Abstract
Objective
The purpose of the present study was to evaluate the potential therapeutic effects of NZ on lipopolysaccharide (LPS)-induced RAW264.7 cells and explore its underlying mechanisms.
Methods
The effect of NZ on NO generation in LPS-activated macrophage was measured by Griess assay. The concentrations of TNF-α, IL-18, IL-1β were analyzed with ELISA kits. The LPS-induced production of reactive oxygen species (ROS) was determined by flow cytometry. The protein expressions of TLR4, NF-κB and NLRP3 signaling pathway were investigated with Western blot analysis.
Results
It was shown that NZ significantly reduced the production of NO and the generation of pro-inflammatory cytokines in LPS-induced RAW264.7 cells. In addition, NZ markedly inhibited the up-regulation of toll-like receptor 4 (TLR4), myeloid differentiation factor 88 (MyD88) and the activation of nuclear factor kappa B (NF-κB) in LPS-stimulated RAW 264.7 macrophages. Of note, NZ suppressed the expression of the inflammasome component such as NOD-like receptor 3(NLRP3), apoptosis-associated speck-like protein containing CARD(ASC), as well as the levels of cytokines including Interleukin-18(IL-18) and Interleukin-1β(IL-1β).
Conclusion
These results indicated that NZ inhibited the generations of NO and pro-inflammatory cytokines by suppressing TLR4/MyD88/NF-κB pathway, suggesting that NZ could be an effective candidate for ameliorating LPS-induced inflammatory responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammation, primarily featured by many pathological conditions including tissue injuries, is well recognized as a localized protective response and plays a significant role in scavenging pro-inflammatory substances. On the other hand, chronic inflammation associated with excessive pro-inflammatory mediators may disturb the normal function of the body and lead to lung injury [1], infarction [2], cardiovascular diseases [3], neurodegenerative disorders [4] or even death. Therefore, the duration and magnitude of inflammation must be controlled. However, few effective therapeutic drugs with assuasive side effects have been discovered to date, which suggests the significance for seeking more effective and non-cytotoxic anti-inflammatory agents.
Macrophage, known as one of the most dominant and widely distributed inflammatory cells, is involved in the initiation and maintenance of acute inflammatory response [5]. Lipopolysaccharide (LPS), the major component of the cell outer membrane of Gram-negative bacteria, is essentially important to pathogen-induced inflammation [6]. LPS is capable of triggering a cascade of inflammatory processes, among which the initiation of toll-like receptor 4 (TLR4) signaling pathway could further lead to more intricate biological responses including the secretion of a number of pro-inflammatory mediators.
When bound with LPS, the receptor TLR4 is initiated, which consequently promotes the downstream events. [7]. NF-κB drives a classical signal transduction pathway and gene regulation, which is implicated in various diseases including inflammatory disorders. Inactive NF-κB in the cytoplasm is normally governed by a family of inhibitory proteins (IκBs). The IκB kinase complex (IKK) is also involved in NF-κB pathway and is activated by various stimuli associated with tissue lesion. IKK contributes to the phosphorylation and degradation of IκB [8]. Subsequently, NF-κB is activated and initiates the transcription and expression of pro-inflammatory gene, then leads to excessive accumulation of various mediators such as tumor necrosis factor (TNF)-α, interleukin (IL)-1β and nitric oxide (NO). Particularly, NO, a crucial inflammatory mediator which is synthesized by inducible form of nitric oxide synthase (iNOS), is paradoxical in the pathogenesis of inflammation depending on its concentration [9]. Appropriate amount of NO is beneficial for regulating considerable physiological condition, whereas the sustained over-expression of NO is believed to be dangerous to human. Therefore, the regulation of the NO amount is a promising therapeutic strategy for many inflammatory diseases.
As is well known, pro-inflammatory cytokines are the most essential NF-κB target and play critical roles in numerous immune processes. Apart from TNF-α and IL-18, IL-1β acts as an indispensable pro-inflammatory cytokine as well. The production of IL-1β requires proteolytic cleavage changed from inactive precursor pro-IL-1β to an active form by caspase-1 promoting [10]. Moreover, the formation of inflammasome is the premise of the activation of caspase-1. NLRP3, a multiprotein complex composed of the Nod-like receptor (NLR) family of intracellular recognition molecules, the adapter protein apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) and pro-caspase-1, is one of the best studied inflammasomes [11]. Upon initiated by stimuli including LPS, NLRP3 proteins polymerize and combine with ASC adaptor, which in turn accelerates the recruitment and activation of pro-caspase-1 [12]. After that the inactive precursors of IL-18 and IL-1β are proteolytic cleaved by the promotion of caspase-1. With the release of pro-inflammatory cytokines, the numerous inflammatory process is exacerbate.
Triterpenoids, recognized as a family of natural products, have been widely applied for medicinal purposes in their natural forms or as templates for synthetic modification in many countries. Oleanolic acid (OA), as the well-known major triterpenoid acid, is widely distributed throughout the plant kingdom. OA possesses a wide variety of properties such as hepatoprotective, anti-viral, and anti-inflammatory effects [13]. On account of the comparatively low activity of triterpenoids in their natural forms, new derivatives have been synthesized to meet the clinical purposes. It is noteworthy that a typical synthetic oleanane-type triterpenoid, 2,3-dichloro-5,6-dicyano-1,4-benzoquinone (CDDO) has been served as an effective structural template for searching more potent anticancer and antioxidant agents over the past decade [14]. Our previous studies demonstrated that CDDO-Me significantly attenuated the mRNA expression of TNF-α, IL-1β and IL-6 in LPS-stimulated RAW264.7 cells, which are involved in blocking activation of NF-κB [15]. While only few CDDO derivatives have been designed and synthesized to enhance the anti-inflammatory activities. Taking CDDO as an effective structural template, we conducted a great deal of chemical modification and structural transformation. Thus, olean-28,13β-olide 2 (NZ) was designed and synthesized. Encouragingly, NZ is shown to overcome poor water solubility and enhance anti-inflammatory activity. However, its molecular mechanism of anti-inflammatory activity in RAW264.7 cells remains poorly understood. Thus, the present study was aimed to evaluate the anti-inflammatory activity of NZ in LPS-induced RAW264.7 cells and explore its potential mechanism.
Materials and methods
Reagents
NZ (Fig. 1a, purity more than 99 %, was synthesized by Pro. Yihua Zhang as previously described [16]) was dissolved in DMSO at a concentration of 200 mM and stored at 4 °C. The final concentration of DMSO was less than 0.1 % [v/v] in any of the experiments. LPS (E. coli: Serotype 055:B5) and NO kit (catalog no. S0021) were purchased from Beyotime Institute of Biotechnology (Nanjing, China). 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was supplied by Sigma Chemical Company (St. Louis, MO, U.S.). Mouse IL-18, IL-1β, and TNF-α enzyme-linked immunosorbent assay (ELISA) kits were purchased from Biolegend (San Diego, CA, USA). Dulbecco’s modified Eagle’s medium (DMEM) was purchased from Life Technologies (Carlsbad, CA, USA). Primary antibodies against iNOS, TLR-4, MyD88, IKKα, p-IKKα/β, p-IκB-α, IκB-α, p65, NLRP3, ASC, caspase-1, β-actin and horseradish peroxidase-conjugated anti-rabbit antibodies were obtained from Cell Signaling Technology (Beverly, MA, USA).
Cell culture
Murine macrophage cell line RAW264.7 was obtained from the American Type Culture Collection (ATCC, Rockville, MD). The cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10 % heat-inactivated fetal bovine serum (FBS, Hyclone, South America), 100 IU/ml penicillin and 100 μg/ml streptomycin (Amresco, USA) in a humidified incubator containing 5 % CO2 at 37 °C.
Cell viability assay
The RAW264.7 cells were plated at a density of 1.0 × 104 cells/well in 96-well plates and incubated in humidified environment at 37 °C for 24 h. The cells were treated with different concentrations of NZ for another 20 h. Cell viability was assessed using methylthiazoletetrazolium (MTT) assay. Briefly, 20 μl of MTT (5 mg/ml) working solution was added to each well and incubated at 37 °C for 4 h. Then, the culture medium was removed and dimethyl sulfoxide (DMSO) of 150 μl was added to dissolve the formazan crystals. The absorbance values were measured at 490 nm using a microplate spectrophotometer (Tecan, Switzerland). The optical density of formazan crystals in the control group was taken as 100 % of viability. The assay was performed in triplicate at each concentration.
Determination of nitric oxide (NO) production
1 × 104 cells/well RAW264.7 cells were seeded on 96-well plates and incubated overnight, followed by the treatment with various concentrations of NZ for 2 h before LPS stimulation. Cells were treated with LPS (1 μg/ml) for an additional 24 h. Nitric oxide in culture medium was measured directly using a commercially available kit (Beyotime, China) based on the Griess reaction. Culture supernatants (50 μl) were mixed with 100 μl Griess reagent for 3 min at room temperature. The absorbance values were measured at 540 nm on a microplate spectrophotometer.
Enzyme-linked immunosorbent assay (ELISA)
After incubated with various concentrations of NZ for 2 h, the RAW 264.7 cells (1 × 105 cells/well in 6-well plates) were subsequently treated with or without LPS (1 μg/ml) for 6 h. We collected the cell culture supernatants for further cytokine analysis. The contents of tumor necrosis factor (TNF)-α, interleukin (IL)-1β and IL-18 were evaluated with their respective commercially available enzyme-linked immunosorbent assay (ELISA) kits according to the manufacturer’s instructions. Then the absorbance of each well was read at 450 nm with a microplate spectrophotometer. Finally, the contents were calculated according to the standard curves.
Detection of intracellular ROS
The production of intracellular ROS was assessed in RAW264.7 cells using the oxidation-sensitive fluorescent dye carboxy-DCFH-DA. To summarize, the RAW264.7 cells were cultured at 1 × 105 cells/well in 6-well plates. Cells were pre-treated with various concentrations of NZ (2 nM, 4 nM, 8 nM) in the presence or absence of LPS (1 μg/ml) and incubated for 4 h. Then they were washed twice with 1× washing buffer and loaded with 10 mM 2,7-dichlorofluorescein diacetate (DCFH-DA) detection reagent. After incubated in darkness for a further 20 min at 37 °C, cells were washed twice with 1× washing buffer. Finally, DCF fluorescence distributions were analyzed by the flow cytometry with excitation wavelength and emission wavelength of 488 and 525 nm, respectively.
Western blotting
The RAW264.7 cells pre-treated with NZ (2, 4 nM, 8 nM) with or without LPS were collected, washed twice by cold PBS and lysed in a RIPA buffer (Beyotime, China). The total protein concentration was measured using a BCA protein assay kit (Beyotime, China). 60 μg cellular proteins were mixed with five times loading dye (Laemmli Buffer) and 2-mercapto ethanol, then were heated at 95 °C for 5 min. The protein samples were resolved and separated by 8–12 % sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). After that the blots were transferred to polyvinylidene difluoride membranes (Millipore, MA, USA), which subsequently were blocked with 5 % (w/v) non-fat milk in TBST buffer for 1 h at room temperature. Then the membranes were treated with corresponding primary antibodies overnight at 4 °C. The membranes were washed three times with 1× TBST, followed by incubated with appropriate horseradish peroxidase-conjugated secondary antibodies (1:5000; Bioworld, MN, U.S.) for 2 h. Finally, protein bands were visualized with an enhanced chemiluminescence (ECL) system (KeyGEN Biotechnology, Nanjing, China) and scanned with a Chemiluminescence imaging system (Gel Catcher 2850, China). The relative optical densities of protein bands were analyzed with a ChemiScope analysis program.
Statistical analysis
The results in this study were analyzed using one-way ANOVA with Tukey multiple comparison test. They were presented as the mean ± standard deviation (S.D.). A p value of less than 0.05 was considered to be statistically significant (p < 0.05).
Results
Effects of NZ on cell viability
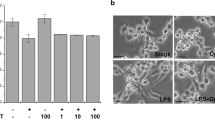
To investigate whether NZ has any cytotoxic in RAW264.7 macrophages, we first examined its effects on cell viability using MTT assay. The RAW264.7 cells incubated with various concentrations of NZ were harvested after 24 h incubation. As shown in Fig. 1b, NZ did not display any cellular toxicity with NZ at 2, 4, 8 nM. These results proved that the inhibitory effect caused by NZ treatment was not due to its cytotoxicity. For the above reason, all subsequent experiments were conducted at different concentrations (2, 4 and 8 nM) of NZ.
Effects of NZ on LPS-induced NO production in RAW264.7 cells
The production of nitric oxide (NO) after LPS challenge was an important reflection of the inflammatory process. To assess whether NZ inhibited LPS-induced inflammation, the production of NO was determined in RAW264.7 macrophages. As shown in Fig. 2a, in LPS-stimulated RAW264.7 cells, NO production markedly up-regulated, which was dramatically suppressed with the pre-treatment with NZ in a concentration-dependent manner. Since the overproduction of NO is mainly on account of high expression of iNOS, we also analyzed the ability of NZ to regulate the LPS-induced iNOS expression. As shown in Fig. 2b, iNOS expression was significantly attenuated by the pre-treatment with NZ (2, 4 and 8 nM) in LPS-induced RAW264.7 cells. Together, these results indicated that NZ exerted inhibitory effect by reducing the production of NO and the expression of iNOS.
Effects of NZ on NO production and iNOS protein expression in LPS-stimulated RAW264.7 cells. RAW264.7 cells were seeded on 96-well plates with 1 × 104 cells/ml for 24 h. Then they were incubated with different concentrations of NZ (2, 4, 8 nM) for 2 h, and subsequently treated with or without LPS (1 μg/ml) for another 24 h. The nitrite in the culture supernatants was collected and assessed by Griess reaction. The absorbance was measured at 540 nm. β-Actin was used as an internal controls for Western blot analysis. a Effect of NZ on the suppression of NO production in LPS-induced RAW264.7 cells. b Effect of NZ on LPS-induced iNOS protein in RAW264.7 cells. All data were expressed as mean ± SD of three separate experiments, ### p < 0.001 compared with control group, *** p < 0.001, ** p < 0.01 compared with LPS group
Effects of NZ on LPS-induced pro-inflammatory cytokines in RAW264.7 cells
Cytokines are important mediators in regulating host responses to inflammation. To further evaluate the anti-inflammatory effect of NZ on LPS-stimulated pro-inflammatory cytokines, we investigated the productions of TNF-α (Fig. 3a), IL-1β (Fig. 3b) and IL-18 (Fig. 3c) by treating RAW264.7 cells with LPS. As expected, in normal cells, the productions of several pro-inflammatory cytokines were almost unobserved. The levels of pro-inflammatory cytokines increased significantly in LPS treatment alone. Whereas these conditions were markedly attenuated by pre-treatment with NZ (2, 4 and 8 nM). These results showed that NZ inhibited the synthesis and release of pro-inflammatory cytokines TNF-α, IL-1β and IL-18 in concentration-dependent manners in LPS-stimulated RAW264.7 cells.
Effects of NZ on the expressions of TNF-α, IL-1β and IL-18 in LPS-induced RAW264.7 cells. The RAW264.7 cells were treated with various concentrations of NZ for 2 h and subsequently stimulated with LPS (1 μg/ml) for another 6 h. Then the culture supernatant was collected and assessed for cytokines TNF-α, IL-1β and IL-18 by ELISA kit. NZ also inhibited LPS-induced TNF-α (a), IL-1β (b) and IL-18 (c) secretions in RAW264.7 cells. All data were expressed as mean ± SD of three separate experiments, ### p < 0.001 compared with control group, *** p < 0.001, ** p < 0.01, * p < 0.05 compared with LPS group
Effects of NZ on ROS production
The TLR4-dependent production of ROS was required for the activation of NLRP3 inflammasome, and ROS could be significantly increased by LPS. To detect the involvement of ROS during LPS-induced inflammation in RAW264.7 cells, the production of ROS was measured using DCFH-DA probe. RAW264.7 cells were pre-treated with different concentrations of NZ with or without LPS. DCF fluorescence was monitored by flow cytometry. As shown in Fig. 4, treatment with NZ significantly inhibited ROS production compared with that of treatment with LPS alone. Based on these results, we could draw a conclusion that NZ might reduce the secretions of IL-18 and IL-1β via suppressing ROS production.
NZ suppressed ROS generation in RAW264.7 cells. The cells were treated with various concentrations of NZ (2, 4, 8 nM) in the presence or absence of LPS (1 μg/ml). Then they were incubated for 4 h and added 100 μL DCFH-DA, prior to a further 30-min incubation at 37 °C. ROS production was measured using flow cytometry. All data were presented as mean ± SD of three experiments performed in duplicate. ### p < 0.001 compared with control group, *** p < 0.001 compared with LPS group
Effects of NZ on activation of TLR4 and MyD88 in RAW264.7 cells
To assess the effect of NZ on the LPS-activated TLR4 signaling pathway, we used Western blot analysis to examine whether NZ influences TLR4 protein expression. The results showed that TLR4 protein expression was significantly up-regulated in the LPS-treated group compared with that in the normal group (Fig. 5b). However, NZ could markedly decrease the protein levels of TLR4. In addition, MyD88 was an adaptor protein for TLR4, so we further checked the protein level of MyD88. Our data demonstrated that NZ could suppress LPS-induced activation of MyD88 in RAW264.7 cells (Fig. 5c). Therefore, it was indicated that LPS-induced activation of TLR4 signaling pathway was probably restrained by NZ.
The inhibitions of NZ on TLR4 and MyD88 expressions. Cells were incubated with NZ (2, 4, 8 nM) for 2 h and then treated with 1 μg/ml LPS. The protein samples were analyzed using Western blot analysis. β-Actin was used as a control. Three independent experiments were performed and the results are presented as the mean ± SD. ### p < 0.001 compared with control group, *** p < 0.001, ** p < 0.01, * p < 0.05 compared with LPS group
Effects of NZ on NF-κB (p65) activation and translocation in RAW264.7 cells
NF-κB pathway is a crucial regulator in mediating the expression of iNOS genes and pro-inflammatory cytokines in activated RAW264.7 cells. To better demonstrate the mechanisms, we sought to measure whether the NF-κB signaling activation was also related to the inhibitory effects of NZ. The activation degree of NF-κB was assessed by Western blotting. Our data revealed that LPS-induced increase in protein levels of the phosphorylation of IκB-α (Fig. 6c) and IKKα/β (Fig. 6b) was dramatically blocked by co-treated with LPS and NZ. Furthermore, the protein level of cytosolic NF-κB p65 subunit was significantly alleviated (Fig. 6d), while the nuclear phosphorylation of p65 was attenuated by co-treatment with NZ (Fig. 6e). Taken together, these results suggested that NZ might be involved in NF-κB pathway-mediated inflammatory process in LPS-induced RAW264.7 cells.
NZ decreased the activation of NF-κB signaling in RAW264.7 cells. Cytosolic total and phosphorylation of IκB-α, IKKα/β and NF-κB p65 expressions were determined by representative Western blotting in RAW264.7 macrophages. β-Actin was used as internal control. Relative protein levels were quantified by densitometry, c the degradation and phosphorylation of IκB-α, b the phosphorylation of IKKα/β, d, e the activation of NF-κB p65. Each value represents the mean ± SD of three experiments performed in triplicates. ### p < 0.001 compared with control group, *** p < 0.001, ** p < 0.01, * p < 0.05 compared with LPS group
Effects of NZ on the activation of the NLRP3 inflammation and caspase-1 in RAW264.7 cells
In our study, it was showed that NZ could reduce IL-18 and IL-1β productions in LPS-induced RAW264.7 cells in Fig. 3b, c. Moreover, recent literature has revealed that IL-18 and IL-1β are inactive cytoplasmic precursors (pro-IL-1β and pro-IL-18) before turning to the active forms, which are cleaved by caspase-1. The activation of caspase-1 was mediated by NLRP3 inflammasome. Consequently, to elucidate whether its anti-inflammatory effect was related with NLRP3 inflammasome, we further explored the level of NLRP3 inflammasome in RAW264.7 cells (Fig. 7). Western blot analysis showed that co-treated with NZ and LPS dramatically blocked the LPS-induced up-regulations of NLRP3, ASC and pro-caspase-1 compared with treatment with LPS alone. These results indicated that NZ might reduce the promotion of NLRP3 inflammasome to inhibit inflammation.
NZ inhibited NLRP3 inflammasome activation in RAW264.7 cells. Protein levels of NLRP3, ASC, caspase-1 were determined by Western blotting and analyzed by densitometry. The representative data are shown. Data were presented as mean ± SD of three experiments performed in duplicate. ### p < 0.001 compared with control group, *** p < 0.001, ** p < 0.01, * p < 0.05 compared with LPS group
Discussion
In the present study, the inhibitory effects of NZ on inflammatory pathogenesis and molecular mechanism were evaluated in LPS-stimulated RAW264.7 cells. The data showed that NZ prevented inflammation via a underlying mechanism involved in the activation of NF-κB and NLRP3 inflammasome in LPS-induced RAW264.7 cells.
Inflammation is a complex localized physiological response accounting for high morbidity and mortality in various diseases such as cancer, rheumatoid, atherosclerosis and lung injury [17]. LPS, a pivotal inducer in inflammatory process, promotes the inflammatory pathogenesis via triggering the acute massive accumulation of neutrophils and the release of inflammatory mediators such as TNF-α, IL-1β, IL-18 [18].
NZ, a new derivative synthesized from ODDO, has attracted extensive attention due to its anticancer properties and anti-inflammatory. Our study was conducted to explore the underlying molecular effects of NZ on pro-inflammatory cytokines generation and inflammasome activation in RAW264.7 macrophages. RAW264.7 cells treated with lipopolysaccharide are considered as a canonical model on inflammation research. Our experimental data revealed that NZ took non-cytotoxic effects on macrophages when given alone with the experimental concentrations, or when given in combination with 1 μg/ml LPS.
As one of the most important pattern recognition, TLR4 acts as an integral role in innate immune system. Treatments aimed at modulating TLR4 signaling might have potential therapeutic advantages for inflammatory diseases [19]. Upon LPS stimulation, macrophages could be typically activated via TLR4 receptors and subsequently secreted excessive inflammatory cytokines including TNF-α, IL-1β and IL-18 [19]. The elevated levels of inflammatory cytokines are observed in the early stage of a variety of inflammatory diseases. TNF-α is acknowledged as the earliest and primary cytokine of inflammation reaction, which stimulates the production of other cytokines and promotes the process of immune response [20]. IL-18 functions as an important role in the regulation of immune network and inflammatory cascade [21]. IL-1β, a “administrator” that arranges the following immune responses at both the local and systemic levels, stimulates macrophages to secret other inflammatory cytokines [22]. To explore the potential anti-inflammatory effects of NZ, the LPS-induced generations of these cytokines with the treatment of NZ were examined. Our results demonstrated that NZ was an effective anti-inflammatory compound down-regulated the LPS-stimulated productions of TNF-α, IL-1β, IL-18. Therefore, we supposed that the inhibitory effect of NZ on inflammation might be related to TLR4 signaling pathway.
NO is acknowledged as an intracellular messenger during the pathogenesis of inflammation. It was previously reported that the expression of iNOS could be up-regulated in LPS-induced RAW264.7 cells, which subsequently caused NO generation in large amounts and physiological dysfunction [23]. In the present study, we analyzed the efficacy of NZ against LPS-induced NO release in RAW264.7 macrophages. As expected, NZ was found to efficaciously elevate NO generation and iNOS expression in LPS-induced RAW264.7 cells.
It has been illustrated that the activation of NF-κB is implicated in the signaling pathways which involved in the generation of pro-inflammatory cytokines when LPS is recognized by TLR4 receptors. Thus, NF-κB has been investigated as a key target for the treatment of inflammation [24]. NF-κB functions as a major transcription factor, interacting with promoter of the cytokines genes in LPS-stimulated macrophages [25]. To elucidate the precise mechanism involved in LPS-induced inflammation in RAW264.7 cells, the effects of NZ on NF-κB activation were examined. LPS stimulation leads to the activation of TLR4-MyD88 and subsequent the activation of NF-κB via the phosphorylation and degradation of IκBα [26]. IκBα, known as inhibitors of NF-κB, is regulated by IκB kinases (IKKs). Once activated, NF-κB subunit p65 separates from IκBα and translocates from cytoplasm to nucleus, which triggers the transcription of the target genes such as TNF-α, IL-1β and IL-6 [27]. As shown in our present study, NZ pre-treatment significantly inhibited the phosphorylation of IKKα/β, IκBα and p65 NF-κB activation in LPS-induced RAW264.7 macrophages. These results indicated that NZ inhibited the levels of NO and pro-inflammatory cytokines by suppressing TLR4/MyD88/NF-κB pathway.
Recent studies have found that NLRs is another vital factor except TLR-NF-κB signaling. NLRP3 inflammasome, one of NLRs extensively studied in recent, is consisted by three sections including NLRP3, ASC and caspase-1. Previous evidence indicated that NLRP3 governed the productions of pro-inflammatory cytokines [28]. Recent studies have suggested that the NLRP3 region is implicated in the pathogenesis of more common inflammatory diseases [29]. The activation of caspase-1 is required to convert pro-IL-1β to its mature active form IL-1β, which depends on activated NLRP3 inflammasome. Upon activation, NLRP3 proteins combine to ASC adaptor and subsequently induce the translocation and activation of pro-caspase-1 [30]. Moreover, caspase-1 is responsible for triggering pro-inflammatory cytokines and allowing for the secretions of mature forms [31]. We observed that pre-treated with NZ effectively decreased the levels of IL-1β and IL-18 in RAW264.7 macrophages, which was due to the down-regulation of NLRP3 protein expression and the inhibition of ASC adaptor as well as caspase-1 activity.
Oxidative stress caused by ROS is one of the causative factors of various inflammatory diseases [32]. ROS is also known to be a proposed common NLRP3 inflammasome activator, which leads to the generation and modification of ligand for NLRP3 or the assembly of NLRP3 proteins [33, 34]. Of note, we found that pro-incubated NZ reduced ROS production in LPS-stimulated macrophages. The result suggested that NZ could ameliorate oxidative stress to inhibit NLRP3 inflammasome. Simplified overview of the above signaling pathways was as illustrated in Fig. 8.
In conclusion, we explored the effect of NZ on the inhibition of inflammation in RAW264.7 macrophage. Our results showed that NZ reduced the generations of inflammatory cytokines. Suppressions of IL-18 and IL-1β secretions by NZ are related to the production of ROS. Furthermore, it could at least partially suppress TLR-NF-κB signaling, NLRP3 expression and caspase-1 activation. These results indicated that NZ exerted its anti-inflammatory effect via the inhibitions of NF-κB signaling and NLRP3 inflammasome, suggesting that NZ might be a promising agent for the therapy of inflammatory-associated diseases.
References
Su ZQ, Mo ZZ, Liao JB, Feng XX, Liang YZ, Zhang X, et al. Usnic acid protects LPS-induced acute lung injury in mice through attenuating inflammatory responses and oxidative stress. Int Immunopharmacol. 2014;22:371–8.
De Jesus NM, Wang L, Herren AW, Wang J, Shenasa F, Bers DM, et al. Atherosclerosis exacerbates arrhythmia following myocardial infarction: role of myocardial inflammation. Heart Rhythm Off J Heart Rhythm Soc. 2015;12:169–78.
Reddy SA, Shelar SB, Dang TM, Lee BN, Yang H, Ong SM, et al. Sulforaphane and its methylcarbonyl analogs inhibit the LPS-stimulated inflammatory response in human monocytes through modulating cytokine production, suppressing chemotactic migration and phagocytosis in a NF-kappaB- and MAPK-dependent manner. Int Immunopharmacol. 2015;24:440–50.
Kim EA, Han AR, Choi J, Ahn JY, Choi SY, Cho SW. Anti-inflammatory mechanisms of N-adamantyl-4-methylthiazol-2-amine in lipopolysaccharide-stimulated BV-2 microglial cells. Int Immunopharmacol. 2014;22:73–83.
Li Y, Wu Q, Deng Y, Lv H, Qiu J, Chi G, et al. D(-)-Salicin inhibits the LPS-induced inflammation in RAW264.7 cells and mouse models. Int Immunopharmacol. 2015;26:286–94.
Piazza M, Calabrese V, Baruffa C, Gioannini T, Weiss J, Peri F. The cationic amphiphile 3,4-bis(tetradecyloxy)benzylamine inhibits LPS signaling by competing with endotoxin for CD14 binding. Biochem Pharmacol. 2010;80:2050–6.
Byun EB, Sung NY, Park JN, Yang MS, Park SH, Byun EH. Gamma-irradiated resveratrol negatively regulates LPS-induced MAPK and NF-kappaB signaling through TLR4 in macrophages. Int Immunopharmacol. 2015;25:249–59.
Ahmad SF, Ansari MA, Zoheir KM, Bakheet SA, Korashy HM, Nadeem A, et al. Regulation of TNF-alpha and NF-kappaB activation through the JAK/STAT signaling pathway downstream of histamine 4 receptor in a rat model of LPS-induced joint inflammation. Immunobiology. 2015;220:889–98.
Ma J, Shi H, Mi C, Li HL, Lee JJ, Jin X. Malloapelta B suppresses LPS-induced NF-kappaB activation and NF-kappaB-regulated target gene products. Int Immunopharmacol. 2015;24:147–52.
Beninson LA, Fleshner M. Exosomes in fetal bovine serum dampen primary macrophage IL-1beta response to lipopolysaccharide (LPS) challenge. Immunol Lett. 2015;163:187–92.
Abderrazak A, Syrovets T, Couchie D, El Hadri K, Friguet B, Simmet T, et al. NLRP3 inflammasome: from a danger signal sensor to a regulatory node of oxidative stress and inflammatory diseases. Redox Biol. 2015;4:296–307.
Karasawa T, Kawashima A, Usui F, Kimura H, Shirasuna K, Inoue Y, et al. Oligomerized CARD16 promotes caspase-1 assembly and IL-1beta processing. FEBS Open Biol. 2015;5:348–56.
Huang Z, Fu J, Liu L, Sun Y, Lai Y, Ji H, et al. Glycosylated diazeniumdiolate-based oleanolic acid derivatives: synthesis, in vitro and in vivo biological evaluation as anti-human hepatocellular carcinoma agents. Org Biomol Chem. 2012;10:3882–91.
To C, Ringelberg CS, Royce DB, Williams CR, Risingsong R, Sporn MB, et al. Dimethyl fumarate and the oleanane triterpenoids, CDDO-imidazolide and CDDO-methyl ester, both activate the Nrf2 pathway but have opposite effects in the A/J model of lung carcinogenesis. Carcinogenesis. 2015;36:769–81.
Chen T, Mou Y, Tan J, Wei L, Qiao Y, Wei T, et al. The protective effect of CDDO-Me on lipopolysaccharide-induced acute lung injury in mice. Int Immunopharmacol. 2015;25:55–64.
Ding Y, Huang Z, Yin J, Lai Y, Zhang S, Zhang Z, et al. DDQ-promoted dehydrogenation from natural rigid polycyclic acids or flexible alkyl acids to generate lactones by a radical ion mechanism. Chem Commun. 2011;47:9495–7.
Chen T, Xiao L, Zhu L, Ma S, Yan T, Ji H. Anti-asthmatic effects of ginsenoside Rb1 in a mouse model of allergic asthma through relegating Th1/Th2. Inflammation. 2015. doi:10.1007/s10753-015-0159-4.
Tianzhu Z, Shihai Y, Juan D. The effects of morin on lipopolysaccharide-induced acute lung injury by suppressing the lung NLRP3 inflammasome. Inflammation. 2014;37:1976–83.
Wang Y, Cui Y, Cao F, Qin Y, Li W, Zhang J. Ganglioside GD1a suppresses LPS-induced pro-inflammatory cytokines in RAW264.7 macrophages by reducing MAPKs and NF-kappaB signaling pathways through TLR4. Int Immunopharmacol. 2015;28:136–45.
Tian Y, Zhang Y, Zhang R, Qiao S, Fan J. Resolvin D2 recovers neural injury by suppressing inflammatory mediators expression in lipopolysaccharide-induced Parkinson’s disease rat model. Biochem Biophys Res Commun. 2015;460:799–805.
Jing W, Chunhua M, Shumin W. Effects of acteoside on lipopolysaccharide-induced inflammation in acute lung injury via regulation of NF-kappaB pathway in vivo and in vitro. Toxicol Appl Pharmacol. 2015;285:128–35.
Wu XF, Ouyang ZJ, Feng LL, Chen G, Guo WJ, Shen Y, et al. Suppression of NF-kappaB signaling and NLRP3 inflammasome activation in macrophages is responsible for the amelioration of experimental murine colitis by the natural compound fraxinellone. Toxicol Appl Pharmacol. 2014;281:146–56.
Jo YH, Park HC, Choi S, Kim S, Bao C, Kim HW, et al. Metabolomic Analysis Reveals Cyanidins in Black Raspberry as Candidates for Suppression of Lipopolysaccharide-Induced Inflammation in Murine Macrophages. J Agric Food Chem. 2015;63:5449–58.
Wu XL, Liou CJ, Li ZY, Lai XY, Fang LW, Huang WC. Sesamol suppresses the inflammatory response by inhibiting NF-kappaB/MAPK activation and upregulating AMP kinase signaling in RAW264.7 macrophages. Inflamm Res. 2015;64:577–88.
Cui L, Feng L, Zhang ZH, Jia XB. The anti-inflammation effect of baicalin on experimental colitis through inhibiting TLR4/NF-kappaB pathway activation. Int Immunopharmacol. 2014;23:294–303.
Pan H, Xu LH, Ouyang DY, Wang Y, Zha QB, Hou XF, et al. The second-generation mTOR kinase inhibitor INK128 exhibits anti-inflammatory activity in lipopolysaccharide-activated RAW264.7 cells. Inflammation. 2014;37:756–65.
Ni W, Zhang Q, Liu G, Wang F, Yuan H, Guo Y, et al. Escherichia coli maltose-binding protein activates mouse peritoneal macrophages and induces M1 polarization via TLR2/4 in vivo and in vitro. Int Immunopharmacol. 2014;21:171–80.
Jang SE, Jeong JJ, Hyam SR, Han MJ, Kim DH. Ursolic acid isolated from the seed of Cornus officinalis ameliorates colitis in mice by inhibiting the binding of lipopolysaccharide to Toll-like receptor 4 on macrophages. J Agric Food Chem. 2014;62:9711–21.
Luo YP, Jiang L, Kang K, Fei DS, Meng XL, Nan CC, et al. Hemin inhibits NLRP3 inflammasome activation in sepsis-induced acute lung injury, involving heme oxygenase-1. Int Immunopharmacol. 2014;20:24–32.
Chao LK, Lin CH, Chiu HW, Wong WT, Chiu HW, Tasi YL, et al. peroxyauraptenol inhibits inflammation and nlrp3 inflammasome activation by inhibiting reactive oxygen species generation and preserving mitochondrial integrity. J Agric and Food Chem 2015.
Li X, Zhong F. Nickel induces interleukin-1beta secretion via the NLRP3-ASC-caspase-1 pathway. Inflammation. 2014;37:457–66.
Wang S, Zhao J, Wang H, Liang Y, Yang N, Huang Y. Blockage of P2X7 attenuates acute lung injury in mice by inhibiting NLRP3 inflammasome. Int Immunopharmacol. 2015;27:38–45.
Park J, Min JS, Kim B, Chae UB, Yun JW, Choi MS, et al. Mitochondrial ROS govern the LPS-induced pro-inflammatory response in microglia cells by regulating MAPK and NF-kappaB pathways. Neurosci Lett. 2015;584:191–6.
Li Y, Li J, Li S, Li Y, Wang X, Liu B, et al. Curcumin attenuates glutamate neurotoxicity in the hippocampus by suppression of ER stress-associated TXNIP/NLRP3 inflammasome activation in a manner dependent on AMPK. Toxicol Appl Pharmacol. 2015;286:53–63.
Acknowledgments
This work was supported by the National College Students Innovation Project for the R&D of Novel Drugs (J1030830) and by the Specialized Research Fund for the Doctoral Program of Higher Education (20130096110005).
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: John Di Battista.
Rights and permissions
About this article
Cite this article
Xiang, P., Chen, T., Mou, Y. et al. NZ suppresses TLR4/NF-κB signalings and NLRP3 inflammasome activation in LPS-induced RAW264.7 macrophages. Inflamm. Res. 64, 799–808 (2015). https://doi.org/10.1007/s00011-015-0863-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-015-0863-4