Abstract
Purpose
We performed a systematic review and meta-analysis of studies investigating the passive leg raising (PLR)-induced changes in cardiac output (CO) and in arterial pulse pressure (PP) as predictors of fluid responsiveness in adults.
Methods
MEDLINE, EMBASE and Cochrane Database were screened for relevant original and review articles. The meta-analysis determined the pooled area under the ROC curve, the sensitivity, specificity and threshold for the PLR test when assessed with CO and PP.
Results
Twenty-one studies (991 adult patients, 995 fluid challenges) were included. CO was measured by echocardiography in six studies, calibrated pulse contour analysis in six studies, bioreactance in four studies, oesophageal Doppler in three studies, transpulmonary thermodilution or pulmonary artery catheter in one study and suprasternal Doppler in one study. The pooled correlation between the PLR-induced and the fluid-induced changes in CO was 0.76 (0.73–0.80). For the PLR-induced changes in CO, the pooled sensitivity was 0.85 (0.81–0.88) and the pooled specificity was 0.91 (0.88–0.93). The area under the ROC curve was 0.95 ± 0.01. The best threshold was a PLR-induced increase in CO ≥10 ± 2 %. For the PLR-induced changes in PP (8 studies, 432 fluid challenges), the pooled sensitivity was 0.56 (0.49–0.53), the pooled specificity was 0.83 (0.77–0.88) and the pooled area under the ROC curve was 0.77 ± 0.05. Sensitivity and subgroup analysis were consistent with the primary analysis.
Conclusions
PLR-induced changes in CO very reliably predict the response of CO to volume expansion in adults with acute circulatory failure. When PLR effects are assessed by changes in PP, the specificity of the PLR test remains acceptable but its sensitivity is poor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fundamentally, the only reason to give a patient a fluid challenge is to increase cardiac output (CO) [1]. Patients who increase their CO following a fluid challenge are known as fluid responders. Studies in diverse patient populations have demonstrated that only about 50 % of haemodynamically unstable patients are fluid responders [2]. In patients with acute circulatory failure, predicting whether volume expansion will actually induce a significant increase in CO has become a common practice, is recommended by International guidelines [3, 4] and has generated considerable research [2].
Among the tests and indices that have been developed to predict fluid responsiveness, the passive leg raising (PLR) test has gained considerable attention [4, 5]. The PLR is performed by raising the legs of the patient to 45° [6]. This results in a hydrostatic increase in the mean systemic pressure, thus mimicking the effects of volume expansion. In case of preload dependence of both ventricles, the resultant increase in central venous return will result in an increase in CO and venous return.
The substantial increase in cardiac preload induced by PLR [7] challenges preload dependence of both ventricles. One of the advantages of the PLR test is that it can be used in instances in which the fluid responsiveness indices that are based on the respiratory variation of stroke volume are not reliable, such as spontaneous breathing, cardiac arrhythmias, low lung compliance and low tidal volume [8]. Furthermore, no fluid is actually administered and the PLR can thereby be considered a reversible or “virtual” fluid challenge.
Following the first study demonstrating the accuracy of the PLR test [9], this test has been the subject of a number of publications. In 2010, a meta-analysis pooling the nine studies that had been published at that time confirmed its accuracy [10]. Since this meta-analysis, some original articles dealing with the PLR test have been published [11–23], some of them casting doubt on its reliability.
We conducted a systematic review of all these studies and performed a meta-analysis in order to assess the ability of PLR to predict fluid responsiveness, to determine the pooled threshold of the PLR-induced increase in CO (or surrogates) that should be considered as significant, and to compare the diagnostic accuracy of PLR when assessed by changes in CO (or surrogates) or by changes in arterial pulse pressure (PP). Our hypothesis was that the diagnostic ability of the PLR test is good when its effects are assessed on CO and less when its effects are assessed on PP.
Methods
Clinical research question
The clinical research question was: What is the sensitivity and specificity of the passive leg raising test to predict fluid responsiveness when assessing its effects on cardiac output and arterial pressure?
PICO statement
The PICO statement was the following:
-
P-patient, problem or population: Patients with acute circulatory failure in whom the effect of volume expansion on cardiac output is unknown and needs to be predicted.
-
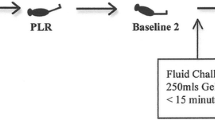
I-intervention: Passive leg raising (PLR), induced by moving the patient from the semi-recumbent or horizontal position
-
C-comparison, control or comparator: Fluid responsiveness was defined as a significant increase of cardiac output during a volume expansion.
-
O-outcomes: Ability of the PLR test to predict fluid responsiveness.
Identification of records
Our aim was to identify all studies evaluating the ability of the PLR test to predict a significant increase in CO, cardiac index, stroke volume or a surrogate (aortic flow velocity, aortic velocity time integral) compared to that induced by a subsequent fluid infusion. We only included studies that provided the sensitivity and specificity of the PLR test. Furthermore, only studies that were published in full text or accepted for publication in indexed journals were included in this analysis. We excluded studies in which fluid was not administered to test fluid responsiveness. We included only studies performed in adult patients. Figure 1 illustrates the search strategy.
We searched the US National Library of Medicine’s MEDLINE database, the EMBASE database and the Cochrane Database of Systematic Reviews for relevant studies published in English from 1966 to April 2015. We used the following medical subjects headings and keywords: “passive leg raising or raise”, “fluid or preload or volume responsiveness”, “fluid or preload challenge”, “preload dependence or independence or dependency or independency”, “functional haemodynamic monitoring” and “fluid therapy or management”. We also looked for relevant articles cited in review articles, commentaries and editorials. The search was performed iteratively until no new records could be found. The quality of the included studies was evaluated by using the QUADAS-2 scale [24]. The meta-analysis was performed according to the PRISMA statement (http://www.prisma-statement.org ).
Data extraction
Using a standardised data form, we extracted several data elements from the included studies including characteristics of the investigated population, the methods used to perform the PLR test and to assess its haemodynamic effects, the modalities of fluid administration and definition of fluid responsiveness, the correlation observed between the changes in CO or surrogates induced by volume expansion and by PLR, the number of true positives, true negatives, false positives and false negatives, the area under the receiver operation characteristics (ROC) curve and the best threshold of PLR-induced increase in CO or surrogates that was found to predict fluid responsiveness. If the ability of the PLR-induced changes in arterial PP to predict fluid responsiveness were also investigated, these results were also extracted. For studies in which more than one technique was used to estimate CO, we only included the technique which is considered to be the most reliable. When both calibrated pulse contour analysis and end-tidal carbon dioxide or bioreactance were used to estimate CO, only the results provided by the calibrated pulse contour analysis were evaluated. Indeed, end-tidal carbon dioxide has been suggested to reflect cardiac output changes in very few studies [25, 26] and the reliability of bioreactance has been questioned by some studies [13, 27, 28]. When the effects of PLR were assessed by echocardiography and by uncalibrated pulse contour analysis or end-tidal carbon dioxide or Doppler femoral peak velocity, only the results provided by echocardiography were included in the analysis. The reliability of uncalibrated pulse contour analysis in patients receiving vasopressors has been questioned [4, 29] and the reliability of Doppler femoral peak velocity to estimate CO changes has not been evaluated. When the effects of PLR were assessed by bioreactance and carotid Doppler, only the results provided by bioreactance were included in the analysis. No other publications support the use of carotid Doppler as a reflection of change in CO.
Assessment of risk of bias in included studies
Two authors (X.M. and P.E.M.) assessed the risk of bias of the included studies by following the criteria specified in the QUADAS-2 scale [24]. For the “patient selection” domain, they examined whether patients were consecutively included and whether inappropriate exclusions were avoided. For the “index test” domain, they examined whether the threshold used to define volume responsiveness was pre-specified. For the “reference standard” domain, they examined whether the result of volume expansion on CO was assessed without knowledge of the PLR test result and whether the reliability of the device used to estimate changes in CO induced by PLR is widely validated. Finally, for the “flow and timing” domain, the authors examined whether there was an appropriate interval between PLR and volume expansion, whether patients received the same volume expansion and whether all patients were included in the analysis. For each criterion, the risk was judged as high, low or unclear.
Statistical analysis
We performed a meta-analysis in order to determine the pooled area under the ROC curve, the pooled sensitivity and specificity and pooled threshold for PLR as a predictor of fluid responsiveness when its effects are assessed on CO (or surrogate) and when they are assessed on PP. The pooled correlation between the PLR-induced and the fluid-induced changes in CO (or surrogate) was also determined.
Homogeneity between studies was tested by the Chi-squared test (likelihood ratios test for sensitivity and specificity and Cochran’s Q test based upon inverse variance weights for likelihood ratios and diagnostic odds ratios) and by the I 2 index. To investigate a threshold effect, we also calculated the Spearman correlation coefficient between sensitivity and specificity. According to heterogeneity, a random effect model was used to perform meta-analysis.
In addition, in order to investigate the influence of study heterogeneity, we conducted subgroup analyses. We compared studies with ICU setting versus non-ICU setting, making the hypothesis that the PLR test could be more reliable in ICU patients. We compared studies with pulse contour analysis or echocardiography versus studies with other methods for measuring CO, making the hypothesis that the reliability of the PLR test is better when assessed by pulse contour analysis-derived cardiac output or by echocardiography than by other techniques. We compared studies with suprasternal Doppler or bioreactance versus studies with other methods for measuring CO, making the hypothesis that the reliability of the PLR test is poorer when assessed by suprasternal Doppler or bioreactance than by other devices. We compared studies where fluid responsiveness was defined by an increase in CO or surrogate ≥15 % versus studies with other definitions of fluid responsiveness, testing the hypothesis that the reliability of the PLR test is better when fluid responsiveness is defined by a larger increase in cardiac output. We compared studies where volume expansion was performed with crystalloids versus studies where it was performed by colloids, testing the hypothesis that the reliability of the PLR test is better when volume expansion is performed with colloids. Finally, we compared studies with the lowest risk of bias versus highest risk of bias, testing the hypothesis that the reliability of the PLR test is the best in studies with a highest risk of bias. To distinguish studies with the lowest and highest risks of bias, we attributed points to the risk of bias for each item of the QUADAS evaluation (one point for low risk, three points for high risk, two points for unclear risk). For each study, we calculated the sum of these points, which was used as an estimate of the global risk of bias. If the sum was below the median of the sums of all studies, the study was classified in the lowest risk of bias group, and the opposite if the sum was higher than the median. A subgroup analysis was also performed with the method of PLR (starting with the trunk at 0° or at 30°–45°) as moderating variables. The hypothesis was that the PLR test was more reliable to detect fluid responsiveness when started from the 45° semi-recumbent position than from the horizontal position. Causes of heterogeneity were also investigated by meta-regression based on the Littenberg and Moses linear model and including the same criteria as the subgroup analyses.
Results are expressed as mean (95 % confidence interval) or as mean ± standard deviation. The meta-analysis was performed with Meta-Disc v.1.4 (Universidad Complutense, Madrid, Spain) [30]. The additional statistical analysis was performed with MedCalc 15.2.2 (MedCalc Software, Mariakerke, Belgium).
Results
Characteristics of included studies
A flow diagram describing the study selection is provided in Fig. 1. We identified 21 studies (991 adult patients, 995 fluid challenges) that reported the ability of the PLR to predict fluid responsiveness [9, 11–23, 31–37]. The characteristics of the included studies are presented in Table 1. Thirteen studies [11–23] had not been included in the meta-analysis of Cavallaro et al. [10]. The vast majority of the studies were conducted in patients with acute circulatory failure. The absence of intra-abdominal hypertension was mentioned in four studies [14, 17, 18, 35]. The PLR was started from the supine position at 0° in four studies [21, 23, 31, 37] and from the semi-recumbent position in the remaining studies (Table 1).
Fluid responsiveness was defined by an increase in CO (or surrogate) by more than 15 % in 16 studies [9, 11–19, 31–36], 10 % in 2 studies [20, 21], 12 % in 1 study [37], 9 % in 1 study [22] and 7 % in 1 study [23] (Table 1).
CO was measured by echocardiography in 6 studies [16, 19, 32, 35–37], calibrated pulse contour analysis in 6 studies [12–14, 17, 18, 34], bioreactance in 4 studies [11, 20, 22, 23], oesophageal Doppler in 3 studies [9, 15, 31], either transpulmonary thermodilution or pulmonary artery catheter in 1 study [21] and suprasternal Doppler in 1 study [33] (Table 1). For the 2 studies in which the effects of PLR were assessed by echocardiography using both cardiac output and aortic velocity time integral [32, 37], we included only the cardiac output data.
For 2 studies in which the effects of PLR were assessed by calibrated pulse contour analysis and by end-tidal carbon dioxide [17] or bioreactance [13], only the results provided by the calibrated pulse contour analysis were evaluated. For the 3 studies in which the effects of PLR were assessed by echocardiography and by uncalibrated pulse contour analysis [35] or end-tidal carbon dioxide [15] or Doppler femoral peak velocity [36], only the results provided by echocardiography were included in the analysis. For the study in which the effects of PLR were assessed by bioreactance and carotid Doppler [20], we included only the results provided by bioreactance. The diagnostic accuracy of the PLR-induced changes in PP was investigated in 8 studies (392 fluid challenges) [9, 14, 15, 17, 18, 21, 34, 36].
The results of the QUADAS-2 evaluation are provided in Table 2 and Fig. 2. Among the sources of potential biases, 19 studies did not include consecutive patients (or no information was provided on this item).
Correlation between the PLR-induced and the fluid-induced changes in CO
The correlation between the changes in CO (or surrogate) induced by the PLR and volume expansion was reported in 14 studies (541 fluid challenges) [9, 13–19, 22, 31, 32, 34, 36, 37]. The pooled correlation coefficient was 0.76 (0.73–0.80) (p < 0.001) (Fig. 3).
Prediction of fluid responsiveness by the PLR-induced changes in CO
Among the 995 fluid challenges, 54 ± 9 % led to a positive response. All studies but four [11, 19, 21, 22] reported the value of percent changes in CO (or surrogate) induced by PLR in case of response to volume expansion. On average, the increase in CO in such cases was 20 ± 9 %.
For the PLR-induced changes in CO (or surrogate), the pooled sensitivity was 0.85 (0.81–0.88) and the pooled specificity was 0.91 (0.88–0.93) (Table 3). All studies but two [11, 20] reported the area under the corresponding ROC curve. The pooled AUC was 0.95 ± 0.01 (Table 3; Fig. 4). All the studies but one [23] reported the best threshold of the PLR-induced increase in CO (or surrogate) that predicted fluid responsiveness; this averaged 10 ± 2 %, ranging from 7 % [21] to 15 % [33] (Table 3).
Receiver operating characteristics curve (with 95 % confidence interval) for the prediction of fluid responsiveness by the effects of passive leg raising on cardiac output or surrogates. Circles represent each study included in the meta-analysis. The size of each solid circle indicates the size of each study
When including only studies in which PLR was started from the semi-recumbent position (n = 17, 783 fluid challenges), the pooled sensitivity for the PLR-induced changes in CO (or surrogate) was 0.85 (0.81–0.88) and the pooled specificity was 0.91 (0.88–0.94).
Prediction of fluid responsiveness by the PLR-induced changes in arterial PP
For the PLR-induced changes in PP (8 studies, 432 fluid challenges), the pooled sensitivity was 0.56 (0.49–0.53) and the pooled specificity was 0.83 (0.77–0.88). The pooled area under the ROC curve was 0.77 ± 0.05 (Fig. ESM2). The best threshold of PLR-induced increase in PP that predicted fluid responsiveness was 12 ± 4 % on average, ranging from 6 [17] to 18 % [14] (Table 3).
Investigation of heterogeneity and of causes of heterogeneity
The Spearman correlation coefficient between sensitivity and specificity was −0.178 (p = 0.441), indicating no threshold effect. The heterogeneity Chi-squared was 58 % for sensitivity and 47 % for specificity. The I 2 statistics was 67 % for sensitivity, 58 % for specificity, 34 % for the pooled ROC curve analysis and 10 % for the coefficient of correlation analysis.
Subgroup analyses are presented in Fig. ESM1. None of the covariates included in the meta-regression were found to be the significant source of heterogeneity (Table ESM1). In particular, the comparison between studies with pulse contour analysis or echocardiography versus studies with other devices, and between studies with bioreactance or suprasternal Doppler versus other devices had no influence on sensitivity and specificity. In studies with pulse contour analysis or echocardiography, the average threshold indicating a positive PLR was 10 ± 2 %. In the studies with bioreactance or suprasternal Doppler, it was 11 ± 3 %. Sensitivity and subgroup analyses were consistent with the primary analysis
Discussion
This meta-analysis which summarised the results of 21 studies conducted in 991 adult patients and including 995 fluid challenges demonstrated that the changes in CO (or surrogate) during a PLR test predicted fluid responsiveness with excellent pooled sensitivity and specificity. The pooled area under the ROC curve was 0.95 ± 0.01. The mean of the best threshold was a PLR-induced increase in CO of more than 10 ± 2 %. The PLR test less accurately predicted fluid responsiveness when its effects were assessed by the arterial PP.
The PLR test has been developed to predict whether volume expansion will increase CO during the resuscitation of patients with acute circulatory failure. Moving the patient to a position in which the trunk is horizontal and the lower limbs are lifted at 45° increases the stressed blood volume due to the gravitational transfer of some venous blood from the lower limbs and the abdomen toward the cardiac cavities. PLR significantly increases the mean systemic pressure [38], what promotes venous return. It increases the right and left cardiac preload to an extent that is sufficient to challenge preload responsiveness of both ventricles [7], although this has been challenged [21, 39]. The PLR is now accepted as a test for predicting fluid responsiveness in clinical practice. It is recommended by a recent consensus conference of the European Society of Intensive Care Medicine [4] and has been implemented in the bundles of the surviving sepsis campaign [5].
In 2010, Cavallaro and co-workers performed a systematic review and meta-analysis that included nine studies evaluating the diagnostic accuracy of the PLR test in predicting fluid responsiveness [10]. These authors concluded that the PLR-induced changes in CO reliably predicted fluid responsiveness regardless of ventilation mode, underlying cardiac rhythm and technique of CO measurement. Since this meta-analysis, additional studies have been published, some of them reporting less positive results [21, 22]. In addition, some studies and one editorial [40] have suggested that the PLR would not be reliable under specific conditions, such as insufficient increase in central venous pressure [21] or intra-abdominal hypertension [39]. Furthermore, recent publications have offered the opportunity to better establish the threshold of PLR-induced increase in CO that must be considered to detect volume responsiveness. Finally, the meta-analysis of Cavallaro et al. included only three studies investigating the prediction of fluid responsiveness provided by PLR when assessed by changes in PP [10]. All these arguments justified an updated meta-analysis.
Our meta-analysis confirms the meta-analysis performed by Cavallaro et al. [10] and reinforces the message that the PLR test is valid to test fluid responsiveness. Based on the results obtained in a large number of patients, we found that the area under the pooled ROC curve was large and close to one. In addition, the studies reported threshold values of PLR-induced increases in CO that were close to each other, which further reinforce the consistency of our positive conclusion.
Some authors have claimed that, in order to be a valid test of preload responsiveness, the PLR should increase the central venous pressure by more than 2 mmHg, reflecting an adequate increase in cardiac preload [21]. The present meta-analysis does not support this concept, as we demonstrated that the PLR was highly predictive of fluid responsiveness without taking into account how the PLR changed the central venous pressure. It has already been suggested that the results obtained by Lakhal et al. were explained by the fact that PLR was started from the supine position and not from the semi-recumbent position [41]. This may have resulted in a lesser increase in the mean systemic pressure, which is the upstream pressure of venous return, and thus of central venous pressure.
Mahjoub et al. have suggested that the PLR test produces false negative results in patients with intra-abdominal pressure [40]. The results of this study were not included in the present meta-analysis as it only included patients who were fluid responsive. This study has a number of limitations, including the fact that the investigators did not measure the intra-abdominal pressure during the test [40]. We postulate that the PLR may decrease intra-abdominal pressure by reducing the weight of the diaphragm and thorax on the abdominal cavity. Nevertheless, since the intra-abdominal pressure was not assessed in the studies included in the present meta-analysis, the question remains unresolved as to whether intra-abdominal hypertension reduces the diagnostic accuracy of the PLR test in predicting fluid responsiveness.
The diagnostic accuracy of the PLR test was poorer when its haemodynamic effects were assessed on the arterial PP than on CO, confirming what had been already observed by Cavallaro et al. [10]. This is likely due to the fact that changes in PP and CO are not well correlated and that changes in PP are a poor indicator of the changes in CO [43, 44]. When assessed through changes in PP, the specificity of the PLR test was 0.83. The sensitivity was much poorer. This suggests that, when assessed by changes in PP, the PLR should be taken into account only if it increases PP, and that even in such a case, this should be done cautiously. This finding illustrates an important shortcoming of the PLR test, that only the CO (or surrogate) should be used when performing the PLR test.
The importance of correct positioning of the patient when performing the PLR test has been previously emphasised [45]. Compared to starting the test from the horizontal lying position, starting it from the semi-recumbent position augments the effects of the test on cardiac preload [45], likely by mobilising the venous blood from the abdominal compartment in addition to that of the lower limbs [6]. This meta-analysis could not confirm this finding. However, this result should be interpreted with caution since PLR was started from the horizontal position in only four studies.
An important point to keep in mind is that a positive PLR test should not systematically lead to administering fluid. It is only in cases of circulatory failure, as assessed by low arterial pressure and/or signs of poor tissue perfusion, when the need for increasing CO is required, that fluid administration should be considered. In addition, the beneficial increase of CO induced by volume expansion in patients who are fluid responsive must always be balanced with the risk of excessive fluid administration, which may be harmful, especially in patients with septic shock [46], acute renal failure [47] and acute respiratory distress syndrome [48]. Of note, using the PLR test has never been demonstrated to improve survival. Fluid responsiveness is not associated with improved outcome. This is not surprising since it is a diagnostic tool. Nevertheless, as many diagnosis tools, the test is not required to change outcome to be useful.
Various methods of measuring CO were used in the studies included in this meta-analysis. This must be regarded as a limitation, since the reliability of the PLR test likely depends on the accuracy of the device used to measure CO [49]. In particular, the threshold used to define fluid responsiveness should be higher than the least significant change of the CO measurement method. While this least significant change has been reported to be lower than 5 % for echocardiography [50], pulse contour analysis [34, 51] or oesophageal Doppler [15], it has been reported to be higher for bioreactance [22, 52, 53], while, as far as we know, it has not been investigated for suprasternal Doppler. Subgroup analysis does not support that the reliability of the PLR test was influenced by the type of cardiac output monitoring device, including bioreactance and suprasternal Doppler. Nevertheless, some of the subgroups were small. Thus, it is reasonable to consider that the reliability of the PLR test may be less solid if assessed with less reliable measures of cardiac output.
The heterogeneity of the included studies represents a limitation of the meta-analysis. Nevertheless, no threshold effect was detected. Furthermore, both the subgroup analyses and the meta-regression argued against the influence of heterogeneity on the results. A further limitation of this study is that the included studies were mainly conducted in the ICU, the sample size was generally small and that several different methods of measuring of CO were used. Therefore, this systematic review is only applicable to the specific patient populations studied and the devices used to measure CO. In addition, this systematic review was not prospectively registered in Prospero, an international database of prospectively registered systematic reviews in health and social care, what may have increased the risk of reporting bias. Additional limitations include the fact that we did not include studies not reporting sensitivity/specificity, non-full-text studies, studies not in English, and unpublished studies. This may have also increased the risk of reporting bias. Since the reliability of the PLR test in cases of intra-abdominal hypertension and in cases of insufficient increase in central venous pressure was investigated in one study for each condition, the meta-analysis does not definitely come to a conclusion about this reliability of PLR in these circumstances. Finally, two of the authors (X.M. and J.L.T.) were the authors of a large number of the studies included in the meta-analysis. Nevertheless, this was not the case for the third author (P.E.M.), so that the risk of bias was minimized.
In conclusion, this meta-analysis shows that the PLR test is accurate to predict fluid responsiveness in the intensive care unit. Its accuracy is better when its haemodynamic effects are assessed by a direct measurement of CO than by the arterial PP.
References
Lira A, Pinsky MR (2014) Choices in fluid type and volume during resuscitation: impact on patient outcomes. Ann Intensive Care 4:38
Marik PE, Monnet X, Teboul JL (2011) Hemodynamic parameters to guide fluid therapy. Ann Intensive Care 1:1
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39(2):165–228
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40:1795–1815
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R (2015) Updated bundles in response to new evidence. In: Surviving sepsis campaign. http://www.survivingsepsis.org/sitecollectiondocuments/ssc_bundle.pdf (in press)
Monnet X, Teboul JL (2015) Passive leg raising: five rules, not a drop of fluid! Crit Care 19:18
Boulain T, Achard JM, Teboul JL, Richard C, Perrotin D, Ginies G (2002) Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 121:1245–1252
Monnet X, Teboul JL (2013) Assessment of volume responsiveness during mechanical ventilation: recent advances. Crit Care 17:217
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Cavallaro F, Sandroni C, Marano C, La Torre G, Mannocci A, De Waure C, Bello G, Maviglia R, Antonelli M (2010) Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med 36:1475–1483
Duus N, Shogilev DJ, Skibsted S, Zijlstra HW, Fish E, Oren-Grinberg A, Lior Y, Novack V, Talmor D, Kirkegaard H, Shapiro NI (2015) The reliability and validity of passive leg raise and fluid bolus to assess fluid responsiveness in spontaneously breathing emergency department patients. J Crit Care 30(217):e211–e215
Dong ZZ, Fang Q, Zheng X, Shi H (2012) Passive leg raising as an indicator of fluid responsiveness in patients with severe sepsis. World J Emerg Med 3:191–196
Kupersztych-Hagege E, Teboul JL, Artigas A, Talbot A, Sabatier C, Richard C, Monnet X (2013) Bioreactance is not reliable for estimating cardiac output and the effects of passive leg raising in critically ill patients. Br J Anaesth 111:961–966
Silva S, Jozwiak M, Teboul JL, Persichini R, Richard C, Monnet X (2013) End-expiratory occlusion test predicts preload responsiveness independently of positive end-expiratory pressure during acute respiratory distress syndrome. Crit Care Med 41:1692–1701
Monge Garcia MI, Gil Cano A, Gracia Romero M, Monterroso Pintado R, Perez Madueno V, Diaz Monrove JC (2012) Non-invasive assessment of fluid responsiveness by changes in partial end-tidal CO2 pressure during a passive leg-raising maneuver. Ann Intensive Care 2:9
Guinot PG, Zogheib E, Detave M, Moubarak M, Hubert V, Badoux L, Bernard E, Besserve P, Caus T, Dupont H (2011) Passive leg raising can predict fluid responsiveness in patients placed on veno–venous extracorporeal membrane oxygenation. Crit Care 15:R216
Monnet X, Bataille A, Magalhaes E, Barrois J, Le Corre M, Gosset C, Guerin L, Richard C, Teboul JL (2013) End-tidal carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med 39:93–100
Monnet X, Bleibtreu A, Ferré A, Dres M, Gharbi R, Richard C, Teboul JL (2012) Passive leg raising and end-expiratory occlusion tests perform better than pulse pressure variation in patients with low respiratory system compliance. Crit Care Med 40:152–157
Brun C, Zieleskiewicz L, Textoris J, Muller L, Bellefleur JP, Antonini F, Tourret M, Ortega D, Vellin A, Lefrant JY, Boubli L, Bretelle F, Martin C, Leone M (2013) Prediction of fluid responsiveness in severe preeclamptic patients with oliguria. Intensive Care Med 39:593–600
Marik PE, Levitov A, Young A, Andrews L (2013) The use of bioreactance and carotid Doppler to determine volume responsiveness and blood flow redistribution following passive leg raising in hemodynamically unstable patients. Chest 143:364–370
Lakhal K, Ehrmann S, Runge I, Benzekri-Lefevre D, Legras A, Dequin PF, Mercier E, Wolff M, Regnier B, Boulain T (2010) Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Med 36:940–948
Benomar B, Ouattara A, Estagnasie P, Brusset A, Squara P (2010) Fluid responsiveness predicted by noninvasive bioreactance-based passive leg raise test. Intensive Care Med 36:1875–1881
Kang WS, Kim SH, Kim SY, Oh CS, Lee SA, Kim JS (2014) The influence of positive end-expiratory pressure on stroke volume variation in patients undergoing cardiac surgery: an observational study. J Thorac Cardiovasc Surg 148:3139–3145
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Tautz TJ, Urwyler A, Antognini JF, Riou B (2010) Case scenario: increased end-tidal carbon dioxide: a diagnostic dilemma. Anesthesiology 112:440–446
Weil MH, Bisera J, Trevino RP, Rackow EC (1985) Cardiac output and end-tidal carbon dioxide. Crit Care Med 13:907–909
Conway DH, Hussain OA, Gall I (2013) A comparison of noninvasive bioreactance with oesophageal Doppler estimation of stroke volume during open abdominal surgery: an observational study. Eur J Anaesthesiol 30(8):501–508
Fagnoul D, Vincent JL, Backer DD (2012) Cardiac output measurements using the bioreactance technique in critically ill patients. Crit Care 16:460
Monnet X, Teboul JL (2015) Minimally invasive monitoring. Crit Care Clin 31:25–42
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31
Lafanechère A, Pène F, Goulenok C, Delahaye A, Mallet V, Choukroun G, Chiche JD, Mira JP, Cariou A (2006) Changes in aortic blood flow induced by passive leg raising predict fluid responsiveness in critically ill patients. Crit Care 10(5):R132
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL (2007) Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33:1125–1132
Thiel SW, Kollef MH, Isakow W (2009) Non-invasive stroke volume measurement and passive leg raising predict volume responsiveness in medical ICU patients: an observational cohort study. Crit Care 13:R111
Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL (2009) Predicting volume responsiveness by using the end-expiratory occlusion in mechanically ventilated intensive care unit patients. Crit Care Med 37:951–956
Biais M, Vidil L, Sarrabay P, Cottenceau V, Revel P, Sztark F (2009) Changes in stroke volume induced by passive leg raising in spontaneously breathing patients: comparison between echocardiography and Vigileo/FloTrac device. Crit Care 13:R195
Preau S, Saulnier F, Dewavrin F, Durocher A, Chagnon JL (2010) Passive leg raising is predictive of fluid responsiveness in spontaneously breathing patients with severe sepsis or acute pancreatitis. Crit Care Med 38:989–990
Maizel J, Airapetian N, Lorne E, Tribouilloy C, Massy Z, Slama M (2007) Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med 33:1133–1138
Guérin L, Teboul JL, Persichini R, Dres M, Richard C, Monnet X (2015) Effects of passive leg raising and volume expansion on mean systemic pressure and venous return in shock in humans. Crit Care 19:411. doi:10.1186/s13054-015-1115-2
Mahjoub Y, Pila C, Friggeri A, Zogheib E, Lobjoie E, Tinturier F, Galy C, Slama M, Dupont H (2009) Assessing fluid responsiveness in critically ill patients: false-positive pulse pressure variation is detected by Doppler echocardiographic evaluation of the right ventricle. Crit Care Med 37:2570–2575
Malbrain ML, Reuter DA (2010) Assessing fluid responsiveness with the passive leg raising maneuver in patients with increased intra-abdominal pressure: be aware that not all blood returns! Crit Care Med 38:1912–1915
Monnet X, Teboul JL (2010) Passive leg raising: keep it easy! Intensive Care Med 36:1445–1446
Mahjoub Y, Touzeau J, Airapetian N, Lorne E, Hijazi M, Zogheib E, Tinturier F, Slama M, Dupont H (2010) The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med 38:1824–1829
Monnet X, Letierce A, Hamzaoui O, Chemla D, Anguel N, Osman D, Richard C, Teboul JL (2011) Arterial pressure allows monitoring the changes in cardiac output induced by volume expansion but not by norepinephrine*. Crit Care Med 39:1394–1399
Pierrakos C, Velissaris D, Scolletta S, Heenen S, De Backer D, Vincent JL (2012) Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med 38:422–428
Jabot J, Teboul JL, Richard C, Monnet X (2009) Passive leg raising for predicting fluid responsiveness: importance of the postural change. Intensive Care Med 35:85–90
Marik PE (2014) Early management of severe sepsis: concepts and controversies. Chest 145:1407–1418
Prowle JR, Kirwan CJ, Bellomo R (2014) Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol 10:37–47
Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, Teboul JL, Monnet X (2013) Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome. Crit Care Med 41:472–480
Marik PE (2013) Noninvasive cardiac output monitors: a state-of the-art review. J Cardiothorac Vasc Anesth 27:121–134
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, Zoric L, Suehs C, de La Coussaye JE, Molinari N, Lefrant JY (2011) An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology 115:541–547
Hamzaoui O, Monnet X, Richard C, Osman D, Chemla D, Teboul JL (2008) Effects of changes in vascular tone on the agreement between pulse contour and transpulmonary thermodilution cardiac output measurements within an up to 6-hour calibration-free period. Crit Care Med 36:434–440
Squara P, Denjean D, Estagnasie P, Brusset A, Dib JC, Dubois C (2007) Noninvasive cardiac output monitoring (NICOM): a clinical validation. Intensive Care Med 33:1191–1194
Marque S, Cariou A, Chiche JD, Squara P (2009) Comparison between Flotrac–Vigileo and bioreactance, a totally noninvasive method for cardiac output monitoring. Crit Care 13:R73
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Jean-Louis Teboul and Xavier Monnet are members of the Medical Advisory Board of Maquet. They are the authors of the majority of the studies included in this meta-analysis. Paul E Marik has no conflicts to disclose.
Additional information
Take-home message: In this meta-analysis of 21 studies including 991 adult patients in whom 995 fluid challenges were performed, total, we found that the changes in cardiac output induced by a passive leg raising test are highly reliable in predicting fluid responsiveness. When its effects were assessed by changes in arterial pulse pressure, the specificity of passive leg raising remains good but its sensitivity is poor.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Monnet, X., Marik, P. & Teboul, JL. Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis. Intensive Care Med 42, 1935–1947 (2016). https://doi.org/10.1007/s00134-015-4134-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4134-1