Abstract
Introduction
This is a state-of-the-art article of the diagnostic process, etiologies and management of acute right ventricular (RV) failure in critically ill patients. It is based on a large review of previously published articles in the field, as well as the expertise of the authors.
Results
The authors propose the ten key points and directions for future research in the field. RV failure (RVF) is frequent in the ICU, magnified by the frequent need for positive pressure ventilation. While no universal definition of RVF is accepted, we propose that RVF may be defined as a state in which the right ventricle is unable to meet the demands for blood flow without excessive use of the Frank–Starling mechanism (i.e. increase in stroke volume associated with increased preload). Both echocardiography and hemodynamic monitoring play a central role in the evaluation of RVF in the ICU. Management of RVF includes treatment of the causes, respiratory optimization and hemodynamic support. The administration of fluids is potentially deleterious and unlikely to lead to improvement in cardiac output in the majority of cases. Vasopressors are needed in the setting of shock to restore the systemic pressure and avoid RV ischemia; inotropic drug or inodilator therapies may also be needed. In the most severe cases, recent mechanical circulatory support devices are proposed to unload the RV and improve organ perfusion
Conclusion
RV function evaluation is key in the critically-ill patients for hemodynamic management, as fluid optimization, vasopressor strategy and respiratory support. RV failure may be diagnosed by the association of different devices and parameters, while echocardiography is crucial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For years, the left ventricle (LV) has been considered by cardiologists and intensivists as the essential ventricle for maintenance of effective circulation. The LV, after all, holds the central role in defining arterial pressure, one of the main determinants of organ perfusion with blood flow. However, as better bedside hemodynamic monitoring and advanced imaging techniques have evolved, the linkage between Guytonian physiology and cardiovascular assessment demonstrated the essential role of right ventricular (RV) function in cardiovascular homeostasis. This realization is supported by several parallel lines of evidence. First, many critical care patients receive positive-pressure ventilation. The increasing airway pressure artificially increases right atrial pressure (RAP), the back pressure to venous return [1], limiting cardiac output, while simultaneously increasing RV afterload [2]. The phasic changes in RV output due to positive-pressure breathing define most of the dynamic changes in LV output, quantified as either arterial pulse pressure or LV stroke volume variations [3]. Second, the RV is the main limiting factor of fluid-responsiveness, as shown in pulmonary embolism (PE) [4] and in septic shock [5]. Indeed, its primary function is to optimize systemic venous return by decreasing or keeping RAP as low as possible while simultaneously ejecting its highly varying end-diastolic volume into a highly compliant and low resistance pulmonary circulation. When the RV fails, it cannot achieve these goals and the patient becomes fluid-unresponsive. Third, many situations in the critical care setting may promote RV failure (RVF) by causing increases in pulmonary vascular resistance, as described below.
Thus, it is not surprising that the occurrence of RVF reflects loss of cardiovascular reserve and is strongly associated with a poor prognosis. Worsening RV function is both a marker of adverse outcome and a direct contributor to mortality in a variety of disease states experienced in the critical care settings, as discussed later in acute respiratory distress syndrome (ARDS), RV myocardial infarction (MI) or decompensated pulmonary artery hypertension (PAH). The interplay between the RV and the pulmonary vasculature is a critical component of cardiac performance and patient outcomes while a number of diseases can directly or indirectly alter this interaction.
This state-of-the-art paper is an invited paper for the cardiovascular issue of Intensive Care Medicine. It reports the current definition, epidemiology and etiologies of RVF in the critical care setting, as well as the current recommendations for diagnostic workup and management. This paper is written by recognized experts in the field who also propose 10 key points regarding RVF based on the current knowledge, as well as main uncertainties/controversies in the field (Table 1
Pathophysiology and definition of acute RV failure
Acute RVF in critically ill patients is sometimes called the “acute right heart syndrome” (ARHS). A commonly used definition for RVF does not exist, while a recent statement defined ARHS as a rapidly progressive syndrome with systemic congestion resulting from impaired RV filling and/or reduced RV flow output [6]. We propose here a universal definition of RVF based on pathophysiology. In critically ill patients, ARHS is usually clinically diagnosed by a combination of systemic hypoperfusion (cool extremities, confusion, chest pain, arrhythmia, ileus, oliguria, lactic acidosis) and systemic congestion (turgescent jugular veins, hepatomegaly, oedema, ascites). Oedema and ascites are only present in patients with pre-existing chronic RVF or dysfunction. If a pulmonary artery catheter (PAC) is present in patients with predominant RVF, it displays a RAP higher than the pulmonary artery occlusion pressure, at which point the patient is usually hemodynamically unstable. In patients with severe biventricular failure, RAP may be elevated without an elevated ratio. Bedside echocardiography shows dilated or remodelled right heart chambers and depressed indices of systolic function most often in the presence of increased pulmonary artery pressures (PAP), as measured directly by the PAC or estimated by echo on the basis of increased velocity of tricuspid regurgitation and shortened acceleration time of RV ejection flow-velocity. A notch on the pulmonary flow signal is often indicative of pulmonary vascular obstruction (proximal or more distal). When a paradoxical intraventricular septal motion is also observed, some authors have also named this pattern cor pulmonale [7].
In situations where pulmonary hypertension (PH) is prominent, the ARHS is basically caused by a failure of RV systolic function adaptation to increased loading conditions (homeometric adaptation, or Anrep mechanism). According to the Anrep mechanism, rapid increase in PAP (within minutes) augments RV contractility (measured by end-systolic elastance, Ees) in order to match the afterload (measured by pulmonary arterial elastance, Ea). However, homeometric adaptation is often limited in critically-ill patients where pulmonary hypertension is associated with systemic hypotension and systemic inflammation, two factors contributing to RV injury. Optimal RV-arterial coupling relies on an Ees/Ea ratio of 1.5–2 to ensure flow output at minimal energy expenditure. When the Ees/Ea decreases to 1 and below, the RV enlarges to preserve flow output (heterometric adaptation, or Starling mechanism), at the price of increased filling pressures and systemic congestion [8]. The tricuspid valve is an essential part of RV structure and function. Unlike the mitral valve, the tricuspid value can dilate in its lateral dimension over a short time period resulting in acute regurgitation. This is a useful short-term adaptation, as it serves to decompress the acutely overloaded RV chamber preventing further dilatation. This adaptive regurgitation however results in increased venous and hepatic congestion and reduced forward flow.
Accordingly, RVF is defined by a state in which the RV is unable to meet the demands for blood flow without excessive use of the Frank–Starling mechanism (i.e. increase in stroke volume associated with increased preload). This definition was initially proposed by Sagawa and colleagues after having shown that the “laws of the heart” (i.e. Anrep and Starling mechanisms) equally apply to both the RV and the LV [9] in spite of their obvious embryological and structural differences [10]. The evolution of RV functional adaptation to increased loading conditions is non-linear. RV dimensions may markedly increase with moderate increases in preload or afterload even though homeometric adaptation remains [8]. Thus, RV dimensions can be increased above normal limits (defined on healthy control populations), yet flow output remains sufficient without onset of systemic congestion. This intermediate zone may be called RV maladaptation or RV dysfunction, as it may be associated with eventual biological alterations and “pending” RVF.
Once RV systolic function becomes uncoupled from the pulmonary circulation and the RV dilates, there is a negative diastolic interaction due to ventricular competition for space within indistensible pericardium. Associated with RV dilation both LV filling and cardiac output decrease [11]. This decreasing cardiac output eventually manifests as a decreased systemic arterial pressure, decreasing coronary blood flow and its associated negative systolic interaction. The vicious circle is further aggravated by RV ischemia due to decreased coronary perfusion pressure (gradient between diastolic blood pressure and right atrial pressure) [12] and contraction asynchrony [10, 13]. Right heart distension reflexly activates the sympathetic nervous system and the renin–angiotensin–aldosterone sequence which both result in renal salt and water retention aggravating systemic congestion and worsening ventricular interactions by further dilatation of the RV [14, 15].
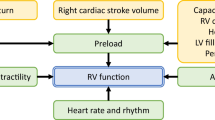
Understanding these mechanisms, summarized in Fig. 1, helps to identify targets of therapeutic interventions.
Pathophysiology of RV failure process (bold arrows) with the main target for therapeutic interventions (striped arrows). EDV end-diastolic volume, RHC right heart catheterization, PEA pulmonary endarterectomy, iNO inhaled nitric oxide, PGI 2 prostaglandin I2, PDE5i phosphodiesterase type 5 inhibitor, ERA endothelin receptor antagonists, BPA balloon pulmonary angioplasty, ABG arterial blood gases
Etiologies and epidemiology of RVF in the critical care settings
RVF in medical situations
RVF is a heterogeneous syndrome rather than a single disease. Treatment approaches, therefore, must be individualized based on the underlying etiology and mechanism of dysfunction. Because of differences in methodology and definition of RVF, as well as a paucity of prospective studies, the prevalence of acute RVF in the critical care setting has not been defined precisely. Moreover, the prevalence or incidence of RVF may vary depending on the criteria used.
Acute RVF occurs in many different situations (Fig. 2), which induce the described RV-arterial uncoupling. The most common cause of RVF is PH. Uncoupling of RV systolic function is generally observed with rapid increase of PAP or end-stage PAH, but also occurs with only mild PH in patients with lung inflammatory states (e.g. ARDS), sepsis and LV failure, all conditions also associated with negative inotropic effects. RVF may also develop in patients with PAH, because chronic RV remodelling has already occurred and the clinical presentation and treatments can be different from acute PH, for example, PAH with connective tissue diseases causing marked RV hypertrophy. In many of these acute and chronic situations, high airway pressure and high tidal volume mechanical ventilation intensify or even may cause acute RVF by increasing pulmonary vascular resistance [16]. In ARDS, one of the most common causes of acute RVF in the critical care setting, pulmonary vascular dysfunction is common [17]. Acute cor pulmonale (ACP) occurs in 14–50% of ventilated ARDS, with most studies reporting a prevalence of around 25% [18]. Causes are multiple and usually combined lung inflammation, pulmonary artery injury and the effects of positive pressure ventilation [19]. In a large cohort of more than 700 patients with moderate to severe ARDS and ventilated in a “protective” manner (e.g. with a tidal volume around 6 mL/kg and a strict limitation of plateau pressure below 30 cmH2O), ACP was found in 22% of cases. Four risk factors were identified, i.e. pneumonia, PaO2/FiO2 < 150 mmHg, PaCO2 ≥ 48 mmHg and driving pressure ≥ 18 mmHg [20]. Those patients with ACP are usually more tachycardic, have a lower systolic and mean arterial pressure and are more frequently in shock (86 versus 67%) [21]. In acute PE, cardiogenic shock occurs in ~ 4.5% of patients [22], and some evidence of RV strain occurs in about one-third of acute PE patients [23]. Pulmonary artery thrombosis has also been reported in sickle cell disease during acute chest syndrome in 17% of cases [24]. This is associated with an overall 24% incidence of RVF, especially when ARDS is also present [25]. RV MI is seen in about one third of cases of inferior wall acute MI [26]. Like other causes of acute RVF, RV MI causes uncoupling of RV systolic function and the pulmonary circulation, producing systemic congestion and reduced flow [6]. However, unlike most conditions associated with critical illness, in RV MI the lesion resides within the right ventricle, rather than in the pulmonary circulation.
Classification and stages of acute right ventricular failure (RVF). a RVF may affect a sub-pulmonic (by far the most common) or the systemic ventricle in transposition of the great arteries. Failed Fontan circulation is rare, but observed more frequently in referral centres. Although ventricular failure often affects both ventricles because of ventricular interactions, for clinical purposes it is useful to classify RVF as predominantly affecting the right ventricular or part of a biventricular failure profile. Pulmonary hypertension is the most common cause of RVF in the ICU. In many cases in the ICU, pressure overload, volume overload and decreased contractility often coincide. b Stage of acute RVF. Patients with acute RVF may present as there first presentation or as an acute on chronic RVF. In acute RVF the vicious cycle of hypotension, ischemia and arrhythmia has to be avoided as it leads to clinical deterioration. Recovery of acute RVF may be variable and the early recovery-post-discharge phase is known to be also vulnerable. RV right ventricle, HFREF heart failure with reduced ejection fraction, HFPEF heart failure with preserved ejection fraction, ARVC arrhythmogenic RV cardiomyopathy
The prevalence of acute RVF in other conditions (e.g. COPD exacerbations, left heart failure, sleep-disordered breathing) is not exactly known. However, many of these conditions are common, and some form of RV dysfunction (acute or chronic) may occur in as many as 80% of these patients [27, 28]. RVF is also common in various forms of PAH and may occur as acute-on-chronic RVF or as new-onset RVF. Precipitating factors include infection, volume overload, myocardial ischemia, PE, anaemia, trauma, surgery, arrhythmias, medical non-adherence, and progression of previously undiagnosed PAH [29, 30].
A common theme in all these conditions is that the occurrence of RVF is associated with a significantly worse survival. For example, the 90-day mortality rate for patients with massive PE is 52% [22]; RV MI raises the risk of death more than twofold [31]; severe ACP is associated with increased mortality in ARDS [20]; and ICU mortality for patients admitted with decompensated PAH and RVF is 41% [30].
Lastly, there has been a recent focus on the management of patients who are resuscitated from cardiopulmonary arrest and transferred to a critical care unit. Up to 50% of these patients will need vasopressor support for hemodynamic instability [32]. A study investigating RV function in the first few hours after cardiac arrest showed that around 90% of this group of patients demonstrated both RV structural and functional abnormalities and that increase in the chamber dimensions was associated with increased mortality [33].
Perioperative RVF
RVF is much more likely to complicate cardiac surgery with numerous causes [34], while patients with existing severe PH and undergoing non-cardiac surgery may also have perioperative RVF. Patients with pre-existing PH, impaired RV function and tricuspid valve insufficiency are at increased risk of acute decompensation [35, 36]. RVF may occur following cardiac surgery secondary to acute left sided pathology, including LV failure, ventricular septal defects following MI and acute severe mitral valve regurgitation. Isolated acute right-sided failure may occur because of inadequate intraoperative right-sided cardioplegia administration or complications related to coronary artery graft flow or tricuspid valvuloplasty surgery. Intracoronary air and long cardiopulmonary bypass times may be contributory factors. Surgery involving the pulmonary arteries such as lung transplant and pulmonary endarterectomy can precipitate RVF [37]. An identifiable group of patients at higher risk of acute RVF are those undergoing cardiac transplantation, where RVF has been identified as an important cause of early deaths, and those receiving a LV assist device (LVAD) [38]. Transplant patients can develop acute RV pressure overload as a consequence of myocardial ischemia–reperfusion injury associated with organ preservation combined with either acute or chronically raised pulmonary vascular resistance. In a recent large study of 2988 patients from the European Registry of patients with Mechanical Circulatory Support (EUROMACS), RVF following LVAD implantation occurred in 22% of patients within 30 days of surgery with 7% requiring Mechanical Circulatory Support (MCS). Consistent with other risk stratification models, patients with evidence of RV function impairment were at higher risk [39]. Congenital heart disease and corrective surgeries such as those for Tetralogy of Fallot may result in RVF for a number of reasons and may limit the feasibility of the procedure. Acute cardiogenic shock mimicking RVF may also occur in the presence of pericardial thrombus causing a localized compression and obstruction to RV filling with significantly raised central venous pressure.
Diagnostic workup
Clinical presentation, examination, ECG, biochemical assessment and imaging are involved in the diagnosis of acute RVF and monitoring response to treatment. Signs, symptoms and laboratory tests can elucidate acute RVF etiologies. However, these findings lack sensitivity and specificity [40] and abnormal signs, symptoms and lab results can be from a variety of other pathology causing organ hypoperfusion (Table 2). There is no specific biochemical marker that identifies acute RVF [6, 41]. Diagnostic workup is, therefore, highly dependent on the clinical diagnosis aided by imaging. In particular, echocardiography plays a major diagnostic role [42]. We suggest a possible diagnostic pathway in the Fig. 3.
Best standard of care (for diagnosis and investigation)
A high level of suspicion ensures timely identification of acute RVF, which is essential for appropriate management. Delayed diagnosis and treatment of the underlying cause, as well as failure to prevent further injury to the RV (e.g. through fluid overload or worsening RV afterload) are all associated with worse outcomes. Early signs which should raise concern include hypoxemia, acidosis, hyperlactatemia, troponin rise, minor coagulopathy, and acute renal and liver dysfunction due to increased venous pressure. These are all non-specific findings and should prompt further investigation, particularly a thorough echocardiographic examination.
Initial assessment
Clinical presentation and examination vary with etiology and presence of co-morbidities, especially chronic RV changes. Recognition of pre-existing PAH (e.g. from parenchymal lung disease) is important as it dramatically impacts the patient’s ability to cope with increases in PAP [43] and predisposes to death from acute on chronic RVF [44]. ECG and CXR findings may be normal, however, ECG may identify arrhythmias or RV strain pattern and CXR examination may suggest new parenchymal lung disease or volume overload potentially caused by left-sided heart disease [45].
Echocardiography (Fig. 4, Table 3)
Echocardiography plays an important role in the diagnosis of acute RVF in the ICU, initially by identifying presence of left-sided heart disease. In addition, echocardiography can non-invasively assess RV preload, contractility and afterload. Focused cardiac studies provide a method to identify RV dysfunction and dilation and its use has been suggested to decrease mortality in the ICU setting [46]. Comprehensive studies using Doppler enable hemodynamic and valvular assessment. The ability to rapidly assess response to treatment in terms of cardiac output, filling pressures, RV size and function and PAP makes echocardiography highly versatile. The complex RV geometry and position can make accurate analysis challenging. All views should be used to assess RV size and function, particularly the apical four-chamber view (the RV is normally less than 60% the size of the LV) where there is reduced inter-observer variability [45]. Care should be taken if there is LV enlargement as RV size may be underestimated (dimensions and area should be measured). Moreover, the concept that RV dilation must be present to diagnose RVF is contentious and it would be more accurate to describe a dynamic situation of increasing RV volumes by fluid expansion without changes in cardiac output as a signature of acute RVF. LV and left atrial enlargement point towards postcapillary PH involvement (although other etiologies need to be considered), whereas RVF associated with precapillary PH can be associated with a shift of the interventricular septum towards the left and a relatively under-filled LV. RV function can be assessed with multiple parameters and qualitative, as well as quantitative parameters are important [47]. The majority of echocardiography parameters for assessment of pulmonary hemodynamics in the critically ill have been shown to be accurate. Particular care should be taken with integration of findings into the clinical presentation. Importantly, dynamic measures of RV systolic function, such as speckle tracking, have proven highly sensitive in defining both early RV strain prior to overt RVF and improvements in RV function in response to specific therapies, such as pulmonary vasodilator therapy [48, 49].
Current imaging techniques in acute right ventricle (RV) failure diagnosis and recent advances. Echocardiography: panels a–n. All view needs to be used to assess RV size and RV function, a parasternal long axis view, b parasternal short axis view (including eccentricity index in assessment of ventricular interdependence), c apical four chamber view (dimensions and area may be useful particularly if the LV is dilated), d subcostal view. Preload analysis: e assessment for fluid responsiveness by stroke volume variation with respiration ± passive leg raise, f IVC size variation with respiration (less accurate in presence of RVF and significant tricuspid regurgitation), g presence of pericardial effusion. Contractility assessment: h fractional area change, j subjective analysis, k TAPSE (tricuspid annular plane systolic excursion). Afterload assessment: l tricuspid regurgitation jet used for estimation of peak systolic pulmonary artery pressures (4[TRVmax]2 + right atrial pressure), where TRVmax is the maximal velocity of the tricuspid regurgitation, m RV outflow tract flow analysis (e.g.: “flying W sign” in raised pulmonary vascular resistance), n pulmonary regurgitation flow for estimation of diastolic pulmonary artery pressures (4[PRVend-diastolic]2 + RAP), where PRV is the velocity of the pulmonary regurgitation. Computed tomography (CT): panels o–q. o LV/RV diameter ratio, p pulmonary artery size and presence of thrombus, q IVC contrast regurgitation in acute RV failure. Recent advances: panels r–t. r Speckle tracking echocardiography, s 3D echo volumetric analysis, t apical dyskinesia by magnetic resonance imaging (MRI) due to pulmonary embolism
In RV MI, a key distinguishing characteristic is that RV systolic pressure, along with related echocardiographic indices such as the tricuspid regurgitation jet velocity, is not significantly elevated. Thus echocardiographic assessment is essential for distinguishing RV MI from other causes of acute RVF. However, some of these patients may also require positive pressure ventilation in case of associated cardiogenic pulmonary edema due to large inferior MI or mitral regurgitation, and the pattern of RVF is closer to that is usually observed in situations with injury of the pulmonary circulation.
Transoesophageal echocardiography (TOE) is the essential diagnostic tool for all RVF following cardiac surgery, transthoracic windows are generally poor in patients following sternotomy. A more recently developed disposable TOE probe has been described that can be used for up to 72 h, and can track RV functional recovery and inform changes in hemodynamic therapy [50, 51].
Computed tomography (CT) (Fig. 4)
CT pulmonary angiography is the imaging method of choice in acute PE and echocardiography should not be used to exclude venous thromboembolism [52]. RV size is assessed, with or without ECG-gating [53], by analysing RV/LV diameter ratio (greater than 1 predicts risk for adverse outcomes in PE); however, there are reports of significant inter-observer variability and volumetric analysis may be better [54]. Increased RV/LV ratio can also point towards PH that is not related to acute PE, in particular when it is accompanied by pulmonary artery diameters exceeding that of the aorta [55]. RV function can be further assessed by the determination of ejection fraction (assessment requires ECG gating) and the presence of interventricular septal bowing and inferior vena cava contrast reflux [56]. Additionally, CT angiographic determination of the left to right atrial ratio can help to distinguish between pre- and post-capillary forms of PH [57].
Invasive monitoring
Pulmonary artery catheter (PAC) use provides continuous monitoring of PAP and may identify those patients with acute RV dysfunction with poor compliance through monitoring of RV pressures (using proximal port in RV) vs PAP (steeper RV diastolic pressure slope) [58]. Since PAC use is still common in cardiac surgical critical care [59] clinicians need to be cognizant of these hemodynamic signatures when following these patients post bypass. Although less used nowadays due to the risks of placement, use of the PAC may help in those at risk of acute RVF (e.g. history of significant PAH) or those not responding to conventional treatment. Still, when available, the estimate of pulmonary vascular compliance (pulmonary arterial pulse pressure to stroke volume ratio) offers more insight into defining RV performance in ARDS patients than doing measures of pulmonary vascular resistance [60, 61]. Combining echocardiography with invasive PAC monitoring seems the ideal method for monitoring this challenging group of patients. Temporal trends in PAP and RAP likely hold more benefit than static measures (e.g. increasing PAP and decreasing RAP may indicate improved RV output into a pulmonary system with high resistance). Thermodilution-based cardiac output estimations should be used with caution in acute RVF as significant acute tricuspid regurgitation may lead to underestimation [62], especially when the severity of the regurgitation is not fixed for beat to beat, as it may occur in mechanically ventilated patients. However, when used very rigorously, it has been suggested to have a good accuracy in a small population of spontaneous ventilated patients with PAH [63]. Transpulmonary thermodilution (PICCO® device), another popular invasive monitoring device, has been reported not to be appropriate in detecting isolated RVF [64].
Recent advances
Several novel PH biomarkers are described that relate to heart failure, inflammation, cardiovascular remodelling and endothelial cell-smooth muscle cell interaction [65]. They have predominantly been studied in animals or in small patient numbers, in single centres for risk stratification of PE and chronic PAH cohorts, and never in acutely ill patients [66,67,68]. Many studies also suffer from publication bias, multiple testing and retrospective analysis which limits their validity [65].
Speckle tracking echocardiography appears to be a promising monitoring approach. Recently developed software can track the movement of the grey-scale pixels relative to each other providing a quantitative measure of deformation (known as “strain”), a negative dimensionless value, which describes a relative change in distance between pixels. Strain is used as a surrogate for systolic performance but not contractility; the greater the negative value, the greater the degree of deformation. RV function is classically assessed by tracking the movement of the RV free wall only. Known as RV free wall strain (normal values are more negative than − 20 to − 25%), it has been shown to describe cardiac dysfunction not elucidated by conventional echocardiographic techniques [69] and is highly prognostic in PAH cohorts [70], as well as in septic patients [71]. Speckle tracking echocardiography requires a reasonably high level of experience and training to perform as erroneous results are easy to acquire if the tracking is inappropriately performed. Measuring RV free wall longitudinal strain using manual tracing of RV end-diastolic and end-systolic length may be more simple and has been shown to be prognostic in patients with PAH [72]. As RVF induces congestion, the role of portal vein flow and renal flow monitoring by simple Doppler method should also be investigated to evaluate RV function.
Three-dimensional echocardiography is emerging with the potential to overcome the limitations of single-plane imaging seen in conventional echocardiography. For the RV this has particularly interest due to the abnormal concentric shape. Widespread use has been limited by imaging difficulties and availability, however its accuracy has been validated against cardiac magnetic resonance imaging (CMR) [73]. Further advances include the development of 3D speckle tracking of the RV in PAH [74]. To date, the use of 3D imaging of the RV has not been well investigated in the critically ill.
CMR is often used as the reference standard in studies investigating accuracy of RV imaging [75, 76]. CMR allows comprehensive evaluation of RV anatomy, volume, function and tissue characterization, with features such as RV dilation, abnormal septal and free wall motion, and tricuspid regurgitation easily recognized [77]. RV functional changes over time are much more accurately assessed by CMR than by echocardiography [78]. Native T1 mapping [79], T2-weighted and late gadolinium enhancement [80] potentially enable characterization of oedema, infarction or inflammation, although the RV free wall is not always easily detected and RV analysis is not well-validated or imprecise. However, CMR studies in the critically ill are currently lacking due to the restricted access, limitations of compatible equipment, patient and staff safety and time needed for imaging. Newer methods, as open-MRI with limited magnetic field [81], or methods aimed to reduce speed of MRI from 45–60 min to potentially 15 min [82] should make CMR increasingly available for critically ill patients.
Management
Treatment of the cause
It is obvious that, when reversible, the priority must be to specifically treat the cause of RVF. For instance, fibrinolysis or even surgical embolectomy may be considered in RVF-related PE [52]. RV MI also presents some unique options for treatment, including percutaneous coronary intervention. Precipitating factors of decompensated chronic RVF have to be controlled (see previous sections for the precipitating factors).
Hemodynamic support (Fig. 5)
The management of acute RVF focuses on stabilizing hemodynamics, optimizing loading conditions and treating potential reversible cause. Prompt treatment of arrhythmias (tachy or brady) is also essential to avoid the vicious circle of hypotension, ischemia and further arrhythmias.
Physiological consideration during the management of acute RVF. The cardiopulmonary unit is central in tailoring management of RVF. Pulmonary vascular resistance or impedance is influences by hypoxemia, hypercapnia and acidosis, lung volumes and positive pressure ventilation. Maintenance of blood pressure and coronary pressure is essential in managing RVF. In addition, management of RVF including fluid management has to take into account zone ventricular interactions, pericardial constraint, fluid responsiveness (zone of the Starling curve). Abdomino-thoracic and cardio-thoracic are essential to consider in acute RVF in the ICU setting as these can be overlooked caused of hemodynamic instability
One of the most important misconceptions in managing RVF is assuming that the majority of patients are on the preload dependent zone of the Frank–Starling relationship and would, therefore, benefit from volume loading. However, acute RVF leads to diastolic LV failure [83, 84], wherein both hypovolemia and hypervolemia are poorly tolerated and the optimal RV filling volume is often difficult to define. Even small fluid boluses can be poorly tolerated in acute RVF and ACP. In 13 patients with hemodynamic and radionuclide ventriculographic evidence of RV MI, progressive volume loading has been demonstrated to significantly increase RAP and PAOP but without significant change in cardiac index [85]. In canine model of PE or in the positive pressure ventilated setting, the lack of hemodynamic improvement following fluid challenge has been reported [86, 87]. In a landmark study in the setting of experimental RV MI (pig model), the importance of pericardial constraint was demonstrated, highlighting the importance of ventricular interactions [11]. Experimental studies in RV MI, PE and PAH have all shown that volume loading can increase right cavity size, increase pericardial constraint and further limit LV filling through the mechanisms of ventricular interdependence [88,89,90]. In a model of acute-on-chronic pulmonary thromboembolic disease, Boulate et al. also recently demonstrated that fluid challenge is not associated with an increase in stroke volume or cardiac output [91]. Taken together, these experimental and clinical studies would argue against routine volume loading in acute RVF unless clear evidence of hypovolemia or stroke volume responsiveness to physiological variation is noted. Patients with RV MI could benefit from volume repletion in the presence of clear evidence of hypovolemia; the usually lower afterload and lower ventricular wall stress compared to patients with chronic pressure overload can placed them at a more favourable portion of the Frank–Starling relationship. If fluid is given, starting with low volume repletion of 100–250 mL is often preferred while monitoring stroke volume or blood pressure response (unless active source of rapid volume loss is known to co-exist). Several studies including an excellent comprehensive review by Marik et al. have shown than RAP alone should not be considered a reliable marker of volume status or volume responsiveness [92], while other parameters for fluid responsiveness have been proposed [93], some of them unfortunately limited in RVF. Briefly, echocardiography is key in optimizing fluid loading, while IVC diameter has been recently reported to poorly predict the response to fluids in mechanically ventilated patients [94] and in fact there is no magic parameter to guide the need for fluids [95]. Measuring changes in cardiac output in response to a passive leg raise manoeuvre define volume responsiveness and can be used to attempt judicious fluid loading (with assessment of response to the intervention) [96]. In fact, the majority of patients with acute RVF associated with chronic PAH, congenital heart disease or biventricular failure would respond more to volume removal than infusion.
Since most RV coronary flow occurs in systole, if PAP increases above systemic arterial pressure, RV ischemia can develop. The primary salvage treatment to sustain cardiovascular function is the infusion of vasopressors (e.g. norepinephrine, vasopressin or terlipressin) to keep systemic arterial pressure greater than pulmonary arterial pressure. In a canine model of acute obstruction of the pulmonary circulation, fluid loading worsened RVF, while in contrast norepinephrine infusion restored mean arterial pressure to baseline, decreased biventricular filling pressure and increased cardiac index [97]. Inotropic drugs have also been proposed, while no reasonable study may clearly recommend their use in acute RVF-related PH. There is probably no place for isoproterenol in the management of ARF, as in a model of experimental PE, all dogs randomized to receive isoproterenol died [98]. In PE, dobutamine has been reported to improve hemodynamics and reduced pulmonary vascular resistance [99]. In RVF related to ARDS, it makes sense to use inodilator to improve RV-pulmonary circulation coupling, as reported in a pilot study in which levosimendan was infused in 35 patients [100]. In 25 patients with cardiogenic shock related to myocardial infarction not sufficiently improved after percutaneous revascularization and infusion of dobutamine or norepinephrine, RV performance, as well as hemodynamics, was improved by levosimendan infusion [101]. However, at this time, no clear recommendation can be made due to the absence of sufficient data.
An exciting novel direction in the management of RVF is the use of MCS devices. In situations where medical therapy is inadequate, the employment of MCS devices to augment cardiac output, decrease RA and RV preload and improve oxygenation and acidosis can provide a lifesaving bridge to either recovery or transplant. Surgically implanted RV assist devices (RVADs) have been used for more than two decades for this purpose. However, their placement via sternotomy or thoracotomy is often not feasible in critically ill patients. More recently, interest has turned to percutaneously placed support devices, which have the potential to revolutionize our approach to this patient population, providing the advantage of rapid deployment without the surgical risk. The Impella RP (Abiomed Inc) can be placed via one venous access site (usually the femoral vein) with delivery of blood from the RA to PA via a 22F impeller mounted on an 11F catheter. In a prospective cohort study including 30 patients with refractory RVF, 18 post LVAD and 12 following cardiotomy or RV infarct, hemodynamics improved in all patients immediately following device placement [102]. The overall mortality at 30 days was 73.3%, which compares favourably to previous case series of surgically placed RVADs. Two other percutaneously placed MCS devices also exist, one requiring two venous catheters and the other a dual-lumen cannula for RA inflow and PA outflow [103,104,105]. Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) can offer both right and left sided circulatory support and is currently the most widely utilized percutaneously deployed MCS for acute or acute on chronic RVF. The creation of mobile “ECMO teams” allows the utilization of this treatment modality throughout the hospital in a rapid response manner, including code situations. The successful use of “awake” ECMO, with placement of the venous and arterial catheters using only conscious sedation, avoiding mechanical ventilation, has garnered recent attention in the management of PH as a bridge to transplant.
Respiratory strategy
RVF in the ICU is clearly promoted and worsened by positive-pressure ventilation, either related to respiratory settings or to their consequences, which are blood gasses (PaO2, PaCO2). Though especially true in ARDS, it can potentially be seen in any mechanically ventilated patient. In general, plateau pressure and driving pressure have to be limited [20, 106]. As hypercapnia by increasing the hypoxic pulmonary vasoconstriction is deleterious for the right ventricle, especially when inducing acidosis [107], PaCO2 has to be controlled. This may be achieved by different ways: limiting intrinsic PEEP (PEEP i ) by decreasing respiratory rate (RR) in acute exacerbation of COPD or acute asthma, increasing RR without inducing PEEPi in ARDS, and removing CO2 by extracorporeal circulation [108]. Hypoxia also contributes slightly to PH [109], thus oxygenation has to be optimized. However, recruitment manoeuvres followed by application of a high PEEP, to “optimize lung aeration and oxygenation”, increase mortality and hemodynamic compromise in ARDS patients [110]. At the opposite, ventilation in prone position has been reported to increase oxygenation, decrease PaCO2, plateau pressure and driving pressure in ARDS, and finally to correct RVF [111]. Nitric oxide inhalation (iNO) could also be tried in refractory PH with acute RVF, not to improve oxygenation, as it failed to improve prognosis in ARDS [112], but with a goal to decrease PAP and RV afterload and then to improve hemodynamic status. iNO has been suggested to be associated with a lower mortality in patients with PAH at risk of RVF after orthotopic heart or lung transplantation which is not the case after cardiac surgery or in medical patients with hypoxemia [113].
Conclusion
We propose in this manuscript a universal definition of RVF, which is defined by a state in which the RV is unable to meet the demands for blood flow without excessive use of the Frank–Starling mechanism. RVF is frequent in the critically ill ICU patient, while studies are lacking to precisely know its incidence in unselected population. It may occur de novo (“acute”) or by decompensation of a pre-existing condition (“acute-on-chronic”). It is associated with worse prognosis. Hemodynamic and respiratory management is mainly based on pathophysiological rationale, as the absence of sufficient clinical studies to compare one direction or the other does not allow doing any formal recommendation. Future research should be based on large database study of admitted unselected patients to evaluate incidence, impact and management.
References
Guyton AC (1955) Determination of cardiac output by equating venous return curves with cardiac response curves. Physiol Rev 35:123–129
Scharf S, Brown R, Saunders N, Green L (1980) Hemodynamic effects of positive pressure inflation. J Appl Physiol 49:124–131
Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2003) Cyclic changes in arterial pulse during respiratory support revisited by Doppler echocardiography. Am J Respir Crit Care Med 168:671–676
Mercat A, Diehl JL, Meyer G, Teboul JL, Sors H (1999) Hemodynamic effects of fluid loading in acute massive pulmonary embolism. Crit Care Med 27:540–544
Mahjoub Y, Pila C, Friggeri A, Zogheib E, Lobjoie E, Tinturier F, Galy C, Slama M, Dupont H (2009) Assessing fluid responsiveness in critically ill patients: false-positive pulse pressure variation is detected by Doppler echocardiographic evaluation of the right ventricle. Crit Care Med 37:2570–2575
Harjola VP, Mebazaa A, Celutkiene J, Bettex D, Bueno H, Chioncel O, Crespo-Leiro MG, Falk V, Filippatos G, Giggs S, Leite-Moreira A, Lassus J, Masip J, Mueller C, Mullens W, Naeije R, Nordegraaf AV, Parissos J, Riley JP, Ristic A, Rosano G, Rudiger A, Ruschitzka F, Seferovic P, SztrymfB Vieillard-Baron A, Yilmaz MB, Konstantinides S (2016) Contemporary management of acute right ventricular failure: a statement from the heart failure association and the working group on pulmonary circulation and right ventricular function of the European Society of Cardiology. Eur J Heart Fail 18:226–241
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111:209–217
Vonk Noordegraaf A, Westerhof BE, Westerhof N (2017) The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol 69:236–243
Sagawa Maughan, Suga Sunagawa, Sagawa K, Maughan L, Suga H, Sunagawa K (1988) Cardiac contraction and the pressure–volume relationship. Oxford University Press, New York
Friedberg MK, Redington AN (2014) Right versus left ventricular failure: differences, similarities and interactions. Circulation 29:1033–1044
Goldstein JA, Vlahakes GJ, Verrier ED, Schiller NB, Tyberg JV, Ports TA, Parmley WW, Chatterjee K (1982) The role of right ventricular systolic dysfunction and elevated intrapericardial pressure in the genesis of low output in experimental right ventricular infarction. Circulation 65:513–522
Cross CE (1962) Right ventricular pressure and coronary flow. Am J Physiol 202:12–16
Naeije R, Badagliacca R (2017) The overloaded right ventricle and ventricular interdependence. Cardiovasc Res 113:1474–1485
Naeije R, Manes A (2014) The right ventricle in pulmonary arterial hypertension. Eur Respir Rev 23:476–487
Ventetuolo CE, Klinger JR (2014) Management of right ventricular failure in the intensive care unit. Ann Thorac Surg 11:811–822
Katira BH, Giesinger RE, Engelberts D, Zabini D, Kornecki A, Otulakowski G, Yoshida T, Kuebler WM, McNamara PJ, Connelly KA, Kavanagh BP (2017) Adverse heart-lung interactions in ventilator-induced lung injury. Am J Respir Crit Care Med 196:1411–1421
Bull TM, Clark B, McFann K, Moss M, National Institutes of Health/National Heart, Lung, and Blood institute ARDS Network (2010) Pulmonary vascular dysfunction is associated with poor outcomes in patients with acute lung injury. Am J Respir Crit Care Med 182:1123–1128
Repessé X, Charron C, Vieillard-Baron A (2015) Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Chest 147:259–265
Price LC, McAuley DF, Marino PS, Finney SJ, Griffiths MS, Wort SJ (2012) Pathophysiology of pulmonary hypertension in acute lung injury. Am J Physiol Lung Cell Mol Physiol 302:L803–L815
Mekontso-Dessap A, Boissier F, Charron C, Bégot E, Repessé X, Legras A, Brun-Buisson C, Vignon P, Vieillard-Baron A (2016) Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med 42:862–870
Boissier F, Katsahian S, Razazi K, Thille AW, Roche-Campo F, Leon R, Vivier E, Brochard L, Vieillard-Baron A, Brun-Buisson C, Mekontso-Dessap A (2013) Prevalence and prognosis of cor pulmonale during protective ventilation for acute respiratory distress syndrome. Intensive Care Med 39:1725–1733
Kucher N, Rossi E, De Rosa M, Goldhaber SZ (2006) Massive pulmonary embolism. Circulation 113:577–582
Grifoni S, Olivotto I, Cecchini P, Pieralli F, Camaiti A, Santoro G, Conti A, Agnelli G, Berni G (2000) Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation 101:2817–2822
Mekontso-Dessap A, Deux JF, Abidi N, Lavenu-Bombled C, Melica G, Renaud B, Godeau B, Adnot S, Brochard L, Brun-Buisson C, Galacteros F, Rahmouni A, Habibi A, Maitre B (2011) Pulmonary artery thrombosis during acute chest syndrome in sickle cell disease. Am J Respir Crit Care Med 184:1022–1029
Cecchini J, Boissier F, Gibelin A, de Prost N, Razazi K, Carteau G, Galacteros F, Maitre B, Brun-Buisson C, Mekontiso Dessap A (2016) Pulmonary vascular dysfunction and cor pulmonale during acute respiratory distress syndrome in sicklers. Shock 46:358–364
Kinch JW, Ryan TJ (1994) Right ventricular infarction. N Engl J Med 330:1211–1217
Morrison DA, Adcock K, Collins CM, Goldman S, Caldwell JH, Schwarz MI (1987) Right ventricular dysfunction and the exercise limitation of chronic obstructive pulmonary disease. J Am Coll Cardiol 9:1219–1229
Mohammed SF, Hussain I, Abou Ezzedine OF, Takahama H, Kwon SH, Forfia P, Roger VL, Redfield MM (2014) Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation 130:2310–2320
Hoeper MM, Granton J (2011) Intensive Care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med 184:1114–1124
Sztrymf B, Souza R, Bertoletti L, Jaïs X, Sitbon O, Price LC, Simonneau G, Humbert M (2010) Prognostic factors of acute heart failure in patients with pulmonary arterial hypertension. Eur Respir J 35:1286–1293
Hamon M, Agostini D, Le Page O, Riddell JW, Hamon M (2008) Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta-analysis. Crit Care Med 36:2023–2033
Bougouin W, Aissaoui N, Combes A, Deye N, Lamhaut L, Jost D, Maupain C, Beganton F, Bougle A, Karam N, Dumas F, Marijon E, Jouven X, Cariou A (2017) Post-cardiac arrest shock treated with veno-arterial extracorporeal membrane oxygenation: an observational study and propensity-score analysis. Resuscitation 110:126–132
Wardi G, Blanchard D, Dittrich T, Kaushal K, Sell R (2016) Right ventricle dysfunction and echocardiographic parameters in the post-cardiac arrest patients: a retrospective cohort study. Resuscitation 103:71–74
Haddad F, Couture P, Tousignant C, Denault A (2009) The right ventricle in cardiac surgery, a perioperative perspective: II. Pathophysiology, clinical importance, and management. Anesth Analg 108:422–433
Dávila-Román VG, Waggoner AD, Hopkins WE, Barzilai B (1995) Right ventricular dysfunction in low output syndrome after cardiac operations: assessment by transesophageal echocardiography. Ann Thorac Surg 60:1081–1086
Kaul TK, Fields BL (2000) Postoperative acute refractory right ventricular failure—incidence, pathogenesis, management and prognosis. Cardiovasc Surg 8:1–9
Sullivan TP, Moore JE, Klein AA, Jenkins DP, Williams LK, Roscoe A, Tsang W (2017) Evaluation of the clinical utility of transesophageal echocardiography and invasive monitoring to assess right ventricular function during and after pulmonary endarterectomy. J Cardiothorac Vasc Anesth. https://doi.org/10.1053/j.jvca.2017.09.026
Grant AD, Smedira NG, Starling RC, Marwick TH (2012) Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol 60:521–528
The EUROMACS (European Registry for Patients with Mechanical Circulatory Support) right-sided heart failure risk score (2017) Derivation and validation of a novel right-sided heart failure model after implantation of continuous flow left ventricular assist devices. Circulation 136. https://doi.org/10.1161/circulationaha.117.030543
Grignola JC, Domingo E (2017) Acute right ventricular dysfunction in intensive care unit. Biomed Res Int 2017. https://doi.org/10.1155/2017/8217105
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200
Krishnan S, Schmidt GA (2015) Acute right ventricular dysfunction: real-time management with echocardiography. Chest 147:835–846
Hoeper MM, Galié N, Murali S, Olschewski H, Rubenfire M, Robbins IM, Farber HW, McLaughlin V, Shapiro S, Pepke-Zaba J, Winkler J, Ewert R, Opotz C, Westerkamp V, Vachiery JL, Torbicki A, Behr J, Barst RJ (2002) Outcome after cardiopulmonary resuscitation in patients with pulmonary arterial hypertension. Am J Respir Crit Care Med 165:341–344
Tsapenko MV, Tsapenko AV, Comfere TB, Mour GK, Mankad SV, Gajic O (2008) Arterial pulmonary hypertension in noncardiac intensive care unit. Vasc Health Risk Manag 4:1043–1060
Lang RM, Badano LP, Mor-Avi V, Afilo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzchel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1–39):e14
Levitov A, Frankel HL, Blaivas M, Kirkpatrick AW, Su E, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S, McLaughlin M, Marik P, Elbarbary M (2016) Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part II. 44:1206–1227. Crit Care Med 44:1206–1227
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Pinsky MR (2016) The right ventricle: interaction with the pulmonary circulation. Crit Care 20:1–9
Simon MA, Rajagopalan N, Mathier MA, Shroff SG, Pinsky MR, Lopez-Candales A (2009) Tissue Doppler imaging of right ventricular decompensation in pulmonary hypertension. Congest Heart Fail 15:271–276
Vieillard-Baron A, Slama M, Mayo P, Charron C, Amiel JB, Esterez C, Leleu F, Repessé X, Vignon P (2013) A pilot study on safety and clinical utility of a single-use 72-hour indwelling transesophageal echocardiography probe. Intensive Care Med 39:629–635
Fletcher N, Geisen M, Meeran H, Spray D, Cecconi M (2015) Initial clinical experience with a miniaturized transesophageal echocardiography probe in a cardiac intensive care unit. J Cardiothorac Vasc Anesth 29:582–587
Konstantinides SV, Torbicki A, Agnelli G et al (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35:3033–3069
Lu MT, Cai T, Ersoy H, Whitmore AG, Levit NA, Goldhaber SZ, Rybicki FJ (2009) Comparison of ECG-gated versus non-gated CT ventricular measurements in thirty patients with acute pulmonary embolism. Int J Cardiovasc Imaging 25:101–107
Kang DK, Thilo C, Schoepf UJ, Barraza M, Nance JW, Bastarrika G, Abro JA, Ravenel JG, Costello P, Goldhaber SZ (2011) CT signs of right ventricular dysfunction: prognostic role in acute pulmonary embolism. JACC Cardiovasc Imaging 4:841–849
Spruijt OA, Bogaard H-J, Heijmans MW, Lely RJ, van de Veerdonk MC, de Man FS, Westerhof N, Vonk-Noordegraaf A (2015) Predicting pulmonary hypertension with standard computed tomography pulmonary angiography. Int J Cardiovasc Imaging 31:871–879
Dogan H, de Roos A, Geleijins J, Huisman MV, Kroft LJ (2015) The role of computed tomography in the diagnosis of acute and chronic pulmonary embolism. Diagn Interv Radiol 21:307–316
Huis In’t Veld AE, Van Vliet AG, Spruijt OA, Handoko ML, Marcus JT, Vonk Noordegraaf A, Bogaard HJ (2016) CTA-derived left to right atrial size ratio distinguishes between pulmonary hypertension due to heart failure and idiopathic pulmonary arterial hypertension. Int J Cardiol 223:723–728
Denault AY, Haddad F, Jacobsohn E, Deschamps A (2013) Perioperative right ventricular dysfunction. Curr Opin Anaesthesiol 26:71–81
Judge O, Ji F, Fleming N, Liu H (2015) Current use of the pulmonary artery catheter in cardiac surgery: a survey study. J Cardiothorac Vasc Anaesth 29:69–75
Metkus TS, Tampakakis E, Mullin CJ, Houston BA, Kolb TM, Mathai SC, Damico R, Maron BA, Hassoun PM, Brower RG, Tedford RJ (2017) Pulmonary arterial compliance in acute respiratory distress syndrome: clinical determinants and association with outcome from the fluid and catheter treatment trial cohort. Crit Care Med 45:422–429
Pinsky MR (2017) Exploring the dark side of the moon: pulmonary vascular dysfunction in acute respiratory distress syndrome. Crit Care Med 45:559–561
Hrymak C, Strumpher J, Jacobsohn E (2017) Acute right ventricle failure in the intensive care unit: assessment and management. Can J Cardiol 33:61–71
Hoeper MM, Maier R, Tongers J, Niedermeyer J, Hohlfeld JM, Hamm M, Fabel H (1999) Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med 160:535–541
Combes A, Berneau JB, Luyt CE, Trouillet JL (2004) Estimation of left ventricular systolic function by single transpulmonary thermodilution. Intensive Care Med 30:1377–1383
Foris V, Kovacs G, Tscherner M, Olschewski A, Olschewski H (2013) Biomarkers in pulmonary hypertension: what do we know? Chest 144:274–283
Lankeit M, Kempf T, Dellas C, Cuny M, Tapken H, Peter T, Olschewski M, Konstantinides S, Wollert KC (2008) Growth differentiation factor-15 for prognostic assessment of patients with acute pulmonary embolism. Am J Respir Crit Care Med 177:1018–1025
Lankeit M, Dellas C, Panzenböck A, Skoro-Sajer N, Bonderman D, Olschewski M, Schäfer K, Puis M, Konstantinides S, Lang IM (2008) Heart-type fatty acid-binding protein for risk assessment of chronic thromboembolic pulmonary hypertension. Eur Respir J 31:1024–1029
Puls M, Dellas C, Lankeit M, Olschewski M, Binder L, Geibel A, Reiner C, Schäfer K, Hasenfuss G, Konstantinides S (2007) Heart-type fatty acid-binding protein permits early risk stratification of pulmonary embolism. Eur Heart J 28:224–229
Huang SJ, Orde S (2013) From speckle tracking echocardiography to torsion: research tool today, clinical practice tomorrow. Curr Opin Crit Care 19:250–257
Fine NM, Chen L, Bastiansen PM, Frantz RP, Pellikka PA, Oh JK, Kane GC (2013) Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging 6:711–721
Orde SR, Pulido JN, Masaki M, Gillepsie S, Spoon JN, Kane GC, Oh JK (2014) Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function. Crit Care 18:R149
Amsallem M, Sweatt AJ, Aymani MC, Kuznetsova T, Selej M, Lu HQ, Mercier O, Fadel E, Schnittger I, McConnell MV, Rabinovitch M, Zamanian RT, Haddad F (2017) Right-heart end-systolic remodelling index strongly predicts outcomes in pulmonary arterial hypertension: comparison with validated models. Circ Cardiovasc Imaging 10:e005771. https://doi.org/10.1161/circimaging.116.005771
Shimada YJ, Shiota M, Siegel RJ, Shiota T (2010) Accuracy of right ventricular volumes and function determined by three-dimensional echocardiography in comparison with magnetic resonance imaging: a meta-analysis study. J Am Soc Echocardiogr 23:943–953
Smith BC, Dobson G, Dawson D, Charalampopoulos A, Grapsa J, Nihoyannopoulos P (2014) Three-dimensional speckle tracking of the right ventricle: toward optimal quantification of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol 64:41–51
Laser KT, Horst J-P, Barth P, Kelter-Klöpping A, Haas NA, Burchert W, Kececioglu D, Köperich H (2014) Knowledge-based reconstruction of right ventricular volumes using real-time three-dimensional echocardiographic as well as cardiac magnetic resonance images: comparison with a cardiac magnetic resonance standard. J Am Soc Echocardiogr 27:1087–1097
Vonk Noordegraaf A, Haddad F, Bogaard HJ, Hassoun PM (2015) Noninvasive imaging in the assessment of the cardiopulmonary vascular unit. Circulation 131:899–913
Galea N, Carbone I, Cannata D, Cannavale G, Conti B, Galea R, Frustaci A, Catalano C, Francone M (2013) Right ventricular cardiovascular magnetic resonance imaging: normal anatomy and spectrum of pathological findings. Insights Imaging 4:213–223
Spruijt OA, Di Pasqua MC, Bogaard HJ, van der Bruggen CE, Oosterveer F, Marcus JT, Vonk-Noordegraaf A, Handoko ML (2017) Serial assessment of right ventricular systolic function in patients with precapillary pulmonary hypertension using simple echocardiographic parameters: a comparison with cardiac magnetic resonance imaging. J Cardiol 69:182–188
Spruijt OA, Vissers L, Bogaard HJ, Hofman MB, Vonk-Noordegraaf A, Marcus JT (2016) Increased native T1-values at the interventricular insertion regions in precapillary pulmonary hypertension. Int J Cardiovasc Imaging 32:451–459
Masci PG, Francone M, Desmet W, Ganame J, Todiere G, Donato R, Siciliano V, Carbone I, Mangia M, Strata E, Catalano C, Lombardi M, Agati L, Janssens S, Bogaert J (2010) Right ventricular ischemic injury in patients with acute ST-segment elevation myocardial infarction: characterization with cardiovascular magnetic resonance. Circulation 122:1405–1412
Maury E, Arrivé L, Mayo PH (2017) Intensive Care Medicine in 2050: the future of medical imaging. Intensive Care Med 43:1132–1137
D’Angelo T, Grigoratos C, Mazziotti S, Bratis K, Pathan F, Blandino A, Elen E, Puntmann VO, Nagel E (2017) High-throughput gadobutrol-enhanced CMR: a time and dose optimization study. J Cardiovasc Magn Reson 19:83
Haddad F, Doyle R, Murphy D, Hunt S (2008) Right ventricular function in cardiovascular disease, part II. Pathophysiology, clinical importance, and management of right ventricular failure. Circulation 117:1717–1731
Dalabih M, Rischard F, Mosier JM (2014) What’s new: the management of acute right ventricular decompensation of chronic pulmonary hypertension. Intensive Care Med 40:1930–1933
Dell’Italia LJ, Starling MR, Blumhardt R, Lasher JC, O’Rourke RA (1985) Comparative effects of volume loading, dobutamine, and nitroprusside in patients with predominant right ventricular infarction. Circulation 72:1327–1335
Belenkie I, Dani R, Smith ER, Tyberg JV (1989) Effects of volume loading during experimental acute pulmonary embolism. Circulation 80:178–188
Mitchell JR, Whitelaw WA, Sas R, Smith ER, Tyberg JV, Belenkie I (2005) RV filling modulates LV function by direct ventricular interaction during mechanical ventilation. Am J Physiol Heart Circ Physiol 289:H549–H557
Belenkie I, Dani R, Smith ER, Tyberg JV (1988) Ventricular interaction during experimental acute pulmonary embolism. Circulation 8:761–768
Belenkie I, Sas R, Mitchell J, Smith ER, Tyberg JV (2004) Opening the pericardium during pulmonary artery constriction improves cardiac function. J Appl Physiol 96:917–922
Tyberg JV, Grant DA, Kingma I, Moore TD, Sun Y, Smith ER, Belenkie I (2000) Effects of positive intrathoracic pressure on pulmonary and systemic hemodynamics. Respir Physiol 119:171–179
Boulate D, Arthur Ataam J, Connolly AJ, Giraldeau G, Amsallem M, Decante B, Lamrani L, Fadel E, Dorfmuller P, Perros F, Haddad F, Mercier O (2017) Early development of right ventricular ischemic lesions in a novel large animal model of acute right heart failure in chronic thromboembolic pulmonary hypertension. J Cardiac Fail 23:876–886
Marik PE, Baram M, Vahid B (2008) Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 134:172–178
Monnet X, Marik PE, Teboul JL (2016) Prediction of fluid responsiveness: an update. Ann Intensive Care 6:111
Vieillard-Baron A, Evrard B, Repessé X, Maizel J, Jacob C, Goudelin M, Charron C, Prat G, Slama M, Geri G, Vignon P (2018) Limited value of end-expiratory inferior vena cava diameter to predict fluid-responsiveness. Impact of intra-abdominal pressure. Intensive Care Med. https://doi.org/10.1007/s00134-018-5067-2
Vignon P, Repessé X, Bégot E, Léger J, Jacob C, Bouferrache K, Slama M, Prat G, Vieillard-Baron A (2017) Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med 195:1022–1032
Monnet X, Marik P, Teboul JL (2016) Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis. Intensive Care Med 42:1935–1947
Ghignone M, Girling L, Prewitt RM (1984) Volume expansion versus norepinephrine in treatment of a low cardiac output complicating an acute increase in right ventricular afterload in dogs. Anesthesiology 60:132–135
Molloy WD, Lee KY, Girling L, Schick U, Prewitt RM (1984) Treatment of shock in a canine model of pulmonary embolism. Am Rev Respir Dis 130:870–874
Jardin F, Genevray B, Brun-Ney D, Margairaz A (1985) Dobutamine: a hemodynamic evaluation in pulmonary embolism shock. Crit Care Med 13:1009–1012
Morelli A, Teboul JL, Maggiore SM, Vieillard-Baron A, Rocco M, Conti G, De Gaetano A, Picchini U, Orecchioni A, Carbone I, Tritapepe L, Pietropaoli P, Westphal M (2006) Effects of levosimendan on right ventricular afterload in patients with acute respiratory distress syndrome: a pilot study. Crit Care Med 34:2287–2293
Russ M, Prondzinsky R, Carter J et al (2009) Right ventricular function in myocardial infarction complicated by cardiogenic shock: improvement with levosimendan. Crit Care Med 37:3017–3023
Anderson MB, Goldstein J, Milano C, Morris LD, Kormos RL, Bhama J, Kapur NK, Bansal A, Garcia J, Baker JN, Silvestry S, Holman WL, Douglas PS, O’Neill W (2015) Benefits of a novel percutaneous ventricular assist device for right heart failure: the prospective RECOVER RIGHT study of the Impella RP device. J Heart Lung Transplant 34:1549–1560
Atiemo AD, Conte JV, Heldman AW (2006) Resuscitation and recovery from acute right ventricular failure using a percutaneous right ventricular assist device. Catheter Cardiovasc Interv 68:78–82
Giesler GM, Gomez JS, Letsou G, Vooletich M, Smalling RW (2006) Initial report of percutaneous right ventricular assist for right ventricular shock secondary to right ventricular infarction. Catheter Cardiovasc Interv 68:263–266
Kapur NK, Paruchuri V, Korabathina R, Al-Mohammdi R, Mudd JO, Prutkin J, Esposito M, Shah A, Kiernan MS, Sech C, Pham DT, Konstam MA, Denofrio D (2011) Effect of a percutaneous mechanical circulatory support device for medically refractory right ventricular failure. J Heart Lung Transplant 30:1360–1367
Jardin F, Vieillard-Baron A (2007) Is there a safe plateau pressure in ARDS? The right heart only knows. Intensive Care Med 33:444–447
Lejeune P, Brimioulle S, Leeman M, Hallemans R, Melot C, Naeije R (1990) Enhancement of hypoxic pulmonary vasoconstriction by metabolic acidosis in dogs. Anesthesiology 73:256–264
Morimont P, Guiot J, Desaive T, Tchana-Sato V, Janssen N, Cagina A, Hella D, Blaffart F, Defraigne JO, Lambermont B (2015) Veno-venous extracorporeal CO2 removal improves pulmonary hemodynamics in a porcine ARDS model. Acta Anaesthesiol Scand 59:448–456
Brimioulle S, Lejeune P, Naeije R (1996) Effects of hypoxic pulmonary vasoconstriction on pulmonary gas exchange. J Appl Physiol (1985) 81:1535–1543
Writing group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome (ART) investigators, Cavalcanti AB et al (2017) Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 318:1335–1345
Vieillard-Baron A, Charron C, Caille V, Belliard G, Page B, Jardin F (2007) Prone position unloads the right ventricle in severe ARDS. Chest 132:1440–1446
Afshari A, Brok J, Moller AM, Wetterslev J (2010) Inhaled nitric oxide for acute respiratory distress syndrome and acute lung injury in adults and children: a systematic review with meta-analysis and trail sequential analysis. Cochrane Database Syst Rev 7:CD002787
George I, Xydas S, Topkara VK, Ferdinando C, Barnwell EC, Gableman L, Sladen RN, Naka Y, Oz MC (2006) Clinical indication for use and outcomes after inhaled nitric oxide therapy. Ann Thorac Surg 82:2161–2169
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
AVB has received Grant from GSK for conducting clinical research and is membership of the scientific advisory board. RN has relationship with drug companies including AOPOrphan Pharmaceuticals, Actelion, Reata, Lung Biotechnology Corporation and United Therapeutics. In addition to being investigator in trials involving these companies, relationships include consultancy service, research Grants, and membership of scientific advisory board. FH declares no conflict of interest with regards to the content of this manuscript. HJB declares research Grants from Actelion, GSK, Therabell and speaker fees from Actelion, GSK. TMB declares investigator initiated Grant from Bayer Pharmaceuticals NF declares no conflict of interest. TL declares conflict of interest with Bayer (speaker bureau), Actelion (consulting), Gilled (scientific review committee) and Eli Lilly (research reagents). SM declares no conflict of interest with regards to the content of this manuscript. SO declares no conflict of interest. GS declares no conflict of interest with regards to the content of this manuscript. MRP declares no conflict of interest with regards to the content of this manuscript.
Rights and permissions
About this article
Cite this article
Vieillard-Baron, A., Naeije, R., Haddad, F. et al. Diagnostic workup, etiologies and management of acute right ventricle failure. Intensive Care Med 44, 774–790 (2018). https://doi.org/10.1007/s00134-018-5172-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5172-2