Abstract
Background
Several MPFL reconstructions are commonly performed for recurrent patellar dislocation, but misleading data are currently available in the literature on the ability of the different techniques to re-create a functioning ligament.
Materials and methods
In this study, we showed the biomechanical properties of two different procedures for MPFL reconstruction using a natural orientation during uniaxial tensile testing. Eighteen fresh-frozen human knees were randomly assigned to two groups of nine each. In the group A, the reconstruction was performed using a double converging tunnels technique and in the group B was used a single-tunnel technique with semitendinosus autograft. The specimens were loaded in natural orientation using an Instron tensile test machine, and the stiffness and ultimate load were determined.
Results
The ultimate load was 213 ± 90 and 171 ± 51 N using our double-bundle technique (group A) and the single-bundle technique (group B), respectively. One (11 %) specimen failed at the patellar side due to patellar fracture in the group B. There was no statistical significant difference (p > 0.05) between the two groups in terms of stiffness and ultimate load.
Conclusion
This study is the first biomechanical evaluation of the MPFL reconstructions in natural orientation. Both the procedures achieved safe fixation of the graft at the femoral attachment; however, the single-bundle technique reported 11 % of failure at the patellar side due to patellar fracture. In addition, the double-bundle technique can better restore the anatomy of the native ligament.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patello-femoral instability is challenging for orthopedic surgeons and rehabilitators due to its multifactorial etiology. The etiologies that predispose patients to lateral patellar dislocation are believed to be genu valgum, patella alta, ligament laxity, contracture of the lateral patellar soft tissues, hypoplasia of the lateral femoral condyle, a laterally located tibial tubercle, vastus medialis insufficiency, and abnormal attachment of the iliotibial tract [1].
Medial patello-femoral ligament (MPFL) is the primary passive restraint against lateral translation of the patella [2–6]. Conlan et al. [7–9] found that the MPFL contributes for 50–60 % of the medial restraining force against lateral patellar translation. The MPFL extends from the superior two-thirds of the medial patellar margin to just distal of the adductor tubercle, with superficial fibers extending to the posterior capsule [3, 10, 11].
Previous studies have demonstrated that this structure is always injured after lateral patellar dislocation [10, 12, 13]; thus, MPFL reconstruction is commonly performed to restore the patello-femoral stability.
However, many technical errors during MPFL reconstruction could overload and alter the patello-femoral joint [14, 15]. MPFL reconstruction reproduces a postero-medial force that increases contact pressure on the medial patellar facet.
Understanding the biomechanical properties of the MPFL reconstructions is a key point to keep in mind. However, the orientation of the specimen can have significant influence on the final results [16, 17].
We hypothesized that MPFL reconstruction with double-bundle converging tunnels could achieve better biomechanical properties than the single-bundle technique.
The purpose of our study was to evaluate the biomechanical properties of a double-bundle technique for MPFL reconstruction in comparison with a single-bundle reconstruction using hamstring autografts in natural orientation.
Materials and methods
Technical note
Double-bundle converging tunnels technique
By means of 2-cm incision at the pes anserinus, the gracilis tendon was freed by the muscle and harvested with a tendon stripper and detached by the distal insertion from fresh-frozen cadaveric knees. Using a work station, the free ends of the tendon were sutured with No. 2 Ethicon sutures by Krackow suture and pretensioned for 10 min with 40 N using a tensioner to avoid tendon creep.
Through a 3-cm incision, the medial border of the patella was exposed and two Kirschner wires were drilled in a converging fashion at the proximal one-third and at the center of the medial edge trying to reproduce an angle of 90° [1] (Fig. 1a, b). Patellar guidewires were overdrilled using a 4.5-mm cannulated reamer until the sockets were in communication. The femoral tunnel was anatomically placed at the insertion of the native ligament, distally to the adductor tubercle [10, 11, 13]. The graft was passed through the patellar converging tunnels forming a loop of U-shaped (Fig. 2a). Then, by blunt dissection the free ends of the graft were passed through an interval between the capsule and the vastus medialis obliquus and lastly pulled through the femoral tunnel. The graft tensioning was performed manually pulling the suture on the lateral aspect of the femur avoiding overtensioning.
After five cycles of flexion–extension, at the tibial side the graft was sutured by transperiostal stitches (PDS No. 0) and at the femoral side the fixation was achieved by a 8 × 20 mm bioabsorbable interference screw (Biorci, Smith, and Nephew) at 60° of flexion angle (Fig. 1).
We secured the graft to the femur with the knee flexed at 60° because maximal graft length has been reported in this position as demonstrated by Smirk [18].
Single-bundle technique
The reconstruction was performed drilling a transverse 7-mm tunnel at the middle third of the patellar medial border and a 7-mm femoral tunnel placed slight distal to the adductor tubercle (Fig. 2b) as described in the tunnel procedure by Mountney [19]. In this group, the fixation was achieved with 8 × 20 mm bioabsorbable interference screws (Biorci, Smith, and Nephew) both to the patella and the femur.
Tensile test with natural orientation
Eighteen fresh-frozen human cadaveric knees were used for this study. Each specimen was screened for a history of trauma, neurologic disease and stored at −20 °C [20] (Moon 2006). Prior to testing, the specimen was thawed for 24 h at room temperature. The semitendinosus tendons were harvested from each knee and wrapped in saline-soaked gauze to prevent dehydration. Then MPFL reconstruction was randomly performed with our double-bundle technique (group A) and with a single-bundle technique (group B).
In preparation for testing, the femur and the tibia were cut approximately 20 cm from the joint line and all soft tissues were removed 10 cm away from the joint line on both the femur and the tibia [21]. Then, the femur and the tibia were completely dissected from the soft tissue except the MPFL reconstructed and potted in cylinders using cement and fixed to the tensile machine (Instron Inc., Norwood, MA, USA) by custom-made clamps. The tensile testing was performed in anatomical orientation with the femur 37° ± 2° internally rotated to the coronal plane [16, 19] and the patella placed with an angle of 90° to the MPFL (Fig. 3a, b).
All the samples were preconditioned with ten cycles between 0 mm and 2 mm of elongation and then underwent to failure at 10 mm/min. The load elongation curve was determined, and the stiffness and ultimate load were evaluated.
Statistical analysis
The statistical analysis was performed using unpaired T test. A p value <0.05 was considered statistically significant.
Results
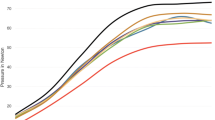
The ultimate load was 213 ± 90 and 171 ± 51 N using our double-bundle technique (group A) and the single-bundle technique (group B), respectively. The linear stiffness was 17.11 ± 5 and 13.9 ± 5.4 N in group A and group B, respectively. One (11 %) specimen failed at the patellar side due to patellar fracture in group B. All the other specimens failed at the graft midsubstance. There was no statistical significant difference (p > 0.05) between the two groups in terms of stiffness and ultimate load.
Discussion
This study is the first biomechanical evaluation of the MPFL reconstruction in human specimen using a natural orientation.
As found by Kim et al. in a porcine study [16], the natural orientation mimics the in situ loading condition of the MPFL and should be used to obtain representative data.
Previous biomechanical study should be considered misleading cause the non natural orientation of the patella during the uniaxial loading [19]. Testing the patella in non-anatomical position reproduces a non-physiological vector force on the patella–MPFL–tibia complex (PMTC).
The double-bundle technique achieved better biomechanical properties than the single-bundle reconstruction.
We found a better ultimate load with the double-bundle technique even though there was no statistical significant difference (p < 0.05) in comparison with the single-bundle procedure.
Kim et al. [16] demonstrated that 90 % of failures at the femoral attachment of the native MPFL, where there is the narrowest portion of the ligament. In our study, we found 89 % of failure at the graft midsubstance. Both double and single-bundle techniques achieved safe fixation of the graft at the femoral attachment.
The single-bundle technique reported 11 % of failure at the patellar side due to a patellar fracture and none with the double-bundle technique.
The advantages of this technique are a more equal distribution of stress on the patella by means of the converging tunnels and the consequent decrease in the risk of patellar fracture. Attention should be paid to avoid too close placement of the converging tunnels.
In addition, our double-bundle technique does not include any fixation device on the patella; it is relatively simple, quick and cost-effective procedure in comparison with the single-bundle procedure.
The double bundle with converging patellar tunnels restores the sail shape of the MPFL [3] and can better restore the anatomy of the native ligament regarding the patellar insertion.
Limitation of this study was the mean age of the specimen, 71 years. The linear stiffness was low, and those results could be attributable to the suboptimal quality of hamstring autografts.
A converging V-shaped tunnel was proposed by Nelitz [22] and found a significant improvement in knee function and patient satisfactions without any episode of redislocations.
In addition, a larger surface area allows a better graft healing into the patellar bone tunnels.
In a clinical study, Wang et al. [23] confirmed that double-bundle reconstruction achieved clinical outcomes far better than the single-bundle technique.
However, we had demonstrated that the single-bundle technique is a safe technique and achieves a reliable fixation at the femoral attachment, but tricky remains the screw fixation of the graft at the patellar side cause the risk of fracture.
Some authors had used single-bundle technique for MPFL reconstruction avoiding screw fixation at the patella. Deie et al. [24] fixed the semitendinosus, leaving intact its tibial insertion, to the patella by means of suture to the anterior surface of the patella.
In 2005, Schottle [25] reported a single-bundle technique using semitendinosus with suture anchor fixation at the patella.
Conclusion
This study is the first biomechanical evaluation of the MPFL reconstructions in natural orientation.
Previous biomechanical studies on MPFL reconstruction can be considered tricky due to non-natural loading condition of the specimen during the uniaxial testing.
We have demonstrated that both the procedures achieved safe fixation of the graft at the femoral attachment; however, the single-bundle technique reported 11 % of failure at the patellar side due to patellar fracture. In addition, the double-bundle technique can better restore the anatomy of the native ligament especially at the patellar insertion where the double-bundle converging tunnels mimic the sail shape of the native ligament.
References
Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M (2005) A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc 13(7):522–528. doi:10.1007/s00167-005-0641-x
Burks RT, Desio SM, Bachus KN, Tyson L, Springer K (1998) Biomechanical evaluation of lateral patellar dislocations. Am J Knee Surg 11(1):24–31
Nomura E (1999) Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop 23(5):260–263
Sally PIPJ, Speer KP et al (1996) Acute dislocation of the patella: a correlative pathoanatomical study. Am J Sport Med 24:52–60
Dandy DJ (1996) Chronic patellofemoral instability. J Bone Joint Surg Br 78(2):328–335
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75(5):682–693
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10(3):215–220
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13(7):510–515. doi:10.1007/s00167-004-0607-4
Placella G, Tei M, Sebastiani E, Speziali A, Antinolfi P, Delcogliano M, Georgoulis A, Cerulli G (2015) Anatomy of the Medial Patello-Femoral Ligament: a systematic review of the last 20 years literature. Musculoskelet Surg 99(2):93–103. doi:10.1007/s12306-014-0335-y
Nomura E, Inoue M (2003) Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthrosc J Arthrosc Relat Surg 19(5):E47. doi:10.1053/jars.2003.50167
Placella G, Tei MM, Sebastiani E, Criscenti G, Speziali A, Mazzola C, Georgoulis A, Cerulli G (2014) Shape and size of the medial patellofemoral ligament for the best surgical reconstruction: a human cadaveric study. Knee Surg Sports Traumatol Arthrosc 22(10):2327–2333. doi:10.1007/s00167-014-3207-y
Beck P, Brown NA, Greis PE, Burks RT (2007) Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 35(9):1557–1563. doi:10.1177/0363546507300872
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34(9):1478–1485. doi:10.1177/0363546506287486
Kim KE, Hsu SL, Woo SL (2014) Tensile properties of the medial patellofemoral ligament: the effect of specimen orientation. J Biomech 47(2):592–595. doi:10.1016/j.jbiomech.2013.11.026
Criscenti G, De Maria C, Sebastiani E, Tei M, Placella G, Speziali A, Vozzi G, Cerulli G (2015) Material and structural tensile properties of the human medial patello-femoral ligament. J Mech Behav Biomed Mater 54:141–148. doi:10.1016/j.jmbbm.2015.09.030
Smirk C, Morris H (2003) The anatomy and reconstruction of the medial patellofemoral ligament. Knee 10(3):221–227
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 87(1):36–40
Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 19(3):217–225
Zamarra G, Fisher MB, Woo SL, Cerulli G (2010) Biomechanical evaluation of using one hamstrings tendon for ACL reconstruction: a human cadaveric study. Knee Surg Sports Traumatol Arthrosc 18(1):11–19. doi:10.1007/s00167-009-0911-0
Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S (2013) Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med 41(1):58–63. doi:10.1177/0363546512463683
Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, Wang J (2013) Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop 37(4):617–624. doi:10.1007/s00264-013-1788-6
Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H (2003) Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br 85(6):887–890
Schottle PB, Fucentese SF, Romero J (2005) Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 13(7):516–521. doi:10.1007/s00167-005-0659-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Placella, G., Speziali, A., Sebastiani, E. et al. Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single-bundle technique. Musculoskelet Surg 100, 103–107 (2016). https://doi.org/10.1007/s12306-016-0397-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0397-0