Abstract
Static rotational knee laxity measurements have the advantages of precisely quantifying laxity and are thus potentially more objective than manual tests. Moreover, they can help to establish the diagnosis of knee injuries and to evaluate the success of reconstruction procedures after surgical intervention. As a consequence, they may systematically be part of follow-up to knee injuries (i.e. anterior cruciate ligament injuries). Numerous devices to measure knee rotation in a non-invasive manner exist. Although further efforts are necessary to improve the use of rotational laxity measurements in daily clinical practice, existing data on static rotational knee laxity measurements is encouraging to further investigate it in healthy and injured persons. Rotational knee laxity measurements allow (1) for the evaluation of the physiological knee laxity as a risk factor for knee injuries and poor reconstruction outcomes, (2) for the diagnosis of knee injuries (i.e. anterior cruciate ligament injuries) and (3) to follow knee ligament reconstructions postoperatively. The lack of knowledge of rotational knee laxity measurements in injured/reconstructed knees, however, prevents us to conclude the best treatment or reconstruction techniques. The present chapter aims to analyse the current knowledge and the potential for rotational knee laxity measurements to follow and individualise care for knee injuries and diseases.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Clinical assessment of knee laxity is useful prior to surgery to assist in establishing the diagnosis of knee injuries and after surgical intervention to evaluate the success of reconstruction procedures. Clinically, rotational knee laxity is evaluated by subjective manual tests, such as the dial or the pivot shift tests [27]. Whereas the former is ‘static’ and uniaxial, the latter is ‘dynamic’ and tests the knee in more than one direction [21]. There is a debate as to whether static or dynamic measurements should be preferred in the evaluation of anterior cruciate ligament (ACL) injuries [51]. While the pivot shift test is accepted to be more closely correlated with the clinical symptoms of dynamic instability (‘giving way’) than do static tests, it appears to be generally accepted that the latter are of interest in the diagnosis and follow-up of knee soft tissue injuries [51]. Moreover, static tests induce a less complex movement of the knee in comparison to dynamic tests, which may be easier to standardise and to control with a device. Increased attention has been paid over the last decade to develop instruments measuring static rotational knee laxity. To date, few data report rotational knee laxity measurements in vivo. A systematic review reported that in 74 articles where knee rotation was measured under a controlled load, 61 used human cadavers and only 13 using living humans [31]. Preliminary data showed that rotational knee laxity measurements are of a much higher degree of complexity compared with sagittal knee laxity measurements.
The aim of the present chapter is to provide an overview of current knowledge on static rotational knee laxity measurements.
2 Structures Influencing Knee Rotation: What Can We Measure?
Laxity tests must be utilised with caution; there is always more than one contributing structure in one direction being tested. As a consequence, it can be challenging to isolate the structure under investigation. Between 0° and 30° of knee flexion, internal rotation is primarily restrained by the posterior oblique ligament and the iliotibial band. Secondary restraints include the ACL, the superficial fibres of the medial collateral ligament (MCL), the menisci, the popliteal tendon and the anterolateral ligament (ALL). At 60° of knee flexion, internal rotation is first restrained by the deep fibres of the MCL and the iliotibial band and then by the ACL, the menisci, the popliteal tendon and the ALL. In terms of external rotation, at full extension of the knee, it is primarily restrained by the lateral collateral ligament (LCL) and secondly by the menisci, the deep fibres of the MCL and the popliteofibular ligament complex. From 30° to 90° of knee flexion, primary restraints of external rotation are the superficial fibres of the MCL, the LCL and the popliteal tendon. Secondary restraints are the posterior cruciate ligament (PCL), the menisci and the popliteofibular ligament complex [21].
As contributing structures vary with the degree of knee flexion, patient position and/or devices to measure static rotational knee laxity must be chosen in relation to the structure(s) to be analysed. For example, cadaver studies showed that the increase of rotation related to an ACL deficiency was apparent mainly between 0° and 30° of knee flexion and disappeared with further knee flexion [6, 53, 85]. ACL-injured patients should thus be assessed at a maximal angle of 30°. In knee flexion angles below 30°, the section of the ACL lead to 2.4–4° increase more specifically in internal rotation [32, 36, 42, 53]. The same amount of increment is observed in in vivo studies (rotation of the injured knee patients with a chronic ACL injury was increased by 3° compared to the healthy knee) [40]. Given the rather limited amount of additional rotation induced by the absence of the ACL, the challenge with non-invasive measurements is to reach a high degree of precision to detect such low changes.
3 Static Laxity Measurements: How to Start With?
Several factors related to patient positioning, measurement methods, testing protocols and device precision deserve particular consideration to correctly understand static rotational knee laxity measurements. Patient position (i.e. knee and hip flexion angles) influences laxity measurements. At a knee flexion of 20°, greater values of knee rotation are observed when the hip is near extension compared with when the hip is flexed at 90°. On the other hand, for a similar position of the hip, knee rotation is greater at 90° of knee flexion compared with 20° [59].
Devices also differ by measurement methods (location of sensors to measure torque applied and displacement). In all reported instruments, torque is applied at the foot. Consequently, the torque may partially be absorbed by the device and other joints of the leg than the knee joint. The final torque applied to the knee may thus differ between devices depending on efficacy to immobilise the hip and ankle joints. With regard to the measurement of rotation, some devices measure knee rotation at the foot [3, 11, 37] and others directly at the tibia [49, 55, 70]. For a 10 Nm torque, Shoemaker and Markolf estimated that foot rotation represented twice the tibiofemoral rotation, i.e. two-thirds of the measured angle [59]. This aspect is specific of each device depending on the fixation of the ankles and hips. However, foot rotation may be avoided with a direct evaluation of tibial rotation via electromagnetic sensors placed on the tibia [2].
Researchers and knee surgeons should also be aware how testing protocols are standardised. The amount of torque applied usually varied between 5 and 15 Nm depending on fixation and patient comfort within the device. These amounts of torque allow for a safe test as structural integrity of the knee ligaments are only compromised for a torque greater than 35 Nm directly applied to the tibia [59]. Several researchers have shown improved reliability for total range of rotation than for internal and external rotation separately [3, 85]. Most researchers apply this torque from internal to external rotation or from external to internal rotation to obtain a complete cycle of rotation. In these cases, the hysteresis phenomenon should not be neglected as it may influence the reproducibility of the measurements. A solution to avoid this phenomenon is to perform separate measurements of internal and external rotation and includes ‘preconditioning trials’ [12, 44, 66]. A lack of reproducibility may also be explained by a non-reproducible starting position of the test, an aspect related to patient installation that should be carefully monitored.
All of the previously mentioned aspects influence the precision of the device, which remains poorly investigated. The determination of precision is, however, necessary to draw meaningful conclusions from any comparison study as it accounts for the measurement error. It is helpful to detect abnormalities occurring during a subject follow-up and helps to conclude if an observed difference is clinically relevant and meaningful. Studies are often limited to computations of ICCs, which depend strongly on data dispersion and do not provide a clear understanding of device precision. A conservative approach is the use of the minimum detectable change (MDC) [82]. The MDC represents the minimal required difference with a given instrument in a defined setting to be confident that a true change has indeed occurred.
4 Static Rotational Knee Laxity Devices: How to Measure Knee Rotation?
Knee laxity measurement devices have been specifically designed to allow for an objective and standardised evaluation of knee laxity. The authors present non-invasive devices measuring knee rotation angle in humans with a known applied torque (Fig. 13.1). Instruments associated to imaging and/or assessing complex knee movements like the pivot shift test or the rotation associated with anterior or valgus movement of the knee will not be presented. To the best of the authors knowledge, none of the devices reported below are presently commercialised.
4.1 Genucom Knee Analysis System (FARO Medical Technologies, Montreal, Ontario, Canada) [54]
This device was developed in the late 1980s and allows measurement of anteroposterior laxity, as well as rotational and varus-valgus laxity [54]. A six-degrees-of-freedom dynamometer indicates to the examiner the force or torque applied to the knee, and an electrogoniometer measures the displacement. The ability of the device to measure rotation has been poorly explored. This may be partly explained by a poor reproducibility. Indeed, at 20° of knee flexion, the least significant difference reached 17.5° in tibial rotation; in other words, a change of 17.5° is required to indicate a real change in one subject’s laxity [43].
4.2 Vermont Knee Laxity Device [77]
The Vermont knee laxity device measures anterior, rotational and varus-valgus laxity. The subject lies supine with knees flexed at 20° and hips at 10°, and the thighs are fixed with clamps at the femoral epicondyles. Rotation angle is measured on tibia through electromagnetic sensors. The intraclass correlation coefficient (ICC) is above 0.86 for internal, external and total range of rotation. The 95 % confidence interval (CI) of the absolute measurement errors were evaluated to reach 5–7°, respectively, for internal and external rotation [70].
4.3 Rottometer [3]
The patient sits on a modified chair with knees and hips flexed to 90°. To limit artefacts and target tibiofemoral rotation, the thigh is fixed above the knee with clamps. The ankle is fixed by two screws at the calcaneus and four screws placed at the medial and lateral malleoli. An adjustable spanner is used to apply torque and a stick following the foot plate indicated the resulting degree of rotation. A comparative study using radiostereometry analysis (RSA) demonstrated that the Rottometer systematically overestimated tibiofemoral rotation by about 100 % [3]. Depending on the amount of torque and degree of knee flexion, the inter-rater ICC varied between 0.49 and 0.85, with the highest ICC obtained for the highest torque (9 Nm) and the higher degree of knee flexion (90°) [4]. The 95 % CI between measurements of both examiners varied between −7.9° for the lower bound and 3.8° for the upper bound [4].
4.4 Device by Musahl et al. [49]
This device consists of an Aircast Foam Walker boot with a 6-degrees-of-freedom moment sensor fixed on a handle bar attached to the boot. A bubble level attached to the handle bar determines the neutral rotation. To measure the relative rotation of the tibia with regard to the femur, magnetic sensors are placed on the boot, on the medial surface of the proximal tibia and on the anterior surface of the thigh. The examiner holds the leg while applying the torque, which may influence muscle relaxation and flexion angles. An initial cadaver study reported a high intra- and inter-rater ICC (>0.94) [49]. In 11 healthy subjects, inter-rater ICC was greatest at 90° of knee flexion (0.88). The 95 % CI of the standard error of measurements reached 3.2° for the total range at 90° of knee flexion and 5.1° at 30° [76]. The average side-to-side difference between normal knees was reported to be 3.5° [76].
4.5 Device by Park et al. [55]
Park et al. [55] presented the first motorised device to measure knee rotational laxity. The patient sits in a modified chair with the hips flexed at 85° and knees at 60°. The thighs are fixed with clamps. Three LED markers were positioned on the anteromedial surface of the tibia to measure the angle of rotation. No data is available on its reproducibility.
4.6 Rotameter [37]
Two prototypes of the Rotameter exist. In both versions, the subject is lying prone to reproduce the dial test position. Thighs are fixed in half cones with Velcro strap band. Hips are extended and knees flexed at 30°. The subject is wearing boots (home-made boot in the first version and ski boots of appropriated size in the second version) attached to the handle bar that allows both to apply the torque and measure the degree of rotation. A cadaver study showed a high correlation (Pearson r > 0.85) between measurements of the first prototype and knee navigation system [36, 37]. The Rotameter, however, overestimates the total range of rotation at 5, 10 and 15 Nm in average of 5, 10 and 25°, respectively [37]. The assessment of the reliability of the first Rotameter is questionable. Greater ICC were observed for inter-tester reliability (>0.88) compared with intra-rater ICC (>0.67), suggesting that participants were not reinstalled between the measurements undertaken by the two examiners [38]. No confidence intervals for measurement errors were reported. Regarding the second version of the Rotameter, it provides lower rotation than the first device due to improvements in the standardisation of the patient installation and joint fixation. The MDC has been determined to reach 4.2° for internal rotation and 5.9° for external rotation [45]. Individualised normative references have been established considering individual characteristics [44, 45].
4.7 Robotic Knee Testing System [ 11 ]
Branch et al. developed a custom robotic knee system adjustable to the patient’s natural lower limb alignment to avoid pretension in leg anatomical structures. The patient lies supine with knees flexed at 25°. The femur and patella are stabilised with clamps, and the ankle is stabilised in pronation and dorsiflexion to limit its rotation during the test. Rotation is measured at the foot with an inclinometer. Electromagnetic sensors placed on the proximal tibia showed that tibial rotation represented in average 48.7 % of the total rotation measured at the foot [11]. The authors corrected their measurements according to these results, which may introduce bias, as this correction may vary between individuals (95 % CI: 45.3–52.1 %). Inter-rater ICC for total range of rotation reached 0.97 at a torque of 5.65 Nm [11].
4.8 Rotational Measurement Device [1]
This device consists of three parts: (1) a femoral clamp and (2) a tibial splint, to which inclinometers are fixed to measure rotation and (3) a boot with a torque wrench. Subjects are positioned at 90° of knee flexion. Measurements at the foot overestimate rotation in average by 136 % (95 % CI, −102 % to −171 %) compared to the rotational measurement device placed on the tibia. The latter slightly overestimated rotation (in average 2°: 95 % CI −4.5° to 0.4°) when compared to electromagnetic sensors placed on the tibia [1]. Intra-rater ICC reached 0.9 [1].
Fact Box 1
-
Static rotational knee laxity only assesses knee rotation. Dynamic tests constrain the knee in more than one direction (i.e. pivot shift test).
-
Structures contributing to knee rotation are numerous (menisci, lateral ligaments …) and depend on the degree of knee flexion.
-
Rotational knee laxity measurements are of a much higher degree of complexity compared to anterior knee laxity measurements.
-
To date, eight devices have been reported with measurements of rotational knee laxity in vivo. The torque applied varies between 5 and 15 Nm. The report of their precision is insufficient for proper use in the daily practice.
-
Hip flexion, knee flexion, location of sensors to measure torque applied and rotation, as well as testing protocols, critically influence rotational laxity results.
5 Rotational Laxity in the Normal Knee
Physiological knee laxity is the natural laxity of the knee. Recent literature reveals that physiological knee laxity may influence injury risk, as well as treatment outcomes. As such, a better understanding of physiological laxity may benefit both athletes and injured patients alike.
5.1 Relation with Knee Function
It is commonly accepted that knee laxity has no relation to knee function. In fact, the literature specifies that the amount of side-to-side difference in knee laxity observed after ACL reconstruction is not linked to clinical outcomes [22, 30, 56]. Nevertheless, subjects with excessive physiological knee laxity have been reported to have movement patterns associated with non-contact ACL injury mechanisms. They display greater hip and knee movements in the transverse, sagittal and frontal planes during drop landings [65, 75]. Subjects with higher anterior knee laxity also display increased knee moments [69] and delayed onset timing of muscle activation that is compensated by a higher muscle activity [60]. Moments and onset timing of muscle activation have not yet been investigated for patients with higher rotational knee laxity. These primary findings suggest that individuals may benefit from intensive neuromuscular training adapted to their laxity profile, which could have a direct impact in knee injury prevention and patient care.
5.2 Risk Factor for Injuries
It is well recognised that hypermobility (as defined by the Beighton score [8]) is associated with an increased risk of musculoskeletal injuries [83]. The same principle may apply to physiological rotational knee laxity. In adulthood, as for anterior knee laxity [78, 84], the healthy contralateral knee of ACL-injured patients displays, on average, greater internal rotation than healthy knees of a control group [11, 46]. Mouton et al. set a threshold to help discriminate rotational knee laxity between healthy subjects and the healthy contralateral knee of ACL-injured patients [46]. Above the established threshold, a subject was 2.45-fold (95 % CI 1.37–4.36) more likely to be in the injured group [46]. These findings must be confirmed by prospective studies, but they suggest that prospective screening may be of interest to identify subjects at risk for non-contact ACL injuries as well as for other knee injuries.
5.3 Risk for Poor Reconstruction Outcomes
After ACL reconstruction with a bone-patellar tendon-bone graft, patients identified with an increased physiological rotational laxity have lower Lysholm [29] and IKDC subjective [12, 29] scores. As preoperative scores were not reported, it remains unclear whether this finding is the consequence of the ACL reconstruction or of the injury itself. Still, these results raise the question of whether patients with higher knee laxity may benefit from adapted, individualised care (i.e. graft choice) compared with other patients.
5.4 Influencing Factors
Previous studies have demonstrated that external rotation exceeds internal rotation by approximately 50 % [11, 38, 48, 55, 70]. However, the study of rotational knee laxity is much more complex than simply measuring internal and external rotation. Physiological laxity is indeed influenced by several individual characteristics. Females have greater rotational knee laxity than males [5, 11, 26, 44, 45, 55] and body mass appears to be inversely correlated to rotational knee laxity [44, 45, 61]. No relation has been reported between height and rotational knee laxity [44, 45].
Increased knee laxity in the paediatric population is generally well accepted [7, 17, 23]. Rotational knee laxity evolves during the adolescence and stabilises at the age of 14 years in girls and at 16 years in boys [7]. This stiffening of knee laxity coincides with the emergence of ACL injuries [14]. In adulthood, the influence of age is debated [5, 61]. Shultz et al. reported that older subjects had lower laxities. However, these researchers in their study did not include a large range of age: males were 22 ± 3 years old and females were 21 ± 3 years old [61]. In contrast, in two studies with large number of subjects and including subjects with a large range of age, no significant influence of age could be observed neither in males nor females [5, 44, 45].
While several studies suggest that anterior knee laxity may vary during the menstrual cycle of females [62, 63], the effect of the menstrual cycle on rotational knee laxity has been analysed in only one study [66]. The authors assessed rotational knee laxity in females at two different time points. Based on previous research of these authors [64], the two time points were the estimated days of minimum and maximum anterior knee laxity during menses and the early luteal phase, respectively. No increase in rotational knee laxity could be observed in females between these two time points [66].
A relation may exist between knee laxity and lower leg alignment. Healthy subjects with increased laxity compared with subjects with decreased laxity have greater navicular drop (increased: 7.1 ± 5.0 mm, decreased: 5.2 ± 3.1 mm), lower Q-angle (increased: 12.9 ± 3.9°, decreased: 11.6 ± 4.7°), lower tibial torsion (increased: 14.8 ± 7.3°, decreased: 18.6 ± 5.2°), lower quadriceps peak torque (increased: 2.3 ± 0.4 Nm/kg, decreased: 2.5 ± 0.4 Nm/kg) and shorter femur length (increased: 41.3 ± 2.6 cm, decreased: 44.5 ± 2.5 cm) [61]. Some differences are, however, minor and their clinical value has not yet been established. Another study established that subjects with foot pronation displayed higher internal rotation than subjects without pronation [13].
Physical activity has also been reported to influence rotational knee laxity. Shultz et al. measured rotational knee laxity in 59 participants during an intermittent exercise protocol [67]. The measurements were performed before and after warm-up and every 15 min during and for 1 h after the end of the exercise. The largest mean change observed was 1.7 ± 4.9° (increase of 7 % compared to before warm-up) [67]. Thirty-three percent of each sex had an increment superior to 5.2°, thereby suggesting that all participants may not respond in a similar way to an exercise. The study of Shultz et al. therefore confirms previous studies, which showed increased rotational knee laxity associated with exercise [28, 73]. Interestingly, as rotational knee laxity increases with exercise, women tend to have greater knee valgus and more absorbed energy at the knee [68]. The importance of the valgus is related to the subject’s physiological knee laxity [68].
Finally, osteoarthritis may affect knee laxity. Cross-sectional studies have found that rotational laxity [80] decreased with the severity of knee osteoarthritis. It may thus be useful to consider osteoarthritis as a potential confounding factor in future studies [52].
5.5 Normative References
To define ‘excessive’ knee laxity, normative references for each device must first be established in order to define ‘normal’ laxity. Mouton et al. proposed a methodological approach to calculate standardised laxity scores for anterior and rotational knee laxity taking into account influencing individual characteristics [45]. For rotational knee laxity, sex and body mass were found to significantly influence its measure and to explain a non-negligible amount of the variability in internal and external rotation (46–60 %). As a consequence, the latter parameters were taken into account to calculate an individualised score. The individualisation of scores has the advantage to allow for the direct comparison of individuals, regardless of differences in sex or body mass. The final score represents the distance of the individual to the average of the healthy control group. One unit represents the standard deviation of the healthy control group. As one standard deviation has already been previously used as a threshold [78], the authors decided to use it to categorise knees as being hypo- (score < −1), normo- (score between −1 and 1) and hyperlax (score > 1) [45]. For internal and external rotation, the individualised scores follow a normal distribution (Figs. 13.2 and 13.3).
Distribution of the knee laxity score for internal rotation at 5 Nm corrected for sex and body mass [31]
Distribution of the knee laxity score for external rotation at 5 Nm corrected for sex and body mass [31]
Anterior and rotational knee laxity are poorly correlated [45, 71], which suggests that they yield complementary information. A single measure of knee laxity is thus likely inappropriate to describe the static knee laxity envelope. The existence of specific knee laxity profiles has been suggested [61]. Mouton et al. showed by combining the anterior displacement to internal and external rotation that only 32 % of the participants showed a normal profile (scores > −1 and <1 for all three directions), 33 % were concerned by hyperlaxity in at least one direction, 40 % by hypolaxity in at least one direction and 5 % by both (Fig. 13.4). The diversity of the identified laxity profiles highlights both the complexity of the interpretation of multidirectional knee laxity and the necessity for individualised care of knee injuries and diseases.
Distribution of laxity profiles expressed in percentage (%). Decreased: laxity score < −1, normal: laxity score between −1 and 1, increased: laxity score >1. ATD200 anterior tibial displacement at 200 N, IR5 internal rotation at 5 Nm, ER5 external rotation at 5 Nm [31]
Fact Box 2
-
Subjects with excessive physiological knee laxity have been reported to display greater knee movements and moments and delayed muscle onset compensated by a higher muscle activity.
-
Excessive physiological knee laxity may play a role in the risk of knee injuries and may influence outcomes after ligament, e.g. ACL reconstruction.
-
External rotation has been reported to be 50 % greater than internal rotation.
-
Physiological rotational knee laxity may be influenced by many individual characteristics such as sex, body mass, age, menstrual cycle, lower leg alignment, osteoarthritis, as well as exercise. These parameters can be considered in the establishment of normative references.
-
A single measure of knee laxity is inappropriate to describe knee laxity. The interpretation of knee laxity profiles is complex and still at a very early stage.
6 Rotational Laxity in the Injured Knee
In contrast to physiological knee laxity, which only considers the healthy knee, pathological laxity typically considers the laxity of the injured knee and its difference against the contralateral knee.
Laxity measurements can be useful to establish the diagnosis of ACL injuries in complement to the clinical and imaging evaluation. Presently, the diagnosis of ACL injuries with arthrometers mainly focuses on anterior laxity measurements. However, concomitant measures of additional laxities, such as rotational knee laxity, have been proposed to refine the diagnosis of ACL injuries [16]. In cadaver studies, the section of the ACL leads to an increment of tibial internal rotation of 2.4–4° [32, 36, 42, 53]. Similar increase of 3° in tibial internal rotation could be observed in vivo [40]. More specifically, the posterolateral bundle may play a role in restraining rotation as its section induced the major increase in internal rotation [36].
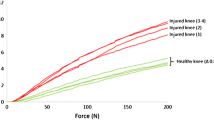
To date, only the sensitivity and specificity of the Rotameter to detect an ACL injury has been reported in the literature [47]. A threshold of 3.2° for the side-to-side difference in internal rotation at 5 Nm led to correctly identify 38 % of patients (sensitivity) and reject 95 % of healthy subjects (specificity) (Fig. 13.5). Although the sensitivity of the Rotameter seems extremely low, it is still superior to the sensitivity of 24 % reported for the pivot shift test in a previous meta-analysis [9]. Moreover, compared with the common analysis of anterior displacement (side-to-side difference in anterior displacement at 200 N), further analysis of knee internal rotation increased the diagnostic sensitivity by 9 % (from 75 to 84 %) [47]. To further improve the diagnosis of ACL injuries, consideration of the slope of the curves (representative of knee stiffness) is advised as it has been shown to increase the specificity of anterior and rotational knee laxity tests to 100 %. As a result, simultaneous consideration of displacement and knee stiffness provide a test without a false positive [47].
It should be highlighted that associated injuries such as meniscal or collateral ligament injury may influence the interpretation of laxity measurements in the diagnosis of ACL injuries [25, 72, 81] but remain poorly considered. Only 40 % of ACL ruptures are, however, reported to be isolated [19].
Rotational knee laxity measurements may also be of interest in posterolateral corner injuries. These injuries induce an increase in tibial external rotation [79] of 6–14° [33, 39, 41], resulting in posterolateral rotational instability. This increment is much more important than in terms of an ACL injury and may also be easier to detect. Clinically, posterolateral corner injuries are assessed with the dial test [20]. An increment greater than or equal to 15° in the injured knee suggests a posterolateral injury [20]. The dial test does not allow for an objective assessment of posterolateral rotatory instability but to the author’s knowledge, results of instrumented measurements have never been reported in such injuries.
Finally, as knee osteoarthritis affects rotational knee laxity [80], rotational knee laxity measurements may have the potential to be an indicator of the type and severity of osteoarthritis.
7 Rotational Laxity in the Reconstructed Knee
Ideally, knee reconstruction surgery aims to restore knee laxity in all directions and prevent further degeneration of the knee joint. Therefore, knee laxity measurements are of interest after surgery as a postoperative control to follow the graft evolution and detect potential anomalies like elongation, recurrent tears, etc.
After ACL reconstruction, patient follow-up remains based on manual tests and/or on anterior knee laxity measurements. Most studies considering knee rotation analysed the pivot shift test and as such, a paucity of data exists regarding static rotational knee laxity measurements. However, these may help to detect anomalies because increased postoperative laxities may be observed in graft malpositioning [34, 57] or graft failures [18].
The effect of ACL reconstruction on rotational knee laxity and its evolution after reconstruction are not known yet. Lorbach et al. [35] reported no significant differences in static rotational knee laxity between the reconstructed and non-injured knee 27 months after ACL reconstructive surgery with a bone-patellar tendon-bone graft. Moreover, Branch et al. showed that the side-to-side differences in internal rotation did not differ between single- and double- reconstruction techniques using a semitendinosus and gracilis graft [12]. These researchers, however, did not report preoperative laxity measurements; it is thus not possible to conclude whether the ACL reconstruction reduces rotational knee laxity or whether it was already normal in these patients before surgery. Moreover, they only measured laxity at a single time point during patient follow-up.
To date, the knowledge on postoperative laxity is also insufficient to conclude on the best reconstructive technique to restore rotational knee laxity in an injured knee. With a navigation system, Bignozzi et al. demonstrated that the total range of rotation (internal and external rotation) was significantly reduced after anatomical double-bundle ACL reconstruction [10]. Moreover, Hofbauer et al. demonstrated that, using a navigation system, an anatomic double-bundle reconstruction technique reduced significantly more internal rotation (15.6°) than did an anatomic single-bundle ACL reconstruction (7.1°) [24]. A systematic review, however, showed that anatomic double-bundle ACL reconstruction did not lead neither to a lower grade of pivot shift test compared with single-bundle nor to a greater reduction in rotational knee laxity [15].
Postoperative knee laxity measurements are poorly considered after many other surgical interventions. It has, for example, been shown that medial meniscectomy will influence knee laxity [50, 58]. As for posterolateral corner injuries, Tardy et al. reported for the first time in vivo static rotational knee laxity after anatomic posterolateral corner reconstruction [74]. External rotation was in average similar to a healthy control group after reconstruction. However, the authors found a remaining significant increase in internal rotation of the tibia in 40 % of patients. They assumed that this finding was either due to the surgical technique or to associated lesions and/or unrecognised soft tissue damage at the time of injury.
Fact Box 3
-
Rotational knee laxity measurements in combination with anterior knee laxity measurements improve the diagnosis of ACL injuries. They may also help to establish the diagnosis of posterolateral corner injuries.
-
The diagnosis of ACL injuries may be skewed by associated injuries to structures also contributing to knee rotation.
-
Rotational knee laxity measurements can improve the follow-up of knee injuries and diseases especially after knee reconstruction if used as a postoperative control (i.e. ACL or posterolateral corner injury). No prospective follow-up of patients was however reported.
8 Conclusions
Knee laxity measurements should be perceived as a supplement to clinical tests and imaging techniques. They should be systematically performed in order to assist the clinician with establishing a diagnosis and follow-up of knee injuries to systematically identify any abnormal evolution.
The development of arthrometers to measure static rotational knee laxity is relatively new and further studies are needed to develop further understanding. To date, we know that external rotation is greater than internal rotation and that females have greater rotational knee laxity than males. Moreover, body mass is inversely correlated to rotational knee laxity measurements. Other influencing factors remain under investigation.
The interest in physiological knee laxity is growing. Subjects with excessive physiological knee laxity are reported to have movement patterns associated with non-contact ACL injuries. This may partly explain why an increased laxity was observed in the healthy contralateral knee of ACL-injured subjects compared with a control group. This excessive physiological knee laxity may also explain inferior outcomes after an ACL reconstruction. As a consequence of this growing interest, the need for normative references has emerged. However, the analysis of either rotational or multidirectional knee laxity as well to the consideration of influencing factors lead to a high complexity of knee laxity profiles.
Recently, rotational knee laxity measurements have been shown to improve the diagnosis of ACL injuries as performed with anterior knee laxity measurements. This should encourage researchers to evaluate the diagnostic power of their own devices. The knowledge about postoperative rotational knee laxity measurements is evolving. The choice of reconstruction, the effect of reconstruction and its evolution are still insufficiently understood.
Static rotational knee laxity measurements offer the possibility to improve the understanding of physiological, pathological and reconstructed knee laxity and may help individualise the care of knee injuries and diseases.
References
Alam M, Bull AM, Thomas R, Amis AA (2013) A clinical device for measuring internal-external rotational laxity of the knee. Am J Sports Med 41(1):87–94
Alam M, Bull AM, Thomas RD, Amis AA (2011) Measurement of rotational laxity of the knee: in vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med 39(12):2575–2581
Almquist PO, Arnbjornsson A, Zatterstrom R, Ryd L, Ekdahl C, Friden T (2002) Evaluation of an external device measuring knee joint rotation: an in vivo study with simultaneous Roentgen stereometric analysis. J Orthop Res 20(3):427–432
Almquist PO, Ekdahl C, Isberg PE, Friden T (2011) Measurements of knee rotation-reliability of an external device in vivo. BMC Musculoskelet Disord 12:291
Almquist PO, Ekdahl C, Isberg PE, Friden T (2013) Knee rotation in healthy individuals related to age and gender. J Orthop Res 31(1):23–28
Andersen HN, Dyhre-Poulsen P (1997) The anterior cruciate ligament does play a role in controlling axial rotation in the knee. Knee Surg Sports Traumatol Arthrosc 5(3):145–149
Baxter MP (1988) Assessment of normal pediatric knee ligament laxity using the genucom. J Pediatr Orthop 8(5):546–550
Beighton P, Horan F (1969) Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br 51(3):444–453
Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther 36(5):267–288
Bignozzi S, Zaffagnini S, Lopomo N, Fu FH, Irrgang JJ, Marcacci M (2010) Clinical relevance of static and dynamic tests after anatomical double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18(1):37–42
Branch TP, Browne JE, Campbell JD, Siebold R, Freedberg HI, Arendt EA, Lavoie F, Neyret P, Jacobs CA (2010) Rotational laxity greater in patients with contralateral anterior cruciate ligament injury than healthy volunteers. Knee Surg Sports Traumatol Arthrosc 18(10):1379–1384
Branch TP, Siebold R, Freedberg HI, Jacobs CA (2011) Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc 19(3):432–440
Coplan JA (1989) Rotational motion of the knee: a comparison of normal and pronating subjects. J Orthop Sports Phys Ther 10(9):366–369
Csintalan RP, Inacio MC, Funahashi TT (2008) Incidence rate of anterior cruciate ligament reconstructions. Perm J 12(3):17–21
Desai N, Bjornsson H, Musahl V, Bhandari M, Petzold M, Fu FH, Samuelsson K (2014) Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22(5):1009–1023
Di Iorio A, Carnesecchi O, Philippot R, Farizon F (2014) Multiscale analysis of anterior cruciate ruptures: prospective study of 49 cases. Orthop Traumatol Surg Res 100(7):751–754
Flynn JM, Mackenzie W, Kolstad K, Sandifer E, Jawad AF, Galinat B (2000) Objective evaluation of knee laxity in children. J Pediatr Orthop 20(2):259–263
George MS, Dunn WR, Spindler KP (2006) Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med 34(12):2026–2037
Granan LP, Forssblad M, Lind M, Engebretsen L (2009) The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop 80(5):563–567
Grood ES, Stowers SF, Noyes FR (1988) Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 70(1):88–97
Halewood C, Amis AA (2015) Clinically relevant biomechanics of the knee capsule and ligaments. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3594-8
Higuchi H, Terauchi M, Kimura M, Kobayashi A, Takeda M, Watanabe H, Takagishi K (2003) The relation between static and dynamic knee stability after ACL reconstruction. Acta Orthop Belg 69(3):257–266
Hinton RY, Rivera VR, Pautz MJ, Sponseller PD (2008) Ligamentous laxity of the knee during childhood and adolescence. J Pediatr Orthop 28(2):184–187
Hofbauer M, Valentin P, Kdolsky R, Ostermann RC, Graf A, Figl M, Aldrian S (2010) Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(9):1201–1207
Hsieh HH, Walker PS (1976) Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am 58(1):87–93
Hsu WH, Fisk JA, Yamamoto Y, Debski RE, Woo SL (2006) Differences in torsional joint stiffness of the knee between genders: a human cadaveric study. Am J Sports Med 34(5):765–770
Jakob RP, Staubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br 69(2):294–299
Johannsen HV, Lind T, Jakobsen BW, Kroner K (1989) Exercise-induced knee joint laxity in distance runners. Br J Sports Med 23(3):165–168
Kim SJ, Choi DH, Mei Y, Hwang BY (2011) Does physiologic posterolateral laxity influence clinical outcomes of anterior cruciate ligament reconstruction? J Bone Joint Surg Am 93(21):2010–2014
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32(3):629–634
Lam MH, Fong DT, Yung PS, Chan KM (2012) Biomechanical techniques to evaluate tibial rotation. A systematic review. Knee Surg Sports Traumatol Arthrosc 20(9):1720–1729
Lane JG, Irby SE, Kaufman K, Rangger C, Daniel DM (1994) The anterior cruciate ligament in controlling axial rotation. An evaluation of its effect. Am J Sports Med 22(2):289–293
LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32(6):1405–1414
Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H, Kim CH (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23(7):771–778
Lorbach O, Kieb M, Brogard P, Maas S, Pape D, Seil R (2012) Static rotational and sagittal knee laxity measurements after reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 20(5):844–850
Lorbach O, Pape D, Maas S, Zerbe T, Busch L, Kohn D, Seil R (2010) Influence of the anteromedial and posterolateral bundles of the anterior cruciate ligament on external and internal tibiofemoral rotation. Am J Sports Med 38(4):721–727
Lorbach O, Wilmes P, Maas S, Zerbe T, Busch L, Kohn D, Seil R (2009) A non-invasive device to objectively measure tibial rotation: verification of the device. Knee Surg Sports Traumatol Arthrosc 17(7):756–762
Lorbach O, Wilmes P, Theisen D, Brockmeyer M, Maas S, Kohn D, Seil R (2009) Reliability testing of a new device to measure tibial rotation. Knee Surg Sports Traumatol Arthrosc 17(8):920–926
Markolf KL, Graves BR, Sigward SM, Jackson SR, McAllister DR (2007) Effects of posterolateral reconstructions on external tibial rotation and forces in a posterior cruciate ligament graft. J Bone Joint Surg Am 89(11):2351–2358
Markolf KL, Kochan A, Amstutz HC (1984) Measurement of knee stiffness and laxity in patients with documented absence of the anterior cruciate ligament. J Bone Joint Surg Am 66(2):242–252
McCarthy M, Camarda L, Wijdicks CA, Johansen S, Engebretsen L, Laprade RF (2010) Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med 38(8):1674–1681
McQuade KJ, Crutcher JP, Sidles JA, Larson RV (1989) Tibial rotation in anterior cruciate deficient knees: an in vitro study. J Orthop Sports Phys Ther 11(4):146–149
McQuade KJ, Sidles JA, Larson RV (1989) Reliability of the genucom knee analysis system. A pilot study. Clin Orthop Relat Res 245:216–219
Mouton C, Seil R, Agostinis H, Maas S, Theisen D (2012) Influence of individual characteristics on static rotational knee laxity using the Rotameter. Knee Surg Sports Traumatol Arthrosc 20(4):645–651
Mouton C, Seil R, Meyer T, Agostinis H, Theisen D (2014) Combined anterior and rotational laxity measurements allow characterizing personal knee laxity profiles in healthy individuals. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3244-6
Mouton C, Theisen D, Meyer T, Agostinis H, Nuhrenborger C, Pape D, Seil R (2015) Noninjured knees of patients with noncontact ACL injuries display higher average anterior and internal rotational knee laxity compared with healthy knees of a noninjured population. Am J Sports Med 43(8):1918–1923
Mouton C, Theisen D, Meyer T, Agostinis H, Nührenbörger C, Pape D, Seil R (2015) Combined anterior and rotational knee laxity measurements improve the diagnosis of anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3757-7
Mouton C, Theisen D, Pape D, Nuhrenborger C, Seil R (2012) Static rotational knee laxity in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 20(4):652–662
Musahl V, Bell KM, Tsai AG, Costic RS, Allaire R, Zantop T, Irrgang JJ, Fu FH (2007) Development of a simple device for measurement of rotational knee laxity. Knee Surg Sports Traumatol Arthrosc 15(8):1009–1012
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38(8):1591–1597
Musahl V, Seil R, Zaffagnini S, Tashman S, Karlsson J (2012) The role of static and dynamic rotatory laxity testing in evaluating ACL injury. Knee Surg Sports Traumatol Arthrosc 20(4):603–612
Myklebust G, Bahr R (2005) Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med 39(3):127–131
Nielsen S, Ovesen J, Rasmussen O (1984) The anterior cruciate ligament of the knee: an experimental study of its importance in rotatory knee instability. Arch Orthop Trauma Surg 103(3):170–174
Oliver JH, Coughlin LP (1987) Objective knee evaluation using the Genucom Knee Analysis System. Clinical implications. Am J Sports Med 15(6):571–578
Park HS, Wilson NA, Zhang LQ (2008) Gender differences in passive knee biomechanical properties in tibial rotation. J Orthop Res 26(7):937–944
Pollet V, Barrat D, Meirhaeghe E, Vaes P, Handelberg F (2005) The role of the Rolimeter in quantifying knee instability compared to the functional outcome of ACL-reconstructed versus conservatively-treated knees. Knee Surg Sports Traumatol Arthrosc 13(1):12–18
Rupp S, Muller B, Seil R (2001) Knee laxity after ACL reconstruction with a BPTB graft. Knee Surg Sports Traumatol Arthrosc 9(2):72–76
Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 34(5):721–732
Shoemaker SC, Markolf KL (1982) In vivo rotatory knee stability. Ligamentous and muscular contributions. J Bone Joint Surg Am 64(2):208–216
Shultz SJ, Carcia CR, Perrin DH (2004) Knee joint laxity affects muscle activation patterns in the healthy knee. J Electromyogr Kinesiol 14(4):475–483
Shultz SJ, Dudley WN, Kong Y (2012) Identifying multiplanar knee laxity profiles and associated physical characteristics. J Athl Train 47(2):159–169
Shultz SJ, Kirk SE, Johnson ML, Sander TC, Perrin DH (2004) Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exerc 36(7):1165–1174
Shultz SJ, Levine BJ, Nguyen AD, Kim H, Montgomery MM, Perrin DH (2010) A comparison of cyclic variations in anterior knee laxity, genu recurvatum, and general joint laxity across the menstrual cycle. J Orthop Res 28(11):1411–1417
Shultz SJ, Sander TC, Kirk SE, Perrin DH (2005) Sex differences in knee joint laxity change across the female menstrual cycle. J Sports Med Phys Fitness 45(4):594–603
Shultz SJ, Schmitz RJ (2009) Effects of transverse and frontal plane knee laxity on hip and knee neuromechanics during drop landings. Am J Sports Med 37(9):1821–1830
Shultz SJ, Schmitz RJ, Beynnon BD (2011) Variations in varus/valgus and internal/external rotational knee laxity and stiffness across the menstrual cycle. J Orthop Res 29(3):318–325
Shultz SJ, Schmitz RJ, Cone JR, Copple TJ, Montgomery MM, Pye ML, Tritsch AJ (2013) Multiplanar knee laxity increases during a 90-min intermittent exercise protocol. Med Sci Sports Exerc 45(8):1553–1561
Shultz SJ, Schmitz RJ, Cone JR, Henson RA, Montgomery MM, Pye ML, Tritsch AJ (2015) Changes in fatigue, multiplanar knee laxity, and landing biomechanics during intermittent exercise. J Athl Train 50(5):486–497
Shultz SJ, Schmitz RJ, Nguyen AD, Levine BJ (2010) Joint laxity is related to lower extremity energetics during a drop jump landing. Med Sci Sports Exerc 42(4):771–780
Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH (2007) Measurement of varus-valgus and internal-external rotational knee laxities in vivo – part I: assessment of measurement reliability and bilateral asymmetry. J Orthop Res 25(8):981–988
Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH (2007) Measurement of varus-valgus and internal-external rotational knee laxities in vivo – part II: relationship with anterior-posterior and general joint laxity in males and females. J Orthop Res 25(8):989–996
Slocum DB, Larson RL (2007) Rotatory instability of the knee: its pathogenesis and a clinical test to demonstrate its presence. 1968. Clin Orthop Relat Res 454:5–13; discussion 13–14
Stoller DW, Markolf KL, Zager SA, Shoemaker SC (1983) The effects of exercise, ice, and ultrasonography on torsional laxity of the knee. Clin Orthop Relat Res 174:172–180
Tardy N, Mouton C, Boisrenoult P, Theisen D, Beaufils P, Seil R (2014) Rotational profile alterations after anatomic posterolateral corner reconstructions in multiligament injured knees. Knee Surg Sports Traumatol Arthrosc 22(9):2173–2180
Torry MR, Myers C, Pennington WW, Shelburne KB, Krong JP, Giphart JE, Steadman JR, Woo SL (2011) Relationship of anterior knee laxity to knee translations during drop landings: a bi-plane fluoroscopy study. Knee Surg Sports Traumatol Arthrosc 19(4):653–662
Tsai AG, Musahl V, Steckel H, Bell KM, Zantop T, Irrgang JJ, Fu FH (2008) Rotational knee laxity: reliability of a simple measurement device in vivo. BMC Musculoskelet Disord 9:35
Uh BS, Beynnon BD, Churchill DL, Haugh LD, Risberg MA, Fleming BC (2001) A new device to measure knee laxity during weightbearing and non-weightbearing conditions. J Orthop Res 19(6):1185–1191
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31(6):831–842
Veltri DM, Deng XH, Torzilli PA, Warren RF, Maynard MJ (1995) The role of the cruciate and posterolateral ligaments in stability of the knee. A biomechanical study. Am J Sports Med 23(4):436–443
Wada M, Imura S, Baba H, Shimada S (1996) Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 35(6):560–563
Wang CJ, Walker PS (1974) Rotatory laxity of the human knee joint. J Bone Joint Surg Am 56(1):161–170
Weir JP (2005) Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 19(1):231–240
Wolf JM, Cameron KL, Owens BD (2011) Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg 19(8):463–471
Woodford-Rogers B, Cyphert L, Denegar CR (1994) Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train 29(4):343–346
Zarins B, Rowe CR, Harris BA, Watkins MP (1983) Rotational motion of the knee. Am J Sports Med 11(3):152–156
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mouton, C., Theisen, D., Seil, R. (2017). Static Rotational Knee Laxity Measurements. In: Musahl, V., Karlsson, J., Kuroda, R., Zaffagnini, S. (eds) Rotatory Knee Instability. Springer, Cham. https://doi.org/10.1007/978-3-319-32070-0_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-32070-0_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-32069-4
Online ISBN: 978-3-319-32070-0
eBook Packages: MedicineMedicine (R0)