Abstract
Purpose
The purpose of this study was to evaluate the influence of individual characteristics on rotational knee laxity in healthy participants. Our second aim was to verify whether the contralateral knee of patients with a non-contact ACL injury presents greater rotational knee laxity than a healthy control group.
Methods
Sixty healthy participants and 23 patients having sustained a non-contact ACL injury were tested with a new Rotameter prototype applying torques up to 10 Nm. Multiple linear regressions were performed to investigate the influence of gender, age, height and body mass on rotational knee laxity and to establish normative references for a set of variables related to rotational knee laxity. Multiple analyses of covariance were performed to compare the contralateral knee of ACL-injured patients and healthy participants.
Results
Being a women was associated with a significantly (P < 0.05) higher rotational knee laxity, and increased body mass was related to lower laxity results. In the multiple analyses of covariance, gender and body mass were also frequently associated with rotational knee laxity. When controlling for these variables, there were no differences in measurements between the contralateral leg of patients and healthy participants.
Conclusion
In the present setting, gender and body mass significantly influenced rotational knee laxity. Furthermore, based on these preliminary results, patients with non-contact ACL injuries do not seem to have excessive rotational knee laxity.
Level of evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past years, the evaluation of rotational knee laxity has received increased attention from the medical and scientific community. Its main interests lie with the examination of the anterior cruciate ligament (ACL) after serious knee injury and the follow-up of patients after ACL reconstruction. The pivot-shift test is currently the best approach to diagnose an ACL tear [5]. However, it is highly subjective and does not allow for precise quantification of knee laxity [19]. Therefore, several devices have been designed to measure static rotational knee laxity non-invasively under controlled conditions [4, 7, 15, 18, 20, 25]. Normative references for the different instruments are often lacking, which makes it currently difficult to distinguish pathological cases from normality. Several studies have found that women tend to have greater rotational knee laxity than men [12, 20, 26]. Except for gender, no individual characteristics have so far been investigated. Additional factors such as age, height and body mass could potentially influence rotational knee laxity measurements and could thus have relevance when comparing patients with uninjured controls.
Some investigations put forward that anterior knee laxity and generalized joint laxity might be risk factors of ACL injury [9, 28, 30]. Rotational knee laxity has been little investigated, but it has been suggested that increased external tibial rotation could be a risk factor [3], despite the fact that internally directed torques generate greater strain on the ACL [17]. If increased rotational knee laxity is indeed a risk factor of non-contact ACL injuries, then patients having sustained such an injury should have greater results compared with a control group. The assessment of the uninjured, contralateral knee could serve as a proxy measurement for rotational knee laxity of the involved knee before the injury.
The main purpose of the present study was to analyse if individual characteristics influence rotational knee laxity of healthy control subjects with no previous knee injuries, evaluated with the second Rotameter prototype (P2). We hypothesized that rotational knee laxity is influenced by gender, age, height and body mass. A secondary aim was to investigate the rotational knee laxity of the contralateral knee of patients who sustained a non-contact ACL injury. Our hypothesis was that these patients have a greater rotational knee laxity compared with a healthy control group, which would suggest that increased rotational knee laxity is a risk factor of sustaining a non-contact ACL injury. This question was addressed based on preliminary patient data from an ongoing clinical research project.
Materials and methods
Healthy participants were recruited based on the following selection criteria: aged between 18 and 60 years, no previous knee injury, no lower limb injury during the 6 months preceding the test, no disease influencing joint mobility or restricting activities of daily living and ability to take part in high demanding sports activities, such as basketball, football or handball. Patients with ACL injuries were recruited from an ongoing clinical research project at our institution. Only patients with non-contact ACL injuries were included. The knee laxity results of the contralateral knee were considered regardless of the treatment of the involved knee (surgical or conservative), associated injuries or treatment phase. Patients were excluded if they had had previous knee injuries on their contralateral leg. Pregnancy was an exclusion criterion for female participants in both the control and injured group. Sixty healthy participants and 23 patients were recruited for this study according to their respective inclusion criteria. All participants received a full account of the study objectives and procedures in oral and written form and signed a consent agreement. The study protocol had previously been approved by the National Ethics Committee for Research.
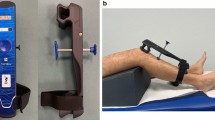
New Rotameter prototype (P2)
Rotational knee laxity was assessed using the second version of the Rotameter prototype (P2) and a similar testing procedure as previously described [16]. Briefly, the patient was positioned on an examination table in the prone position with his/her thighs secured into 2 half cone-shaped leg supports using Velcro straps. The tested leg was tightly immobilized in a ski boot of appropriate size, which was itself fixed to the rotational handle bar and frame of the Rotameter. The device was fixed to the examination table at an angle so as to induce a knee flexion of 30° and a hip flexion of 0°, given the patient position. Different torques can be applied to the examined lower limb in internal and external rotation via the handle bar. The applied torque was measured using a custom-made, previously calibrated electronic torque sensor (strain gauge, resolution 0.001 Nm) integrated into the handle bar. Rotation angle was measured using an inclinometer (NG4U, SEIKA Mikrosystemtechnik GmbH, Germany, resolution 0.01°) fitted to the rotational part of the device. During the test, applied torque and resulting rotation angle were amplified, sampled at 60 Hz by a 24-bit A/D converter (USB NI 9219DS, National Instruments, Texas, USA) and stored on a PC. Custom-made software was used to handle all data and to provide real time feedback to the operator.
Testing procedures and calculations
Once the patient was installed, the zero angle of the system was defined with the rotational handle bar placed horizontally and the position of the patient’s foot perpendicular to the ground. Following the calibration, the handle bar was released, so that the leg returned to its natural resting position (offset), which was used as the starting position for the test. Four trials were subsequently performed with applied torques of up to 10 Nm, first in internal rotation (IR), then in external rotation (ER). Separating evaluations of knee laxity for IR and ER was preferred compared to applying entire cycles in both directions [1, 8, 20, 24, 27]. Based on previous pilot testing (data not shown), this procedure was found to allow for optimal foot positioning within the boot during “preconditioning” trials and thus decrease the influence of movement artefacts during subsequent trials. The same procedure was applied on both limbs. The order of testing was randomized for the control group while in patients, the tests were first performed on the uninvolved leg.
Acquired data were smoothed using a 10-point moving average. Subsequently, offset due to the natural resting position of the leg was set to zero. Instead of limiting the analysis of rotational knee laxity to the mere angle reached for a given torque applied in internal or external rotation [4, 15, 18], we wanted to draw a more complete picture of rotational knee laxity by measuring additional variables [7, 20, 22]. Therefore, the following 10 variables were calculated on the ascending limb of the curve (Fig. 1): rotation angle at 5 and 10 Nm, primary compliance (PC) calculated as the slope of the curve between 2 and 5 Nm, and secondary compliance (SC) computed as the slope of the curve between 5 and 10 Nm. All variables were determined separately for IR and ER. Finally, total range (TR) was taken as the sum of angles obtained with applied torques of 5 and 10 Nm for IR and ER. The first 2 preconditioning trials were used to optimize foot positioning within the boot and were therefore discarded; data are reported as average values of trials 3 and 4. With this measurement procedure, the precision of the device was determined by the minimum detectable change (MDC) according to Weir [29]. MDC calculation was based on a repeated measures analysis of variance performed on the results of 50 healthy participants tested on 2 different occasions by 2 different examiners. The MDC was comprised between 3 and 5° for IR and ER at 5 and 10 Nm; MDC was 6 and 7° for TR at 5 and 10 Nm, respectively; MDC was between 0.3 and 0.8°/Nm for PC and SC.
Outcome variables for rotational knee laxity measured with the second Rotameter prototype (P2). IR5Nm, internal rotation angle at a torque of 5 Nm; ER5Nm, external rotation angle at a torque of 5 Nm; IR10Nm, internal rotation angle at a torque of 10 Nm; ER10Nm, external rotation angle at a torque of 10 Nm; PCIR, primary compliance in internal rotation; PCER, primary compliance in external rotation; SCIR, secondary compliance in internal rotation; SCER, secondary compliance in external rotation
Data analysis
All statistics were performed using version 19.0 of the SPSS software. Differences between the left and right knee of healthy participants were evaluated using independent Student’s t tests. To analyse the influence of individual characteristics on the different variables representing rotational knee laxity, multiple linear regressions (descending method) were performed including gender, age, height and body mass as independent variables. Final models were analysed using the independent variables that were most frequently significant. All variables were reviewed for normality and heteroscedasticity using normal P–P plots and residuals plots, respectively. Multicollinearity was considered if the variation inflation factor was superior to 10 and the condition index superior to 30.
To compare the rotational knee laxity of the contralateral knee of patients with that of the healthy participants, multiple analyses of covariance (MANCOVA) were performed. The models included health status (control vs. patients) and those variables that were previously found to have an influence on rotational knee laxity. Significance was set at P < 0.05.
Results
Table 1 provides an overview of the basic demographics of the healthy participants and the patients recruited for the present study.
Influence of individual characteristics on rotational knee laxity
No significant differences were found between the left and the right knee of healthy subjects. Therefore, the results from the left and right side of each subject were averaged to represent the values for the healthy participants. Stepwise linear regressions revealed that gender had a significant influence on 8 out of 10 variables of rotational knee laxity. Body mass was found to be significant for 7 out of 10 variables (P < 0.05). No systematic influence was found for the other factors analysed. Considering these results, only gender and body mass were entered into the final regression models. Unstandardized coefficients, their 95% confidence intervals, associated P-values and R square values of the final models are provided in Table 2. Being a women was associated with a significantly higher rotational knee laxity for 7 out of 10 variables (P < 0.05). Increased body mass was related to lower laxity results for 6 out of 10 variables (P < 0.05). The model including gender and body mass explained between 22 and 57% of the variance of rotational laxity variables.
Comparison of contralateral and healthy knees
Differences between the laxity measurements of our healthy participants and the contralateral knee of patients were tested using status (control subject or patient) as the dependent variable and including gender and body mass as independent variables in the MANCOVA model. None yielded a significant result for an interaction term of the tested variables, such that the simpler model with no interaction was eventually preferred. Table 3 shows descriptive data and the results from the MANCOVA. As for the multiple linear regressions, gender and body mass were frequently associated with rotational knee laxity. However, there were no differences in rotational knee laxity measurements between the contralateral leg of patients and our healthy participants. Statistical power for status determined post hoc was generally low, with a maximal value of 0.50 for PCIR.
Discussion
The present study revealed two key findings. First, gender and body mass influenced rotational knee laxity in the present setting with the second Rotameter prototype, thus partly confirming our first hypothesis. Second, our preliminary results suggest that the rotational laxity of the contralateral knee of patients suffering a non-contact ACL injury is not significantly greater than the one from healthy controls. However, these results must be viewed as preliminary considering the limited number of patients tested and the low statistical power.
The gender effect on rotational knee laxity has been previously investigated by Shultz et al. [26]. They found that women (n = 10) showed significantly greater TR5Nm than men (n = 10). Their difference of 35% fits well with the difference of 40% found in the current investigation. However, in the study of Shultz et al. [26], IR5Nm and ER5Nm were not significantly different between genders. Park et al. [20] found a significant difference between women (n = 10) and men (n = 10) with an applied torque of 7 Nm, but only in external rotation. Unfortunately, they did not investigate total range and did not provide quantitative data for internal and external rotations (except for graphical representation). The present study revealed differences between women (n = 25) and men (n = 35) for a greater number of variables related to knee joint laxity. The reason for these slight discrepancies with the two prior investigations might result from a greater sample size studied here, as well as differences in subject positioning and measuring methods. Shultz et al. [26] studied their participants in a supine position, with a hip flexion of 10° and a knee flexion of 20° and measured tibio-femoral rotation with electromagnetic sensors on the thigh and the tibia. On the other hand, Park et al. [20] had their subjects seated with the hip flexed at 85° and the knee flexed at 60°, using a kinematical approach to measure knee rotation. In spite of these methodological differences, collectively their results plus our own findings suggest that women have a higher rotational knee laxity compared with men.
When considering compliance data, women either tended to have (PCER, +25%) or did have (PCIR, +29%) significantly greater values compared with men for torques between 2 and 5 Nm. These findings suggest that the gender difference in knee laxity could mainly be related to differences in the first degrees of knee rotation under low torques. A similar conclusion was reached by Schmitz et al. [22] who found a lower stiffness (i.e. greater compliance) in women but only for torques up to 1 Nm. For greater torques (up to 5 Nm), stiffness was either similar (external rotation) or greater (internal rotation) than in men. Well in line with the current results, the cadaver study of Hsu et al. [12] revealed that stiffness between 2.5 and 5 Nm was 25% lower in female specimens.
The higher primary compliance and greater rotational knee laxity observed in women could be a risk factor for non-contact ACL injuries. Indeed, in a sport context, female athletes were shown to have a significantly greater ACL injury incidence than men (0.43 injuries/1,000 athlete’s exposure vs. 0.09 injuries/1,000 athlete’s exposure) [10]. Amongst other determinants (anatomical, genetic, neuromuscular or hormonal), anterior knee laxity has been identified as a risk factor of non-contact ACL injuries, but only for women [28]. In a similar way, increased rotational knee laxity could represent a higher injury risk.
To the authors’ knowledge, the present study is the first to investigate other individual characteristics than gender. Body mass was found to negatively influence rotational knee laxity. The explanation for this effect is not straightforward. It could be that people with a greater body mass have an increased amount of leg soft tissue, leading to a greater stiffness of the leg and lower measured rotational knee laxity. Another explanation could be linked to the testing procedure and patient installation used here, with a greater leg mass and volume causing a firmer immobilisation of the thigh, thus controlling better for hip rotation during the test. The influence of body mass and other personal characteristics should be further investigated with other rotational knee laxity measurement devices.
Regarding rotational knee laxity, the contralateral knees of patients suffering a non-contact ACL injury had similar responses compared with our healthy control group. These preliminary findings do not support our second hypothesis. However, it should be noted that the study was clearly underpowered, which calls for attention when interpreting these negative results. Still, there was a tendency for PCIR to be increased in our patients (P = 0.051). Although speculative, it is possible that testing a greater sample of patients could have revealed significant differences for variables related to internal rotational knee laxity. The study of Branch et al. [7] found increased IR at 5.65 Nm in the contralateral knees of ACL-injured patients compared with uninjured controls. They suggested that increased IR may place a subject at a greater risk of sustaining an ACL injury. The mechanism of non-contact ACL injuries provides further support that excessive rotational knee laxity could be a risk factor. Investigating the phenomenon in real sport situations, Koga et al. [13] found that during the first 40 ms after initial contact, the knee rotated internally by approximately 8° and then externally by 17° [13]. The external rotation might occur after the ACL is already torn. It should be noted, however, that ACL injuries are generally caused by complex movements occurring in multiplanar directions [21] including knee valgus and/or excessive anterior tibial displacement [3, 11, 14, 21]. It has been suggested that only combined movements produce a sufficiently high strain on the ACL and that mere internal or external rotations might not suffice to tear an ACL [6]. Future research is warranted to draw final conclusions on whether increased knee laxity in internal rotation is a risk factor. In that context, it should be acknowledged that static rotational knee laxity measurements do not reflect functional knee movements.
The second prototype of the Rotameter used in the present study yielded lower rotational knee laxity results than the previous one [16]. Lorbach et al. [16] found a TR of about 97° at 10 Nm in a mixed healthy population (15 men and 15 women), which is higher than the TR that was measured here, both in men (71.2° ± 11.5°) and women (92.5° ± 11.8°). The second prototype of the Rotameter provides a better ankle immobilization via the ski boot, limits thigh movements and has an enhanced overall rigidity. Despite these improvements, TR5Nm measured here (42° and 59° for men and women, respectively) was approximately twice the values reported by Shultz et al. [24–26] in a control population (20° and 27° for men and women, respectively). This difference could be largely explained by the measuring method used, Shultz et al. [24–26] analysing the tibio-femoral rotation directly at the knee via electromagnetic sensors positioned on the thigh and the tibia. Rotational knee laxity at 10 Nm measured here (on average around 80° here) also represent twice the results of Shoemaker et al. [23]. They described a TR10Nm of some 40° for a mixed population, as they also measured the rotation angle directly at the tibia. Based on results from a subgroup of their study participants, Branch et al. [7] calculated that tibio-femoral rotation represented 49% of the total leg rotation using tibial electromagnetic sensors. The authors therefore corrected all their presented results by this factor, a procedure that would have yielded similar results in the current investigation compared with the previously cited studies.
From the preceding discussion, it appears that absolute measurements of rotational knee laxity performed at the foot are overestimated with regard to true tibial rotation [2]. This shortcoming also concerns the present device and represents a limitation that should be taken into account when interpreting absolute results. However, this does not disqualify the approach for repeated measurements during patient follow-up or within patient side-to-side comparisons, given the satisfactory precision of the measurements. Another drawback of this investigation is the lack of patients included in the second part of the study. A greater and more balanced patient group might have yielded significant results and confirmed our hypothesis of increased knee laxity in the contralateral leg of individuals with non-contact ACL injuries. Thus, further study is warranted to elucidate this question.
Conclusion
Age and height do not seem to influence rotational knee laxity. However, being a women leads to greater values of rotational knee laxity and increased body mass to lower values. The clinical relevance of these findings is that individual characteristics can have a significant influence on rotational knee laxity and should be more systematically investigated. These factors should be taken into account when different groups are being compared, using appropriate statistical models. When controlling for gender and body mass, the contralateral leg of patients having sustained a non-contact ACL injury did not exhibit excessive rotation compared with a healthy control group. However, this negative finding could be due to a small sample size tested and should be further investigated.
References
Ahrens P, Kirchhoff C, Fischer F, Heinrich P, Eisenhart-Rothe R, Hinterwimmer S, Kirchhoff S, Imhoff AB, Lorenz SG (2011) A novel tool for objective assessment of femorotibial rotation: a cadaver study. Int Orthop 35(11):1611–1620
Alam M, Bull AM, Thomas RD, Amis AA (2011) Measurement of rotational laxity of the knee: in vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med 39(12):2575–2581
Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lazaro-Haro C, Cugat R (2009) Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc 17(7):705–729
Almquist PO, Arnbjornsson A, Zatterstrom R, Ryd L, Ekdahl C, Friden T (2002) Evaluation of an external device measuring knee joint rotation: an in vivo study with simultaneous Roentgen stereometric analysis. J Orthop Res 20(3):427–432
Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther 36(5):267–288
Berns GS, Hull ML, Patterson HA (1992) Strain in the anteromedial bundle of the anterior cruciate ligament under combination loading. J Orthop Res 10(2):167–176
Branch TP, Browne JE, Campbell JD, Siebold R, Freedberg HI, Arendt EA, Lavoie F, Neyret P, Jacobs CA (2010) Rotational laxity greater in patients with contralateral anterior cruciate ligament injury than healthy volunteers. Knee Surg Sports Traumatol Arthrosc 18(10):1379–1384
Branch TP, Siebold R, Freedberg HI, Jacobs CA (2011) Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc 19(3):432–440
Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE Jr, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C, Jr., Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B (2006) Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med 34(9):1512–1532
Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR (1999) The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med 27(6):699–706
Hewett TE, Torg JS, Boden BP (2009) Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med 43(6):417–422
Hsu WH, Fisk JA, Yamamoto Y, Debski RE, Woo SL (2006) Differences in torsional joint stiffness of the knee between genders: a human cadaveric study. Am J Sports Med 34(5):765–770
Koga H, Nakamae A, Shima Y, Iwasa J, Myklebust G, Engebretsen L, Bahr R, Krosshaug T (2010) Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med 38(11):2218–2225
Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, Hewett TE, Bahr R (2007) Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med 35(3):359–367
Lorbach O, Wilmes P, Maas S, Zerbe T, Busch L, Kohn D, Seil R (2009) A non-invasive device to objectively measure tibial rotation: verification of the device. Knee Surg Sports Traumatol Arthrosc 17(7):756–762
Lorbach O, Wilmes P, Theisen D, Brockmeyer M, Maas S, Kohn D, Seil R (2009) Reliability testing of a new device to measure tibial rotation. Knee Surg Sports Traumatol Arthrosc 17(8):920–926
Markolf KL, Gorek JF, Kabo JM, Shapiro MS (1990) Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am 72(4):557–567
Musahl V, Bell KM, Tsai AG, Costic RS, Allaire R, Zantop T, Irrgang JJ, Fu FH (2007) Development of a simple device for measurement of rotational knee laxity. Knee Surg Sports Traumatol Arthrosc 15(8):1009–1012
Noyes FR, Cummings JF, Grood ES, Walz-Hasselfeld KA, Wroble RR (1991) The diagnosis of knee motion limits, subluxations, and ligament injury. Am J Sports Med 19(2):163–171
Park HS, Wilson NA, Zhang LQ (2008) Gender differences in passive knee biomechanical properties in tibial rotation. J Orthop Res 26(7):937–944
Quatman CE, Quatman-Yates CC, Hewett TE (2010) A ‘plane’ explanation of anterior cruciate ligament injury mechanisms: a systematic review. Sports Med 40(9):729–746
Schmitz RJ, Ficklin TK, Shimokochi Y, Nguyen AD, Beynnon BD, Perrin DH, Shultz SJ (2008) Varus/valgus and internal/external torsional knee joint stiffness differs between sexes. Am J Sports Med 36(7):1380–1388
Shoemaker SC, Markolf KL (1982) In vivo rotatory knee stability. Ligamentous and muscular contributions. J Bone Joint Surg Am 64(2):208–216
Shultz SJ, Schmitz RJ, Beynnon BD (2011) Variations in varus/valgus and internal/external rotational knee laxity and stiffness across the menstrual cycle. J Orthop Res 29(3):318–325
Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH (2007) Measurement of varus-valgus and internal-external rotational knee laxities in vivo—part I: assessment of measurement reliability and bilateral asymmetry. J Orthop Res 25(8):981–988
Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH (2007) Measurement of varus-valgus and internal–external rotational knee laxities in vivo—part II: relationship with anterior-posterior and general joint laxity in males and females. J Orthop Res 25(8):989–996
Tsai AG, Musahl V, Steckel H, Bell KM, Zantop T, Irrgang JJ, Fu FH (2008) Rotational knee laxity: reliability of a simple measurement device in vivo. BMC Musculoskelet Disord 9:35
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31(6):831–842
Weir JP (2005) Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 19(1):231–240
Woodford-Rogers B, Cyphert L, Denegar CR (1994) Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train 29(4):343–346
Acknowledgments
The present project is supported by the National Research Fund, Luxembourg.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mouton, C., Seil, R., Agostinis, H. et al. Influence of individual characteristics on static rotational knee laxity using the Rotameter. Knee Surg Sports Traumatol Arthrosc 20, 645–651 (2012). https://doi.org/10.1007/s00167-011-1877-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1877-2