Abstract
Background
Preperitoneal packing (PPP) has been widely accepted as a damage control technique for severe bleeding from pelvic fractures. It is supposed to work by direct compression and tamponade of the bleeding source in the pelvis and it has been suggested to be effective for both venous and arterial bleeding. However, there is little evidence to support its efficacy or the ability to place the laparotomy pads in proximity of the desired location.
Methods
Bilateral PPP was performed on 10 fresh human cadavers, followed by laparotomy and measurements of resultant pad placement in relation to critical anatomic structures.
Results
A total of 20 assessments of laparotomy pad placement were performed. Following completion of PPP, a midline laparotomy was performed to determine proximity and closest distance of the laparotomy pads to sites of potential bleeding in pelvic fractures. In almost all cases, the pad placement was not contiguous with the key anatomic structure with mean placement 3.9 + 1.1 cm from the sacroiliac joint, 3.5 + 1.6 cm from the common iliac artery, 1.1 + 1.2 cm from the external iliac artery, 2.8 + 0.8 cm from the internal iliac artery, and 2.3 + 1.2 cm from the iliac bifurcation. Surgeon experience resulted in improved placement relative to the sacroiliac joint, however the pads still did not directly contact the target point.
Conclusion
This human cadaver study has shown that PPP, even in experienced hands, may not be placed in significant proximity of anatomical structures of interest. The role of PPP needs to be revisited with better clinical or human cadaver studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preperitoneal packing (PPP) has been used as a damage control procedure for severe bleeding from pelvic fractures and is recommended in the clinical practice guidelines of many societies. However, there is little evidence to support the effectiveness of this technique. The purpose of this fresh human cadaver study was to evaluate the anatomical position of the gauze placed with the PPP technique in relation to potential bleeding sites after pelvic fracture.
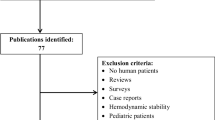
Materials and methods
Adult (>18 years old) human cadavers at the Los Angeles County-University of Southern California Fresh Tissue Dissection Laboratory were used for the purpose of the study. All cadavers were fresh, non-embalmed human bodies, maintained in compliance with hospital policy and California law. They were kept in refrigerated storage prior to being allowed to warm to room temperature for the procedure. There were no exclusion criteria, but evidence of prior low abdominal or pelvic surgery was captured at time of procedure if identified.
All procedures were performed by a board certified or board eligible general surgeon. All surgeons reviewed the technique of PPP before the procedure. The surgeon’s prior experience with the procedure, number of procedural attempts, and any identified technical errors were captured.
All cadavers were positioned supine on a standard operating room table. PPP was then performed as described in standard techniques [1]. A 6–8 cm midline incision was performed extending from below the umbilicus to the pubis. After dissection of the subcutaneous tissue, the fascia was exposed and incised, without entering the peritoneal cavity. The preperitoneal prevesical space was exposed and the bladder and peritoneum were swept medially, using blunt dissection. The dissection was continued posterior to the pubic symphysis and along the lateral pelvic side wall into the retroperitoneal spaces of the right and left hemipelvis and aiming to the sacrum. Three laparotomy pads were placed in each side of the pelvis. The first laparotomy pad was placed after medial retraction of the lateral wall of the bladder and the abdominal viscera, exerting firm pressure and aiming the packing inferiorly toward the sacrum. Two additional packs were then placed next to the first one, pushing firmly against the sacrum and the lateral pelvic ring. The second sponge was placed over the first sponge, at the middle of the pelvic brim and the third sponge was placed in the space deep and lateral to the bladder[1]. The procedure was then repeated on the other side of the pelvis. Following completion of PPP, a midline laparotomy was performed to determine proximity of the laparotomy pads to major pelvic vascular landmarks and the sacroiliac joint, via direct visualization. An upper midline laparotomy was initially performed, staying above the area of the preperitoneal dissection for the packing. If required, the laparotomy was extended inferiorly, and if this was required, the peritoneum was secured to the fascia in the midline with running suture to maintain pack position as dissection progressed. The exposure of the vessels started with an incision over the aortic bifurcation and proceeding laterally and inferiorly. Pack location was carefully evaluated prior to proceeding with dissection of the overlying peritoneum for identification of pack proximity to predetermined landmarks. Measurements were taken by a single individual for each cadaver, including closest distance of the packs to the sacroiliac joint, common, internal and external iliac artery, and the iliac artery bifurcation.
Statistical evaluation of complications and the surgeon’s prior experience were completed using chi-square and unpaired t-test analyses.
Results
In total, 10 cadavers with bilateral packing, totaling 20 assessments of PPP, were used for the study purpose. In five cadavers, there were prior abdominal operations, including low midline laparotomy (n = 3), appendectomy (n = 2) and suprapubic catheter placement (n = 1). During the PPP the peritoneum was inadvertently opened in 3 cadavers, 1 with prior abdominal surgery, and 2 without (Table 1). The violation of the peritoneum was identified during the exploratory laparotomy. In these cases the peritoneotomy did not affect the placement of the PPP. Interestingly, prior low abdominal surgery was not associated with an increased rate of accidental peritoneotomy (p = 0.49).
The distance of the closest pack to the target location was measured (Table 2). Using the closest point measurement, on average, the packs were placed 3.9 ± 1.1 cm from the sacroiliac joint, 3.5 ± 1.6 cm from the common iliac artery, 1.1 ± 1.2 cm from the external iliac artery, 2.8 ± 0.8 cm from the internal iliac artery, and 2.3 ± 1.2 cm from the iliac bifurcation. Direct pack contact was most likely to be achieved at the level of the external iliac artery, occurring in 45% of cases (n = 9). The iliac artery bifurcation was contacted in only 5% of cases (n = 1) and the sacroiliac joint in zero. The packs were within 2 cm of the sacroiliac joint in 5% of cases and within 3 cm in 40% (n = 8).
The value of operative surgeon’s prior experience was not realized in this study. Although experience improved placement in terms of proximity to the target point, the placement still did not reliably contact vessels or landmarks of interest. A total of four surgeons participated in the study, two with prior clinical experience in PPP, accounting for eight of the cadavers, and two without, accounting for two of the cadavers (Table 3). Surgeons with prior experience placed the laparotomy pads significantly closer to the sacroiliac joint than those that did not have experience (p = 0.001), although the pads were still not in direct contact with the target point. Proximity of placement neared significance relative to the external iliac artery with prior experience (p = 0.07); placement relative to the remaining landmarks was not significant based on experience (common iliac, p = 0.60; internal iliac, p = 0.25; bifurcation, p = 0.34).
Discussion
Pelvic packing was first reported for control of bleeding from pelvic fractures in 2000[2]. The technique involved extraperitoneal packing of the presacral and paravesical regions using between four and eight swabs, through a lower abdominal incision without entering the peritoneum. The procedure was refined and popularized in 2005 by Smith et al. [1] and since then, it has been adopted as an option for damage control in severe bleeding from pelvic fractures and has been promoted as an effective way of controlling bleeding from venous, arterial and bony bleeding. It is currently recommended in the clinical practice guidelines of many societies [3,4,5]. Some centers have even advocated that PPP can supplant the need for emergent angiography [6].
Overall, PPP is rarely performed in pelvic fractures, although many courses and workshops on the technical aspects of the procedure are taught nationally and internationally. Costantini et al. in an American Association for the Surgery of Trauma prospective, observational multi-institutional trial, reviewed the methods of hemorrhage control in pelvic fractures currently being used in clinical practice. A total of 1,339 patients with pelvic fracture were enrolled from 11 Level I trauma centers. PPP was used in 35 patients (2.6%) with pelvic fracture or in 13.3% of 178 patients admitted in shock[7].
The evidence supporting PPP is very weak, because it is very difficult to conduct well-designed randomized controlled studies. In the updated practice management guideline from the Eastern Association for the Surgery of Trauma, in 2020, there is a conditional recommendation for PPP in patients who remain hemodynamically unstable due to their pelvic fractures after the initial resuscitation, if angioembolization is not immediately available. In hemodynamically unstable patients due to their pelvic fractures and in a facility where resources to perform PPP and angioembolization are readily available, the guideline states that it cannot recommend for or against initial use of PPP versus pelvic angioembolization. The authors emphasized the very low quality of available evidence, which included only small observational studies. However, in their conclusions it is stated that, “PPP is an effective damage control technique that may be used as either the sole bleeding control intervention or in conjunction with either angioembolization or external fixation in patients who are hemodynamically unstable due to their pelvic fractures” [4].
Magnone et al. in a consensus conference, suggested that PPP is effective in controlling hemorrhage, when used as a salvage technique. However, this recommendation was based, as admitted by the authors, on Level IV evidence (case control studies or their metanalysis) and it was graded as level B, which was defined as “not always recommended but must be taken in consideration” [5]. Coccolini et al., in a World Society of Emergency Surgery guideline, stated that PPP is an effective surgical measure of early hemorrhage control in hypotensive patients with bleeding pelvic ring disruptions [Grade 1B: Strong recommendation, moderate-quality evidence] and that patients with pelvic fracture-related hemodynamic instability should always be considered for preperitoneal pelvic packing, especially in hospitals with no angiography service [Grade 1C: Strong recommendation, low-quality or very low-quality evidence but subject to change when higher quality evidence becomes available] [3].
The efficacy of PPP in controlling bleeding from pelvic fractures is not clear and the available evidence is very poor and based on small retrospective observational series, which does not support the often-enthusiastic conclusions in various studies or guidelines [6, 8,9,10,11]. Osborn et al. in a retrospective study matched 20 hemodynamically unstable patients treated with PPP and 20 patients treated with early angiography. Although the study showed no significant difference in mortality, complications, overall transfusion requirements, ventilator days, ICU days, or hospital days, the authors concluded that PPP t reduced pelvic arterial bleeding and that PPP is “as effective as pelvic angiography for stabilizing hemodynamically unstable patients with pelvic fractures, and may reduce early mortality due to exsanguination from pelvic hemorrhage” [9]. Attempting to directly compare outcomes of the various therapeutic interventions for bleeding control from pelvic fractures, is very difficult and may lead to the wrong conclusions, because of the bias and major heterogeneity of the reported study populations. In addition, the major changes in the resuscitation and blood transfusion protocols in the last few years make any outcome comparisons between older and more recent studies unreliable [12].
PPP is supposed to work by direct compression of the bleeding source in the pelvis and it has been suggested to be effective for both venous and arterial injuries. This human cadaver study showed that using the standard PPP technique, the packs were significantly away from potential sources of bleeding after severe pelvic fractures, such as the sacroiliac joint and common, external and internal iliac arteries. The distance of the packs from the iliac veins is even bigger, having in mind the anatomical location of the veins, medial and posterior to the arteries (Fig. 1). It has been suggested that in severe pelvic fractures, the most common source of bleeding is the venous plexus around the fracture site, accounting for about 85% of bleeding, which may be a good indication for PPP [13]. However, in a significant number of patients there is an associated major iliac vascular injury. In a study of 3,221 patients with severe pelvic fractures, 16.1% had an injury to the common or external iliac vessels, including a laceration in 10.7% of the patients. Patient age greater than or equal to 65 years was an independent predictor of major vascular injury, with an incidence of iliac vessel laceration of 13.6% [14]. It has been suggested that PPP produces tamponade, which controls bleeding. However, it is unlikely that packing which does not compress directly the bleeding site will produce an effective tamponade, especially for bleeding from a vascular laceration. In these cases, it is likely that the hematoma will expand in the retroperitoneum rather than the packed lateral or anterior pelvis. In addition, packing does not produce a significant tamponade effect for arterial bleeding, as shown by another human cadaver study. Sato et al., in a cadaver model investigated whether PPP generates pressure that exceeds the venous pressure and arterial pressure in the pelvis [15]. They placed pressure sensors in the posterior, middle and anterior pelvic rim and the pelvic floor, and the pressure at each point was measured after a standard PPP. The average pressure in the pelvic cavity after PPP was 12.3 ± 4.5 mm Hg. The pressure on the pelvic floor and pelvic posterior brim was significantly higher than the lateral or anterior pelvic brim. The authors hypothesized that a pressure of 12 mmHg would be adequate to tamponade venous bleeding. However, this pressure is highly unlikely to have any tamponade effect on arterial bleeding.
The effectiveness of PPP in controlling arterial bleeding after pelvic fractures was challenged by Sandhu et al., in a recent study designed to evaluate the efficacy of PPP in controlling arterial hemorrhage from pelvic trauma [16]. The study included 139 patients with pelvic fractures who underwent angiographic intervention, with or without prior PPP. On angiography, arterial extravasation was seen in 48.2% of the study patients. In the subgroup of 49 patients with PPP prior to angiogram, 57.1% continued to have arterial extravasation on subsequent angiography. Interestingly, there was no significant difference in the rate of arterial extravasation on angiography between patients who received PPP versus those who did not (28/49 [57.1%] vs. 39/90 [43.3%], p = 0.15). Similarly, among the patients who underwent PPP with documented arterial extravasation on preoperative CT angiogram, 73.3% continued to have arterial extravasation on subsequent angiography despite PPP. The study concluded that PPP is not an effective method for definitive control of arterial hemorrhage in pelvic fractures. In addition, the authors expressed concern that PPP may potentially delay the definitive treatment of angiographic intervention, which was highly effective in this series. McDonogh et al., in a systematic review and meta-analysis of 18 studies with a total of 579 patients, of which 402 were treated with PPP and 177 with angioembolization, reported that 27% of patients treated with PPP did not achieve bleeding control and required subsequent angioembolization [12].
Early identification and definitive management of arterial bleeding in pelvic fractures is a key factor in reducing preventable mortality. Tesoriero et al., in a retrospective study which covered the period 2002–2012, reported that the median time from arrival to embolization was greater than 5 h and 80% of all deaths could be attributed to early uncontrolled hemorrhage and associated with delays in hemostasis [17]. However, the new guidelines for trauma center verification by the ACS COT, require that “Level I and II trauma centers must have the necessary human and physical resources continuously available so that an endovascular or interventional radiology procedure for hemorrhage control can begin within 60 min of request (CD 4.15)” [18]. Recent studies report much shorter times to angioembolization. Sandhu reported a mean time of 51.3 min, from the decision of angiography to the procedure in patients who went straight to angiography without any other surgical intervention, which is comparable with reported times in obtaining PPP [16].
Another interesting finding in the present study was the relatively high incidence of violation of the peritoneum during PPP. This technical accidental breaching was not recognized at the time of packing and was not dependent on surgeon’s previous experience with the technique or the presence of a previous laparotomy incision. The breaching of the peritoneum may compromise the tamponade effect of PPP, because of the possible decompression of any bleeding from the fracture site into the peritoneal cavity.
Finally, PPP might not be without risk. In a study of 79 patients, that underwent PPP for complex pelvic fracture, after exclusion of early deaths, screening ultrasound identified a 23% incidence of DVT and 8% incidence of PE, although it is unclear how much is related to the fracture and how much to the packing [19].
The study has several limitations: The sex of the cadavers was not documented, which might be important because of anatomical differences between males and females. The study was performed on cadavers with an intact pelvis and no active bleeding. It is possible that in a disrupted pelvis, especially in the presence of an extraperitoneal hematoma, the packs could be in a different anatomical location than in an intact pelvic ring without a pelvic hematoma. The presence of a hematoma may reduce the risk of accidental breaching of the peritoneum, which occurred in 30% of cases in this study. Similarly, although the packs were away from the common source of bleeding, no conclusions can be made about the hemostatic effect of the packing in the presence of active bleeding or hematoma.
Conclusions
This human cadaver study has shown that PPP, even in experienced hands, may not be placed in significant proximity of anatomical structures of interest. The role of PPP for bleeding control from pelvic fracture needs to be revisited with better clinical or human cadaver studies.
References:
Smith WR, Moore EE, Osborn P et al (2005) Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: report of two representative cases and a description of technique. J Trauma 59(6):1510–1514
Tscherne H, Pohlemann T, Gansslen A, Hufner T, Pape HC (2000) Crush injuries of the pelvis. Eur J Surg 166(4):276–282
Coccolini F, Stahel PF, Montori G et al (2017) Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 12:5
Bugaev N, Rattan R, Goodman M et al (2020) Preperitoneal packing for pelvic fracture-associated hemorrhage: a systematic review, meta-analysis, and practice management guideline from the Eastern Association for the Surgery of Trauma. Am J Surg 220(4):873–888
Magnone S, Coccolini F, Manfredi R et al (2014) Management of hemodynamically unstable pelvic trauma: results of the first Italian consensus conference (cooperative guidelines of the Italian Society of Surgery, the Italian Association of Hospital Surgeons, the Multi-specialist Italian Society of Young Surgeons, the Italian Society of Emergency Surgery and Trauma, the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care, the Italian Society of Orthopaedics and Traumatology, the Italian Society of Emergency Medicine, the Italian Society of Medical Radiology -Section of Vascular and Interventional Radiology- and the World Society of Emergency Surgery). World J Emerg Surg 9(1):18
Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR (2007) Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: a paradigm shift. J Trauma 62(4):834–839
Costantini TW, Coimbra R, Holcomb JB et al (2016) Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg 80(5):717–723
Burlew CC, Moore EE, Stahel PF et al (2017) Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage due to unstable pelvic fractures. J Trauma Acute Care Surg 82(2):233–242
Osborn PM, Smith WR, Moore EE et al (2009) Direct retroperitoneal pelvic packing versus pelvic angiography: a comparison of two management protocols for haemodynamically unstable pelvic fractures. Injury 40(1):54–60
Jang JY, Shim H, Jung PY, Kim S, Bae KS (2016) Preperitoneal pelvic packing in patients with hemodynamic instability due to severe pelvic fracture: early experience in a Korean trauma center. Scand J Trauma Resusc Emerg Med 24:3
Ron G, Epstein D, Ben-Galim P, Klein Y, Kaban A, Sagiv S (2015) Extra-peritoneal pressure packing without external pelvic fixation: a life-saving stand-alone surgical treatment. J Emerg Trauma Shock 8(4):181–187
McDonogh JM, Lewis DP, Tarrant SM, Balogh ZJ (2022) Preperitoneal packing versus angioembolization for the initial management of hemodynamically unstable pelvic fracture: a systematic review and meta-analysis. J Trauma Acute Care Surg 92(5):931–939
Stahel PF, Mauffrey C, Smith WD, McKean J, Hao J, Burlew CC et al (2013) External fixation for acute pelvic ring injuries: decision making and technical options. J Trauma Acute Care Surg 75(5):882–887
Cho J, Benjamin E, Inaba K, Lam L, Demetriades D (2018) Severe bleeding in pelvic fractures: considerations in planning damage control. Am Surg 84(2):267–272
Sato Y, Sekine K, Shibusawa T et al (2017) Effect of retroperitoneal pelvic packing on pelvic cavity pressure: a cadaveric study. Orthopedics 40(6):e947–e951
Sandhu J, Abrahams R, Miller Z, Bhatia S, Zakrison TL, Mohan P (2020) Pelvic Trauma: factors predicting arterial hemorrhage and the role of Angiography and preperitoneal pelvic packing. Eur Radiol 30(11):6376–6383
Tesoriero RB, Bruns BR, Narayan M et al (2017) Angiographic embolization for hemorrhage following pelvic fracture: Is it “time” for a paradigm shift? J Trauma Acute Care Surg 82(1):18–26
Surgeons ACo. Resources for Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2022.
Heelan AA, Freedberg M, Moore EE et al (2020) Worth looking! venous thromboembolism in patients who undergo preperitoneal pelvic packing warrants screening duplex. Am J Surg 220(6):1395–1399
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benjamin, E.R., Warriner, Z. & Demetriades, D. Preperitoneal Packing for Pelvic Fracture Bleeding Control: A Human Cadaver Study. World J Surg 47, 621–626 (2023). https://doi.org/10.1007/s00268-022-06859-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06859-5