of osteoclasts from CD14-positive human peripheral blood mononuclear cells by receptor activator of nuclear factor kappaB ligand (RANKL). Clin Sci 99(2):133
Bas S, Gauthier BR, Spenato U, Stingelin S, Gabay C (2004) CD14 is an acute-phase protein. J Immunol 172(7):4470–4479
Zhang J, Fu Q, Ren Z, Wang Y, Wang C, Shen T, et al (2014) Changes of serum cytokines-related Th1/Th2/Th17 concentration in patients with postmenopausal osteoporosis. Gynecol Endocrinol 1–8
Eriksson AL, Movérare‐Skrtic S, Ljunggren Ö, Karlsson M, Mellström D, Ohlsson C (2014) High‐sensitivity CRP is an independent risk factor for all fractures and vertebral fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 29(2):418–423
Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA et al (1991) The cardiovascular health study: design and rationale. Ann Epidemiol 1(3):263–276
Reiner AP, Lange EM, Jenny NS, Chaves PH, Ellis J, Li J et al (2013) Soluble CD14: genomewide association analysis and relationship to cardiovascular risk and mortality in older adults. Arterioscler Thromb Vasc Biol 33(1):158
Nicu EA, Laine ML, Morré SA, Van der Velden U, Loos BG (2009) Soluble CD14 in periodontitis. Innate Immun 15(2):121–128
Mikuls TR, LeVan TD, Sayles H, Yu F, Caplan L, Cannon GW et al (2011) Soluble CD14 and CD14 polymorphisms in rheumatoid arthritis. J Rheumatol 38(12):2509–2516
Raj DSC, Carrero JJ, Shah VO, Qureshi AR, Bárány P, Heimbürger O et al (2009) Soluble CD14 levels, interleukin 6, and mortality among prevalent hemodialysis patients. Am J Kidney Dis 54(6):1072
Fernández-Real JM, Broch M, Richart C, Vendrell J, López-Bermejo A, Ricart W (2003) CD14 monocyte receptor, involved in the inflammatory cascade, and insulin sensitivity. J Clin Endocrinol Metab 88(4):1780–1784
Valiathan R, Miguez MJ, Patel B, Arheart KL, Asthana D (2014) Tobacco smoking increases immune activation and impairs T-cell function in HIV infected patients on antiretrovirals: a cross-sectional pilot study. PLoS One 9(5):e97698
Frank J, Witte K, Schrödl W, Schütt C (2004) Chronic alcoholism causes deleterious conditioning of innate immunity. Alcohol Alcohol 39(5):386–392
Abraham AG, Darilay A, McKay H, Margolick JB, Estrella MM, Palella FJ, et al (2015) Kidney dysfunction and markers of inflammation in the multicenter AIDS cohort study. J Infect Dis jiv159
Robinson-Cohen C, Katz R, Mozaffarian D, Dalrymple LS, de Boer I, Sarnak M et al (2009) Physical activity and rapid decline in kidney function among older adults. Arch Intern Med 169(22):2116–2123
Wilczynski C, Camacho P (2014) Calcium use in the management of osteoporosis: continuing questions and controversies. Curr Osteoporos Rep 12(4):396–402
Carmeliet G, Dermauw V, Bouillon R (2015) Vitamin D signaling in calcium and bone homeostasis: a delicate balance. Best Pract Res Clin Endocrinol Metab 29(4):621–631
Leavy B, Byberg L, Michaelsson K, Melhus H, Aberg AC (2015) The fall descriptions and health characteristics of older adults with hip fracture: a mixed methods study. BMC Geriatr 15:40
Cauley JA, Robbins J, Chen Z, Cummings SR, Jackson RD, LaCroix AZ et al (2003) Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA 290(13):1729–1738
Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret G-Y (2007) Effects of statins on bone mineral density: a meta-analysis of clinical studies. Bone 40(6):1581–1587
Carbone LD, Johnson KC, Bush AJ, Robbins J, Larson JC, Thomas A et al (2009) Loop diuretic use and fracture in postmenopausal women: findings from the Women’s Health Initiative. Arch Intern Med 169(2):132–140
Bolland MJ, Ames RW, Horne AM, Orr-Walker BJ, Gamble GD, Reid IR (2007) The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos Int 18(4):479–486
Uzzan B, Campos J, Cucherat M, Nony P, Boissel JP, Perret GY (1996) Effects on bone mass of long term treatment with thyroid hormones: a meta-analysis. J Clin Endocrinol Metab 81(12):4278–4289
Ioannidis G, Pallan S, Papaioannou A, Mulgund M, Rios L, Ma J et al (2014) Glucocorticoids predict 10-year fragility fracture risk in a population-based ambulatory cohort of men and women: Canadian Multicentre Osteoporosis Study (CaMos). Arch Osteoporos 9(1):1–8
Fernández-Real J-M, López-Bermejo A, Castro A, Broch M, Peñarroja G, Vendrell J et al (2005) Opposite relationship between circulating soluble CD14 concentration and endothelial function in diabetic and nondiabetic subjects. Thromb Haemost 94(3):615–619
R Core Team (2008) R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. ISBN 3-900051-07-0, URL http://www.Rproject.org
Johnson GB, Riggs BL, Platt JL (2004) A genetic basis for the “Adonis” phenotype of low adiposity and strong bones. FASEB J 18(11):1282
Hopwood B, Tsykin A, Findlay DM, Fazzalari NL (2009) Gene expression profile of the bone microenvironment in human fragility fracture bone. Bone 44(1):87
Nose M, Yamazaki H, Hagino H, Morio Y, Hayashi S-I, Teshima R (2009) Comparison of osteoclast precursors in peripheral blood mononuclear cells from rheumatoid arthritis and osteoporosis patients. J Bone Miner Metab 27(1):57
D’Amelio P, Grimaldi A, Di Bella S, Tamone C, Brianza SZM, Ravazzoli MGA et al (2008) Risedronate reduces osteoclast precursors and cytokine production in postmenopausal osteoporotic women. J Bone Miner Res 23(3):373
Levy BT, Ritchie JM, Smith E, Gray T, Zhang W (2003) Physician specialty is significantly associated with hormone replacement therapy use. Obstet Gynecol 101(1):114–122
Kodama M, Takahashi H, Iwagaki H, Itoh H, Morichika T, Yoshida A et al (2002) Effect of steroids on lipopolysaccharide/interleukin 2-induced interleukin 18 production in peripheral blood mononuclear cells. J Int Med Res 30(2):144–160
Markofski MM, Carrillo AE, Timmerman KL, Jennings K, Coen PM, Pence BD et al (2014) Exercise training modifies ghrelin and adiponectin concentrations and is related to inflammation in older adults. J Gerontol A-Biol Sci Med Sci 69(6):675–681
Bell NH, Williamson BT, Hollis BW, Riggs BL (2001) Effects of race on diurnal patterns of renal conservation of calcium and bone resorption in premenopausal women. Osteoporos Int 12(1):43–48
Finkelstein JS, Sowers M, Greendale GA, Lee M-LT, Neer RM, Cauley JA et al (2002) Ethnic variation in bone turnover in pre-and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab 87(7):3051–3056
Sowers MR, Zheng H, Greendale GA, Neer RM, Cauley JA, Ellis J et al (2013) Changes in bone resorption across the menopause transition: effects of reproductive hormones, body size, and ethnicity. J Clin Endocrinol Metab 98(7):2854–2863
Garnero P, Hausherr E, Chapuy MC, Marcelli C, Grandjean H, Muller C et al (1996) Markers of bone resorption predict hip fracture in elderly women: the EPIDOS prospective study. J Bone Miner Res 11(10):1531–1538
Johansson H, Odén A, Kanis JA, McCloskey EV, Morris HA, Cooper C et al (2014) A meta-analysis of reference markers of bone turnover for prediction of fracture. Calcif Tissue Int 94(5):560–567
Strotmeyer ES, Cauley JA, Schwartz AV, Nevitt MC, Resnick HE, Bauer DC et al (2005) Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition study. Arch Intern Med 165(14):1612–1617
Janghorbani M, Feskanich D, Willett WC, Hu F (2006) Prospective study of diabetes and risk of hip fracture the nurses’ health study. Diabetes Care 29(7):1573–1578
Yu EW, Putman MS, Derrico N, Abrishamanian-Garcia G, Finkelstein JS, Bouxsein ML (2014) Defects in cortical microarchitecture among African-American women with type 2 diabetes. Osteoporos Int 1–7
Barbour KE, Lui LY, Ensrud KE, Hillier TA, LeBlanc ES, Steven W et al (2014) Inflammatory markers and risk of hip fracture in older white women: the study of osteoporotic fractures. J Bone Miner Res 29(9):2057–2064
Acknowledgments
This research was supported by contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and grant U01HL080295 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by R01AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work does not reflect the views of the Veterans Health Administration or the United States government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bethel, M., Bůžková, P., Fink, H.A. et al. Soluble CD14 and fracture risk. Osteoporos Int 27, 1755–1763 (2016). https://doi.org/10.1007/s00198-015-3439-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3439-9