Abstract
The purpose of this study was to explore the anatomy and evaluate the function of the medial patellofemoral ligament (MPFL). Anatomical dissection was performed on 12 fresh-frozen knee specimens. The MPFL is a condensation of capsular fibers, which originates at the medial femoral condyle. It runs transversely and inserts to the medial edge of the patella. With the landmark of the medial femur epicondyle (MFE), the femoral origination was located: just 8.90 ± 3.27 mm proximally and 13.47 ± 3.68 mm posteriorly to the MFE. The most interesting finding in present study was functional bundles of its patellar insertion. Approximately from the femoral origination point, fibers of the MPFL form two relatively concentrated fiber bundles: the inferior-straight bundle and the superior-oblique bundle. The whole length of each was 71.78 ± 5.51 and 73.67 ± 5.40 mm, respectively. The included angle between bundles was 15.1° ± 2.1°. Although the superior-oblique bundle and the inferior-straight bundle run on the patellar MPFL inferiorly and superiorly, respectively, as their name indicates, the two bundles are not entirely separated, which make MPFL one intact structure. The inferior-straight bundle is the main static soft tissue restraints where the superior-oblique bundle associated with vastus medialis obliquus (VMO) is to serve as the main dynamic soft tissue restraints. So this finding may provide the theoretical foundation for the anatomical reconstruction of the MPFL and shed lights on the future researchers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellar dislocation remains a common but challenging treatment problem for an orthopedic surgeon. In most cases, medial patellofemoral ligament (MPFL) is found to become loose or torn, especially in the cases without the bone abnormalities [1, 3, 20, 21, 23]. Biomechanics studies have confirmed that the MPFL is the major soft tissue stabilizer in preventing lateral subluxation or dislocation of the patella [6, 8]. Therefore, the reconstruction of the MPFL might be an effective way to restore normal peripatellar anatomy and its function. Initial outcomes have been encouraging, with good to excellent clinical results in up to 96% of cases at the mid-term follow-up [14]. Sandmeier et al. [19] and David et al. [7] reported, however, the reconstruction of the MPFL alone was not able to restore normal patellar tracking from mid to deep flexion of the knee. Failure to restore proper anatomy or isometry of the MPFL may account for this issue and ultimately limit the long-term success of such reconstruction.
In 1957, Kaplan [12] first described the MPFL as the transverse reinforcement between the base of the patella and the tendon of the medial head of the gastrocnemius. Since then, many authors [7, 20] have described the MPFL as a distinct structure in the second layer of the medial soft tissues above the knee coursing from the medial femoral epicondyle to the supra-medial two-thirds of the patella. In addition, Nomura et al. [16] specially dissected the femoral attachment; however, anatomical reconstruction of the MPFL deals with not only the femoral insertion, but also the insertion to the medial border of the patella is important. Despite the fact that some authors [7, 15] demonstrated the anatomical reconstruction procedure to restore a triangular form of the MPFL, detailed information about the patellar insertion is not addressed enough.
The purpose of the present study was to describe the anatomic structure of the MPFL, in particular of its patellar attachment and relationship with the neighboring soft tissue and to improve clinical outcome of anatomical reconstruction of MPFL.
Materials and methods
Twelve knees (5 left and 7 right) from 7 (5 men and 2 women) fresh-frozen cadavers in the department of anatomy of Hebei Medical University were dissected in the present study with the approval for the study by the Academic Ethics Committee of Hebei Medical University. The specimens were frozen at −21°C and thawed to room temperature the night prior to dissection. The mean age was 50 years (range from 30 to 65). The cause of death is unknown, but all knees especially medial surfaces were intact and did not have indication of injury. No scar tissue was found during the dissection procedure.
The skin and subcutaneous tissue of the medial side of the knee were removed, and the distal insertion of the vastus medialis obliquus (VMO) and its muscle belly were entirely exposed. Along the inferior border of the VMO, dissection was performed until the upper margin of MPFL was fully exposed. The soft tissue over the MPFL was blunt dissected and removed, where the VMO, combined with the tendon of adductor magnus (TAM), served as reference to identify and dissect the MPFL. With a forceps under the MPFL, the femoral attachment and patellar insertion were blunt identified and dissected.
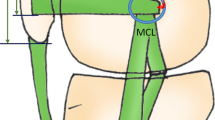
General feature of the MPFL and its femoral and patellar insertions were observed. All anatomical landmarks were carefully identified and marked (Fig. 1). A series of measurements were conducted and recorded, including the length of the double bundles of the MPFL and the angle in between, the width of the patellar MPFL insertion, and the paralleled and perpendicular distance between the femoral attachment of MPFL and medial femur epicondyle (MFE). All data were obtained, described, and analyzed in the form of mean ± SD. All measurements were taken with a sliding caliper by the same person in order to reduce the interobserver variation. The accuracy of the sliding caliper is 0.1 mm.
The schematic diagram shows all anatomical landmarks in the dissection. Point A, the superior patellar pole, is the patellar insertion point of the SOB. Point B, the center of the medial patellar margin, is the patellar insertion point of the ISB. They are together originate from the Point D. Length AD and BD are measured as the length of SOB and ISB, respectively. The included angle between line AD and line BD is also measured. Point C is the inferior patellar pole, and length AC is measured as the total patellar height. Length AB is the patellar insertion of MPFL. Point E is the position of MFE. Relative to the long axis of the femur, the paralleled and perpendicular distances between D and E are identified and measured. SOB the superior-oblique bundle of the MPFL, ISB the inferior-straight bundle of the MPFL, MPFL the medial patellofemoral ligament, MFE medial femur epicondyle
Results
The MPFL was found in all specimens we dissected. There were two knee specimens on which the ligament was thinner than usual but still with well-defined structure. Among all knee specimens, the MPFL was found to locate in the second layer of the medial side of the knee. When the distal part of the VMO was reflected anteriorly along its lower margin, the upper margin of the MPFL was observed to adhere to the deep aspect of the VMO (Fig. 2). The triangle formed by the superior edge of the MPFL, the TAM, and the VMO was a consistent anatomical feature to ensure recognizing and exploration of the MPFL. The structure of the MPFL originates from the medial aspect of the femur condyle, distal to the insertion of the TAM, and proximal to the femoral attachment of the medial collateral ligament. The fibers of MPFL fan out to the medial margin of the patella with direct insertion, and the superior bundle of fibers extends out of the upper end of the patella and joins the superior patellar quadriceps fibers. Along its course, it becomes wider, and a shape of triangle is formed by the structure of double bundles with the patella being the third boundary [7, 15].
The location of femoral attachment of MPFL is not as clear as other ligaments of the knee. Its origination has been controversial. In the present study, the center of the area where fibers of the MPFL originated was carefully identified as the initiation point of the MPFL, which was not located at the adductor tuberosity or the MFE in knee specimens of this dissection. Referring to the MFE, the position of the initiation point was located: the paralleled and perpendicular distance relative to the long axis of femur between it and MFE was 8.90 ± 3.27 and 13.47 ± 3.68 mm, respectively (Table 1).
The patellar insertion of the MPFL is wider than its femoral insertion. The MPFL is a thin band of retinacular tissue transversally connecting the medial condyle to the medial aspect of patella. The MFE is enwrapped by the course of MPFL. Approximately from the origination, fibers of the MPFL become wider as fan-sharp along its trip, forming two relative centered fiber bundles (Fig. 3). The lower fiber bundle, named as inferior-straight bundle (ISB), attaches the medial aspect of the patella nearly horizontally, and its length equal to the distance between the femur initiation point and the medial edge of patella was 71.78 ± 5.51 mm. The upper fiber bundle, named as superior-oblique bundle (SOB), also attaches the superior-medial aspect of patella, with some fibers merging into the patellar quadriceps fibers, and its length from the femur initiation point to the superior pole of patella measured was 73.67 ± 5.40 mm. The angle formed by the two fiber bundles was 15.1° ± 2.1°. Although the inferior-straight bundle insertion is in the inferior part of the patellar MPFL footprint and the superior-oblique bundle in the superior part, the bundles are not separated completely. This makes the MPFL the intact structure, where its patellar footprint was 22.28 ± 2.92 mm. The total height of patella was 49.73 ± 3.84 mm, and the percentage of the MPFL footprint was calculated to be about 1/2 (Table 2).
The photograph shows two relative centered fiber bundles of MPFL. The lower fiber bundle (ISB) attaches the medial aspect of the patella nearly horizontally. The upper fiber bundle (SOB) also attaches the supra-medial aspect of patella, with some fibers merging into the supra patellar quadriceps fibers. They originate from the femoral origination together and not separated entirely. This makes the MPFL intact with a fan-sharp structure. The point marked by black arrow is the femoral origination of the MPFL. E medial femoral epicondyle, P patella, VMO the vastus medialis obliquus, ISB inferior-straight bundle, SOB superior-oblique bundle
Discussion
The most important finding of the present study was functional bundles of MPFL, on the basis of confirmation of its existence. Since 1979, Warren and Marshall [26] first described a three-layer tissue structure on the medial side of the knee with the MPFL placed in the second layer. The knowledge about MPFL as a very thin band of tissue connecting the region of the femoral adductor and condyle to the proximal part of the medial edge of the patella has been confirmed in nearly all knees reports [10]. Different outcomes of measurement have been demonstrated; however, the existence of the MPFL is consistent and confirmed. On the other hand, Reider et al. [18] documented the presence of the MPFL in only 35% of knees cases (7 of 20), Conlan et al. [6] could not detect or palpate the MPFL in 4 of 33 knees. With more and more studies on the MPFL, the presence and importance of the MPFL in the preventing of lateral patellar dislocation are increasingly accepted by more and more clinical researchers. Different from other studies, the present study described the anatomic structure of the MPFL in much greater details, especially the patellar insertion, which may contribute to the anatomical reconstruction of the MPFL.
The femoral attachment of the MPFL is relatively compact. There have been some debates about the exact location of the attachment. The attaching points, once reported as the attachment site, include the medial femoral epicondyle [5, 11], the point just anterior to the medial epicondyle [10], and the adductor tubercle [6, 25]. In the present study, the center of the area where fibers of the MPFL originated was defined as initiation point of the MPFL, which was not located at the adductor tubercle (AT) or the MFE in knee specimens. Referring to the MFE, the origination point was positioned: just 8.90 ± 3.27 mm proximal and 13.47 ± 3.68 mm posterior to the MFE.
MPFL is known for its thin and wispy structure, especially in its femoral insertion. Several studies have indicated the thin feature of the MPFL, with the width measured as 12.2 ± 2.6 mm [24], 15.4 mm (range, 11–20 mm) [23], 19 mm (range, 10–30 mm) [17], 17.1 mm (range, 10–28.8 mm) [4], and 20.7 mm (range, 9–30 mm) [3]. A number of studies have found this delicate structure as major soft tissue restraint to resist lateral patellar translation; however, no paper has explained this mechanism definitely, on its function of guiding the patella into the confines of the femoral trochlea smoothly during the initial stages of knee flexion.
Anatomical descriptions [2] show that MPFL femoral insertion is not a clearly delineated structure due to the convergence of many tissues toward the medial epicondyle and coverage of the superficial fibers derived from the posteromedial capsule; the deep fibers were actually anchored to the bone just distal to the adductor tubercle. This anatomical feature was termed single point fixation [13, 16], which makes the femoral insertion the main location for injures to the MPFL in cases of acute dislocation of the patella [13]. When the reconstructed femoral attachment was taken out of position, by only 5 mm, from the normal femoral attachment, their length patterns differed greatly from those at the anatomical femoral attachment. Therefore, accurately identifying the anatomical point is very important in providing useful information on the best location for graft attachment during ligament reconstruction surgery.
Steensen et al. [23] studied the isometry of the MPFL, described that the portion of the MPFL extending from the inferior aspect of its patellar attachment to the superior aspect of its femoral attachment was most isometric, with the superior femoral attachment being the most important. Therefore, if the isometry has to be considered during reconstruction, the femoral site for graft must be identified precisely in order to achieve good clinical outcome. At present, there is no recommendation for a specific attachment point. The MFE is considered an adequate landmark during surgery, so our data may be useful to implant the graft at the best location and ultimately lead to better long-term outcome.
In the present study, the anatomic structure of the patellar insertion was described in great details with the introduction of the concept the functional bundles of the MPFL for the first time. It is a thin fiber tissue connecting the region of the femoral condyle to the medial edge of the patella. Approximately from the femur origination, the fibers of the MPFL become wider as fan-sharp, forming two relatively concentrated fiber bundles: the inferior-straight bundle (ISB) and the superior-oblique bundle (SOB). Although the ISB and SOB run on the patellar MPFL inferiorly and superiorly, respectively, as their name indicates, the two bundles are not entirely separated, which make MPFL one intact structure.
Despite the prevalence of the literature describing the morphology and function of the MPFL, little has been touched on the concept of functional bundles. Aragāo et al. [4] described in their study that the margins of the MPFL were concave or rectilinear in shape. At the upper margin, the concave shape predominated and was well characterized, while at the lower margin, the rectilinear shape was predominated, which sometimes was very difficult to distinguish. Amis et al. [2] found the MPFL seems to have two functional bands of fibers, which run along the proximal and distal edges; however, the functional significance, if any, of this two-band structure remains unknown. In the present dissection, the double-bundle structure was found from the well-developed ligaments; however, the assumption about the function of each bundle needs to be further studied and confirmed. To our knowledge, we are the first to conduct studies and confirm the composition of double functional bundles of the structure of the MPFL, although reconstruction of double bundles of MPFL has been emphasized during the knee surgery, and numerous studies indicate that better clinical outcomes have been achieved by focusing on the reconstruction of double bundles [3, 21, 22].
The medial patellar stabilizers consist of the medial retinaculum, the MPFL, the medial patellomeniscal ligament, and the VMO are important structures in preventing the lateral displacement of the patella and controlling the moving trajectory of the patella [6, 11, 15, 18]. The function of the MPFL was the first to be widely accepted and considered as the most important among all the medial patellar stabilizers. Some author even proposed that the essential lesion, without which the patella could not move to an abnormal lateral position, is the damage to the MPFL [2].
Patellofemoral contact begins with the distal part of the patella at approximately 20° of flexion, and it progresses to the proximal pole of the patella at 90° of flexion [20, 26]. With the flexion of the knee, the VMO starts to contract, the superior-oblique bundle is pulled proximally and appears shorter due to the tension through fibers attached to the VMO. As a result, the superior-oblique bundle with VMO provides the major dynamic soft tissue restraints and pulls the patella medially. When the knee is in flexion of 20°–30°, the patella slips into the femoral trochlea groove, and the resultant lateral force is resisted by the prominent lateral facet of the femoral trochlea. Therefore, the role of the MPFL with the knee in deep flexion remains unknown. The pressure between the patellofemoral joint might be balanced by the tension of the MPFL.
Under general condition when without VMO contraction, fibers of superior-oblique bundle become slack with weak tension. So the lower fiber bundle (ISB) acts as the main static soft tissue restraint to balance the resultant lateral force that works on patella caused by the Q angle.
Over the past years, interest in the passive restraints of the patellofemoral joint and their contribution to patellar stability has resulted in various techniques for MPFL reconstruction; however, patellar dislocation may be resulted from many factors. Attention to any one of these factors without the recognition of other contributing factors can lead to a surgical failure. The reconstruction of MPFL can not compensate the bony restrains deficiency of trochlear dysplasia, normal bone structure is necessary for MPFL reconstruction. Repair and reconstruction of the MPFL are commonly performed to restore the passive restraint and improve patellofemoral stability. Repair of the MPFL is common for an acute injury, although reconstruction is typically favored for recurrent instability, which can range from clear patellar dislocation to more subtle, symptomatic subluxation episodes. When indicated, trochleoplasty is applied to reestablish the bony constraint of patellofemoral joint or the tibial tuberosity transfer to correct limb alignment, and lateral retinaculum release is assisted where isolated MPFL reconstruction may result in poor outcomes.
Just as understanding of the anatomical bone tunnel site of the cruciate ligament is important to improved results of surgical reconstruction, understanding of the anatomy of MPFL is critical to the success of the MPFL reconstruction. Inadvertent misplacement will lead to either overconstraint or underconstraint. Elias and Cosgarea’s [9] computational analysis, with the simulation of physiological knee function from 30° to 90° flexion, emphasized that anatomical reconstructed graft was similar with the native MPFL, small errors in graft length and position can dramatically increase the force and pressure applied to medial patellofemoral cartilage, which could lead to degradation, pain, and arthrosis. Just as seen in the clinic cases, as Thaunat and Erasmus [24] presented, with pain and loss of flexion due to the overtight of reconstructed MPFL.
Long-term clinical success after MPFL surgery greatly depends on the procedure of MPFL reconstruction, with fully understanding of detailed MPFL anatomy. The present study was to locate the femoral insertion site more precisely to make mini-invasive technique with MFE as reference to locate graft site in reconstruction is more practical and useful. The most important part is to introduce the concept of the functional bundles of MPFL, which may provide the theoretical foundation to better understand clinic double-bundle anatomical MPFL reconstruction and shed lights on the future researchers, consequently improve the clinical outcome of the MPFL reconstruction.
The present study has some limitations. It was the description of the functional bundles of the MPFL for the first time with basis on morphological observation with small sample only. Therefore, lager sample or histological study of ligament fibers may be needed to confirm its existence. The function of MPFL on the patella was the hypothesis based on the anatomy, further biomechanics study is required to confirm and quantify each function.
Conclusion
The present study was to locate the femoral insertion site with the prominent MFE as reference and introduce the concept of the functional bundles of MPFL. Approximately from the femoral origination point, fibers of the MPFL form two relatively concentrated fiber bundles: the inferior-straight bundle (ISB) and the superior-oblique bundle (SOB). Based on anatomical study and relevant literature review, an assumption can be safely made for the function of MPFL: the upper fibers of MPFL with the oblique course (SOB) are not only the static structure but also serve as dynamic maintenance of patella stability combined with the VMO. The lower fibers with horizontal course (ISB) act as the main static soft tissue restraints.
References
Ahmad CS, Stein BE, Matuz D, Henry JH (2000) Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. Am J Sports Med 28:804–810
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10:215–220
Andrikoula S, Tokis A, Vasiliadis HS (2006) The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc 3:214–220
Aragāo JA, Reis FP, Vasconcelos DP, Feitosa VLC, Nunes MAP (2008) Metric measurements and attachments levels of the medial patellofemoral ligament: an anatomical study in cadavers. Clinics 63:541–544
Avikainen VJ, Nikku RK, Seppanen-Lehmonen TK (1993) Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clin Orthop Relat Res 297:12–16
Conlan T, Garth WP, Lemons JE (1993) Evaluation of the medial soft tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
David A, Parker MD, Jerry W, Alexander BS, Michael A, Conditt PHD, Obinna N, Uzodinma BA, William J, Bryan MD (2008) Comparison of isometric and anatomic reconstruction of the medial patellofemoral ligament: a cadaveric study. Orthopedics 31:339–343
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 9:1478–1485
Feller JA, Feagin JA, Garrett WE (1993) The medial patellofemoral ligament revisited: an anatomical study. Knee Surg Sports Traumatol Arthrosc 1:184–186
Hautamaa PV, Fithian DC, Kaufmann KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Kaplan EB (1957) Factors responsible for the stability of the knee joint. Bull Hosp Joint Dis 18(1):51–59
Nomura E (1999) Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop 23:260–263
Nomura E, Horiuchi Y, Kihara M (2000) A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee 7:211–215
Nomura E, Horiuchi Y, Kihara M (2000) Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 7:121–127
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Philippot R, Chouteau J, Wegrzyn J (2009) Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surg Sports Traumatol Arthrosc 5:475–479
Reider B, Marshall JL, Koslin B, Ring B, Girgis FG (1981) The anterior aspect of the knee joint: an anatomical study. J Bone Joint Surg Am 63:351–356
Sandmeier RH, Burks RT, Bachus KN, Billings A (2000) The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med 28(3):345–349
Sallay PI, Poggi J, Speer KP, Garrett WE (1996) Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med 24:52–60
Schöttle PB, Fucentese SF, Romero J (2005) Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 13:516–521
Schöttle P, Schmeling A, Roero J, Weilmer A (2009) Anatomical reconstruction of the medial patellofemoral ligament: using a free gracilis autograft. Arch Orthop Trauma Surg 129:305–309
Steensen RN, Dopirak RM, McDonald WG III (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32:1509–1513
Thaunat M, Erasmus PJ (2009) Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 5:480–483
Tuxoe JI, Teir M, Winge S, Nielsen PL (2002) The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc 10:138–140
Warren LF, Marshall JL (1979) The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 61:56–62
Acknowledgments
Author thanks the Department of Anatomy of Hebei Medical University for providing samples for this study. Thanks also go to Professor Zhang for drawing of schematic diagram in the manuscript. This study receives no financial support.
Conflict of interest statement
All authors have read and contributed to the submitted manuscript, and there is no conflict of interest among the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kang, H.J., Wang, F., Chen, B.C. et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 18, 1511–1516 (2010). https://doi.org/10.1007/s00167-010-1090-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1090-8