Abstract
Purpose
The aim of the present study was to evaluate the clinical, radiological and functional results of patients underwent single-tunnel (ST) and double-tunnel (DT) medial patellofemoral ligament(MPFL) reconstructions with hamstring autograft following recurrent patella dislocation prospectively in a single institution.
Methods
From 2013 to 2017, 80 patients with symptomatic recurrent patellar dislocation or instability were randomly divided into 2 groups for MPFL reconstruction with ST technique or DT technique and evaluated prospectively. In the ST group, there were 20 male and 20 female with a median follow-up of 46.5 months (range 24–74). The median age was 15 years (range 10–28). In the DT group, there were 18 male and 22 female with a median follow-up of 40 months (range 24–74). The median age was 19 years (range 14–29). Clinical scores (Kujala score, Lysholm score, Tegner score and IKDC score) and radiological measurements (congruence angle and patellar tilt angle) of the patients were evaluated preoperatively and at postoperative 24th month. Isokinetic dynamometric tests were performed at postoperative 24th month and the difference between the operated leg and the non-operated leg was found as a percentage deficit.
Results
There were no postoperative complications, redislocation or subluxation in any patient. Kujala, Lysholm, Tegner and IKDC scores were better and statistically significant postoperatively in both groups (p < 0.05). However, there was no statistically significant difference between the groups (n.s.). The congruence angle and patellar tilt angle were found to be returned to normal values postoperatively, but there was no statistically significant difference between the groups (n.s.). There was no statistically significant difference between the two groups in isokinetic dynamometric tests performed as 60° flexion, 60° extension, 180° flexion and 180° extension (n.s.).
Conclusion
The present study is the first that compared the clinical, radiological and functional results of the ST and DT techniques to date. Regardless of the number of the tunnels, similar results were obtained in ST and DT reconstruction using transpatellar tunnel technique.
Level of evidence
Level I.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Patellar instability is a common problem with a prevalence of 6-77/100,000 [13]. The cause of recurrent patellar dislocation (RPD) is multifactorial, primarily due to changes in the joint geometry (trochlear dysplasia), rotational deformity, patellar height and ligamentous laxity [21]. However, failure of the medial patellofemoral ligament (MPFL) has been defined as the main reason for RPD [3].
The MPFL, which prevents lateral dislocation of the patella and provides approximately 60% restraining force, is the most important soft tissue restrictor [10]. Injury is almost always seen after the first dislocation [23]. Magnetic resonance imaging (MRI) studies and emergency surgery explorations performed to knees with acute patellar dislocation have shown MPFL injury in almost 100% of these patients [34]. After the first dislocation, the risk of recurrence is relatively high, and approximately half of patients experience recurrent dislocations. Since patellar instability recurrence occurs at rates of up to 50% following conservative treatment, surgical treatment is the preferred method in patients with RPD [33]. Although there are many surgical methods for recurrent patellar instability, optimal surgical treatment is still controversial. The most recent systematic studies have shown that MPFL reconstruction is an effective procedure providing good functional and subjective results with low recurrence of patellar instability [12]. Various MPFL reconstruction techniques have been described. In addition, there are several options for graft selection, patellar and femoral fixation. Although each has its own advantages and disadvantages, sufficient evidence has not been found about their superiority over each other [18]. In a biomechanical study, it was shown that tunnel reconstruction is stronger than other techniques, has better structural features, and there were no statistically significant difference with native MPFL [21]. The number of studies evaluating the double-tunnel (DT) and single-tunnel (ST) techniques are limited. In two biomechanical studies, it was found that both ST and DT techniques have similar stiffness, ultimate load and elongation, and absorbed energy [9, 26]. In addition, the DT technique has been shown to have a higher risk of patellar fracture [8, 11]. Kang et al. addressed that MPFL has two bundles consisting superior-oblique and inferior-straight bundles [15]. For this reason, many authors argued that double bundle (DB) MPFL reconstruction restores the fan-shape of MPFL and is better in terms of biomechanical and clinical results than single bundle (SB) MPFL reconstruction [20, 26, 36]. However, in a recent systematic review, the results have found similar and there were no significant difference in terms of knee function, recurrent subluxation and complications in both SB and DB MPFL reconstruction [14].
There is not enough study to evaluate the results of ST and DT techniques and their superiority to each other is still unknown. The aim of the present study was to evaluate the clinical, radiological and functional results of patients underwent ST and DT MPFL reconstructions with hamstring autograft following RPD. The hypothesis of the study was that there would be no difference between clinical, radiological and functional results in both ST and DT MPFL reconstruction since we used transpatellar tunnel technique in both techniques. The present study is the first that compared the clinical, radiological and functional results of the ST and DT techniques to date.
Materials and methods
This was a prospective, randomized, controlled study. Institutional Review Board (IRB) approval was obtained from the Ethics Committee of Ankara University School of Medicine under the decision number (06-365-18) and all patients provided written informed consent. From a total of 113 patients with symptomatic RPD or instability treated between 2013 and 2017, 80 patients who met the study inclusion criteria were randomly assigned via a computer random generator (http:// www.randomizer.org) to one of two different treatment groups using blocks of 10 with an allocation ratio of 1:1. Sequentially numbered sealed opaque envelopes were used to conceal the allocation. 40 patients underwent single tunnel-MPFL reconstruction and 40 patients underwent double-tunnel MPFL reconstruction. All patients were followed-up for at least 2 years.
All the patients had recurrent patellar instability. Symptomatic RPD or instability was evaluated as at least two patellar dislocations or persistent patellar instability for more than 3 months following the first dislocation despite conservative treatment including isometric quadriceps exercises, straight leg raises, and strengthening exercises providing vastus medialis obliquus (VMO) stimulation [22]. Radiographs (AP, lateral and Merchant views of the injured knee), computed tomography (CT) and MRI were performed to all the patients. Inclusion criteria were (1) at least two patellar dislocations or patellar instability symptoms (pain, subluxation, or both) continuing for more than 3 months after the first dislocation, (2) positive patellar apprehension test, (3) MPFL laxity on CT showing patellar external overflow, and (4) failure of conservative treatment. Exclusion criteria were (1) previous knee surgery, (2) Q angle > 20° in females and > 17° in males, (3) greater trochlear angle > 145°, tuberositas tibia- trochlear groove (TT–TG) distance ≥ 20 mm, (5) patella alta (Insall-Salvati index > 1.2), (6) concomitant other ligament injuries. To ensure homogeneity of the groups, 33 patients who met these criteria and therefore required distal alignment corrective surgical procedures were excluded from the study.
Surgical technique
All the operations were performed by a single surgeon. With the patient in a supine position, prophylactic antibiotic was administered then a tourniquet was applied to the thigh. The leg was stained and draped in standard surgical manner. The patient was examined under anesthesia to confirm the diagnosis and to evaluate the degree of instability. Lateral retinacular release was not performed to any patient. Diagnostic arthroscopy was performed and associated intra-articular injuries were recorded. During arthroscopy, the position of the patella relative to the trochlea was evaluated, while the knee was fully extended. If the patella did not overlap the trochlea (< 50% overlap with trochlea), patellar subluxation diagnosis was confirmed [32]. Since there is a need for a longer graft in the reconstruction with transpatellar technique, MPFL reconstruction was performed to all the patients (both single and double-tunnel) using ipsilateral semitendinosus tendon autograft. The semitendinosus tendon was harvested in a usual fashion [7].
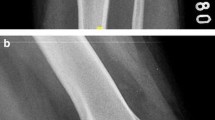
Reconstruction with a single tunnel
A single, 3–4 cm longitudinal incision was made between the medial side of the patella and the adductor tubercle. After opening the superficial fascia, the fan-shaped MPFL was identified on the proximal two-thirds of the patella [1]. Then, a single tunnel was drilled, starting from the midpoint of the medial border, without damaging the chondral surfaces and the anterior cortex. To determine the correct femoral MPFL entry site, the radiographic method was used as described by Schöttle (Fig. 1) [31]. Then, a half tunnel was drilled in the Schöttle point. The graft was passed through the patellar tunnel and pulled back over the anterior surface of the patella (Fig. 2). Both graft ends were transferred to the femoral side between fascial and capsular part of the medial retinaculum [39]. The free graft ends were fixated to the opened tunnel in Schöttle point of the femur with a bioabsorbable BioRCI interference screw (Smith & Nephew Endoscopy, Andover, MA, USA) in approximately 30° of knee flexion and in a suitable tensioning force. During the procedure position of the patella, graft tension and patellar trajectory with flexion extension movements were checked arthroscopically.
Reconstruction with a double tunnel
As in reconstruction with a ST, we used the same single incision and approach. Double tunnel which separated by a 1 cm bone bridge were drilled, from the upper half of the patella. The tendon graft was passed through the parallel tunnels in a looped fashion (Fig. 3) [8]. The fixation method of the femoral side was performed as in the ST reconstruction in approximately 30° of knee flexion and was checked arthroscopically during the procedure.
Postoperative physical therapy and rehabilitation program
Following MPFL reconstruction, the same physical therapy and rehabilitation protocol was applied to all patients by the same team. Active and passive assisted full range of knee motion was started the day after MPFL reconstruction. Weight bearing was gradually increased to full at 3 weeks postoperatively. Jogging was permitted 3 months after reconstruction. Return to sports was allowed 6 months postoperatively, following an evaluation of muscle strength.
Evaluations
All the patients were evaluated preoperatively and at the postoperative 24th month with the Kujala score, the IKDC subjective score, the Lysholm score, the Tegner activity score and the radiographs taken. Lateral radiographic view for Insall-Salvati Index, Merchant radiographic view for congruence and patellar tilt angle, CT for TT–TG distance, Q and trochlear angle, MRI for MPFL injuries and other intra-articular lesions were evaluated. All radiographs were measured twice at an interval of 3 weeks by two orthopedic surgeons to determine intra-observer and inter-observer reliabilities of the radiographic assessments. Intra-class correlation coefficients (ICC) were calculated for intra-observer and inter-observer reliabilities of all measurements. Intra-observer ICCs for each observer were 0.94 and 0.93 and interrater ICC was 0.91. The average values of two separate measurements taken by a single investigator were used in the analyses since these results showed that the reliability of the measurement was excellent according to the criteria of Winer [37].
Isokinetic strength test
Isokinetic data were obtained with an IsoMed 2000 dynamometer (D&R Ferstl GmbH, Hemau, Germany) at the postoperative 24th month. The muscle strength measurement was taken with 6 repetitions at 60°/s angular rate and 12 repetitions at 180°/s in both knees for separate evaluation of hamstring activation (knee flexion) and quadriceps activation (knee extension). The results of the operated side were compared with those of the non-operated side and the percentage deficit was recorded. All the calibrations and all the tests were applied by the same operator.
Statistical analysis
An a priori power analysis was performed using G-Power 3.1.7 (Kiel University, Kiel, Germany). The estimated sample size was predicted as minimum 33 patients in each group with significance level (alpha) of 0.05 and power (1-beta) of 0.95. Data obtained in the study were analyzed statistically using SPSS version 22.0 software (IBM Corp., Armonk, NY, USA). Conformity of the data to normal distribution was tested. In the comparisons, the t test was applied to data showing normal distribution and the Mann–Whitney U test was applied to data not showing normal distribution. In the comparison of two groups of nominal variables, the Chi-square test was used. In the comparison of two groups of time-dependent measurements, variance analysis and the Friedman test were used. A value of p < 0.05 was accepted as statistically significant.
Results
All the postoperative evaluations were made by the same surgeon. No infection, chronic effusion, synovitis or patellar fracture was observed in any patient during the follow-up period. No patellar redislocation or subluxation was observed in any patient and all the patients were seen to have regained full ROM.
There were 20 males and 20 females with a median age of 15 years (range 10–28), a median duration of symptoms of 5.5 months (range 1–47) and a median follow-up period of 46.5 months (range 24–74) in the ST MPFL reconstruction group. There were 18 males and 22 females with a median age of 19 years (range 14–29), a median duration of symptoms of 7 months (range 1–120) and a median follow-up period of 40 months (range 24–74) in the DT MPFL reconstruction group.
The demographic characteristics of the patients are shown in Table 1.
Clinical results
Results of the clinical scores (Kujala, Lysholm, Tegner and IKDC) for ST and DT groups are shown in Table 2. The scores in both groups were determined to have statistically significant increase at 24th month postoperatively compared to the preoperative values (p < 0.05). No statistically significant difference was found between the groups (n.s.). When the group–time interaction was examined, the effects of time on the measurements were similar in both groups, with no statistically significant difference (n.s.) (Fig. 4).
Radiological results
Results of the radiological measurements (congruence angle and the patellar tilt angle) for ST and DT groups are shown in Table 3. In the postoperative period, the congruence angle and the patellar tilt angle in both groups returned to normal values and the change was found to be statistically significant (p < 0.05). No statistically significant difference was found between the groups (n.s.) (Fig. 5).
Functional results
At the postoperative 24th month follow-up examination, the difference of muscle strength was compared between the two extremities in the isokinetic dynamometric strength tests at 60° flexion, 180° flexion, 60° extension and 180° extension. Isokinetic functional results are shown in Table 4. No statistically significant difference was found between the groups in respect of the deficit in these four functions (n.s.) (Fig. 6).
Discussion
The most important finding of this study was that there was no significant difference between the patients who underwent ST or DT MPFL reconstruction in respect to clinical, radiological and functional results. The number of tunnels opened was not seen to have any effect on the knee functions of the patients.
Recurrent patellar instability occurs as a result of abnormal movement of the patella in the trochlea during the functional movement range because of a multifactorial mechanism [2]. Treatment aims to correct underlying abnormalities [6]. There are many surgical treatments for recurrent patellar instability but the optimal surgical treatment is a matter of debate. By improving clinical results, MPFL reconstruction is an effective method to regain patellar anatomy and function [27]. Nevertheless, debate continues on the subject of graft and surgical technique selection. Several reconstruction procedures have been described [16].
Transpatellar tunnel technique was preferred for both ST and DT MPFL reconstruction since in a recent biomechanical study demonstrated that suture anchor reconstruction was significantly weaker than the native MPFL and tunnel technique had the similar strength with native MPFL. This was shown as evidence not to use other reconstruction techniques, especially direct sutures or anchor fixation, which have been reported as the weakest repair [21].
In the present study, it was found that there were no significant differences in terms of Kujala, Lysholm, Tegner and IKDC scores between the ST and DT groups. In a study which compared SB and DB MPFL reconstructions using single and double patellar tunnel fixations, respectively, the DB group was found to have better functional results especially in the long term. Patellar instability was found 26.9% in the SB group and 4.5% the DB group [35]. In another study, DB group had significantly higher postoperative Kujala and IKDC scores compared to SB group. But postoperative Lysholm and Tegner scores were not significantly different [17]. On the contrary, Kang et al. found that there were no significant differences in terms of knee function, recurrent subluxation or dislocation and complications in 1,063 patients underwent SB and DB MPFL reconstruction [14]. Similarly, in another study, there were no significant differences between SB and DB groups in Kujala, Fulkerson and SF-36 questionnaire scores postoperatively at long-term follow-up [4]. This shows that both ST and DT techniques have similar improvements in knee function.
Radiological measurements were found to be significantly improved postoperatively in both groups and there were no significant differences both in congruence and patellar tilt angles between groups. Li et al. showed similar results except for patellar tilt angle in a study that compared SB and DB reconstruction. DB group showed a significantly decreased patellar tilt angle [17].
The present study showed that when the mean strength values were examined, with the exception of the ST 180˚ flexion strength, the operated side was seen to have lost strength compared to the non-operated side in both ST and DT groups. Isokinetic test results following MPFL reconstruction are limited. Ronga et al. evaluated isokinetic data at mean 3.1 years after isolated MPFL reconstruction, and all the data of the operated extremity were found to be consistently weaker compared to the non-operated extremity [28]. Oliva et al. found similar findings in skeletally immature patients [24]. Unlike these previous findings, it was seen that in some patients the operated side had the same strength as the non-operated side and in some cases there were better results. Nevertheless, there were no significant differences between the groups.
The semitendinosus graft was used, especially in patients who underwent double-tunnel reconstruction, to obtain appropriate length in the present study. In a recent study, it was shown that semitendinosus graft had better scores than gracilis tendon graft [19]. In a recent study by Yoo et al. based on CT analysis, the best angle for MPFL reconstruction was shown to be approximately 30° knee flexion [38]. This supports the decision in the present study for fixation of the graft at approximately 30°.
The ST and DT reconstruction methods have some common advantages. Due to the transpatellar tunnel technique, there is no need for the use of additional material for patellar fixation and anatomic healing would be more rapid. Although reported in other studies, there was no case of patellar fracture in the present study [8, 30]. Because of the two tunnels in the DT technique, the risk of patellar fracture is greater than the ST technique. Therefore, as there was no difference between the two groups in the present study, it may be more appropriate to perform MPFL reconstruction with a ST technique to minimize the risk of fracture.
The present study has several limitations. First, there were no preoperative isokinetic strength data and evaluation of generalized ligamentous laxity. Permission was not granted by the Ethics Committee to perform preoperative muscle strength tests on patients with recurrent patellar dislocation, since it was thought that performing the test on the injured knee would have required extra effort and would have damaged the tissues more. Furthermore, postoperative joint effusion of the knee may limit the value of such data by reducing the isokinetic and isometric muscle strength of the vastus medialis and lateralis muscles [25]. Although Runow showed that there was a relationship between patellar dislocation and hyperlaxity, Atkin et al. found that there was no relationship between unilateral patellar dislocation and hyperlaxity [5, 29]. Second, more sophisticated radiological evaluations of limb-length alignment and the angular and rotational profile of the lower extremity and knee was not performed. It was considered inappropriate to over-investigate these patients since radiographs (AP, lateral and Merchant views of the injured knee), CT and MRI were already performed.
To date, the superiority of ST and DT techniques to each other in MPFL reconstruction remains unclear. The present study showed that both techniques had similar clinical, radiological and functional results. This should be considered when selecting the ST or DT techniques for MPFL reconstruction in clinical practice. Based on the current study findings, the feasibility and encouraging results confirm the application of ST technique in the day-by day clinical work.
Conclusion
The present study is the first that compared the clinical, radiological and functional results of the ST and DT techniques to date. Regardless of the number of the tunnels similar results were obtained in ST and DT reconstruction using transpatellar tunnel technique. Unlike previous studies, the present study shows that ST technique seems to be a good alternative of DT technique.
References
Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB (2017) Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc 25(12):3755–3772
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15(2):48–56
Andrish J (2008) The management of recurrent patellar dislocation. Orthop Clin North Am 39(3):313–327
Astur DC, Gouveia GB, de Souza Borges JH, Astur N, Arliani GG, Kaleka CC, Cohen M (2015) Medial patellofemoral ligament reconstruction: a longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J 9:198–203
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28(4):472–479
Bicos J, Fulkerson JP, Amis A (2007) Current concepts review: the medial patellofemoral ligament. Am J Sports Med 35(3):484–492
Charalambous CP, Kwaees TA (2012) Anatomical considerations in hamstring tendon harvesting for anterior cruciate ligament reconstruction. Muscles Ligaments Tendons J 2(4):253–257
Christiansen SE, Jacobsen BW, Lund B, Lind M (2008) Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 24(1):82–87
Criscenti G, De Maria C, Sebastiani E, Tei M, Placella G, Speziali A, Vozzi G, Cerulli G (2016) Reconstruction of medial patello-femoral ligament: Comparison of two surgical techniques. J Mech Behav Biomed Mater 59:272–278
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Dhinsa BS, Bhamra JS, James C, Dunnet W, Zahn H (2013) Patella fracture after medial patellofemoral ligament reconstruction using suture anchors. Knee 20(6):605–608
Fisher B, Nyland J, Brand E, Curtin B (2010) Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy 26(10):1384–1394
Fithian DC, Paxton EW, Lou SM, Silva P, Davis DK, Elias DA, White LM (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32(5):1114–1121
Kang H, Zheng R, Dai Y, Lu J, Wang F (2019) Single-and double-bundle medial patellofemoral ligament reconstruction procedures result in similar recurrent dislocation rates and improvements in knee function: a systematic review. Knee Surg Sports Traumatol Arthrosc 27(3):827–836
Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB (2010) Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 18(11):1511–1516
Lee D-Y, Park Y-J, Song S-Y, Hwang S-C, Park J-S, Kang D-G (2018) Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy 34(11):3082–3093
Li J, Li Z, Wang K, Liu C, Wang Y, Wang H (2019) Medial patellofemoral ligament reconstruction: a comparison of single-bundle transpatellar tunnel and double-anchor anatomic techniques for the treatment of recurrent lateral patellar dislocation in adults. Arthroscopy 35(3):845–854
McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC (2018) Graft choice in isolated medial patellofemoral ligament reconstruction: a systematic review with meta-analysis of rates of recurrent instability and patient reported outcomes for autograft, allograft, and synthetic options. Arthroscopy 34(4):1340–1354
Migliorini F, Trivellas A, Driessen A, Quack V, Tingart M, Eschweiler J (2020) Graft choice for isolated MPFL reconstruction: gracilis versus semitendinosus. Eur J Orthop Surg Traumatol 30(5):763–770
Mohammed R, Hunt N, Gibbon AJ (2017) Patellar complications in single versus double tunnel medial patellofemoral ligament reconstruction. J Orthop Surg (Hong Kong) 25(1):1–4
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Jt Surg Br 87(1):36–40
Nomura E (1999) Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop 23(5):260–263
Nomura E, Horiuchi Y, Inoue M (2002) Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee 9(2):139–143
Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N (2009) The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med 37(9):1814–1820
Palmieri-Smith RM, Kreinbrink J, Ashton-Miller JA, Wojtys EM (2007) Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med 35(8):1269–1275
Placella G, Speziali A, Sebastiani E, Morello S, Tei MM, Cerulli G (2016) Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single bundle technique. Musculoskelet Surg 100(2):103–107
Previtali D, Milev SR, Pagliazzi G, Filardo G, Zaffagnini S, Candrian C (2020) Recurrent patellar dislocations without untreated predisposing factors: medial patellofemoral ligament reconstruction versus other medial soft-tissue surgical techniques—a meta-analysis. Arthroscopy 36(6):1725–1734
Ronga M, Oliva F, Giuseppe Longo U, Testa V, Capasso G, Maffulli N (2009) Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 37(9):1735–1742
Rünow A (1983) The dislocating patella: Etiology and prognosis in relation to generaked joint laxity and anatomy of the patellar articulation. Acta Orthop Scand Suppl 201:1–53
Schiphouwer L, Rood A, Tigchelaar S, Koëter S (2017) Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc 25(1):245–250
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Smith C, Otte J, Steensen R (2018) Empty sunrise sign: an arthroscopic finding in recurrent patellar dislocation. J Knee Surg 33(1):89–93
Smith TO, Song F, Donell ST, Hing CB (2011) Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 19(6):988–998
Spritzer CE, Courneya DL, Burk DL Jr, Garrett WE, Strong JA (1997) Medial retinacular complex injury in acute patellar dislocation: MR findings and surgical implications. AJR Am J Roentgenol 168(1):117–122
Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, Wang J (2013) Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop 37(4):617–624
Wang Q, Huang W, Cai D, Huang H (2017) Biomechanical comparison of single-and double-bundle medial patellofemoral ligament reconstruction. J Orthop Surg Res 12(1):29
Winer BJ (1971) Statistical principles in experimental design, 2ndd edn. McGraw-Hill, New York, pp 283–293
Yoo Y-S, Chang HG, Seo Y-J, Byun JC, Lee GK, Im H, Song SY (2012) Changes in the length of the medial patellofemoral ligament: an in vivo analysis using 3-dimensional computed tomography. Am J Sports Med 40(9):2142–2148
Zhao J, Huangfu X, He Y (2012) The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med 40(6):1355–1364
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Funding
No funding to declare.
Ethical approval
Institutional Review Board (IRB) approval was obtained from Ankara University School of Medicine Ethics Committee under the decision number (06-365-18).
Informed consent
All patients provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ercan, N., Akmese, R. & Ulusoy, B. Single-tunnel and double-tunnel medial patellofemoral ligament reconstructions have similar clinical, radiological and functional results. Knee Surg Sports Traumatol Arthrosc 29, 1904–1912 (2021). https://doi.org/10.1007/s00167-020-06260-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06260-6