Abstract
Purpose
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a controversial haemorrhage control intervention often touted as the bridge to definitive haemorrhage control. This review summarizes the evolution of REBOA from its inception to the latest applications with an emphasis on clinical outcomes.
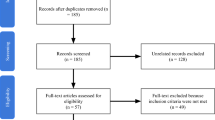
Methods
This is a narrative review based on a selective review of the literature.
Results
REBOA remains a rarely utilized intervention in trauma patients. Complications have remained consistent over time despite purported improvements in catheter technology. Ischemia-reperfusion injuries, end-organ dysfunction, limb ischemia, and amputations have all been reported. Evidence-based guidelines are lacking, and appropriate indications and the ideal patient population for this intervention are yet to be defined.
Conclusion
Despite the hype, purported technological advancements, and the mirage of high-quality studies over the last decade, REBOA has failed to keep up to its expectations. The quest to find the solution for uncontrolled NCTH remains unsolved.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trauma is one of the leading causes of death worldwide, with one person dying every 8 s secondary to injury [1]. Haemorrhage is the leading cause of potentially preventable death in these patients with 80% of the deaths in military trauma and 40% in civilian trauma being caused due to exsanguination [2, 3]. Despite advances in trauma resuscitation such as balanced component transfusion, massive transfusion protocol, permissive hypotension, damage control surgery, and improvements in interfacility transfer, mortality in hypotensive trauma patients has not changed in the last two decades [4]. The advent of tourniquets has helped to reduce bleeding from compressible sites, however, haemorrhage below the trunk, also called noncompressible torso haemorrhage (NCTH) remains a major issue to address. Traditionally, NCTH in patients in cardiac arrest or imminent cardiac arrest was controlled using resuscitative thoracotomy with aortic cross-clamping (RTACC), a highly invasive procedure. This led to increased interest in developing alternate methods to achieve haemorrhage control in the pre-hospital and emergency department settings in patients with NCTH [5].
Brief history of the aortic balloons in trauma
The use of intra-aortic balloon occlusion (IABO) for haemorrhage control was first introduced by Lt. Col. Carl W. Hughes in 1954 during the Korean conflict. He described their experience of using IABO catheters in two trauma patients of whom both died and speculated that earlier use may be beneficial [6]. Gupta et al. implemented IABO in 21 hemodynamically unstable patients of whom 7 survived, but the complication rate was as high as 35%, with complications like paraplegia, aortic injury, and femoral arterial thrombosis [6, 7]. Subsequently, the device did not gain prominence due to high rates of complications and mortality.
The resurgence of aortic balloons in modern trauma resuscitation
Some preclinical studies rekindled the interest in resuscitative endovascular balloon occlusion of the aorta (REBOA) and reignited the debate on its use [9, 10]. A case series published by Brenner et al. in 2013 described six successful cases of REBOA placement with no haemorrhage related mortality. This was one of the earliest studies where REBOA proved to be beneficial in human subjects [11]. Since then, REBOA has been studied in various scenarios. However, several studies have failed to show any significant benefit and reported increased complications and mortality with the use of REBOA [12, 13].
Purported advancements in REBOA technology
Various modifications to the REBOA catheters over the last two decades have shown success in the preclinical studies which increased our hopes on this technology. Firstly, the size of catheters has reduced from 14 Fr in 2010 to 7 Fr and 4 Fr today. Coda balloons (Cook Medical) were used in trauma patients for several years before the advent of wire-free balloon catheters. However, due to the requirement of at least 12 Fr sheath for these balloons, various smaller REBOA-dedicated devices were developed including ER-REBOA (Prytime Medical) and Rescue Balloon (Tokay Medical Products). These wire-free balloon catheters also eliminated the need for fluoroscopy, which was required for optimal deployment of previous generation of devices. Moreover, the current catheters also enabled partial occlusion, with the capability of continuous pressure monitoring proximal and distal to the balloon, which was once considered difficult to achieve. This helps in maintaining flow distal to the balloon to reduce downstream ischemia due to complete occlusion. These newer catheters also come with compliant balloons, atraumatic curved tips with radio-opaque markers for visualization on X-ray. However, despite these advancements, this technology continues to be associated with poor outcomes [5].
Indications
Various guidelines/algorithms/protocols have been proposed to guide the use of REBOA in trauma patients. However, it is important to note that these existing protocols for REBOA are derived from expert opinions and not quality data. In a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians regarding the clinical use REBOA in civilian trauma systems, it is stated that the quality of clinical evidence to support REBOA use in trauma patients is poor with no Class I or II data and thus the existing data must be interpreted with caution [8].
According to the guidelines, for patients arriving in traumatic arrest, use of REBOA must be restricted to those patients with an organized rhythm detected on electrocardiogram or cardiac conduction on ultrasound. Additionally, it is suggested that patients that sustained penetrating injuries and underwent CPR for less than 15 min with source of bleeding in the abdomen/pelvis/extremity with absence of devastating head injury may be candidates for REBOA placement. For patients with signs of life on admission, decision for placement of REBOA must be determined by assessment of vital parameters, response to resuscitation, likely pattern of injury, and the source of haemorrhage [9]. In a 2016 study by Joseph et al. 55% of patients with potential anatomic indications for REBOA did not ultimately have physiologic indications after accounting for response to resuscitation [10]. In such cases, REBOA may be inserted in patients who are transient responders or non-responders after confirmation of subdiaphragmatic source of bleeding using ultrasound. However, one limitation of this argument is the lack of consensus on the definition of the transient response to resuscitation. In hemodynamically unstable patients with isolated pelvic fractures, the primary focus is to stop the haemorrhage using pelvic packing/REBOA/pelvic fixation. Since, REBOA is a less invasive intervention, its use in this patient population must be assessed further.
Contraindications
Strict contraindications for REBOA placement accepted by most providers include patients with aortic injuries, haemorrhage proximal to the balloon such as neck, axilla, and superior mediastinum. REBOA may be hazardous in traumatic brain injuries with reports of worsening intracranial bleeds after balloon inflation [11]. Relative contraindications include older adults, presence of profound comorbidities or terminal illness. Among patients penetrating injuries with thoracoabdominal trajectory, REBOA may be considered after excluding thoracic haemorrhage using ultrasound.
Brief review of the procedure
The key steps to achieve aortic occlusion involves vascular access, balloon positioning, balloon inflation, balloon deflation, and sheath removal. Arterial access is the first and rate limiting step in REBOA and can be achieved through percutaneous or cut-down approach. Percutaneous access can be obtained either by blind puncture or under ultrasound guidance. In the context of this procedure, the aorta is divided into three zones [12]. Zone 1 extends from the left subclavian artery to the celiac artery, zone 2 extends between the celiac artery and the lowest renal artery, and zone 3 represents the infrarenal abdominal aorta from the lowest renal artery to the bifurcation of the aorta. Choosing appropriate location for inflation is a crucial step, as the more proximal the balloon, more severe is the downstream ischemia. Zone 1 REBOA is used in patients with subdiaphragmatic source of bleeding, whereas zone 3 is preferred for patients with isolated pelvic fractures.
Once the balloon is inserted in the desired zone, it must be cautiously inflated until the contralateral femoral pulse is lost to achieve complete occlusion. The joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians states that total aortic occlusion times greater than 30 min are associated with increased ischemic complications and risk of mortality and hence recommends the target occlusion times of less than 30 min [8]. To combat ischemic complications, various balloon inflation techniques have been developed such as partial occlusion (pREBOA), or intermittent occlusion (iREBOA), as opposed to complete occlusion (cREBOA). These newer techniques allow some distal perfusion but must be carefully performed with continuous monitoring of aortic pressure, as small changes in aortic lumen can lead to drastic changes in the flow. In certain animal models, pREBOA and iREBOA have been shown to be superior to cREBOA in terms of ischemic complications [13, 14] and extending survival beyond the golden hour [15]. Once occlusion has been achieved, the primary aim must be to achieve definitive haemorrhage control either through appropriate surgery or angioembolization. These experimental studies investigated short term physiological outcomes, which could be different from long-term survival and complications.
Complications of REBOA
One of the primary reasons for the resistance behind adopting REBOA is the high rates of complications following this procedure. Complications may be due to the device, or technique, or the mechanism of action of REBOA itself. Every step of the procedure is associated with some important complications that REBOA providers must be aware of.
Device related complications
At the beginning of last decade, larger profile REBOA devices were more common with recommended sheath diameters of 12 Fr or higher which have been linked with high rates of complications [16]. Common complications related to sheaths are injuries to the common femoral arteries requiring repair and distal limb ischemia leading to compartment syndrome and amputation [17]. The replacement of 14 Fr to 7 Fr devices with even smaller 4 Fr devices resulted in a reduction of the local complications. However, there have been discordant results regarding the sheath size and complications. In a systematic review and meta-analysis by Shum-Tim et al., the authors found a slight decrease (odds ratio, 0.87; 95% confidence interval, 0.75–0.99) in the incidence of vascular access complications with 7 Fr devices [18]. However, another meta-analysis by Foley et al. found no difference in access complications between 7 Fr and > 10 Fr sheaths [19]. In a 2022 review of 418 patients from the AAST Aortic Occlusion Registry, the incidence of arterial access-related extremity ischemia and/or distal embolism was 8.6% [16].
Technique related complications
As previously mentioned, gaining arterial access is the rate-limiting step of this procedure, and can be achieved through either percutaneous method via blind puncture or under ultrasound guidance, or through surgical cut-down. Very often, trauma patients requiring REBOA are in shock making it difficult to accurately palpate femoral vessels and gain access blindly. Hence, ultrasound guided access became popular and has been shown to be successful in animal studies [20]. However, in an analysis of ABO (aortic balloon occlusion) Trauma Registry and the AORTA (Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery) database, Duchesne et al. found no significant difference in overall complication rates or mortality between percutaneous and ultrasound guided methods [21]. Consistent with these findings, Foley et al. in their meta-analysis also reported no significant difference in the risk of access complications between ultrasound guided and percutaneous landmark guided access [19]. Gaining arterial access has been shown to be more successful by cut-down access compared to percutaneous ultrasound guided access [22], however, cut-down access has also been linked with higher mortality rates [21]. Assessment of distal limb perfusion after REBOA is important to identify ischemic complications, and any suspicion should warrant further diagnostic testing and consultation with vascular surgery. Overinflation of the balloon can lead to balloon rupture and injury to the aorta, which can be devastating. Inflation of balloon in the iliac vessels can also lead to thrombosis and rupture. Since thrombus formation can occur anywhere along the length of the catheter, it is vital to check for Doppler signals after balloon deflation.
Mechanism related complications
A major arena of complications following REBOA are in fact due to the procedure of balloon occlusion itself. There have been reports of worsening haemorrhage proximal to the balloon and worsening of intracranial haemorrhage following inflation [11]. Downstream migration of the catheter has also been reported as a common complication [23]. Inflation of the balloon leads to severe ischemia distal to the balloon, which leads to a plethora of consequences due to ischemia reperfusion injuries. Reperfusion is associated with various electrolyte abnormalities including persistent hypoglycaemia, hypocalcaemia, hyperkalaemia, and lactic acidosis. Moreover, these disturbances appear to be at the peak about 30–60 min after deflation [24]. Hence, REBOA providers must be vigilant regarding such complications. Although partial occlusion has been shown to be beneficial in reducing these complications in animal models, a recent report from the ABO registry showed no significant difference in mortality between partial occlusion and total aortic occlusion. Moreover, complications tended to be higher in the partial occlusion group [25].
Can we really overcome the complications of REBOA?
Various efforts have been made to overcome the above discussed complications, including developing lower profile devices, ultrasound-guided vascular access, and partial occlusion strategies. However, these purported advancements failed to reduce the complications indicating the strong link between complications and nature of the procedure in itself. All the REBOA providers, teams, and centres should be well versed with the technique and complications and prepared to address them to prevent further damage. However, even with proper training the results have been disappointing. In a previous report detailing a level I trauma centre’s experience with REBOA where all trauma, emergency department, and operating room staff underwent training, the providers only placed 9 REBOAs in the first year out of which 4 patients died, and 5 developed complications [26]. Hence, despite training, complications must be expected, and surgeons and institutions must be ready to deal with these complications.
The importance of time
Time is one of the important factors that is associated with survival in haemorrhaging trauma patients. Earlier resuscitative interventions and definitive haemorrhage control surgery have been shown to impact the outcomes [27,28,29]. In a study comparing REBOA with RTACC, Romagnoli et al. reported that the median time from arterial access to aortic occlusion was significantly longer in the REBOA group compared to the median time from skin incision to aortic occlusion in the RTACC group [30]. It is important to note that bleeding control achieved through REBOA is transient and the need to perform definitive surgery to control the source of bleeding persists. Even in the recently concluded randomized UK-REBOA trial, the median time to definitive haemorrhage control surgery was longer in the REBOA group with an average difference of 19 min between the groups, indicating the delay in time to surgery caused by REBOA [31]. Hence, it may be more useful if REBOA is used as an intraoperative adjunct to control bleeding rather than a preoperative resuscitative intervention.
Clinical data
The initial enthusiasm was mainly based on small studies and expert opinion. Despite promising results from preclinical experiments, REBOA has been shown to be associated with worse outcomes in large clinical studies. In 2015 and 2016, the first large studies from Japan reported significantly higher mortality rates after REBOA use in severe polytrauma [32, 33]. Another TQIP study in 2019 by Joseph et al. reported that REBOA was associated with increased mortality, AKI and lower limb amputations. [30].
The only randomized trial which included 90 exsanguinating hemorrhagic patients in 16 major trauma centers, demonstrated that REBOA was associated with worse outcomes. The trial was stopped after the second interim analysis, because the prespecified stopping rule for harm was met. In the REBOA group there was a significantly higher 90-day mortality and bleeding related death [31]. Linderman et al., performed an expanded analysis of the National Trauma Data Bank (NTDB), and concluded that REBOA was associated with increased mortality, and that any unmeasured confounder would need to be more closely related to REBOA and mortality than hypotension, abdominal organ injury, and pelvic fracture or having an ISS greater than 25, to explain the higher mortality in the REBOA group, the existence of which is unlikely [34].
It has been suggested that REBOA might be beneficial in patients with pelvic fractures [35, 36]. However, the available evidence is very poor. Asmar et al. [32] analyzed 156 patients with pelvic trauma undergoing PPP or REBOA and reported that REBOA was associated with improved outcomes compared to PPP. However, they did not include patients who did not receive REBOA or PPP. Werner et al. [33] compared PPP with REBOA and suggested that the combination of the two procedures might be beneficial. Recent publications reported that PPP may not be beneficial in bleeding from pelvic fractures [37].
However, newer, larger and better designed studies failed to show any benefit of REBOA in patients with pelvic fractures [38, 39]. In a recent matched cohort TQIP study, 93 REBOA patients were matched with 279 without REBOA. REBOA was associated with significantly higher mortality and venous thromboembolism [39]. Moreover, the use of REBOA in severe traumatic brain injury patients has failed to show benefit as well. Another recent study from TQIP where 434 REBOA patients were matched to 859 without REBOA showed that the use of REBOA in severe traumatic brain injury patients was associated with significantly higher in-hospital mortality, acute kidney injury and sepsis [40].
In addition, REBOA has been linked with various complications including thromboembolic complications, compartment syndrome, lower extremity amputations, and acute kidney injury [17, 41, 42]. Although partial REBOA has shown some promise in preclinical studies, its benefit in human studies is yet to be determined.
Current state and the future of REBOA
Despite the increased interest in REBOA, this remains a rarely performed intervention. In a survey conducted in 2018 among trauma medical directors (TMDs) of 158 trauma centres in the United States, only 15 TMDs reported using REBOA for pelvic fracture management. In the prospective observational Emergent Truncal Hemorrhage Observational Study, Moore et al. reported that REBOA was placed in 75 of the 8,166 patients with a mortality rate of 52%. Three of the six participating centres contributed to 79% of the REBOA interventions performed [5]. In the recently concluded pragmatic, bayesian, randomized clinical trial conducted at 16 major trauma centres in the United Kingdom, mortality was found to be higher in the REBOA group at all time points. In addition, there were more deaths due to bleeding in the REBOA group compared to standard of care group. Nearly 1/3rd of patients in the REBOA group responded to other resuscitative measures and hence aortic occlusion was not necessary, and arterial access was attempted but could not be achieved in nearly 1/5th of the patients. Importantly, the trial was stopped as the prespecified stopping rule for harm was met in the interim analysis [31]. The Partial REBOA Outcomes Multicentre ProspecTive (PROMPT) Study is the first large-scale multicentre prospective study for partial REBOA which will be conducted across 8 US trauma centres will help us further understand the clinical utility of partial REBOA [43]. In a situation where the guidelines for REBOA use are developed from expert consensus, high quality unbiased studies with good methodology are necessary to further understand the role of REBOA in modern resuscitation. In a study including 288 articles, disclosures were inaccurate in 88% of the articles where authors who had conflicts of interest with the industry [44].
Conclusions
Despite the hype, purported technological advancements, and mirage of high-quality studies over the last decade, REBOA has failed to keep up to its expectations. Its use remains limited, and the ideal patient population has not yet been determined. Training is unstandardized and the variable hospital privileges add another barrier towards its adoption. Complications attributed to REBOA are real and have remained consistent over the years. Conflicts of interest with the industry are prevalent among pro-REBOA centres and providers. It is time to declare REBOA as a collective spectacular failure in modern trauma resuscitation and realize that every step that we put in this direction took us way behind in reaching our goal of improving patient care and reducing mortality due to haemorrhage. The quest to find the solution for uncontrolled NCTH remains unsolved.
Data availability
No datasets were generated or analysed during the current study.
References
Stannard A, Morrison JJ, Scott DJ, Ivatury RA, Ross JD, Rasmussen TE. The epidemiology of noncompressible torso hemorrhage in the wars in Iraq and Afghanistan. J Trauma Acute Care Surg. 2013;74(3):830–4.
Van Oostendorp S, Tan E, Geeraedts L. Prehospital control of life-threatening truncal and junctional haemorrhage is the ultimate challenge in optimizing trauma care; a review of treatment options and their applicability in the civilian trauma setting. Scand J Trauma Resusc Emerg Med. 2016;24(1):1–13.
Harvin JA, Maxim T, Inaba K, Martinez-Aguilar MA, King DR, Choudhry AJ, et al. Mortality after emergent trauma laparotomy: a multicenter, retrospective study. J Trauma Acute Care Surg. 2017;83(3):464–8.
Moore LJ, Fox EE, Meyer DE, Wade CE, Podbielski JM, Xu X, et al. Prospective observational evaluation of the ER-REBOA catheter at 6 U.S. Trauma Centers. Ann Surg. 2022;275(2):e520–6.
Biffl WL, Fox CJ, Moore EE. The role of REBOA in the control of exsanguinating torso hemorrhage. J Trauma Acute Care Surg. 2015;78(5):1054–8.
GUPTA BK, KHANEJA SC, EASTLICK FLORESL, LONGMORE L, SHAFTAN GW. The role of intra-aortic balloon occlusion in penetrating abdominal trauma. J Trauma Acute Care Surg. 1989;29(6):861–5.
Bulger EM, Perina DG, Qasim Z, Beldowicz B, Brenner M, Guyette F, et al. Clinical use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in civilian trauma systems in the USA, 2019: a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical technicians. Trauma Surg Acute Care Open. 2019;4(1):e000376.
Joseph B, Ibraheem K, Haider AA, Kulvatunyou N, Tang A, O’Keeffe T, et al. Identifying potential utility of resuscitative endovascular balloon occlusion of the aorta: an autopsy study. J Trauma Acute Care Surg. 2016;81(5):S128–32.
Uchino H, Tamura N, Echigoya R, Ikegami T, Fukuoka T. REBOA–is it really safe? A case with massive intracranial hemorrhage possibly due to endovascular balloon occlusion of the aorta (REBOA). Am J case Rep. 2016;17:810.
Bogert JN, Davis KM, Kopelman TR, Vail SJ, Pieri PG, Matthews MR. Resuscitative endovascular balloon occlusion of the aorta with a low profile, wire free device: a game changer? Trauma Case Rep. 2017;7:11–4.
Edwards J, Abdou H, Stonko DP, Treffalls RN, Elansary N, Lang E, Morrison JJ. Partial vs full resuscitative endovascular balloon occlusion of the aorta (REBOA) in a swine model of raised intracranial pressure and hemorrhagic shock. J Am Coll Surg. 2023;236(1):241–52.
Kuckelman J, Derickson M, Barron M, Phillips CJ, Moe D, Levine T, et al. Efficacy of intermittent versus standard resuscitative endovascular balloon occlusion of the aorta in a lethal solid organ injury model. J Trauma Acute Care Surg. 2019;87(1):9–17.
Russo RM, Franklin CJ, Davidson AJ, Carlisle PL, Iancu AM, Baer DG, Alam HB. A new, pressure-regulated balloon catheter for partial resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2020;89(2S Suppl 2):S45–9.
Laverty RB, Treffalls RN, McEntire SE, DuBose JJ, Morrison JJ, Scalea TM, et al. Life over limb: arterial access-related limb ischemic complications in 48-hour REBOA survivors. J Trauma Acute Care Surg. 2022;92(4):723–8.
Junior MAFR, Salman SM, Al-Qaraghuli SM, Makki F, Affan RAA, Mohseni SR, Brenner M. Complications associated with the use of resuscitative endovascular balloon occlusion of the aorta (REBOA): an updated review. Trauma Surg Acute Care Open. 2024;9(1):e001267.
Shum-Tim L, Bichara-Allard S, Hopkins B, AlShahwan N, Hanley S, Manzano-Nunez R, et al. Vascular access complications associated with resuscitative endovascular balloon occlusion of the aorta in adult trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2024;96(3):499–509.
Foley MP, Walsh SR, Doolan N, Vulliamy P, McMonagle M, Aylwin C, editors. ‘s Choice–Systematic Review and Meta-Analysis of Lower Extremity Vascular Complications after Arterial Access for Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA): An Inevitable Concern? European Journal of Vascular and Endovascular Surgery. 2023;66(1):103– 18.
Reva VA, Perevedentcev AV, Pochtarnik AA, Khupov MT, Kalinina AA, Samokhvalov IM, Khan MA. Ultrasound-guided versus blind vascular access followed by REBOA on board of a medical helicopter in a hemorrhagic ovine model. Injury. 2021;52(2):175–81.
Tatum D, Duchesne J, McGreevy D, Nilsson K, DuBose J, Rasmusse TE et al. To ultrasound or not to ultrasound: a REBOA femoral access analysis from the ABOTrauma and AORTA registries. J Endovascular Resusc Trauma Manage. 2020;4(2).
Grechenig P, Hallmann B, Eibinger NR, Koutp A, Zajic P, Höfler G, Puchwein P. Percutaneous ultrasound-guided versus open cut-down access to femoral vessels for the placement of a REBOA catheter. Sci Rep. 2024;14(1):9111.
Sugiyama T, Tomita K, Ishida K, Maruhashi T, Matsumura Y. Resuscitative endovascular balloon occlusion of the Aorta complications and its management. J Endovascular Resusc Trauma Manage. 2022;6(1).
Abid M, Neff LP, Russo RM, Hoareau G, Williams TK, Grayson JK, et al. Reperfusion repercussions: a review of the metabolic derangements following resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2020;89(2S):S39–44.
Paran M, McGreevy D, Hörer TM, Khan M, Dudkiewicz M, Kessel B, et al. International registry on aortic balloon occlusion in major trauma: partial inflation does not improve outcomes in abdominal trauma. Surgeon. 2024;22(1):37–42.
Theodorou CM, Salcedo ES, DuBose JJ, Galante JM. Hate to burst your balloon: successful REBOA use takes more than a course. J Endovascular Resusc Trauma Manage. 2020;4(1):21.
Chang R, Kerby JD, Kalkwarf KJ, Van Belle G, Fox EE, Cotton BA, et al. Earlier time to hemostasis is associated with decreased mortality and rate of complications: results from the pragmatic randomized optimal platelet and plasma ratio trial. J Trauma Acute Care Surg. 2019;87(2):342–9.
Chou C-H, Wu Y-T, Fu C-Y, Liao C-H, Wang S-Y, Bajani F, Hsieh C-H. Hemostasis as soon as possible? The role of the time to angioembolization in the management of pelvic fracture. World J Emerg Surg. 2019;14:1–8.
Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma Acute Care Surg. 2002;52(3):420–5.
Romagnoli A, Teeter W, Pasley J, Hu P, Hoehn M, Stein D, et al. Time to aortic occlusion: it’s all about access. J Trauma Acute Care Surg. 2017;83(6):1161–4.
Jansen JO, Hudson J, Cochran C, MacLennan G, Lendrum R, Sadek S, et al. Emergency Department resuscitative endovascular balloon occlusion of the Aorta in Trauma patients with exsanguinating hemorrhage: the UK-REBOA Randomized Clinical Trial. JAMA. 2023;330(19):1862–71.
Norii T, Crandall C, Terasaka Y. Survival of severe blunt trauma patients treated with resuscitative endovascular balloon occlusion of the aorta compared with propensity score-adjusted untreated patients. J Trauma Acute Care Surg. 2015;78(4):721–8.
Inoue J, Shiraishi A, Yoshiyuki A, Haruta K, Matsui H, Otomo Y. Resuscitative endovascular balloon occlusion of the aorta might be dangerous in patients with severe torso trauma: a propensity score analysis. J Trauma Acute Care Surg. 2016;80(4):559–66. discussion 66– 7.
Linderman GC, Lin W, Becher RD, Maung AA, Bhattacharya B, Davis KA, Schuster KM. Increased mortality with resuscitative endovascular balloon occlusion of the aorta only mitigated by strong unmeasured confounding: an expanded analysis using the National Trauma Data Bank. J Trauma Acute Care Surg. 2021;91(5):790–7.
Asmar S, Bible L, Chehab M, Tang A, Khurrum M, Douglas M, et al. Resuscitative endovascular balloon occlusion of the aorta vs pre-peritoneal packing in patients with pelvic fracture. J Am Coll Surg. 2021;232(1):17–26. e2.
Werner NL, Moore EE, Hoehn M, Lawless R, Coleman JR, Freedberg M, et al. Inflate and pack! Pelvic packing combined with REBOA deployment prevents hemorrhage related deaths in unstable pelvic fractures. Injury. 2022;53(10):3365–70.
Benjamin ER, Warriner Z, Demetriades D. Preperitoneal packing for pelvic fracture bleeding control: a human cadaver study. World J Surg. 2023;47(3):621–6.
Kim DH, Moon J, Chang SW, Kang BH. Early experience with resuscitative endovascular balloon occlusion of the aorta for unstable pelvic fractures in the Republic of Korea: a multi-institutional study. Eur J Trauma Emerg Surg. 2023;49(6):2495–503.
Chien CY, Lewis MR, Dilday J, Biswas S, Luo Y, Demetriades D. Worse outcomes with resuscitative endovascular balloon occlusion of the aorta in severe pelvic fracture: a matched cohort study. Am J Surg. 2023;225(2):414–9.
Chiu YC, Katsura M, Takahashi K, Matsushima K, Demetriades D. Resuscitative endovascular balloon occlusion of the aorta (REBOA) in the presence of associated severe traumatic brain injury: a propensity-score matched study. Am J Surg. 2024:115798.
Wu Y-T, Nichols C, Chien C-Y, Lewis MR, Demetriades D. REBOA in trauma and the risk of venous thromboembolic complications: a matched-cohort study. Am J Surg. 2023;225(6):1091–5.
Wu YT, Lewis MR, Arase M, Demetriades D. Resuscitative endovascular balloon occlusion of the aorta is associated with increased risk of extremity compartment syndrome. World J Surg. 2023;47(3):796–802.
Bhogadi SK, Colosimo C, Hosseinpour H, Nelson A, Rose MI, Calvillo AR, et al. The undisclosed disclosures: the dollar-outcome relationship in resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2023;95(5):726–30.
Funding
No funding was received for this manuscript.
Author information
Authors and Affiliations
Contributions
B.J. and D.D. searched the literature.B.J. and D.D. wrote the manuscript. B.J. and D.D. prepared and reviewed the manuscript.
Corresponding author
Ethics declarations
Financial interests
The authors have no financial or proprietary interest in the subject matter or materials discussed in the manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joseph, B., Demetriades, D. REBOA in trauma: a life-saving intervention or a spectacular failure?. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02657-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02657-x