Abstract
Aging is associated with an increase in circulating inflammatory factors. One, the cytokine stromal cell-derived factor 1 (SDF-1 or CXCL12), is critical to stem cell mobilization, migration, and homing as well as to bone marrow stem cell (BMSC), osteoblast, and osteoclast function. SDF-1 has pleiotropic roles in bone formation and BMSC differentiation into osteoblasts/osteocytes, and in osteoprogenitor cell survival. The objective of this study was to examine the association of plasma SDF-1 in participants in the cardiovascular health study (CHS) with bone mineral density (BMD), body composition, and incident hip fractures. In 1536 CHS participants, SDF-1 plasma levels were significantly associated with increasing age (p < 0.01) and male gender (p = 0.04), but not with race (p = 0.63). In multivariable-adjusted models, higher SDF-1 levels were associated with lower total hip BMD (p = 0.02). However, there was no significant association of SDF-1 with hip fractures (p = 0.53). In summary, circulating plasma levels of SDF-1 are associated with increasing age and independently associated with lower total hip BMD in both men and women. These findings suggest that SDF-1 levels are linked to bone homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major public health problem, affecting 12 million Americans [1]. Although the mechanisms involved in age-related osteoporosis remain poorly defined, recent studies from our group and others suggest it may be a stem cell disease [2–4]. Aging triggers impaired localization, proliferation, survival, and differentiation of the main bone marrow (BM) stem cell populations, including bone marrow mesenchymal stromal/stem cells (BMSCs). Aging is also associated with a generalized increase in circulating inflammatory factors. One of these, the cytokine stromal cell-derived factor 1 (SDF-1 or CXCL12), has been shown to be essential to BMSC function [5–7]. SDF-1 likely plays multiple roles in bone formation through regulation of BMSC migration, recruitment, and engraftment, as well as BMSC survival and differentiation into osteoblasts and osteocytes along with osteoblast survival and proliferation [5–9]. Additionally, SDF-1 and its receptors are found in adipocytes and associated with adipose tissue, possibly contributing to what is now being recognized as a Fat-Bone axis [10–13]. This suggests a complex relationship, not only in normal tissue, including skeletal, and adipose tissue, during development and maintenance, but also that this relationship may change with age and chronic inflammatory stimulation.
There appears to be a difference in either expression or turnover of SDF-1 in different tissue compartments that is poorly understood. The cytokine SDF-1 is secreted by cells in multiple tissues as a local paracrine signaling factor and as a long distance chemokine in response to injury to help mobilize and target immune response cells and reparative cells to areas of injury and inflammation [14]. As such, there is a relatively steady basal/homeostatic level of SDF-1 in plasma reflecting summed chronic responses with acute short-term increases induced by events like tissue injury. Given that SDF-1 is a powerful pleiotropic cytokine its secretion and turnover is tightly regulated so that a specific newly secreted molecule is available as a bioactive ligand, one that can bind to and activate its receptors, with a half-life of only a few minutes [8, 15–18]. Newly secreted SDF-1 is rapidly degraded in plasma by a series of proteases and peptidases to a point where the degraded forms are cleared. In plasma, the removal of the first two N-terminal amino acids by Dipeptidyl peptidase-4 (DPP4) occurs within less than 5 min; this initial cleavage prevents SDF-1 from being able to activate its receptor CXCR4. Shortly thereafter, additional degradation of the N-terminal end occurs to the point that ELISA can no longer be used to detect the remnant of the circulating cytokine, and it is cleared by the kidney with a half-life of approximately 25 min [15, 19]. In musculoskeletal tissues, mRNA and protein expression of SDF-1 and its receptors have been reported to both increase and decline with aging, while in the plasma, levels are reported to consistently rise with aging [19–22]. Increases in plasma SDF-1 levels with age maybe compensatory for reduced receptor signaling or other factors including chronic tissue injury. Increased plasma SDF-1 levels have been reported to be linked to a decrease in the level of circulating endothelial progenitor cells that are important in angiogenesis and vascular repair, factors that may be critical in osteogenesis and osteoporosis [20, 22, 23]. For example, this decline in circulating stem cells may be related to higher plasma SDF-1 levels that ultimately result in exhaustion of endothelial progenitor cells, along with other stem cell populations such as mesenchymal BMSC pools, as a consequence of SDF-1 driven mobilization with reduced rehoming to the stem cell niche over time. Alternatively or concurrently, an increase in the percentage of the circulating SDF-1 that is inactivated by proteolytic post-translational modification could result in reduced overall SDF-1 bioactivity with age and therefore reduce BMSC self-replacement or function [20, 23].
Despite an association of SDF-1 to osteogenesis, the relationship of circulating SDF-1 to bone mineral density (BMD), body composition, and osteoporotic fractures has not previously been reported. As such, the purpose of this study was to examine the association of plasma SDF-1 in elderly men and women with BMD of the lumbar spine, total hip and femoral neck, body composition, and incident hip fractures.
Materials and Methods
Participants
The Cardiovascular Health Study [24] is a longitudinal, community-based study of older men and women (age ≥ 65 years) designed to determine the factors that predict development and progression of cardiovascular disease [24]. Participants were recruited through random sampling from Medicare eligibility lists at 4 locations: Forsyth County, North Carolina; Sacramento County, California; Washington County, Maryland; and Allegheny County, Pennsylvania. The main cohort of 5201 participants was enrolled between 10 June 1989 and 30 May 1990. To increase minority representation, an additional 687 African–American participants were recruited from November 1992 through 11 June 1993. Participants were excluded if they were institutionalized, required a proxy to complete informed consent, were planning to move out of the area within 3 years of recruitment, required a wheelchair in the home, were receiving hospice care, or were undergoing radiation or chemotherapy for cancer. In-person, examinations were performed annually from 1989 to 1999 and again in 2005 to 2006. Telephone interviews were conducted semiannually from 1989 to 1999 and biannually thereafter. The total cohort included 5888 participants. Two of the four CHS sites, the Pittsburgh, Pennsylvania, and Sacramento, California, centers, performed dual energy X-ray absorptiometry (DXA) scans on 1,591 participants during the year 7 visit (1994–1995) of CHS. A complete DXA dataset was available for 1,566 participants. Among these individuals, year 7 (1994–1995) plasma SDF-1 measures were available in 1,536 participants, forming our analysis cohort. The institutional review board (IRB) at each site approved the CHS methods, and all participants gave written informed consent. Augusta University’s Office of Human Research Protection Assurance approved the use of human plasma samples previously collected as part of the CHS.
SDF-1 Quantification
Total plasma levels of the most abundant form of human SDF-1, SDF-1α were assayed by ELISA in 1,536 participants’ plasma samples from the year 7 visit (1994–1995) as previously described [25]. Blood samples were collected in the presence of EDTA anticoagulant, and plasma was isolated. All plasma samples obtained from the NIH CHS study bank were de-identified and run in duplicate. Additionally, 3 separate control plasma samples with known quantities of SDF-1α (C1 1000, C2 2500 and C3 5000 pg/ml) were reconstituted, aliquoted, and stored frozen at −80 Celsius to assess coefficients of variation (CVs). All samples for the ELISAs to be run on one day (4 plates, 148 subject samples) were thawed on ice together along with the control plasma samples. A new vial of the SDF-1α standards was reconstituted for each plate and a dilution curve obtained per vendor instructions. The SDF-1α plasma levels were quantified using a sandwich ELISA kit (Quantikine Human CXCL12/SDF-1α Immunoassay, R & D Systems, Inc., Minneapolis, MN) according to the manufacturer’s protocol. All three SDF-1α control samples for each plate were within their acceptable ranges: low 1000 pg/ml (acceptable range = 728–1249 pg/ml), medium 2500 pg/ml (acceptable range = 2156–3432), and high 5000 pg/ml (acceptable range = 4412–6321) concentrations of human SDF-1α. The intra assay CVs were C1 6.1% (mean 859, SD 51 pg/ml), C2 3.7% (mean 2913, SD 109 pg/ml), and C3 2.3% (mean 6191, SD 164 pg/ml). The inter assay CVs were C1 10.5% (mean 819, SD 82 pg/ml), C2 7.2% (mean 2804, SD 203 pg/ml), and C3 8.3% (mean 6037, SD 499 pg/ml).
Bone Mineral Density and Body Composition
Total hip, femoral neck, lumbar spine, and total body BMD were measured in 1591 participants at the 1994–1995 study visits using Hologic QDR-2000 densitometers (Hologic, Inc., Waltham, MA) and read centrally at the University of California San Francisco reading center using Hologic software, version 7.10. All scans were completed using the array beam mode. Standardized positioning and use of QDR software was based on the manufacturer’s recommended protocol. Body composition measurements including total and percentage of lean and fat mass were also obtained from these densitometry scans [26].
Fracture Ascertainment
Incident (new) hip fractures were defined by a hospital discharge International Classification of Diseases, Ninth Revision (ICD-9), code of 820.xx. CHS prospectively obtained all hospitalization data, including discharge summaries, from participants every 6 months. These data were checked against Medicare claims data to identify any hospitalizations not reported by participants. Follow-up for incident hip fracture began at year 7 after the SDF-1α measurements and was continued to a hip fracture event, death, loss to follow-up, or June 30, 2013. Hip fractures caused by motor vehicle accidents or severe injury were excluded.
Covariates
Covariates were selected a priori based on associations with osteoporosis (BMD or fracture) from the year 7 data of CHS (same year as DXA studies and start of analysis). Age, race, and gender were determined by participant self-report. Body weight was measured using a calibrated balance beam scale. Height was measured with a wall-mounted stadiometer. Height and weight were used to calculate body mass index (kg/m2 [BMI]) and change in BMI. We chose to use BMI, instead of weight in these analyses, because we included multiple covariates in the final model. It has been reported that low weight is a better predictor of osteoporosis without other factors being considered, whereas BMI is a better predictor when multiple covariates are included [27]. CHS study sites were included as there may be unmeasured factors that are captured by different geographical regions that relate to osteoporosis risk; in support of this, it has been reported that there can be geographic heterogeneity in fracture incidence [28].
Current smoking history, alcohol use (0 drinks/week, 1–7 drinks/week, >7 drinks/week), and highest level of education achieved (≥ or <12th grade completed) were obtained by participant self-report. Level of education was considered as a surrogate for socioeconomic status, which may be associated with fracture risk [29]. Alcohol use was considered as present in women if there were at least 7 drinks/week and in men who drank at least 14 drinks/week. Prevalent cardiovascular disease (CHD) was defined as a history of angina, myocardial infarction, angioplasty, or coronary artery bypass graft. History of diabetes (use of insulin or oral hypoglycemic agents, non-fasting glucose ≥ 200, or fasting glucose level ≥ 126 mg/dL) was obtained. Both prevalent CHD and history of diabetes were adjudicated within CHS.
Renal function was assessed by cystatin C-based estimated glomerular filtration rate (eGFRcys). Use of selected medications [oral corticosteroids, cardiac medications angiotensin converting enzyme inhibitors (ACE), angiotensin-receptor blockers (ARBs), β-blockers, and diuretics (loop, thiazide, potassium sparing, combination)], opioids, sedative hypnotics (benzodiazepines and other sedatives/hypnotics), anticonvulsants/antidepressants, osteoporosis medications (estrogen, calcium and vitamin D supplements, SERMs, bisphosphonates, and calcitonin), diabetes medications, and proton pump inhibitors was ascertained from a review of prescription bottle labels by interviewers [30]. Self-reported health status (excellent/very good vs. good vs. fair/poor) was obtained [31]. Health was considered good if excellent/very good/good or not fair/poor. Frailty status [frail (defined as 3 or more of the following: unintentional loss of >10 pounds in past year, self-reported exhaustion, weak grip strength, slow walking speed, and low physical activity), intermediate (defined as 1 or 2 of the above criteria), or not frail] [32].
Statistical Analysis
Baseline participant characteristics across SDF-1α quartiles were described using linear trend tests for continuous variables and Chi-square tests for categorical variables. Linear regression analysis was used to estimate the association between measurements of body composition, BMD, and SDF-1α. Time to hip fracture event was calculated as the interval in years from the baseline visit in 1994/95 to the earliest date of first incident hip fracture, death, loss to follow-up, or end of follow-up on June 30, 2013. Cox proportional hazards models were used to estimate the hazard ratio (HR) of incident hip fracture associated with SDF-1α. We performed generalized additive models in both linear regression for BMDs and body composition measures and Cox regression for hip fracture with SDF-1α and found no departures from linearity. We considered 3 nested models: unadjusted models; models adjusted for age, race, clinic site, gender (minimally adjusted models); and fully adjusted models with age, race, clinic site, gender, smoking and alcohol use, BMI, change in BMI, frailty status, diabetes status, prevalent cardiovascular disease, self-reported health, renal function, and medication use.
Owing to differences in the natural history of, body composition between men, and women, in addition to analyzing men and women combined, we a priori stratified our analysis by gender. Analyses were conducted using R R Development Core Team (2016) [33].
Results
Participant Characteristics
Baseline characteristics of the study population by quartiles of SDF-1α are shown in Table 1. 42% of the population were men and 19% were African American. The mean age was 78 years, with a range of 67–97 years. Among the osteoporosis medications used, 8 individuals were taking bisphosphonates, 22 estrogen, and 9 a SERM. 16 persons were taking calcium supplements and 10 were taking vitamin D. None were taking calcitonin. These groups were not mutually exclusive; for example, a person might have taken both a bisphosphonate and a vitamin D supplement.
SDF-1α Association with Age, Gender, and Race
The mean SDF-1α was 2298 pg/ml, with a range of 1047–4760 pg/ml (See Table 1 for SDF-1 quartiles). SDF-1α plasma levels were significantly associated with increasing age (p < 0.01) and male gender (p = 0.04). On average, the SDF-1α level was 18 pg/ml higher for 1 year increase in age. SDF-1α levels were a mean of 48 pg/ml higher in males than females. SDF-1α was not significantly associated with race (p = 0.63).
SDF-1α Association with Bone Mineral Density
In multivariable-adjusted models including age, race, clinic site, gender, smoking, alcohol use, BMI, change in BMI over 2 years, frailty status, health status, prevalent cardiovascular disease, diabetes status, renal function, and medication use, higher SDF-1α levels were associated with lower total hip BMD (p = 0.02), and a trend for lower total body BMD (p = 0.07) and femoral neck BMD (p = 0.09), but not with lumbar spine BMD (p = 0.75) (Table 2). Results were similar for both women and men (data not shown).
SDF-1α Association with Body Composition
In multivariable-adjusted models, SDF-1α was significantly positively associated with total mass (p = 0.05), and total fat mass (p = 0.04), in men, and positively associated was percent lean (p = 0.04) and negatively associated with percent fat (p = 0.04) in women. (Tables 3, 4).
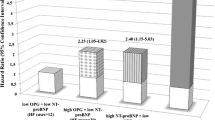
SDF-1α Association with Incident Hip Fracture
There were 169 hip fractures during a median of 11 years of follow-up, with an incidence rate of 1 hip fracture per 100 person-years of follow-up (95% CI 0.8, 1.2). Log rank test p-value across quartiles of SDF-1 revealed a p-value of 0.25. In multivariable-adjusted analyses, there was no significant association between SDF-1 concentrations and risk of incident hip fracture (Table 5).
Discussion
In elderly community dwelling men and women in the CHS, higher SDF-1α concentrations were associated with age and independent of age, with lower total hip BMD. In men, higher SDF-1α was associated with higher total body mass and percentage body fat, while in women, SDF-1 was positively related to percentage of lean mass and inversely related to the percentage of fat mass. There was no significant association of SDF-1α with incident hip fractures.
Blood levels of SDF-1α may represent a gestalt of overall CXCL121α expression and turnover, and our findings that hip BMD is inversely related to SDF-1α plasma concentrations suggest that increased plasma levels of SDF-1α, at least in older adults, are associated with osteoporosis. That older age and lower BMD are independently associated with higher SDF-1α concentrations in CHS patients is on the surface in conflict with observations that SDF-1 signaling is critical for osteogenesis and bone formation [7, 9]. However, little is known about the variation with age in the levels and bioactivity of the SDF-1 axis in the BM microenvironment relative to that seen in the peripheral circulation. There is evidence that the aged BM microenvironment suppresses the function of adult stem cells in bone formation [34], and while regulation of SDF-1 levels with age in the BM microenvironment is poorly understood, SDF-1 bioactivity appears to decrease with age in BM and in BMSCs [21, 22, 35]. The reason for the discrepant finding that SDF-1α is increased in the plasma in association with both higher age and lower BMD may be related to a number of potential mechanisms. For example, chronic elevation of plasma SDF-1 may induce mobilization of the BMSC population that is responsive to peripheral injury. Over time, this may deplete osteoprogenitor numbers in the BM akin to the proposed loss of endothelial progenitor cells with chronic increased circulating SDF-1 [20, 23]. Further, the percentage of SDF-1, that can activate CXCR4, drive osteogenesis, and maintain the BMSC population, as part of the total pool of circulating SDF-1 may decline with age relative to partially N-terminal degraded SDF-1 that is inactive or may have altered bioactivity [17, 18]. Additionally, there have been recent connections established between SDF-1, osteoclast recruitment, and function [36]; this may link increased circulating SDF-1 with increased bone resorption. However, the interactions of SDF-1 with osteoclast development and activity are complex and may depend on the local concentration of bioactive SDF-1, such that low levels of SDF-1 act on pre-osteoclasts to increase differentiated osteoclast activity, but higher levels of SDF-1 block this effect [37]. Distinguishing different post-translationally proteolytically processed forms of circulating SDF-1 from intact forms competent to activate receptors are challenging since the initial N-terminal cleaved SDF-1 isoforms are also detected by the antibodies used in SDF-1 ELISAs [17, 18]. Our finding that high plasma SDF-1α levels are associated with decreased total hip bone mineral density is novel and fits with the idea that the SDF-1 signaling axis is critical in bone homeostasis and that this may become dysfunctional with age. Assessment of SDF-1α plasma levels may potentially be useful as a biomarker for chronic bone disease and may provide a window into pathogenic bone changes.
Our findings that plasma SDF-1 levels were associated with body composition, in particular adipose tissue, in men fits well with the idea that adipose tissue in normal and obese states has differing interactions with SDF-1 expression and function [10–13, 38]. Again, this should be considered in the context that increased plasma SDF-1 levels may reflect increased levels of inactive or alternative bioactive SDF-1. Obesity is recognized as a low-grade chronic inflammatory state, which involves a chemokine network contributing to a variety of diseases. SDF-1 and its receptors have been reported to be expressed in both preadipocytes and adipocytes [11]. It also is tied to the localization of inflammatory regulator cells in peripheral tissues including adipose tissue [13, 39]. SDF-1 is involved in the development and progression of immune responses [40]. It serves as a recruiter for migration and trafficking of leukocytes and progenitor cells and is linked to infiltration of macrophages into adipose tissue in obesity [10, 39]. Adipose tissue itself in diet-induced obese mice is a source of SDF-1 that homes macrophages and is linked to increased pro-inflammatory factors [11, 12]. Treatment of obese mice with a CXCR4 antagonist reduces macrophage accumulation and production of pro-inflammatory cytokines in white adipose tissue (WAT) and improves systemic insulin sensitivity [39]. This may in part be related to a decrease in adipocyte CXCR4 expression with obesity and changes the tissues own responsiveness to SDF-1. Indeed, normally adipocyte CXCR4 activation limits the development of obesity by preventing excessive inflammatory cell recruitment into WAT and by supporting thermogenic activity of brown adipose tissue (BAT), but with a high-fat diet, CXCR4 is reduced and adipose tissue becomes a pro-inflammatory center and develops insulin resistance. Therefore, dysregulation of SDF-1 expression, its processing to non-functional or alternative function forms, and changes in its receptor number and function may link the SDF-1 axis with changes in stem cell mobilization and tissue composition. In contrast to our findings of an association of adipose body composition and SDF-1 in men, Kitahara et al. in a cross-sectional study of 1703 elderly men and women did not see an association of SDF-1 levels overall with BMI for either men or women [41]. However, the multiplex assay used by Kitahara et al. was less sensitive for SDF-1 quantification than the ELISA used here and measurements of body composition were not obtained [41]. Also, in contrast to our findings, in a small study looking at overweight adolescents with metabolic syndrome, Jung et al. saw an inverse relationship between waist circumference and plasma SDF-1 by ELISA [42]. This study utilized a vastly younger age group where both total SDF-1 levels and biologically active SDF-1 levels may also differ significantly.
While there was a slightly higher plasma SDF-1 level on average in men relative to women, both men and women showed similar associations of high SDF-1 levels with lower BMD. However, in contrast, there was an association between higher SDF-1 levels in men and greater adiposity, while the reverse appeared to be true in women. For men, this provides a possible linkage between obesity and decreased BMD via SDF-1. However, this does not hold true for older women, suggesting that there are gender differences in the relationship between adipose tissue and SDF-1 levels. This may be important in understanding differences in age-associated bone loss, and osteoporosis, in older post-menopausal women and similar aged men. As such, this supports understanding the role of SDF-1 expression, BMD and body composition in men and women at different ages and how menopause and different steroid hormones are involved. For example, we have identified age-associated epigenetic changes in human mesenchymal stem cells that target the SDF-1 axis, specifically in the microRNAs miRNA 29b-1-5p and miR-141 (unpublished data), which in turn are sensitive to estrogen inhibition [43].
There are a number of limitations to this study. We did not have information on clinical markers of inflammation. The number of individuals taking osteoporosis medications was too small to assess the association of specific medications on outcomes. Additionally, we did not have information on the length of therapy of osteoporosis medications. Cystatin C measurements were done in year 5 of CHS, which was 2 years prior to the SDF-1 measurements. Renal function may have changed over these 2 years that we would not have accounted for.
We did not have information on renal function in 106 of the participants; however, in a recent study determining, the relationship of plasma SDF-1 and cardiovascular outcomes in subjects with chronic kidney disease adjustment for eGFR did not change the association of SDF-1 levels with cardiovascular outcomes or age [19]. For hip fractures, we only had ICD-9 hospital discharge diagnoses and hip fractures were not further adjudicated in CHS. Additionally, the plasma was not collected in a fasting state, which can affect SDF-1 plasma levels [12]. We only measured the most abundant alternatively spliced variant of SDF-1, SDF-1α; however, other alternatively spliced forms such as SDF-1β can be found in plasma and may have different activity profiles [7]. We were also unable to distinguish total SDF-1 from bioactive SDF-1. Total plasma SDF-1 levels are relatively stable when collected within 30 to 90 min of a blood draw [25]; however, there is rapid degradation and inactivation of SDF-1 occurring probably within the first 5–10 min [16], leaving isoforms that are still detectable by standard ELISA, but the actual normal bioactivity of this pool of SDF-1 is lost [17, 18]. The question remains then, does our finding of an association of higher levels of total plasma SDF-1 with age represent more, or less, bioactive SDF-1 isoforms in circulation? In that the specific SDF-1 isoforms in circulation, and in different tissue compartments, may have specific bioactivities suggests that for future studies, it will be critical to collect blood samples with proteolytic inhibitors (e.g., to DPP4, MMPs, elastase, etc.) already in the collection tubes to prevent ongoing and post-collection proteolysis of SDF-1 and other plasma/serum components in order to “freeze” and accurately assess the in vivo sample isoform profile [44]. Importantly, assessment of these different types of SDF-1 isoforms is now technically possible with Immunoaffinity Enrichment and Tandem Mass Spectrometry analysis [18]. DXA scans were only done at one time period in CHS; thus, we were unable to determine the association of SDF-1 concentrations with changes in BMD or body composition. Finally, while there were significant associations of plasma SDF-1α levels with BMD, age, and for males, body composition, this is not proving cause and effect, and there may be other factors that are involved in the fat-bone axis [10–13].
Conclusions
Circulating plasma levels of SDF-1 are associated with lower total hip bone mineral density in both men and women. The relationship of SDF-1 to body composition differs by gender. These findings suggest that SDF-1 levels are linked to bone homeostasis in elderly men and women and provide the rationale for further assessment of the role of SDF-1 in osteoporosis and age-associated bone loss.
References
Shekelle P, Munjas B, Liu H, Wong E, Paige N, Goldzweig C, Zhou A, Suttorp M (2007) Screening men for osteoporosis: who & how [Internet]. VA evidence-based synthesis program reports. Department of Veterans Affairs (US, Washington (DC)
Conboy IM, Rando TA (2012) Heterochronic parabiosis for the study of the effects of aging on stem cells and their niches. Cell Cycle 11:2260–2267
Joiner DM, Tayim RJ, Kadado A, Goldstein SA (2012) Bone marrow stromal cells from aged male rats have delayed mineralization and reduced response to mechanical stimulation through nitric oxide and ERK1/2 signaling during osteogenic differentiation. Biogerontology 13:467–478
Veronesi F, Torricelli P, Borsari V, Tschon M, Rimondini L, Fini M (2011) Mesenchymal stem cells in the aging and osteoporotic population. Crit Rev Eukaryot Gene Expr 21:363–377
Christopher MJ, Liu F, Hilton MJ, Long F, Link DC (2009) Suppression of CXCL12 production by bone marrow osteoblasts is a common and critical pathway for cytokine-induced mobilization. Blood 114:1331–1339
Kortesidis A, Zannettino A, Isenmann S, Shi S, Lapidot T, Gronthos S (2005) Stromal-derived factor-1 promotes the growth, survival, and development of human bone marrow stromal stem cells. Blood 105:3793–3801
Herberg S, Fulzele S, Yang N, Shi X, Hess M, Periyasamy-Thandavan S, Hamrick MW, Isales CM, Hill WD (2013) Stromal cell-derived factor-1beta potentiates bone morphogenetic protein-2-stimulated osteoinduction of genetically engineered bone marrow-derived mesenchymal stem cells in vitro. Tissue Eng Part A 19:1–13
Herberg S, Shi X, Johnson MH, Hamrick MW, Isales CM, Hill WD (2013) Stromal cell-derived factor-1beta mediates cell survival through enhancing autophagy in bone marrow-derived mesenchymal stem cells. PLoS ONE 8:e58207
Herberg S, Susin C, Pelaez M, Howie RN, Moreno de Freitas R, Lee J, Cray JJ, Jr., Johnson MH, Elsalanty ME, Hamrick MW, Isales CM, Wikesjo UM, Hill WD (2014) Low-dose bone morphogenetic protein-2/stromal cell-derived factor-1beta cotherapy induces bone regeneration in critical-size rat calvarial defects. Tissue Eng Part A 20:1444–1453
Blogowski W, Serwin K, Budkowska M, Salata D, Dolegowska B, Lokaj M, Prowans P, Starzynska T (2012) Clinical analysis of systemic and adipose tissue levels of selected hormones/adipokines and stromal-derived factor-1. J Biol Regul Homeost Agents 26:607–615
Kabir SM, Lee ES, Son DS (2014) Chemokine network during adipogenesis in 3T3-L1 cells: differential response between growth and proinflammatory factor in preadipocytes vs. adipocytes. Adipocyte 3:97–106
Poon K, Barson JR, Ho HT, Leibowitz SF (2016) Relationship of the chemokine, CXCL12, to effects of dietary fat on feeding-related behaviors and hypothalamic neuropeptide systems. Front Behav Neurosci 10:51
Vangaveti VN, Rush C, Thomas L, Rasalam RR, Malabu UH, McCoombe SG, Kennedy RL (2014) Short-chain fatty acids increase expression and secretion of stromal cell-derived factor-1 in mouse and human pre-adipocytes. Hormones (Athens) 13:532–542
Nagasawa T (2014) CXC chemokine ligand 12 (CXCL12) and its receptor CXCR4. J Mol Med (Berl) 92:433–439
Antonsson B, De Lys P, Dechavanne V, Chevalet L, Boschert U (2010) In vivo processing of CXCL12 alpha/SDF-1 alpha after intravenous and subcutaneous administration to mice. Proteomics 10:4342–4351
De La Luz Sierra M, Yang F, Narazaki M, Salvucci O, Davis D, Yarchoan R, Zhang HH, Fales H, Tosato G (2004) Differential processing of stromal-derived factor-1alpha and stromal-derived factor-1beta explains functional diversity. Blood 103:2452–2459
Richter R, Jochheim-Richter A, Ciuculescu F, Kollar K, Seifried E, Forssmann U, Verzijl D, Smit MJ, Blanchet X, von Hundelshausen P, Weber C, Forssmann WG, Henschler R (2014) Identification and characterization of circulating variants of CXCL12 from human plasma: effects on chemotaxis and mobilization of hematopoietic stem and progenitor cells. Stem Cells Dev 23:1959–1974
Wang W, Choi BK K, Li W, Lao Z, Lee AYH, Souza SC, Yates NA, Kowalski T, Pocai A, Cohen LH (2014) Quantification of intact and truncated stromal cell-derived factor-1α in circulation by immunoaffinity enrichment and tandem mass spectrometry. J Am Soc Mass Spectrom 25:614–625
Mehta NN, Matthews GJ, Krishnamoorthy P, Shah R, McLaughlin C, Patel P, Budoff M, Chen J, Wolman M, Go A, He J, Kanetsky PA, Master SR, Rader DJ, Raj D, Gadegbeku CA, Shah R, Schreiber M, Fischer MJ, Townsend RR, Kusek J, Feldman HI, Foulkes AS, Reilly MP (2014) Higher plasma CXCL12 levels predict incident myocardial infarction and death in chronic kidney disease: findings from the chronic renal insufficiency cohort study. Eur Heart J 35:2115–2122
Xiao Q, Ye S, Oberhollenzer F, Mayr A, Jahangiri M, Willeit J, Kiechl S, Xu Q (2008) SDF1 gene variation is associated with circulating SDF1alpha level and endothelial progenitor cell number: the Bruneck Study. PLoS ONE 3:e4061
Guang LG, Boskey AL, Zhu W (2013) Age-related CXC chemokine receptor-4-deficiency impairs osteogenic differentiation potency of mouse bone marrow mesenchymal stromal stem cells. Int J Biochem Cell Biol 45:1813–1820
Subramanian S, Liu C, Aviv A, Ho JE, Courchesne P, Muntendam P, Larson MG, Cheng S, Wang TJ, Mehta NN, Levy D (2014) Stromal cell-derived factor 1 as a biomarker of heart failure and mortality risk. Arterioscler Thromb Vasc Biol 34:2100–2105
Jin CZ, Zhao Y, Zhang FJ, Yao HP, Wu LJ, Zhao HX, Wei HS, Wu NP (2009) Different plasma levels of interleukins and chemokines: comparison between children and adults with AIDS in China. Chin Med J (Engl) 122:530–535
Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A et al (1991) The cardiovascular health study: design and rationale. Ann Epidemiol 1:263–276
Kirkpatrick B, Nguyen L, Kondrikova G, Herberg S, Hill WD (2010) Stability of human stromal-derived factor-1alpha (CXCL12alpha) after blood sampling. Ann Clin Lab Sci 40:257–260
Mitchell D, Haan MN, Steinberg FM, Visser M (2003) Body composition in the elderly: the influence of nutritional factors and physical activity. J Nutr Health Aging 7:130–139
Kim SJ, Yang WG, Cho E, Park EC (2012) Relationship between weight, body mass index and bone mineral density of lumbar spine in women. J Bone Metab 19:95–102
Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC (2016) Epidemiology of fractures in the United Kingdom 1988–2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87:19–26
Reyes C, Garcia-Gil M, Elorza JM, Fina-Aviles F, Mendez-Boo L, Hermosilla E, Coma E, Carbonell C, Medina-Peralta M, Ramos R, Bolibar B, Diez-Perez A, Prieto-Alhambra D (2015) Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone 73:127–131
Psaty BM, Lee M, Savage PJ, Rutan GH, German PS, Lyles M (1992) Assessing the use of medications in the elderly: methods and initial experience in the cardiovascular health study. The cardiovascular health study collaborative research group. J Clin Epidemiol 45:683–692
Leavy B, Byberg L, Michaelsson K, Melhus H, Aberg AC (2015) The fall descriptions and health characteristics of older adults with hip fracture: a mixed methods study. BMC Geriatr 15:40
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-156
Core Team (2015) (2015) R: a language and environment for statistical computing. In, p R foundation for statistical computing, Vienna, Austria
Baker N, Boyette LB, Tuan RS (2015) Characterization of bone marrow-derived mesenchymal stem cells in aging. Bone 70:37–47
Choudhery MS, Khan M, Mahmood R, Mehmood A, Khan SN, Riazuddin S (2012) Bone marrow derived mesenchymal stem cells from aged mice have reduced wound healing, angiogenesis, proliferation and anti-apoptosis capabilities. Cell Biol Int 36:747–753
Ucer S, Iyer S, Kim HN, Han L, Rutlen C, Allison K, Thostenson JD, de Cabo R, Jilka RL, O’Brien C, Almeida M, Manolagas SC (2016) The effects of aging and sex steroid deficiency on the murine skeleton are independent and mechanistically distinct. J Bone Miner Res
Wright LM, Maloney W, Yu X, Kindle L, Collin-Osdoby P, Osdoby P (2005) Stromal cell-derived factor-1 binding to its chemokine receptor CXCR4 on precursor cells promotes the chemotactic recruitment, development and survival of human osteoclasts. Bone 36:840–853
Fenton JI, Nunez NP, Yakar S, Perkins SN, Hord NG, Hursting SD (2009) Diet-induced adiposity alters the serum profile of inflammation in C57BL/6 N mice as measured by antibody array. Diabetes Obes Metab 11:343–354
Kim D, Kim J, Yoon JH, Ghim J, Yea K, Song P, Park S, Lee A, Hong CP, Jang MS, Kwon Y, Park S, Jang MH, Berggren PO, Suh PG, Ryu SH (2014) CXCL12 secreted from adipose tissue recruits macrophages and induces insulin resistance in mice. Diabetologia 57:1456–1465
Karimabad MN, Hassanshahi G (2015) Significance of CXCL12 in type 2 diabetes mellitus and its associated complications. Inflammation 38:710–717
Kitahara CM, Trabert B, Katki HA, Chaturvedi AK, Kemp TJ, Pinto LA, Moore SC, Purdue MP, Wentzensen N, Hildesheim A, Shiels MS (2014) Body mass index, physical activity, and serum markers of inflammation, immunity, and insulin resistance. Cancer Epidemiol Biomarkers Prev 23:2840–2849
Jung C, Fischer N, Fritzenwanger M, Pernow J, Brehm BR, Figulla HR (2009) Association of waist circumference, traditional cardiovascular risk factors, and stromal-derived factor-1 in adolescents. Pediatr Diab 10:329–335
Klinge CM (2015) miRNAs regulated by estrogens, tamoxifen, and endocrine disruptors and their downstream gene targets. Mol Cell Endocrinol 418 Pt 3:273–297
Baerts L, Waumans Y, Brandt I, Jungraithmayr W, Van der Veken P, Vanderheyden M, De Meester I (2015) Circulating stromal cell-derived Factor 1alpha levels in heart failure: a matter of proper sampling. PLoS ONE 10:e0141408
Acknowledgements
This work was supported by contracts and awards to the Cardiovascular Health Study (CHS) from the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute (NHLBI) with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS) including contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC55222N01HC85080, N01HC85081, N01HC85082, N01HC85083, and N01HC85086, and grants HL094555 and 080295; additional support provided by R01AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org. Additional support was provided by P01AG036675 from the NIA (WDH/MWH), the Augusta University Pilot Study Research Program (WDH/LC), and by 1I01CX000930 from the Department of Veterans Affairs (WDH). The contents of this publication do not represent the views of the Department of Veterans Affairs or the United States Government.
Authors’ Roles
LDC: conceiving and designing the study, interpretation of the data, and drafting of the manuscript. PB: statistical analyses and critical review of the manuscript. HAF: critical review of the manuscript, designing the study, and interpretation of the data. JAR: designing the study, interpretation of the data, critical review of the manuscript, and funding support. MB: interpretation of the data and critical review of the manuscript. MWH: critical review of the manuscript and interpretation of data. WDH: conceiving and designing the study, interpretation of the data, performance of SDF-1 laboratory measurements, and critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Laura D. Carbone, Petra Bůžková, Howard A. Fink, John A. Robbins, Monique Bethel, Mark W. Hamrick and William D. Hill declare that they have no conflict of interest.
Disclosures
William Hill has received a Utility Patent. GRU OTT 2013-26 U.S.S.N. 61/712/708 filed 2-22-2013. Publication# US-2014-0288010-A1. The application was published on September 25, 2014. “Compositions and Methods for Increasing Stem Cell Survival” By William D. Hill, Samuel Herberg, & Sudharsan Periyasami-Thandavan. Describing SDF-1’s role in enhancing BMSC autophagy and blocking apoptosis and potential clinical applications, and including inhibition of DPP4 to enhance SDF-1 activity levels.
Human and animal rights and Informed consent
The institutional review board (IRB) at each site approved the CHS methods, and all participants gave written informed consent. Augusta University’s Office of Human Research Protection Assurance approved the use of human plasma samples previously collected as part of the CHS. No animals were used.
Rights and permissions
About this article
Cite this article
Carbone, L.D., Bůžková, P., Fink, H.A. et al. Association of Plasma SDF-1 with Bone Mineral Density, Body Composition, and Hip Fractures in Older Adults: The Cardiovascular Health Study. Calcif Tissue Int 100, 599–608 (2017). https://doi.org/10.1007/s00223-017-0245-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0245-8