Abstract
This review aims to comprehensively explore calcium-enriched mixture (CEM) cement as a crucial biomaterial in dentistry/endodontics. With its growing clinical relevance, there is a need to evaluate its composition, chemical/physical/biological properties, clinical applications, and future perspectives to provide clinicians/researchers with a detailed understanding of its potential in endodontic procedures. Through systematic analysis of available evidence, we assess the advantages/limitations of CEM cement, offering valuable insights for informed decision-making in dental/endodontic practice. Our findings highlight the commendable chemical/physical properties of CEM cement, including handling characteristics, alkalinity, color stability, bioactivity, biocompatibility, sealing ability, and antimicrobial properties. Importantly, CEM cement has shown the potential in promoting regenerative processes, such as dentinogenesis and cementogenesis. It has demonstrated successful outcomes in various clinical applications, including vital pulp therapy techniques, endodontic surgery, open apices management, root resorption/perforation repair, and as an orifice/root canal obturation material. The efficacy and reliability of CEM cement in diverse clinical scenarios underscore its effectiveness in endodontic practice. However, we emphasize the need for well-designed clinical trials with long-term follow-up to further substantiate the full potential of CEM cement. This review serves as a robust reference for researchers/practitioners, offering an in-depth exploration of CEM cement and its multifaceted roles in contemporary dentistry/endodontics.
Similar content being viewed by others
Background
The success of endodontic therapy relies on various factors, including effective root canal instrumentation and obturation techniques. Throughout the years, numerous materials and techniques have been developed to optimize treatment outcomes in endodontics. One promising endodontic biomaterial that has gained significant attention is calcium-enriched mixture (CEM) cement [1]. Similar to mineral trioxide aggregate (MTA), CEM cement is a type of calcium-silicate cement (CSC) that contains calcium compounds [2], which give it distinctive properties like biocompatibility, alkalinity, and bioactivity. As a result, CEM cement has gained significant attention in vital pulp therapy (VPT) within the field of endodontics [3]. Recognizing its potential advantages in various endodontic procedures, including sealing ability, biocompatibility, and release of bioactive ions promoting successful healing and treatment outcomes [4], CEM cement has emerged as a cornerstone in contemporary endodontics.
The composition, properties, and clinical efficacy of CEM cement form the crux of understanding and optimizing its application in endodontic treatments [5]. Responding to the growing interest and the emergence of newer CSCs in endodontics [6], this article aims to provide a more nuanced perspective by addressing the research gap and highlighting the novelty of CEM cement. Through a rigorous assessment of available evidence and analysis of relevant studies, this review delves deeper into the multifaceted aspects of CEM cement. By enabling clinicians/researchers to make informed decisions and advancements, the comprehensive review paves the way for the next phase of endodontic research. This comprehensive overview aims to summarize published studies on CEM cement. However, it is important to acknowledge certain limitations in our search strategy. As detailed in the Methods section (Sect. "Methods of searching existing literature"), we conducted comprehensive searches across multiple electronic databases and reviewed reference lists from relevant articles. Despite these efforts, our search was confined to published studies available in English, and we did not include a specific search for grey literature. Consequently, this may have led to the exclusion of some relevant studies, particularly those found in the grey literature, which could impact the comprehensiveness of our review.
Methods of searching existing literature
Objectives of the review
-
To discuss the composition and physical/chemical/biological properties of CEM cement.
-
To provide an understanding of the clinical applications of CEM cement in endodontics.
-
To examine the available evidence and level of research supporting the use of CEM cement in clinical endodontics.
-
To evaluate the limitations and potential challenges associated with the use of CEM cement in endodontics.
-
To propose future perspectives and potential advancements of CEM cement applications in clinical endodontics.
Search methodology
A comprehensive search strategy was implemented to identify relevant studies for this review. Electronic databases, including MEDLINE (via PubMed), Embase, and Scopus, were searched to retrieve articles published from the inception of the databases to June 2023. The search terms used were "CEM cement" and "calcium-enriched mixture cement".
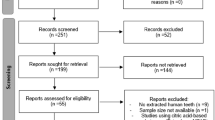
The search strategy adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Keywords and MeSH terms were selected based on initial exploratory searches and expert consultation. The detailed search strategy for PubMed is tabulated to facilitate replication by other researchers (Table 1).
The screening process involved the review of titles/abstracts to assess the relevance of articles to the review topic. Full-text articles that met the inclusion criteria were further evaluated for data extraction/analysis. Additionally, the references of selected articles were examined to identify any additional relevant studies that may have been missed during the initial search. The final search results were exported into EndNote, and duplicates were removed.
Inclusion criteria
-
Studies that investigate CEM cement and provide information on the composition, properties, clinical applications, and future perspectives.
-
Clinical/laboratory studies, systematic reviews, and meta-analyses.
Exclusion criteria
-
Studies not relevant to the topic of CEM cement.
-
Conference abstracts and letters to the editor.
PRISMA flowchart
A PRISMA flowchart (Fig. 1) is included in the revised manuscript to illustrate the selection process, showing the number of records identified, screened, and included in the review.
Risk-of-bias assessment
Although risk-of-bias assessments are crucial in systematic reviews, our study’s primary goal is to provide a broad synthesis of the evidence related to CEM cement rather than performing a meta-analysis of specific outcomes. Due to the variability in study designs, outcomes, and reporting standards among the included studies, conducting a formal risk-of-bias assessment was deemed less relevant. Instead, we have concentrated on summarizing the overall trends and common findings identified in the literature.
Article structure and details
For a detailed overview of the article structure and specifics, please refer to Appendix 1, which outlines the comprehensive organization and content of the review.
Composition and properties of CEM cement
Chemical composition
CEM cement is a member of calcium-silicate cements (CSC) characterized by its specific chemical composition, which plays a crucial role in its performance and clinical applications. Scanning electron microscopy (SEM) and electron probe microanalysis (EPMA) have revealed that CEM cement predominantly consists of calcium oxide (CaO; wt% = 51.81), sulfur trioxide (SO3; wt% = 9.48), phosphorous pentoxide (P2O5; wt% = 8.52), and silicon dioxide (SiO2; wt% = 6.28). Trace amounts of other elements, including aluminum oxide (Al2O3; wt% = 0.95), sodium oxide (Na2O; wt% = 0.35), magnesium oxide (MgO; wt% = 0.23), and chlorine (Cl; wt% = 0.18), are also present [7]. The X-ray diffraction (XRD) results further elucidate the mineralogical content of CEM cement, revealing reflections corresponding to tricalcium silicate (Ca3SiO5), dicalcium silicate (Ca2SiO4), silicon oxide (SiO2), and zirconium oxide (ZrO2), providing insights into the crystalline phases present in the material (unpublished data).
EPMA has shown similar distribution patterns of calcium, phosphorus, and oxygen between CEM cement and the surrounding dentin, indicating its compatibility with dental tissues. However, significant elemental variations have been observed in other CSCs, emphasizing the distinctive composition of CEM cement [8].
The notable concentrations of calcium, phosphorus, and silicon in CEM cement significantly influence its physical/chemical reactions, as well as its interactions with dental tissues. Calcium enhances bioactivity by promoting hydroxyapatite formation, which improves the cement’s bonding and mineralization capabilities. Phosphorus aids in this process by facilitating the formation of a mineralized layer that integrates with dental tissues and maintains a favorable pH balance. Silicon, present as silica, reacts with calcium to form calcium-silicate hydrate, which contributes to the cement’s strength, durability, and resistance to dissolution. Optimal levels of these elements contribute to the bioactivity, biocompatibility, and mechanical properties of CEM cement, making it suitable for a wide range of endodontic procedures [2].
The liquid used for mixing, phosphate-buffered saline (PBS) solution, is a critical component influencing the performance of CEM cement, particularly in its water-reactive characteristics.
Physical properties
Handling characteristics
Handling characteristics of CEM cement are crucial for its successful clinical application and ease of use during endodontic procedures. These properties determine its workability, manipulability, and ability to achieve optimal placement [9]. When the powder and liquid components of CEM cement are mixed, it results in a homogeneous white mixture with a smooth and creamy consistency.
One important aspect of handling characteristics is the working and setting time of CEM cement. According to ISO 6876-2001, the working time of CEM cement is almost similar to that of ProRoot MTA (average of 4.5 ± 0.77 min and 5 ± 0.79 min for CEM and ProRoot MTA, respectively). However, CEM cement has a shorter setting time, typically around 50 ± 7.5 min, as opposed to 70 ± 8.5 min for ProRoot MTA [7].
The flowability of CEM cement is significantly higher than that of ProRoot MTA, with a measurement of approximately 14 ± 1 mm compared to 10 ± 0.79 mm for ProRoot MTA [7]. This improved flowability allows CEM cement to easily penetrate the cavity, reach difficult-to-access areas, and effectively fill and seal irregularities. It plays a crucial role in preventing microleakage and ensuring a more reliable seal.
Furthermore, the film thickness of CEM cement is significantly thinner than that of ProRoot MTA, with an average thickness of approximately 174 ± 25 µm (452 ± 63 µm for ProRoot MTA) [7]. This allows for better adaptation and closer contact of the cement to the root canal walls, improving the quality of the seal and reducing the potential for microleakage. Additionally, CEM cement exhibits minimal dimensional changes compared to ProRoot MTA, with an average of 0.075 ± 0.032 mm, further contributing to its handling characteristics [7].
In summary, the smooth and creamy consistency of CEM ensures ease of use and precise placement. Properties comparable to/better than ProRoot MTA, including similar working time, shorter setting time, higher flowability, thinner film thickness, and minimal dimensional changes, make it a suitable choice for endodontic procedures.
Setting reaction
CEM cement undergoes complex chemical reactions during setting. The setting reaction of CEM cement is a critical process during which transformation from a flowable and creamy consistency to a solid and stable state occurs.
The setting process of CEM cement, similar to other CSCs, involves the reactions of tricalcium silicate and dicalcium silicate during hydration, resulting in the formation of calcium-silicate hydrate gel and calcium hydroxide [Ca(OH)2; CH] [10]. This gel-like substance provides initial cohesion and strength to the mixed cement. Additionally, the reaction between calcium and phosphorus ions contributes to the formation of hydroxyapatite [11], which is essential for the regeneration and remineralization of hard tissues. The alkaline pH of CEM cement is a result of the release of CH during the setting reaction [12]. This alkalinity provides the material with antimicrobial properties and supports the stimulation of hard-tissue formation.
Mixing and placing methods
The mixing and placing methods employed during the handling of CEM cement can have a significant impact on its properties and performance in endodontic procedures. Several studies have investigated the influence of different mixing techniques on various aspects of CEM cement, such as compressive strength, pH, solubility, and push-out bond strength [13,14,15,16,17]. Based on the ISO 6876:2012 standard, it has been demonstrated that an increased water-to-powder ratio leads to a reduction in compressive strength, an elevation in solubility, and a decrease in the microhardness of CEM cement [18, 19].
Furthermore, a systematic review conducted in 2019 assessed the impact of different mixing methods on various properties of CEM cement, including bacterial microleakage, push-out bond strength, flow rate, compressive strength, solubility, pH, film thickness, dimensional changes, working time, setting time, and the quality of the apical plug [20]. While no single mixing method was found to enhance all properties simultaneously, mechanical and manual methods generally showed better effectiveness compared to the ultrasonic method in improving specific properties of CEM cement [20].
These findings highlight the importance of proper mixing and placing techniques for CEM cement to achieve desired outcomes in endodontic procedures. Clinicians should consider the specific properties they aim to optimize and choose an appropriate mixing method accordingly. Mechanical and manual methods are generally recommended for better overall effectiveness.
Release of ions and pH
CEM cement is recognized for its capacity to release calcium (Ca2+) and phosphate (PO43−) ions from indigenous sources over time, which facilitates the formation of mineralized tissues such as dentin and cementum [11]. Notably, studies have demonstrated that CEM cement exhibits a significantly higher release of phosphate ions during the first hour after mixing compared to other materials [12]. Furthermore, the setting reaction of CEM cement generates hydroxyl ions (OH−), leading to an elevated pH level [12]. This alkaline pH environment offers various advantages, including antimicrobial properties and favorable interactions with dental tissues.
Effect of environment
The effect of different environmental conditions on the behavior of CEM cement has been investigated in several studies, encompassing storage solutions, blood contamination, solvents, and variations in pH [11, 21,22,23,24,25,26].
One study demonstrated that the choice of storage solution affects the surface topography of root-end fillings, with CEM cement showing greater hydroxyapatite formation in phosphate buffer solution compared to normal saline solution [11]. Another study evaluated the impact of blood contamination on CEM cement, revealing that while it does not affect compressive strength, the incorporation of blood renders the cement more brittle [21]. Additionally, the response of CEM cement to different solvents was assessed, with solvents found to be more effective in reducing the microhardness of Angelus MTA compared to CEM cement [22].
The effect of blood exposure on push-out bond strength was examined, showing an influence on various CSCs, including CEM cement. After exposure to blood, the push-out bond strength of all materials increased over time [23]. The application of different bleaching agents on the microstructure of set CEM cement was also investigated, revealing variations in the mean elemental distribution of completely set CEM cement when exposed to sodium perborate, carbamide peroxide, and hydrogen peroxide [24]. Furthermore, surface microstructure analysis of CEM cement and other bioceramic materials under different pH conditions provided insights into their behavior [25]. Studies exploring the microstructure and chemical analysis of various CSCs, including CEM cement, under different environmental conditions, have highlighted the impairment of CH formation in the presence of blood and acid exposures in ProRoot MTA and CEM cement [26]. The influence of pH on the physical properties of CEM cement and ProRoot MTA was examined in another study. The surface microhardness and setting time of the cements were evaluated when exposed to acidic, neutral, and alkaline solutions. The results revealed that CEM cement exhibited a faster setting time compared to ProRoot MTA. However, both cements were negatively affected by acidic pH. Furthermore, the surface topography and elemental composition of the cements were altered in different pH environments [27].
Overall, these studies provide valuable insights into the behavior of CEM cement under different environmental conditions, helping to optimize its clinical application.
Compressive strength
Two studies have explored the factors influencing the compressive strength of CEM cement. In one study, the effect of acid etching procedures on the compressive strength of four CSCs, including CEM cement, was evaluated. The results demonstrated that acid etching harmed mechanical properties and compressive strength of all tested CSCs [28]. Another study indicated that the addition of propylene glycol to Angelus MTA and CEM cement affected the compressive strength of both biomaterials [29].
Flexural strength
The flexural strength of CEM cement has been the subject of investigation in several studies, which have compared it with other materials such as MTA, BioAggregate, and CH. In one study, the flexural strength of Angelus MTA, CEM cement, and BioAggregate was compared according to the ISO 4049 standard, revealing significant differences among the three materials [30]. Another study evaluated the short-term effect of CH, ProRoot MTA, and CEM cement on the strength of bovine root dentin, showing that both MTA and CEM cement caused a decrease in the flexural strength of bovine root dentin, similar to CH [31].
Furthermore, a study examined the long-term impact of CEM cement, Angelus MTA, and CH on the flexural strength of bovine dentin. The findings indicated that after 1 year, the flexural strength of dentin decreased in CH and Angelus MTA groups, while the samples exposed to CEM cement maintained their initial strength [32].
Push-out strength
The push-out bond strength of CEM cement has been extensively investigated in various research studies. One study compared the bond strength of CEM cement and ProRoot MTA in root-end cavities prepared using either ultrasonic or Er,Cr:YSGG laser, demonstrating comparable bond strength of CEM and ProRoot MTA which was higher in ultrasonically prepared cavities [33]. Another study emphasized the importance of smear layer removal for achieving higher push-out bond strength in CEM cement [34]. Comparative evaluations of different MTA formulations and CEM cement have provided valuable insights into their push-out bond strength [35].
The effect of an alkaline environment on the push-out bond strength of CEM cement has been investigated, contributing to our understanding of its mechanical properties [36]. Placement of CH before CEM cement in simulated furcation perforations has been shown to improve the bond strength [37]. Furthermore, the impact of calcium chloride on the push-out bond strength of CEM cement and Angelus MTA was explored, revealing an increase in bond strength over time for CEM cement, while the addition of calcium chloride decreased the strength of Angelus MTA [38].
Comparative evaluations of various endodontic irrigants on the push-out bond strength of CEM cement and ProRoot MTA have demonstrated higher bond strength for CEM cement, with an increase over time [15]. Dentin conditioning using a diode and Er:YAG laser has enhanced the bond strength of CEM cement and other CSCs [39]. Studies have shown no adverse effects of intracanal medicaments on the push-out bond strength of CEM cement [40, 41]. Laser-assisted retrograde cavity preparation has also been found to impact the push-out bond strength of CEM cement and Angelus MTA [42].
Comparative evaluations of retrograde root-end filling materials, including CEM cement and Biodentine, have provided insights into their push-out bond strength [43]. Additionally, comparisons between Root MTA and CEM cement have further contributed to understanding their bonding characteristics [44]. The push-out bond strength of two CSCs used for the repair of artificial furcal perforations has been influenced by different power outputs of Nd:YAG laser [45]. These studies collectively enhance our understanding of the push-out bond strength of CEM cement and its performance in various clinical scenarios.
Bond strength
Bond strength directly influences the durability and effectiveness of restorative procedures and a strong bond is essential for the long-term stability and success of dental restorations [46]. Understanding the bond strength properties of dental materials is crucial for optimizing bonding techniques, selecting appropriate materials, and achieving successful clinical outcomes [47]. Several factors contribute to bond strength, including the material used, surface preparation techniques, adhesive systems employed, and the characteristics of the tooth structure being bonded.
Research has demonstrated comparable shear bond strength of CEM cement and ProRoot MTA to composite resin, with surface etching having minimal impact on their bond strength [46]. Resin-modified glass ionomer (RMGI) cement exhibits higher shear bond strength to pulp capping agents compared to composite resin, while the bond strength of composite resin to ProRoot MTA is weaker than that of CEM cement [48]. RMGI cement demonstrates superior bond strength to composite resin compared to ProRoot MTA or CEM cement, regardless of the adhesive system used [49]. ProRoot MTA and CEM cement exhibit higher shear bond strength than Biodentine, making them more suitable for use with flowable composites [50]. The bond strength of self-adhering flowable composite resin to Root MTA and CEM cement is higher than RMGI, and additional adhesive application further enhances the bond strength [51]. The shear bond strength of silorane and nanohybrid composite resins to CEM cement has been evaluated over different time periods [52]. The type of pulp capping material and bonding system have minimal impact on the bond strengths of composite resin to ProRoot MTA and CEM cement [53].
In conclusion, bond strength is a critical aspect of restorative dentistry, and studies have investigated the bond strengths of CEM cement and various MTAs to different substrates.
Fracture resistance
Fracture resistance is a critical parameter in assessing the success and longevity of restorative procedures in dentistry. In an ex vivo study, evaluating the reinforcement of immature teeth by ProRoot MTA and CEM cement after a 6-month period, both biomaterials demonstrated significant improvements in fracture strength [54]. Another study involving simulated immature teeth filled with Angelus MTA, CEM cement, and Biodentine found that all three materials contributed to increased fracture resistance compared to the control group with no statistically significant differences among Angelus MTA, CEM cement, and Biodentine [55]. In another study, no significant differences in fracture strength of teeth restored with a fiber post and Angelus MTA or CEM cement apical plug were observed [56].
These studies emphasize the positive impact of preferred CSCs, including CEM cement, on fracture resistance of restored teeth.
Microhardness
According to several studies comparing the microhardness properties, MTAs generally exhibit higher microhardness values compared to other (bio)materials [27, 57, 58]. Factors such as exposure to acids or PBS can influence the microhardness of these biomaterials, with PBS exposure leading to increased microhardness [57]. On the other hand, humidity conditions and indentation thickness may not have a significant impact on the microhardness of Angelus MTA and CEM cement plugs [58]. It is worth noting that the pH of the environment can affect the microhardness and setting time of these materials, meaning that acidic solutions negatively affect their properties [27].
The microhardness of ProRoot MTA decreases in the presence of bone graft powder, while CEM cement is not significantly affected [59]. Additionally, the immediate placement of coronal restorations can influence the setting reaction of CEM cement. Proper moist curing and hydration before restoration placement are crucial to ensure optimal properties [60].
In a study investigating the microhardness of CEM cement and glass ionomers at different periods, an increase in surface microhardness was observed in both materials over time from 1 to 7 days. This suggests that using glass ionomers adjacent to CEM cement in single-visit restorative treatments could be advantageous [61].
Particle size
In a comparative study, although there were no significant differences in the mean particle size of CEM cement and ProRoot MTA, differences were observed in the particle distribution within the size range of ≤ 30 μm. CEM cement exhibited a narrower range of particle sizes in this range compared to ProRoot MTA. Notably, CEM cement contained a higher percentage of small particles [62].
The presence of a high percentage of small particles in CEM cement contributes to its desirable properties and performance in clinical applications. These small particles facilitate effective sealing, as they can penetrate into microgaps and irregularities, ensuring a more thorough seal. The optimal setting time of CEM cement is also influenced by its particle-size distribution, with the presence of small particles allowing for a more efficient setting reaction. The appropriate film thickness of CEM cement is achieved in part due to the presence of small particles, which contribute to a more compact and closely packed material. Additionally, the flow and adaptability of CEM cement are enhanced by the presence of small particles, allowing for easier manipulation and placement in various clinical scenarios.
Overall, the particle-size distribution of CEM cement, particularly the presence of a high percentage of small particles, contributes to its desirable properties and ensures its effective performance as an endodontic biomaterial.
Radiopacity
While CEM cement exhibits a higher radiopacity at least twice to that of dentin (2.227 mmAl), it is essential to consider that it may not meet the ISO standard (ISO 6877, 2006) [63]. The radiopacity of CEM cement allows for the identification and differentiation of the material from surrounding tooth structures on radiographs, which is beneficial for its clinical use and assessment.
Another study investigated the radiopacity of CEM cement using various scanners. The study found that the Hounsfield unit (HU) and grayscale value (GSV) measurements of dental materials, including CEM cement, varied depending on the scanner used [64].
Elevated radiopacity of CEM compared to dentine provides clinical advantages in terms of material identification and assessment on radiographs. Clinicians must be aware of the potential variations in radiopacity measurements due to different imaging devices and to follow standardized protocols to ensure accurate radiographic evaluation of CEM cement and other dental materials.
Color stability
While no clinical evidence specifically addresses the tooth discoloration potential of CEM cement, studies have investigated CEM cement and various MTAs, comparing them to other dental materials and evaluating their potential for tooth discoloration [65,66,67,68,69,70,71,72,73,74,75]. The findings consistently indicate that both MTA and CEM cement have the potential to cause tooth discoloration, although the degree of discoloration varies between the two biomaterials. ProRoot and Angelus MTAs generally exhibit greater discoloration compared to CEM cement [65, 68]. Comparative studies suggest that CEM cement exhibits a lower color-changing potential compared to Angelus MTA [66, 67]. Furthermore, CEM cement has been found to induce similar levels of discoloration as CH, indicating its suitability for use in esthetically sensitive areas [67].
Factors such as the light curing duration of the restorative material and exposure to different media significantly influence the color stability of ProRoot MTA and CEM cement. Longer light curing durations have been shown to result in decreased lightness (ΔL) and increased overall color change (ΔE) values in both biomaterials [65]. This highlights the importance of proper light curing techniques and durations to minimize the risk of discoloration. Additionally, the interaction of MTA and CEM cement with irrigation solutions, such as chlorhexidine and sodium hypochlorite, has been found to affect their color stability, with severe discoloration observed in some cases [69].
In summary, when performing VPT in esthetic zones, it is crucial to consider the color stability of endodontic biomaterials, particularly MTA and CEM cement. Clinicians should be aware of factors such as light curing duration, exposure to different media, and interactions with irrigation solutions that can influence color stability. By taking these factors into account and selecting appropriate materials, the risk of tooth discoloration can be minimized, leading to better clinical outcomes and patient satisfaction.
Role of additives
The role of additives in modifying the properties of CEM cement has been the subject of several studies. For example, the addition of calcium chloride (CaCl2) was found to significantly decrease the initial setting time of CEM cement [76]. Another study revealed that the addition of propylene glycol (PG) to CEM cement did not affect the flowability of the cement and increased its microhardness over the long term. Moreover, calcium ion release was increased [77].
Incorporating titanium dioxide nanoparticles into various cement types, including CEM cement, was explored in another study, although specific findings and conclusions were not provided [78]. Additionally, the bond strength of CEM cement in the presence of certain concentrations of propylene glycol was decreased [79]. Chemical modification of Angelus MTA and CEM cement by adding alkaline salts led to a decrease in setting time, an increase in pH and calcium ion release, and the deposition of hydroxyapatite on the surface of the samples [80]. These studies highlight the potential of additives to influence various properties of CEM cement, such as setting time, flowability, microhardness, bond strength, pH, and ion release. However, further research is needed to fully understand the effects of different additives on the overall performance and clinical applications of CEM cement.
Sealing ability
Root-end filling
Numerous studies have demonstrated that in comparison to MTA-like biomaterials, CEM cement exhibits comparable or superior sealing properties [81, 82]. CEM cement has shown excellent sealing ability in PBS and has demonstrated similar or better sealing ability than intermediate restorative material (IRM) and amalgam [83,84,85,86]. Moreover, CEM cement has exhibited similar levels of microleakage compared to commonly used root-end filling materials [87]. The presence of a smear layer enhances the sealing ability of both ProRoot MTA and CEM cement in root-end fillings [88].
Several factors have an impact on the sealing ability of CSCs. Saliva contamination has been shown to affect the sealing ability, with CEM cement being less affected [89]. While root resection procedures did not significantly affect the sealing ability of Angelus MTA, they increased microleakage in CEM cement [90]. Studies have indicated that a 3-mm thickness of CEM cement is sufficient for effective root-end sealing [91].
Comparative evaluations of different techniques and mixing methods have not revealed significant differences in sealing ability [92,93,94]. These findings collectively support the sealing effectiveness of CEM cement as a viable alternative to other CSCs, highlighting its potential for use in various endodontic applications.
Perforation repair
Multiple studies have examined the microleakage and sealing ability of CEM cement in the repair of furcation perforations. In comparison to ProRoot MTA, CEM cement has consistently shown significantly less microleakage using the fluid filtration method [95]. In primary molar teeth, studies have reported no significant difference in microleakage between ProRoot MTA and CEM cement [96, 97]. Additionally, the bacterial leakage potential of ProRoot MTA, CEM cement, and Biodentine has been found to be similar [98]. Selecting the appropriate biomaterial is essential for achieving successful furcal perforation repair in dental procedures.
Apical plug
CEM cement has been extensively studied as a biomaterial for use as an apical barrier in endodontic procedures [99,100,101,102,103,104,105,106,107]. CEM cement exhibits superior sealing performance compared to Angelus MTA, particularly in dry and saliva-contaminated conditions [99]. The diameter of the canal and the thickness of the apical plug have been identified as important factors influencing the sealing ability of CEM cement [100]. Various studies have investigated different mixing and placement methods of CEM cement, with manual placement in association with the indirect ultrasonic technique showing promising results in reducing the number of voids [101]. The powder-to-liquid ratio of CEM cement has also been shown to impact its sealing ability, with higher ratios resulting in better sealing outcomes [102]. CH premedication does not have any adverse effect on short- or long-term sealing properties of CEM apical plugs [107]. The influence of alkaline pH and the addition of propylene glycol did not have adverse effects on the sealing ability of Angelus MTA and CEM cement [103, 104]. Microleakage studies have consistently shown that CEM cement exhibits comparable results to other biomaterials, such as Biodentine, and has better sealing ability compared to Angelus MTA [99, 105].
Various factors, including canal diameter, apical plug thickness, mixing and placement techniques, pH conditions, and powder-to-liquid ratios, can influence the sealing performance of these materials.
Coronal barrier
Both CEM cement and ProRoot MTA have been shown to be more effective than amalgam and composite resin in terms of coronal sealing [108]. The thickness of the CEM cement has also been investigated, with no statistically significant difference in coronal microleakage observed between 2 and 3 mm thicknesses [109]. Furthermore, CEM cement, Angelus MTA, and glass ionomer cement have been identified as suitable intra-orifice barriers to provide a coronal seal during nonvital bleaching procedures [110]. Microleakage assessments comparing Angelus MTA, CEM cement, and Biodentine as intra-orifice barriers demonstrated that CEM cement exhibited the least microleakage, although the differences were not statistically significant [111]. Additionally, CEM cement has shown sealing properties comparable to Angelus MTA when used as a cervical barrier during intra-coronal bleaching procedures [112]. In a comparative study, Angelus MTA, CEM cement, and Biodentine showed equally promising results as coronal plugs during internal bleaching procedures [113].
In summary, studies have indicated the effectiveness of CEM cement and MTAs as coronal barriers in endodontically treated teeth. The thickness of the material and its application technique should be considered, and further research is needed to optimize their clinical performance.
Root canal filling
Studies investigating the sealing ability of CEM cement have demonstrated favorable coronal and apical seals when using the simple single-cone technique [114]. It has been concluded that single-cone obturation with both ProRoot MTA and CEM cement is a suitable technique [114, 115]. In an in vitro study comparing orthograde ProRoot MTA and CEM cement, no significant differences were observed in bacterial leakage between the two biomaterials [92]. Additionally, an investigation on apical microleakage in root canals with broken rotary instruments revealed that CEM cement exhibited the lowest microleakage, whereas injected gutta-percha showed the highest microleakage. Importantly, no significant difference in microleakage was found between CEM and OrthoMTA [116].
Marginal adaptation
Studies have investigated the marginal adaptation of CEM cement in various scenarios and compared it to other materials. The findings indicate that CEM cement demonstrates favorable marginal adaptation in different conditions. CH premedication did not negatively affect the marginal adaptation of the CEM cement apical plug [107]. The addition of calcium chloride as an accelerator substance also did not significantly influence the marginal adaptation of CEM cement [117]. Blood contamination did not have an impact on the marginal adaptation of CEM cement, Angelus MTA, Biodentine, or BioAggregate [73]. Additionally, when comparing Angelus MTA and CEM cement in root canal treatment (RCT), a similar prevalence of cracks was observed in the apical plug, suggesting that both materials can be used with potential future surgical access [118].
Antimicrobial attributes
Antibacterial
Studies have consistently shown that CEM cement possesses potent antibacterial activity similar to CH [119,120,121]. The addition of chlorhexidine enhanced the antibacterial activity of both ProRoot MTA and CEM cement [122, 123]. Incorporating dentin powder into the suspension of CEM cement or ProRoot MTA has also resulted in more rapid elimination of bacteria [124]. Moreover, the inclusion of silver nanoparticles in ProRoot MTA and CEM cement has demonstrated increased antimicrobial activity [125]. Comparative studies have highlighted the comparable or even superior antibacterial effects of CEM cement compared to other root canal filling materials. When compared to Biodentine, CEM cement has displayed higher antibacterial activity against Enterococcus (E) faecalis [126, 127]. Similarly, CEM cement has exhibited stronger antimicrobial effects against both E. faecalis and Candida albicans compared to Angelus MTA [127].
These findings underscore the potential for modifying the antibacterial properties of CEM cement and other biomaterials to enhance their performance in combating microbial infections during endodontic procedures.
Antifungal
One study demonstrated that different power/liquid ratios in CEM cement effectively inhibited the growth of Candida albicans, except the early hours, indicating its anti-fungal property which was unaffected by the power/liquid ratio [128]. In another study comparing the anti-fungal effects of CEM cement and ProRoot MTA against Candida albicans, both biomaterials exhibited complete fungicidal activity after 24 and 48 h, even at a concentration of 50 mg/mL [129].
Bioactivity
One study examined the impact of various storage solutions, such as normal saline and phosphate buffer solutions, on the surface characteristics of CEM cement and ProRoot MTA root-end fillings. The findings indicated that both biomaterials experienced crystal formation and precipitation on their surfaces, except for ProRoot MTA stored in normal saline. The composition and structure of the precipitated crystals resembled hydroxyapatite, suggesting a bioactive response. This bioactivity is believed to contribute to the biocompatibility and sealing ability of ProRoot MTA and CEM cement, leading to the formation of an additional biological seal (Bioseal) at the interface between the biomaterial and dentine [11].
Another study investigated the bioactivity of CEM cement, MTA, hydroxyapatite, and nano-hydroxyapatite-chitosan cements. These cements were immersed in a simulated body fluid solution, and parameters, such as pH, surface morphology, calcium–phosphorus ratio, and apatite deposition, were assessed. All tested cements demonstrated bioactivity, with CEM cement and nano-hydroxyapatite-chitosan cements exhibiting superior bioactive characteristics in terms of pH values [130]. A study has demonstrated the bioactivity of CEM cement and ProRoot MTA on dental pulp stem cells (DPSCs) through dentin. These biomaterials have shown the ability to stimulate cell proliferation, promote cell attachment, and induce the formation of calcified structures resembling hydroxyapatite [131].
Biocompatibility
Cytotoxicity
In a study examining the cytotoxicity of CEM cement and ProRoot MTA on L929 cell culture, similar cytotoxic effects were observed between the two materials. However, the viability of cells was better in the presence of set materials compared to fresh ones, indicating improved cell compatibility over time [132]. Another comparative study assessed the cytotoxicity of CEM cement, ProRoot MTA, and IRM, and found that CEM cement exhibited lower cytotoxicity than IRM, suggesting its potential as a less harmful alternative material [133].
Further investigations have evaluated the cytotoxic effects of CEM cement on specific cell types. In vitro cytotoxicity tests on human monocytes compared the effects of four CSCs, including CEM cement and ProRoot MTA, and revealed that CEM cement demonstrated lower cytotoxicity than ProRoot MTA after 48 h of incubation [134]. Similarly, a study on stem cells of human apical papilla (SCAP) demonstrated acceptable biocompatibility of CEM cement and less cytotoxicity compared to ProRoot MTA over time, indicating its suitability for regenerative endodontic procedures [135].
Comparative studies involving various biomaterials have shown comparable cytotoxicity profiles among different CSCs used as root-end filling materials [136]. Another study comparing the cytotoxicity of ProRoot MTA, CEM cement, Biodentine, and octacalcium phosphate against human gingival fibroblasts (HGF) found no significant difference in cytotoxicity among the tested materials, suggesting their overall biocompatibility [137].
Moreover, studies investigating the cytotoxicity of CEM cement on specific cell types have demonstrated favorable biocompatibility. A study examining the effect of three different biomaterials, including CEM cement, on the proliferation and viability of human dental pulp stem cells (DPSCs), showed that all tested biomaterials supported the proliferation of DPSCs, with CEM cement exhibiting the least cytotoxicity over time [138]. Another study evaluated the cytotoxicity of Angelus and nanohybrid MTAs with CEM on human gingival fibroblasts (HGF) and found that both set CEM cement and set MTAs had similar and favorable effects on cell viability [139]. Furthermore, the combination of CEM cement and Emdogain-coated biomaterials demonstrated high cell viability in DPSCs, indicating their potential for regenerative procedures [140]. Additionally, studies on the antimicrobial and cytotoxic properties of CEM cement found that the cement exhibited high viability of dental pulp stem cells in comparison with Iranian propolis and propolis with herbal extracts [141]. Application of low-level laser therapy (LLLT) with dental capping agents, including ProRoot MTA, EMD, and CEM cement, increased the cell viability percentage of SCAPs, suggesting the synergistic effect of LLLT and CEM cement in promoting cell viability [142].
SEM cytotoxicity evaluations of CEM cement in different experimental setups demonstrated normal cell morphology and favorable cell adhesion of HGFs exposed to CEM cement, with no statistically significant differences observed compared to ProRoot MTA [143]. Another study evaluating the attachment of gingival fibroblasts to root surfaces restored with various dental materials, including CEM cement, demonstrated acceptable biocompatibility of CEM cement and other tested materials after 24 h and up to 5 days of incubation [144]. Overall, these studies collectively indicate that CEM cement exhibits favorable biocompatibility and lower cytotoxicity compared to certain other biomaterials.
Mutagenicity
The Ames test was employed to evaluating the mutagenicity of commonly used pulpotomy agents. While ferric sulfate exhibited mutagenic effects at certain concentrations and formocresol displayed significant toxicity, CEM cement did not induce significant reverse mutations and was classified as a non-mutagenic and less toxic agent [145]. These results suggest that CEM cement may present a safer alternative in terms of mutagenicity compared to other pulpotomy agents.
Genotoxicity
In a study investigating the genotoxicity of CEM cement and ProRoot MTA, L929 mouse fibroblast cells were exposed to different concentrations of these biomaterials. At low concentrations, CEM cement exhibited more noticeable genotoxic effects. However, at higher concentrations, CEM cement demonstrated lower genotoxicity compared to ProRoot MTA. Both biomaterials displayed increased genotoxicity in a concentration-dependent manner. The study concluded that CEM cement is biocompatible in terms of cyto- and genotoxicity and suggested that it could serve as a favorable alternative to ProRoot MTA, offering several advantages [146]. These findings provide valuable insights into the genotoxicity profile of CEM cement, indicating its potential for safe use in various dental applications.
Gene expression
In a study investigating the odontogenic differentiation of dental pulp stem cells (DPSCs) induced by CEM cement and ProRoot MTA, the gene expression and cytokine release were examined [147]. The results showed that both CEM cement and ProRoot MTA supported the adherence, proliferation, and spreading of DPSCs. Gene expressions of dentin matrix protein 1 (DMP1) and dentin sialophosphoprotein (DSPP) were similar in CEM cement, ProRoot MTA, and dentin matrix (DM) groups, and significantly higher compared to the negative control. The gene expressions of fibroblast growth factor 4 (FGF4) and bone morphogenetic protein 2 (BMP2) through protein concentration analysis were significantly higher in the CEM cement group. The study concluded that both ProRoot MTA and CEM cement can induce osteo-/odontogenic differentiation of DPSCs, albeit with different gene expressions and growth factor release. In another study comparing the effects of ProRoot MTA, Biodentine, and CEM cement on DPSCs, it was found that the CEM cement group showed minimal expression of dentin sialophosphoprotein (DSPP) and DMP1 [148].
Furthermore, in a study investigating the effect of ProRoot MTA and CEM cement on mineralization-associated gene expression in SCAP, the 2-week expression of various mineralization genes was significantly upregulated compared to the control group [149]. Alizarin red staining confirmed the formation of mineralized nodules in all groups, with larger nodules observed in the ProRoot MTA group at 3 weeks. The study concluded that both ProRoot MTA and CEM cement upregulated mineralization-associated gene expression, with ProRoot MTA showing a greater effect after 3 weeks compared to CEM cement.
These studies provide insights into the gene expression profiles and osteo-/odontogenic differentiation potential of CEM cement and ProRoot MTA, indicating their ability to promote the expression of key genes involved in mineralization and dentin formation.
Cytokine release
The release of cytokines by endodontic biomaterials can influence the behavior of DPSCs, including their proliferation, migration, and differentiation capabilities [150, 151]. CEM cement has shown the capacity to stimulate the release of specific cytokines, which play essential roles in cellular communication and tissue healing [152, 153]. In terms of cytokine release, both CEM cement and ProRoot MTA have demonstrated comparable abilities to induce cytokine production. Studies have revealed that these biomaterials can promote the release of transforming growth factor-beta 1 (TGF-β1) and bone morphogenetic protein-2 (BMP-2), which are involved in crucial cellular processes such as cell proliferation, differentiation, and tissue formation [152, 154].
Cell differentiation
Differentiation of DPSCs into odontogenic/osteogenic lineages is a critical process in regenerative dentistry. Studies have shown that CEM cement, ProRoot MTA, and nano-hydroxyapatite have potential applications in pulp capping and regenerative therapies and can promote odontogenic differentiation of DPSCs [152]. Comparing the effects of CEM cement and ProRoot MTA on the survival and mineralization potential of human mesenchymal stem cells (hMSCs) indicated similar cell viability and CEM cement enhanced osteocalcin gene expression [155]. Another study focused on the effect of CEM cement on the mineralization ability of stem cells of human exfoliated deciduous teeth (SHEDs) using alizarin red staining and reported more mineralized nodules in CEM cement samples [156]. This suggests that CEM cement can stimulate mineral deposit formation and enhance osteoblastic differentiation. Comparative studies have also evaluated the differentiation potential of various biomaterials on stem cells from the apical papilla (SCAPs) [157, 158]. It was found that ProRoot MTA had a greater potential for inducing odontoblastic differentiation of SCAPs, while osteocalcin phosphate cement (OCP) had a higher potential for inducing osteoblastic differentiation [157]. Additionally, a comparative study showed that the CEM/Emdogain combination was highly effective in promoting the differentiation of SCAPs, gene expression related to odontogenesis, and alkaline phosphatase (ALP) activity [158].
These findings demonstrate the potential of CEM cement in promoting the differentiation of dental stem cells toward odontogenic and osteogenic lineages. This supports its use in regenerative dentistry and provides opportunities for developing novel treatment approaches. Further research is needed to explore the underlying mechanisms and optimize the differentiation potential of CEM cement for clinical applications.
Electrophysiological effects
The effects of CEM cement and ProRoot MTA on the firing behavior and action potential (AP) of neuronal cells were examined in a study. Both biomaterials had a significant reduction in neuronal activity which is mediated by the enhancement of outward potassium ion currents. These findings indicate that CEM cement and ProRoot MTA can modulate neuronal activity and may have potential applications in regenerative endodontics [159].
It is important to note that further research is necessary to fully understand the electrophysiological effects of CEM cement and ProRoot MTA on neuronal cells and their implications in clinical settings. The findings suggest the potential for these biomaterials to interact with neuronal cells and provide a basis for exploring their use in neuroregenerative approaches.
Subcutaneous reaction
In a comparative study evaluating subcutaneous tissue responses, CEM cement demonstrated favorable outcomes compared to white and grey ProRoot MTAs [160]. At the 1-week mark, CEM cement did not exhibit any signs of necrosis, while both ProRoot MTAs showed necrotic tissue. At the 60-day mark, CEM cement displayed significantly less inflammation than the other biomaterials. Overall, all biomaterials, including CEM cement, were well tolerated by the subcutaneous tissues, with the presence of dystrophic calcifications near the biomaterials, indicating their osteoinductive properties [160].
These findings suggest that CEM cement has a favorable biocompatibility profile in subcutaneous tissues and can induce osteoinductive responses. However, it is important to note that the study focused on subcutaneous tissue reactions, and further research is needed to evaluate the tissue responses and biocompatibility of CEM cement in other clinical applications.
Intraosseous implantation
In a comparative study evaluating the osseous reaction to the implantation of CEM cement and ProRoot MTA, after 1, 4, and 8 weeks of implantation, the number of inflammatory cells decreased similarly in both CEM cement and ProRoot MTA groups. Additionally, new bone formation increased in both ProRoot MTA and CEM groups, again without statistically significant differences [161]. These findings suggest that CEM cement exhibits a comparable level of osteoconductivity to ProRoot MTA when used for intraosseous implantation.
It is important to note that this study focused on the osseous reaction and biocompatibility of CEM cement and ProRoot MTA in an intraosseous implantation model. Further research is needed to assess the long-term effects, mechanical properties, and clinical outcomes of CEM cement in intraosseous applications to fully evaluate its efficacy as a biomaterial in this context.
Skin test
In a histological study assessing skin test reactivity in rabbits, the ProRoot MTA group exhibited a statistically higher level of inflammation, followed by CEM cement and control groups [162]. Another study found significant differences in erythematous surface areas at 1, 24, and 48 h after removing the implanted materials from rabbits. However, there was no significant difference at 72 h. The average erythematous surface areas were wider in Root MTA compared to CEM cement [163]. These findings suggest that CEM cement exhibits higher biocompatibility than MTAs in terms of skin reaction. Further research is necessary to evaluate the skin reactivity and biocompatibility of CEM cement in human subjects and to assess its clinical implications in dermatological applications.
Induction of dentinogenesis
Animal studies
In an SEM evaluation of dog pulp reactions to CEM cement, ProRoot MTA, and CH, all test pulp capping agents could stimulate calcified tissue formation in the underlying pulp [164]. Furthermore, a comparative histologic study showed that both ProRoot MTA and CEM cement exhibited similar responses and did not induce pulpal inflammation with a complete dentinal bridge formed in 75% of cases. In contrast, CH exhibited inflammation and incomplete dentinal bridge formation in all cases [165]. This suggests that both CEM cement and ProRoot MTA have the potential to promote dentinal bridge formation and preserve pulp vitality, surpassing the performance of CH.
Moreover, a preliminary study investigated the histopathologic response of dental pulp to pulp capping using Angelus MTA or CEM cement in diabetic rats. The results indicated that while both materials induced dentin bridge formation in diabetic and healthy controls, CEM cement-treated diabetic rats exhibited a significantly higher inflammatory response compared to healthy controls [166].
Additionally, another comparative histologic study demonstrated significantly higher dentinal bridge formation, preserved pulp vitality, and absence of inflammation in teeth treated with CEM cement and ProRoot MTA compared to CH [167]. These findings underscore the superior biological responses of CEM cement and ProRoot MTA in pulp capping procedures, indicating their potential applications in preserving pulp vitality and promoting dentin formation.
These animal studies collectively provide evidence that CEM cement and ProRoot MTA can induce dentinogenesis and promote the formation of dentinal bridges in pulp capping procedures. They demonstrate superior biological responses compared to CH, which is a traditional pulp capping material. The results suggest that both CEM cement and ProRoot MTA have potential applications in preserving pulp vitality and promoting dentin formation, contributing to the overall success of endodontic treatments. However, further research and clinical studies are needed to validate these findings and assess their applicability in human subjects.
Human studies on permanent teeth
In a clinical study evaluating the histologic assessment of human pulp response to capping with CEM cement and ProRoot MTA, both biomaterials showed significantly improved pulp response after 8 weeks compared to 2 weeks. They exhibited a thicker and more tubular dentinal bridge pattern, reduced pulp inflammation, and a palisade pattern of odontoblast cells. Although there was no significant difference between ProRoot MTA and CEM cement at both time intervals in each measure, CEM cement induced a thicker dentinal bridge with less pulp inflammation compared to ProRoot MTA [168]. Another immunohistochemical study investigating fibronectin (FN) and tenascin (TN) expression in human tooth pulp capped with ProRoot MTA and CEM cement revealed staining for FN and TN in the dentinal bridge matrix after 2 weeks. However, the expression of both markers decreased significantly after 8 weeks, with staining observed only in the unmineralized parts of the dentinal bridge. The staining pattern of TN in the CEM cement group was slightly higher than in the ProRoot MTA group, although the difference was not significant. The study concluded that both materials are suitable for direct pulp capping (DPC) and contribute to the formation of a reparative dentinal bridge [169]. A comparative study evaluating the histological evaluation of human pulp response to DPC with CEM cement, Angelus MTA, and Biodentine found that although dentin bridge formation and thickness were higher in the Biodentine group, the pulp exhibited greater inflammation compared to CEM cement and Angelus MTA. The study suggested that CEM cement and Angelus MTA performed better as DPC materials [170]. In a preliminary report on the histological outcome of pulpotomy with CEM cement and MTA compared to CH, it was found that CEM cement and ProRoot MTA were reliable biomaterials for full pulpotomy treatment, while the human dental pulp response to CH was unpredictable [171].
Human studies on primary teeth
In a case report examining the histological and CBCT evaluation of a pulpotomized primary molar using CEM cement, thick and complete calcific bridges with tubular dentin were observed at the amputation sites. The underlying dental pulp exhibited a normal structure and was free from inflammation [172]. The findings suggest that CEM cement can elicit a favorable biological response in the dental pulps of primary teeth. In a randomized clinical trial comparing nano-hydroxyapatite (NHA) and CEM cement for DPC in sound primary teeth, CEM cement demonstrated superior outcomes in terms of calcific bridge formation and pulp inflammation scores compared to NHA [173]. A histopathological evaluation of primary teeth after DPC with CEM cement and bioactive glass found that both materials were suitable for DPC, exhibiting calcific bridge formation and low pulp inflammation scores [174]. A study comparing the effects of CEM cement, propolis, and MTA as DPC agents found that their impact on pulpal tissue was comparable [175].
These clinical studies demonstrate that CEM cement is effective in promoting dentin bridge formation and reducing pulp inflammation in both permanent and primary teeth. It shows favorable biocompatibility and holds promise as a biomaterial for pulp capping and pulpotomy procedures.
Induction of cementogenesis
In studies investigating the induction of cementogenesis, CEM cement has shown promising results:
Periradicular regeneration: A study evaluating periradicular regeneration after endodontic surgery using CEM cement and ProRoot MTA observed the deposition of cementum adjacent to the biomaterials in the majority of samples. Both CEM cement and ProRoot MTA demonstrated similar periradicular tissue responses, with no significant differences [176]. This suggests that CEM cement has the potential to induce cementum formation in the periradicular region similar to MTA.
Repair of furcal perforation: Another study focused on the repair of furcal perforation using CEM cement and compared it to ProRoot MTA. Both biomaterials resulted in the formation of hard tissue, indicating successful repair. The inflammatory response observed in the experimental groups was mild, and there were no significant differences between CEM cement and ProRoot MTA [177]. These findings indicate that CEM cement is effective in inducing cementogenesis and promoting the repair of furcal perforations, comparable to ProRoot MTA.
Overall, these studies highlight the ability of CEM cement to promote the deposition of cementum and facilitate the repair of perforations, suggesting its potential for inducing cementogenesis in endodontic procedures.
Clinical applications and treatment outcomes
Endodontic literature has revealed various clinical applications for CEM cement (Fig. 2). In this part, the name of the author(s) as well as the first work/time of utilizing a treatment using CEM cement is mentioned. In addition, the success rates and level of evidence until now will be provided.
Vital pulp therapy
VPT is a conservative approach that aims to preserve the vitality and functionality of the dental pulp in cases of pulp exposure even with irreversible pulpitis (IP) [178]. CEM cement has emerged as a promising biomaterial for VPT, offering favorable biocompatibility and dentinogenic potential. Several reviews and meta-analyses have explored the clinical applications and effectiveness of CEM cement in VPT procedures in primary and permanent teeth with/without IP or apical periodontitis (AP) [4, 179,180,181,182].
Indirect pulp capping
Permanent teeth: Indirect pulp capping (IDPC) utilizing CEM cement was first introduced by Torabzadeh and Asgary in 2013 with Level V evidence supporting its efficacy [183]. In their case report, IDPC with CEM cement was performed on a mature molar with symptomatic IP and AP. After a 1-year follow-up period, the tooth exhibited pulp vitality, normal clinical function, and the absence of pain, tenderness to percussion/palpation, and cold sensitivity. Radiographic examination revealed healing of the periradicular lesion with the formation of new bone, indicating successful treatment outcomes. This case report highlights the effectiveness of IDPC with CEM cement in preserving pulp vitality and promoting periradicular healing.
Moreover, a Level I evidence study conducted in 2018 further supports the effectiveness of IDPC and reported a 100% success rate at 1-year recall [184].
Direct pulp capping
Permanent teeth: The use of CEM cement for direct pulp capping (DPC) was first reported in a case report by Asgary et al. in 2012, providing Level V evidence [185]. In this case report, CEM cement was used for the DPC of a mature molar with symptomatic IP and symptomatic AP. The treatment resulted in successful periapical healing, with the tooth exhibiting normal function, absence of pain, and a normal response to cold testing during follow-ups of up to 15 months. Additionally, a Level I evidence study conducted in 2018 further supports the effectiveness of DPC with CEM cement and reported a 94.7% success rate at 1-year recall [184].
Primary teeth: In a randomized clinical trial conducted by Fallahinejad Ghajari et al. in 2010 (Level I evidence), the outcomes of DPC using CEM cement and ProRoot MTA in primary molar teeth were compared [186]. The trial, using a split-mouth design, demonstrated a high success rate of 94.8% for CEM cement and 100% for ProRoot MTA, with no failures observed on radiographic evaluations at the 6-month follow-up. Subsequent evaluations after 20 months revealed a final success rate of 89% in the CEM cement group and 95% in the ProRoot MTA group, with no statistically significant difference [187]. These results indicate that both CEM cement and ProRoot MTA are effective options for DPC in primary molars. Furthermore, a recent systematic review has provided additional support for the effectiveness of both biomaterials in DPC procedures [188].
Miniature pulpotomy
The concept of miniature pulpotomy (MP) was introduced in a hypothesis article by Asgary and Ahmadyar in 2012, proposing that performing an MP could improve the outcomes of VPT for cariously exposed pulp [189]. The hypothesis was based on biological principles, including creating a clean surgical wound in the pulp, removing infected dentin chips and damaged pulp tissue, controlling bleeding, enhancing the interaction of pulp capping biomaterial with stem cells, and achieving a better seal.
Permanent teeth: The use of CEM cement in the management of complicated crown fractures with MP was described by Asgary and Fazlyab in 2014, providing Level V evidence [190]. At the 1-year follow-up, the treated tooth showed vitality, and radiographic examination revealed the presence of a thick dentinal bridge beneath the CEM cement layer, indicating successful treatment. Other case studies have also reported successful utilization of CEM cement for MP in symptomatic mature permanent teeth, both in immediate and delayed scenarios following pulp exposure [191, 192]. Furthermore, a Level I evidence study conducted in 2018 further supports the effectiveness of MP with CEM cement and reported a 91.4% success rate at 1-year recall [184].
Partial pulpotomy
Permanent teeth: The first reported utilization of partial pulpotomy (PP) treatment with CEM cement was described in a case report by Tavassoli-Hojjati et al. in 2013, providing Level V evidence [193]. The case report presented the management of an exposed pulp in an 8-year-old boy with incomplete root formation in a central incisor. PP was performed using CEM cement, and at the 1-year follow-up, the tooth exhibited a normal response to cold and electric pulp tests, with radiographic examination showing normal closure of the root apex.
A recent clinical trial conducted in 2021 compared the effectiveness of PP using various biomaterials, including CEM cement, in cases of symptomatic IP, providing Level II evidence [194]. The study found no statistically significant differences in the frequencies of clinical and radiographic outcomes among the different biomaterials at various periods up to 1 year. This indicates that CEM cement is a viable option for PP treatment in cases of symptomatic IP.
Coronal pulpotomy
Permanent teeth: The use of coronal pulpotomy (CP) with CEM cement in permanent teeth with IP has been extensively studied. In 2009, Asgary and Ehsani published the first case series on FP with CEM cement, providing Level IV evidence [11]. Positive clinical and radiographic outcomes were reported, with all treated teeth showing normal function and the absence of signs and symptoms during the follow-up period. Histological examination confirmed the formation of complete dentin bridges and the presence of a healthy pulp. Subsequent studies have further supported the effectiveness of CP with CEM cement in managing IP and AP with condensing osteitis, as well as serving as an alternative to tooth extraction in molars with hyperplastic IP [195, 196].
Long-term assessments using micro-computed tomography (Micro CT) have demonstrated complete dentinal bridge formation without negative consequences on the dental pulp, such as pulp canal obliteration or calcification [197]. CP with CEM cement has also shown success in managing pink spots due to internal/external cervical root resorption, restoring aesthetics, and preventing further resorption [198]. Case studies have demonstrated the stability of pulpotomy-treated molars despite recurrent decay, with the formation of complete calcified bridges at the canal orifices [199].
Two multi-center randomized-controlled trials have compared the pain relief effect of CP in mature teeth with clinical signs and symptoms of IP. In one trial, CP using CEM cement was compared to RCT [200]. The results showed a significant difference in the change in mean pain intensity between the two groups, with the CEM group experiencing faster pain relief (18 h) compared to the RCT group (36 h). Additionally, patients in the CEM group had lower pain intensity scores and less pain in response to percussion tests. Another randomized-controlled trial compared post-endodontic pain following CP or RCT in mature teeth with carious pulp exposure [201]. The study found comparable mean pain intensity scores and trends of pain relief among the different treatment groups. Furthermore, the incidences of preoperative moderate–severe pain significantly decreased after 24 h in all groups.
Randomized-controlled trials have evaluated the treatment outcomes of CP in mature permanent molars with IP using CEM cement or ProRoot MTA. Both ProRoot MTA and CEM groups showed high clinical success rates (98% and 97%) and radiographic success rates (95% and 92%) at the 12-month follow-up [202]. Long-term follow-up studies demonstrated clinical success rates > 98% and radiographic success rates of 84% for ProRoot MTA and 78% for CEM at the 5-year mark [203].
In a serial multicenter randomized clinical trial comparing RCT with CP using CEM cement, both treatment groups showed comparable clinical success rates of ≥ 97%. However, the radiographic success rate was significantly higher in the CEM group at the 1-year follow-up (92% vs. 81%) [204]. At the 2-year follow-up, both groups had equal clinical success rates (98%), but the radiographic success rates were 79% for RCT and 86% for CEM, with no statistical difference [205]. Long-term follow-up studies of 5 years also demonstrated the non-inferiority and long-term success of CP using CEM compared to RCT in mature permanent molars, with success rates of 78% and 75% for CEM and RCT groups, respectively [206]. Furthermore, in a randomized clinical trial, CEM and ProRoot MTA full pulpotomy were compared in young permanent molars with IP [207]. The study found no significant difference between the two groups in terms of clinical and radiographic outcomes over 12 months. Both treatments showed excellent success rates.
In a recent randomized-controlled trial comparing RCT or CP using ProRoot MTA or CEM cement, no significant differences in the success rates were found between the treatment groups [208]. The 2-year radiographic success rates were 98% for RCT, 100% for ProRoot MTA, and 98% for CEM full pulpotomy, without statistically significant differences.
These studies collectively provide Level I evidence for the effectiveness of CP with CEM cement in managing IP in permanent teeth, with comparable outcomes to the traditional RCT.
Primary teeth: In primary molars, the effectiveness of CP with CEM cement has been extensively studied. A randomized clinical trial by Malekafzali et al. in 2011 provided Level I evidence comparing CP outcomes using CEM cement and ProRoot MTA [209]. The study found similar clinical and radiographic outcomes between the two biomaterials, indicating that CEM cement is an effective pulp dressing material for CP in primary molars. Several other randomized clinical trials with Level I evidence have compared CP using CEM cement with other techniques and materials, including ProRoot MTA, formocresol, sodium hypochlorite, ferric sulfate, and low-level laser therapy, and have consistently reported high radiographic success rates ranging from 95 to 100% [209,210,211,212,213].
In cases of IP in primary molars, the use of CEM cement for CP has shown promising results. A clinical trial investigating CP using CEM cement reported a high success rate and significant pain relief in the majority of children after treatment, with a radiographic success rate of 90.4% observed at the 1-year recall [214]. Additionally, tampon-based CP using CEM cement has demonstrated reliability in the treatment of vital primary molars with IP, leading to successful outcomes in multiple cases [215, 216].
These studies provide strong evidence for the effectiveness of CP with CEM cement in managing primary molars with IP, with comparable outcomes to other techniques and materials. CEM cement serves as a reliable and successful treatment option for preserving the vitality and functionality of primary molars.
Partial pulpectomy
In partial pulpectomy (PPC), the procedure involves the removal of dental pulp from the coronal third of the roots, followed by the placement of capping material to protect the remaining pulp. CEM cement has shown promising results. The first published work utilizing CEM cement in PPC was a case report by Asgary and Çalışkan in 2015 (Level V evidence) [217]. The case report described the successful treatment of a mature mandibular first molar with hyperplastic pulpitis, internal root resorption, and periradicular periodontitis. After 6 months, a radiographic examination revealed complete healing, and the tooth remained functional without any signs or symptoms of infection or inflammation.
Although more research is needed to establish the effectiveness of CEM cement in PPC, this case report demonstrates its potential as a viable option for managing cases requiring partial removal of pulp. CEM cement offers biocompatibility and dentinogenic properties that contribute to successful healing and preservation of tooth functionality. Further studies and clinical trials are warranted to explore the efficacy of CEM cement in PPC and compare its outcomes with other treatment approaches.
Comparing VPTs
Comparative studies play a crucial role in evaluating and comparing the effectiveness of different VPT techniques. Two studies have provided insights into the comparison of various VPT techniques using CEM cement. In a comprehensive case series, the treatment outcomes of 94 permanent teeth with IP were evaluated using different VPT techniques, including IDPC, DPC, MP, and CP with CEM cement (Level IV evidence) [218]. The study reported a high success rate across all techniques, with 93 teeth demonstrating both radiographic and clinical success. Only one radiographic failure was observed in the DPC group. This case series highlights the favorable treatment outcomes of different VPT techniques utilizing CEM cement in managing IP in permanent teeth.
A randomized clinical trial with Level I evidence compared the treatment outcomes of four VPT techniques (IDPC, DPC, MP, and CP) in mature molars [184]. The study evaluated the success rates at 3 and 12 months and found that all four techniques had comparable success rates of over 91%, with no significant differences observed. The study concluded that these VPT techniques using CEM cement were associated with favorable and comparable clinical and radiographic outcomes. Factors such as pulpal and periapical status, as well as the type and location of pulpal exposure, did not significantly impact the treatment outcomes.
These studies provide valuable evidence supporting the effectiveness of different VPT techniques utilizing CEM cement. However, further research, including larger clinical trials and longer term follow-ups, is necessary to strengthen the evidence and determine the optimal VPT approach for different clinical scenarios.
Health technology assessment
Yazdani et al. conducted a health technology assessment (HTA) to evaluate the use of VPT with CEM cement compared to RCT in permanent molars with IP [219]. The study aimed to assess various factors including patient-related factors, safety, and organizational considerations, as well as the impact on reducing the burden of disease.
Patient-related factors were evaluated based on short- and long-term clinical success. The study found that VPT with CEM cement was more successful in treating IP compared to RCT. Safety factors were assessed by a specialist committee and discussion board, which concluded that VPT with CEM cement was a safe and reliable treatment option.
The organizational evaluation included cost, availability, accessibility, and acceptability. VPT with CEM cement was found to be more accessible, affordable, and available compared to RCT. Additionally, it was deemed acceptable by patients and healthcare providers.
The study also investigated the impact of VPT with CEM cement on reducing the burden of disease. It highlighted the potential benefits of VPT in preserving natural teeth, avoiding unnecessary extractions, and improving oral health-related quality of life.
Overall, the HTA concluded that VPT with CEM cement was a feasible and effective alternative to RCT in mature permanent molars with IP. It emphasized the potential advantages of VPT/CEM in terms of improved clinical outcomes, patient satisfaction, cost-effectiveness, and the overall burden of disease.
This HTA provides valuable insights into the advantages of VPT with CEM cement and supports its consideration as a preferred treatment modality for IP in permanent molars. However, it is important to note that further research and evidence are necessary to validate and expand upon these findings.
Management of open apices
Apexogenesis
In 2010, Nosrat and Asgary published a case report describing successful apexogenesis using CEM cement in a traumatized tooth with long-lasting pulpal exposure (Level V evidence) [220]. The tooth, treated with a complete pulpotomy technique using CEM cement, showed functional status, complete root development, and the formation of a calcified bridge at the apex during follow-up examinations.
Several case studies have also investigated the use of CEM cement in complete pulpotomy techniques for teeth with open apices, reporting successful outcomes, such as continued root development, resolution of symptoms, and radiographic evidence of healing [221,222,223,224]. Although these studies have Level V evidence, they collectively support the efficacy of CEM cement in apexogenesis procedures.
In a randomized clinical trial (Level I evidence), the outcomes of pulpotomy using CEM cement and ProRoot MTA were compared in immature caries-exposed permanent molars [207]. The study found no significant difference in pulp survival and signs of ongoing root development between the two materials. Both CEM cement and ProRoot MTA demonstrated comparable radiographic outcomes, with apexogenesis observed in 76.8% and 73.8% of radiographically evaluated roots in the CEM cement and ProRoot MTA groups, respectively.
Systematic reviews have also evaluated various endodontic medicaments, including CEM cement, for CP in immature permanent teeth. The evidence suggests similar success rates among these biomaterials, as well as other agents such as CH and platelet-rich fibrin [225, 226].
Collectively, these studies and systematic reviews provide valuable evidence supporting the use of CEM cement in apexogenesis procedures for teeth with open apices. However, further research with higher level evidence is necessary to establish standardized protocols and confirm the long-term success of apexogenesis using CEM cement.
Apexification (apical plug)
The effectiveness of CEM cement as an artificial apical plug in teeth with open apices and necrotic pulps was investigated in a study by Nosrat et al. (Level IV evidence) [227]. Thirteen single-rooted teeth were treated with CEM cement as an apical plug, either in the first or second appointment. The teeth were restored, and patients were followed up until radiographic evidence of periradicular healing was observed, with an average follow-up period of 14.5 months. The study demonstrated complete periradicular healing in all cases, indicating the efficacy of CEM cement as an apical plug.
Case reports have also showcased successful outcomes with the use of CEM cement in apexification procedures. In one case report, CEM cement was utilized for the apexification of a traumatized anterior tooth, resulting in positive outcomes during a 1-year follow-up [228]. Another case report described the conservative management of an unset MTA root-end filling using CEM cement, with successful outcomes observed during a 27-month follow-up [229]. Additionally, CEM cement was used as an apical plug in a mandibular premolar with dens invaginatus, leading to positive outcomes during a 36-month follow-up [230]. These case reports further demonstrate the versatility and efficacy of CEM cement in various endodontic treatments. Overall, the studies and case reports provide evidence supporting the effectiveness of CEM cement as an artificial apical plug-in teeth with open apices and necrotic pulps. However, further research with higher level evidence is needed to confirm these findings and establish standardized protocols for apexification procedures using CEM cement.
Revascularization (revitalization)
A study conducted by Nosrat et al. presented the cases of regenerative endodontic treatment (RET), also known as revitalization, in necrotic immature permanent molars (Level V evidence) [231]. The treatment approach involved irrigation with sodium hypochlorite (NaOCl), a triple antibiotic paste dressing, induction of bleeding, and placement of a CEM cement coronal plug. The treated teeth showed complete healing of periapical radiolucencies, continued root development, and remained asymptomatic and functional.
Another case study compared RET with apical plug in necrotic immature maxillary central incisors, demonstrating complete radiographic healing without tooth discoloration [232]. Furthermore, a study on modified revascularization using a treated dentin matrix showed successful outcomes and continued root development [233]. Similarly, a case report of RET and apical plugs in an immature molar resulted in symptom relief and successful management using CEM cement [234].
RET using CEM cement achieved the resolution of periapical radiolucency, apical closure, and positive responses to cold tests in a case of necrotic immature permanent anterior tooth [235]. Finally, a recent case report highlighted the resolution of endodontic lesions, dentinal bridge formation, and continuous root maturation in an infected immature tooth with a talon cusp following RET [236].
Endodontic surgery
Root-end surgery
The use of CEM cement in root-end surgery was first reported in a study by Asgary and Ehsani, where successful treatment outcomes were achieved in 13 out of 14 teeth with persistent apical periodontitis (Level IV evidence) [237]. This study provided the initial evidence of the effectiveness of CEM cement in root-end surgery. Subsequent case reports further demonstrated the successful use of CEM cement in various clinical scenarios.
One case report described the surgical management of a vertically fractured maxillary incisor, where the fracture line and retrograde cavity were treated with CEM cement [238]. Another case report highlighted the use of CEM cement as a root-end filling material in an infected immature incisor with severe root resorption and a large periradicular lesion [239]. Additionally, CEM cement was used to manage a failed overfilled MTA apical plug in a symptomatic open apex upper central incisor [240]. The limitations of CBCT in detecting a labial fiber post-perforation were demonstrated, leading to the importance of exploratory surgery using CEM [241]. These cases demonstrated the versatility of CEM cement in different surgical endodontic scenarios.
Further case reports emphasized the importance of accurate diagnosis and treatment planning in surgical endodontics [242]. Successful outcomes were reported in cases involving the management of large periapical cysts, progressive actinomycosis, symptomatic horizontal mid-root fractures, and therapy-resistant periapical actinomycosis using CEM cement [243,244,245]. Additionally, a case of partial necrosis resulting from the spread of infection from adjacent apical periodontitis was treated with surgical retreatment using CEM cement, leading to complete recovery [246].
These case reports collectively demonstrate the effectiveness of CEM cement in surgical endodontic treatments, highlighting its positive impact on healing, symptom relief, and restoration of tooth functionality [198]. The use of CEM cement in root-end surgery offers a viable treatment option for managing various endodontic challenges and improving patient outcomes. However, further research with higher level evidence, such as randomized-controlled trials, is needed to further evaluate the efficacy and long-term success of CEM cement in surgical endodontics.
Intentional replantation
The first reported utilization of intentional replantation (IR) with CEM cement was described in a case study by Asgary in 2011, demonstrating successful management of a mandibular molar with chronic AP and previous RCT (Level V evidence) [247]. Follow-up examinations showed no signs of infection or inflammation and complete periradicular healing. This case report provided initial evidence of the effectiveness of CEM cement in IR procedures.
A subsequent case series in 2014 further investigated the indications and case selection for IR in endodontics, involving 20 cases treated with IR using CEM cement for root-end filling (Level IV evidence) [248]. The success rate of IR with CEM cement was reported as 90% over a mean follow-up period of 15.5 months. This study demonstrated the favorable outcomes of IR with CEM cement in a larger cohort of patients.
Various case reports have since been published, highlighting the effectiveness of IR with CEM cement in managing specific endodontic complications. These cases include the successful treatment of external root resorption after orthodontic treatment [249], necrotic calcified teeth [250], maxillary molars [251], avulsed immature permanent teeth [252], apical actinomycosis [253], and teeth with multiple endodontic complications [254]. Additionally, CEM cement has been found to decelerate replacement resorption in replanted teeth [255].
These case reports collectively demonstrate the effectiveness of IR with CEM cement in managing a range of endodontic challenges and complications. The use of CEM cement in IR procedures offers a viable treatment option for selected cases where conventional endodontic therapy may not be feasible or successful. However, further research with higher level evidence, such as randomized-controlled trials, is needed to further evaluate the efficacy and long-term success of IR with CEM cement.
Autotransplantation
The first reported use of autogenous tooth transplantation (AT) with CEM cement was described in a case study by Asgary, in 2009, demonstrating successful transplantation of a fully developed mandibular third molar to replace a vertically root-fractured second molar (Level V evidence) [256]. The transplanted tooth was treated with CEM cement as a root-end filling, and clinical follow-up over 2 years showed no complications and normal functionality. This case report provided initial evidence of the effectiveness of CEM cement in AT procedures.
In another case report, AT using a maxillary third molar with closed roots was performed to replace a tooth with a perio-endo lesion [256]. CEM cement was used to fill the roots before transplantation, and the patient had no symptoms during the follow-up period, with radiographic evidence of bone regeneration and a healthy periodontal ligament.
These case reports demonstrate the successful utilization of AT with CEM cement in replacing damaged or compromised teeth. The use of CEM cement in AT procedures offers a promising approach to promote healing, root-end sealing, and long-term stability of transplanted teeth. However, further research, including larger clinical studies, is needed to evaluate the success rates and long-term outcomes of AT with CEM cement compared to other materials or techniques in autotransplantation procedures.
Other surgical applications
The study by Ghanbari et al. aimed to compare the efficacy of CEM cement and ProRoot MTA in the treatment of Class II furcation defects in human mandibular molars (Level IV evidence) [257]. In this study, 40 furcation defects in 16 patients with chronic periodontitis were treated using either CEM cement or ProRoot MTA. Various clinical parameters, including probing depth (PD), vertical and horizontal clinical attachment levels (VCAL and HCAL), open vertical and horizontal furcation depths (OVFD and OHFD), and gingival margin level (GML), were measured at baseline and 3- and 6-month follow-ups. The results of the study showed that both ProRoot MTA and CEM cement significantly reduced PD, VCAL, HCAL, OVFD, and OHFD at the re-entry surgery. This indicates that both materials were effective in improving the clinical parameters and reducing the furcation defects. Importantly, there were no statistically significant differences between the two treatment options in terms of soft- and hard-tissue parameters. This suggests that CEM cement can be a viable alternative to ProRoot MTA in the treatment of Class II furcation defects.
It is worth noting that more research is needed to further evaluate the long-term outcomes and comparative effectiveness of CEM cement and ProRoot MTA in various surgical applications beyond the specific study mentioned above.
Management of root resorptions/perforations
Root perforation repair
In a case report by Eghbal et al., the repair of a strip perforation using CEM cement was successful (Level V evidence) [258]. The patient had a mandibular molar with a history of RCT and experienced a procedural mishap resulting in a perforation. After 1 week of treatment with CEM cement, the patient's symptoms improved, and radiographic evaluation at the 1-year follow-up showed complete healing of the lesion with bone replacement.
Another case report demonstrated the non-surgical repair of an old perforation with pocket formation and oral communication [259]. Despite negative prognostic factors, such as perforations in the coronal third of the tooth and the presence of a radiolucent lesion, the tooth exhibited normal functionality, and probing depths remained within the normal range after 18 months of treatment.
Additionally, a case report discussed the surgical management of a failed internal root resorption (IRR) treatment and highlighted the use of retrograde CEM cement filling following the initial failed treatment with orthograde MTA [260]. This report provided insights into the treatment approach and demonstrated successful outcomes.
Furthermore, another recent case report described the successful management of an unrepairable root perforation resulting from IRR using CEM cement as the root perforation repair material [236]. This case report showcased the potential of CEM cement in addressing challenging root perforation cases.
These case reports collectively demonstrate the effectiveness of CEM cement in repairing root perforations and highlight its role as a valuable material in the management of various types of root perforations, including strip perforations, old perforations with pocket formation, and cases of failed IRR treatment.
Furcal perforation repair
In a case report by Asgary, the repair of a furcal perforation using CEM cement was described (Level V evidence) [261]. The case involved a mandibular first molar with a furcal perforation and accompanying furcal lesion. The treatment approach included RCT to address the infected pulp and the repair of the perforation using CEM cement. At the 24-month recall, the patient showed no evidence of periodontal breakdown, no symptoms, and complete healing of the furcal lesion.
Another case study reported the successful repair of an extensive furcation perforation in a mandibular molar using CEM cement [262]. The patient remained asymptomatic during the 1-year follow-up, indicating a favorable treatment outcome.
In a separate case report, the management and healing of a large furcal lesion were achieved using a novel combination of triple antibiotic paste and CEM cement [263]. This case report highlighted the potential of CEM cement in conjunction with antibiotics for the successful treatment of furcation perforations.
Furthermore, a recent systematic review and meta-analysis compared various materials used for iatrogenic perforation repair in primary molars and found that premixed bioceramics, Atelocollagen, and CEM cement demonstrated superior clinical success rates compared to MTA [264]. This suggests that CEM cement is a viable option for furcal perforation repair in primary molars.
These findings collectively demonstrate the effectiveness of CEM cement in repairing furcal perforations and highlight its potential as a reliable material for the management of such cases.
External root resorption
In the study by Asgary et al., the management of external root resorption (ERR) using CEM cement was investigated (Level V evidence) [265]. The case involved a patient with mobility of a replanted maxillary left central incisor and pain while chewing on the left central/lateral incisors. Radiographic examination revealed progressive inflammatory ERR in the left central incisor, as well as inadequate RCT. Both teeth were immature and had periapical radiolucencies. The treatment approach consisted of thorough irrigation of both teeth, followed by obturation with CEM cement. In the case of the central incisor, initial treatment with CH for 6 weeks was performed before the CEM cement obturation. Follow-up examinations were conducted for up to 40 months. The results demonstrated that the treated teeth remained functional with normal mobility, and the progression of the inflammatory ERR ceased. The resorptive lacunae were filled with newly formed bone, and complete healing of the periapical radiolucencies was observed.
Other case reports have also highlighted the successful management of external root resorption using antibiotics followed by root canal filling with CEM cement [266, 267]. These reports further support the efficacy of CEM cement in the treatment of external root resorption.
Overall, these findings suggest that CEM cement can be an effective treatment option for managing external root resorption, promoting healing, and preserving the functionality of the affected teeth.
Internal root resorption
The case report by Ramazani et al. presented a management approach for internal root resorption (IRR) (Level V evidence) [268]. The treatment plan involved a two-visit non-surgical approach, where CEM cement was utilized during the root canal treatment to address the internal root resorption. Follow-up evaluations conducted for 1 year demonstrated the complete resolution of the patient's signs and symptoms, along with radiographic evidence of complete healing.
In cases of internal root resorption in primary molars of endodontic origin, the traditional treatment approach involves tooth extraction and placement of a space maintainer. However, a study by Tavassoli-Hojjati et al. investigated a different method using CEM cement as a treatment option for three primary molars with extensive internal root resorption and associated furcal lesions (Level V evidence) [269]. The procedure involved accessing the pulp chambers, irrigating with sodium hypochlorite, and filling the cavities with CEM cement. Stainless steel crowns were placed to restore the teeth. Follow-up examinations were performed for up to 17 months. The study showed successful outcomes, as all treated teeth indicated complete bone healing in the affected areas, radiographically. These findings suggest that using CEM cement in the treatment of primary molars with extensive internal root resorption, even in the presence of furcal lesions, may provide a viable alternative to tooth extraction and space maintainer placement.
Overall, these studies demonstrate the efficacy of CEM cement in managing internal root resorption, highlighting its potential for successful resolution of the condition and preservation of affected teeth.
Combined external/internal root resorption
In the study by Asgary and Ahmadyar, the management of combined external and internal root resorptions (ERR/IRR) using CEM cement was investigated (Level V evidence) [270]. Radiographic examination revealed inadequate obturation of the root canals along with severe external and internal root resorptions and a large periradicular lesion. Nonsurgical endodontic retreatment was performed, involving the conventional chemomechanical debridement of the root canals. In the same session, the entire distal root canal was obturated using CEM cement, while the mesial canals were obturated with gutta-percha and sealer. The clinical findings and follow-up radiographs after 12 months showed favorable treatment outcomes, indicating the successful management of the combined external and internal root resorptions using CEM cement.
Another case report presented the management of merged external and internal root resorptions using CEM cement, further demonstrating the effectiveness of CEM cement in treating this challenging condition [271].
These findings suggest that CEM cement can be a suitable material for the management of combined external and internal root resorptions, providing favorable treatment outcomes and potential for successful resolution of these complex cases.
Invasive cervical root resorption
In the study by Asgary and Fazlyab, the management of invasive cervical root resorption (ICRR) in a mandibular canine using CEM cement was investigated (Level V evidence) [272]. The treatment approach involved the placement of CEM cement in the cavity after performing a full mucoperiosteal flap. One week later, CEM cement was polished and covered with composite resin. The 1-year follow-up showed a healthy pulp and a reduction in gingival probing depth, indicating improved attachment.
Another report discussed the conservative management of Class 4 ICRR using CEM cement, further emphasizing the effectiveness of the biomaterial in treating ICRR [273]. This case report demonstrated successful outcomes in managing ICRR with CEM cement.
Additionally, another case report described the intracanal management of a post-traumatic perforative ICRR using CEM cement [274]. The case showcased the successful use of CEM cement in managing the perforation and preserving the tooth structure in ICRR.
Furthermore, a case series by Asgary et al. presented the management of ICRR using VPT with CEM cement (Level IV evidence) [275]. The study included six teeth diagnosed with ICRR and having normal pulpal and periodontal status. Various VPT techniques, such as direct pulp capping (DPC), partial pulpotomy (PP), and partial pulpectomy, were selected based on the accessibility of the resorptive lacunae. The teeth were then restored, and follow-up evaluations were conducted. The results showed that all treated teeth remained functional and asymptomatic, with a healthy periodontium, during an average follow-up period of 19.6 months. No progression of the resorption or development of new resorption was observed.
These studies collectively demonstrate the effectiveness of CEM cement in the management of invasive cervical root resorption, offering promising outcomes and potential for preserving tooth structure and function.
Root canal/orifice obturation
In the study by Asgary and Eghbal, the use of CEM cement for root canal obturation in a mandibular molar with internal root resorption and an open apex was investigated (Level V evidence) [276]. The case report described a non-surgical retreatment procedure in which the root canal was cleaned, shaped, and obturated using CEM cement in combination with gutta-percha and sealer. After a follow-up period of 3 years, the tooth remained asymptomatic, and both clinical and radiographic assessments showed complete healing.
Other case reports have also highlighted the successful use of CEM cement in various clinical scenarios for root canal obturation. One case report focused on the management of infected primary molars using CEM cement, demonstrating positive treatment outcomes [277]. Another case report discussed the successful treatment of non-obturated canals using CEM cement, emphasizing its efficacy in such cases [278].
These reports collectively demonstrate the effectiveness of CEM cement as a root canal obturation material, showcasing its potential for achieving successful endodontic outcomes in different clinical situations.
As a sealer
This section explores the practical application of CEM cement, focusing on its innovative premixed bio-sealer variant, HealApex. While CEM cement is not recommended for use as a sealer, HealApex, derived from CEM powder, is specifically designed to function as an endodontic sealer, providing a unique perspective compared to the established AH-26 [279]. The investigation meticulously assessed crucial parameters such as setting time, working time, film thickness, flow, and radiopacity, adhering to ISO 6876 standards. Biocompatibility evaluations, conducted under ISO 10993-5 and utilizing L929 fibroblasts, yielded positive insights into the cytotoxicity profile of HealApex. Furthermore, the study scrutinized the favorable sealing ability of HealApex through a fluid filtration method spanning one month, revealing its performance in both short-term and long-term scenarios. These findings contribute to a deeper understanding of the practical implications of CEM-based bio-sealers, offering valuable information for optimizing endodontic treatments.
Merits and limitations of CEM cement
Merits
-
1.
Setting time: CEM cement has a relatively shorter setting time compared to ProRoot MTA, allowing for efficient and timely completion of endodontic procedures [7].
-
2.
Handling characteristics: CEM cement has a high percentage of small particles that enable easy manipulation and placement within the root canal system [62]. It adapts well to cavity walls, facilitating precise/effective application.
-
3.
Slight material expansion: CEM cement has been reported to undergo a very slight expansion during the setting process, which can contribute to its excellent sealing ability [7].
-
4.
Moisture resistance: CEM cement is hydrophilic, meaning that it can set and function effectively in the presence of moisture [12, 89]. This characteristic is advantageous in endodontic procedures where moisture control can be challenging, ensuring reliable performance in clinical situations.
-
5.
Sealing ability: CEM cement exhibits superior sealing properties, effectively preventing the microleakage of bacteria/toxins from the root canal system [87]. Its ability to form a tight seal with dentinal walls reduces the risk of reinfection.
-
6.
Alkalinity and calcium ion release: CEM cement's alkaline pH and sustained release of calcium ions offer several advantages [12]. Its alkaline environment inhibits bacterial growth and promotes antibacterial effects. The release of calcium ions facilitates remineralization, aiding in the formation of mineralized tissues and enhancing the overall healing process.
-
7.
Antibacterial properties: CEM cement demonstrates antibacterial effects against various microorganisms commonly associated with intracanal infections [120], enhancing the success rate of endodontic therapy.
-
8.
Reinforcement of tooth structure: CEM cement has been shown to reinforce weakened tooth structure, providing added strength and support to treated teeth [32]. This reinforcement can help prevent fractures and improve the long-term prognosis of the treated tooth.
-
9.
Bioactivity: CEM cement possesses bioactive properties, allowing it to interact with surrounding tissues and promote regeneration/repair of dental structures [11]. It stimulates the formation of new dentin, contributing to the healing process within the root canal system.
-
10.
Biocompatibility: CEM cement demonstrates excellent biocompatibility, making it well tolerated by tissues [143]. Its compatibility with the surrounding biological environment reduces the risk of adverse reactions or inflammation, promoting favorable healing outcomes.
-
11.
Dentinogenesis: CEM cement has the unique ability to stimulate dentin formation [164]. It supports the regeneration/healing of damaged dental tissues, promoting the structural integrity and functionality of the tooth.
-
12.
Versatile applications: CEM cement has versatile applications in endodontics, making it suitable for various procedures, such as root/furcal perforation repair [236], management of root resorptions [198], and obturation of root canals with open apices [232]. Its versatility simplifies treatment protocols and expands the range of clinical challenges it can effectively address.
-
13.
Long-term stability: CEM cement has demonstrated long-term stability in clinical studies, indicating its ability to maintain its sealing and biocompatible properties over time [280]. This long-term stability contributes to the durability and success of endodontic treatments.
-
14.
Cost: The cost of CEM cement is generally lower compared to other commonly used endodontic biomaterials, i.e., ProRoot MTA. This cost advantage makes CEM cement more accessible to a wider range of patients and facilitates its adoption in clinical practice, offering a cost-effective solution for endodontic treatments [219].
It is important to note that the advantages of CEM cement listed here are based on the available knowledge and understanding of the biomaterial up to the current date. Ongoing research and advancements may uncover additional benefits or further support the existing advantages of it.
Limitations and challenges
-
1.
Radiopacity: CEM cement exhibits a higher radiopacity at least twice that of dentin, but it has lower radiopacity compared to related ISO standards.
-
2.
Influence of environmental factors: The setting and properties of CEM cement may be affected by environmental factors such as severe blood contamination, which can impact its performance and clinical outcomes.
-
3.
Learning curve: Familiarity and experience with working with CEM cement are necessary to achieve consistent and predictable results. The learning curve associated with mastering the handling and placement techniques of CEM cement may initially pose a challenge for some practitioners.
-
4.
Limited long-term clinical data: Although CEM cement has shown promising results in various clinical trials and case reports, there is still a relatively limited amount of long-term clinical data available. Further long-term studies are needed to evaluate its performance and success rates over extended periods.
By addressing these challenges and limitations, and with ongoing research and advancements, the full potential of CEM cement as a valuable biomaterial in endodontics can be realized.
Future perspectives and research directions
Advances in CEM cement technology
Ongoing research is focused on enhancing the properties of CEM cement. Efforts are being made to improve its radiopacity, optimize handling characteristics, and refine the setting time. Additionally, researchers are exploring the incorporation of bioactive additives or nanoparticles to enhance their antibacterial properties and regenerative potential. These advancements in CEM cement technology will contribute to its overall performance and expand its applications in various endodontic procedures. Further investigations are crucial to unravel the underlying mechanisms causing discoloration in CEM cement, providing valuable insights that can guide future improvements in its formulation.
Clinical studies and outcomes
Further well-designed and long-term clinical studies are needed to strengthen the evidence base for CEM cement. Large-scale studies with extended follow-up periods will provide valuable insights into the long-term success and durability of CEM cement in different clinical scenarios. Comparative studies comparing CEM cement with other endodontic materials will help evaluate its performance and advantages in specific treatment modalities. Assessing patient-reported outcomes, such as pain, functionality, and satisfaction, will provide a comprehensive understanding of the patient-centered benefits of CEM cement.
Novel applications and modifications
As our understanding of CEM cement expands, there is potential for novel applications and modifications. Researchers are exploring innovative uses of CEM cement beyond the conventional endodontic procedures, such as VPT, regenerative endodontics, and periodontal applications. Modifying CEM cement formulations, such as incorporating growth factors or bioactive molecules, is being investigated to enhance its regenerative potential and expand its therapeutic applications. Exploring these novel applications and modifications will further optimize the clinical outcomes and expand the utility of CEM cement in diverse clinical scenarios.
Biocompatibility and safety studies
While CEM cement has demonstrated excellent biocompatibility, further research is needed to explore its long-term effects on periapical tissues and systemic health. Comprehensive studies evaluating cytotoxicity, immunogenicity, and potential adverse reactions associated with CEM cement are necessary. Additionally, investigations into its biodegradation and biocompatibility in various clinical scenarios, such as re-treatments, will provide insights into its long-term safety and performance.
Conclusions
Summary of key findings
-
1.
CEM cement demonstrates excellent biocompatibility, promoting tissue healing.
-
2.
It exhibits bioactivity and sustained release of calcium/phosphate ions, contributing to hydroxyapatite formation and mineralized tissue regeneration.
-
3.
CEM cement demonstrates favorable sealing ability, contributing to the formation of an effective bioseal and preventing bacterial microleakage, thereby reducing the risk of reinfection.
-
4.
It possesses antibacterial and anti-fungal properties, aiding in infections control.
-
5.
CEM cement stimulates dentinogenesis/cementogenesis, promoting the formation of dentin bridges and cementum.
-
6.
It has good handling characteristics, making it easy to manipulate/place in clinical settings.
-
7.
CEM cement is versatile and can be used in various endodontic procedures.
-
8.
It has shown successful outcomes in VPTs and preserving pulpal vitality.
-
9.
CEM cement is cost-effective, providing an affordable option for endodontic treatment.
-
10.
It is compatible with other dental materials, allowing for successful integration with restorative/prosthetic treatments.
Implications for clinical practice
The use of CEM cement in endodontics has important implications for clinical practice. Clinicians can benefit from its excellent sealing ability, biocompatibility, and antibacterial properties, which contribute to the success of endodontic treatments. CEM cement's regenerative potential makes it particularly suitable for cases involving large periapical lesions, apexification, and root-end filling. Its versatility allows for simplified treatment protocols and effective management of various clinical situations. Clinicians should ensure proper operator experience and training with CEM cement's handling characteristics to achieve optimal results in clinical practice.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Kabbinale P, Chethena K, Kuttappa M. Role of calcium-enriched mixture in endodontics. Arch Med Health Sci. 2015;3(1):80–4.
Utneja S, Nawal RR, Talwar S, Verma M. Current perspectives of bio-ceramic technology in endodontics: calcium enriched mixture cement—review of its composition, properties and applications. Restor Dent Endod. 2015;40(1):1–13.
Parirokh M, Torabinejad M, Dummer P. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part I: vital pulp therapy. Int Endod J. 2018;51(2):177–205.
Asgary S, Ahmadyar M. Vital pulp therapy using calcium-enriched mixture: an evidence-based review. J Conserv Dent. 2013;16(2):92–8.
Bali P, Shivekshith A, Allamaprabhu C, Vivek H. Calcium enriched mixture cement: a review. Int J Contemp Dent Med Rev. 2014;2014:1–13.
Dawood AE, Parashos P, Wong RHK, Reynolds EC, Manton DJ. Calcium silicate-based cements: composition, properties, and clinical applications. J Investig Clin Dent. 2017. https://doi.org/10.1111/jicd.12195.
Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S. The properties of a new endodontic material. J Endod. 2008;34(8):990–3.
Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J, Kheirieh S, Brink F. Comparison of mineral trioxide aggregate’s composition with Portland cements and a new endodontic cement. J Endod. 2009;35(2):243–50.
O'Brien W. Dental materials and their selection. Quintessence Int. 2002.
Raghavendra SS, Jadhav GR, Gathani KM, Kotadia P. Bioceramics in endodontics—a review. J Istanb Univ Fac Dent. 2017;51(3 Suppl 1):S128.
Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J. 2009;35(3):147–52.
Ghazvini SA, Tabrizi MA, Kobarfard F, Baghban AA, Asgary S. Ion release and pH of a new endodontic cement, MTA and Portland cement. Iran Endod J. 2009;4(2):74.
Sahebi S, Sadatshojaee N, Jafari Z. Effect of different mixing and placement methods on the compressive strength of calcium-enriched mixture. Iran Endod J. 2015;10(2):104–6.
Shahi S, Ghasemi N, Rahimi S, Yavari HR, Samiei M, Janani M, Bahari M. The effect of different mixing methods on the pH and solubility of mineral trioxide aggregate and calcium-enriched mixture. Iran Endod J. 2015;10(2):140–3.
Sahebi S, Sobhnamayan F, Naghizade S. The effects of various endodontic irrigants on the push-out bond strength of calcium-enriched mixture cement and mineral trioxide aggregate. Iran Endod J. 2016;11(4):280–5.
Reyhani MF, Ghasemi N, Zand V, Mosavizadeh S. Effects of different powder to liquid ratios on the push out bond strength of CEM cement on simulated perforations in the furcal area. J Clini Exp Dent. 2017;9(6):e785–8.
Shojaee NS, Adl A, Sobhnamayan F, Vasei F. The effect of various mixing techniques on the push-out bond strength of calcium enriched mixture. J Dent (Shiraz, Iran). 2016;17(2):128–33.
Shojaee NS, Adl A, Jafarpour D, Sobhnamayan F. Effect of different water-to-powder ratios on the solubility and microhardness of calcium-enriched mixture cement. Iran Endod J. 2019;14(3):185.
Forough Reyhani M, Hosseinian Ahangarnezhad S, Ghasemi N, Salem MA. Effects of various liquid-to-powder ratios on the compressive strength of calcium enriched mixture. J Dent Res Dent Clin Dent Prospects. 2021;15(2):129–32.
Samiei M, Shirazi S, Azar FP, Fathifar Z, Ghojazadeh M, Alipour M. The effect of different mixing methods on the properties of calcium-enriched mixture cement: a systematic review of in vitro studies. Iran Endod J. 2019;14(4):240.
Adl A, Shojaee NS, Sobhnamayan F, Hashemzade M. The effect of blood contamination on the compressive strength of calcium-enriched mixture. J Dent (Shiraz, Iran). 2015;16(1):37–41.
Shojaee NS, Adl A, Sobhnamayan F, Khademi A, Hamedi M. In Vitro evaluation of different solvents for retrieval of mineral trioxide aggregate and calcium-enriched mixture. Iran Endod J. 2016;11(3):223–7.
Ashofteh Yazdi K, Bolhari B, Sabetmoghaddam T, Meraji N, Kharazifard MJ. Effect of blood exposure on push-out bond strength of four calcium silicate based cements. Iran Endod J. 2017;12(2):196–200.
Samiei M, Janani M, Vahdati A, Alemzadeh Y, Bahari M. Scanning electron microscopy and energy-dispersive X-ray microanalysis of set CEM cement after application of different bleaching agents. Iran Endod J. 2017;12(2):191–5.
Kazemipoor M, Sanati E. Surface microstructure of two bioceramics: calcium-enriched mixture and cold ceramic in setting environments with different ph values. Int J Dent. 2023. https://doi.org/10.1155/2023/7130619.
Ashofteh Yazdi K, Ghabraei S, Bolhari B, Kafili M, Meraji N, Nekoofar MH, Dummer PMH. Microstructure and chemical analysis of four calcium silicate-based cements in different environmental conditions. Clin Oral Invest. 2019;23(1):43–52.
Mohebbi P, Asgary S. Effect of pH on physical properties of two endodontic biomaterials. J Conserv Dent. 2016;19(3):212.
Kayahan MB, Nekoofar MH, McCann A, Sunay H, Kaptan RF, Meraji N, Dummer PM. Effect of acid etching procedures on the compressive strength of 4 calcium silicate-based endodontic cements. J Endod. 2013;39(12):1646–8.
Sobhnamayan F, Adl A, Sadat Shojaee N, Sedigh-Shams M, Zarghami E. Compressive strength of mineral trioxide aggregate and calcium-enriched mixture cement mixed with propylene glycol. Iran Endod J. 2017;12(4):493–6.
Moehaddam N, Jokandan ME, Nouri-Vaskeh M, Milani AS. Comparison of flexural strength of mineral trioxide aggregate, calcium-enriched mixture and bioaggregate. Iran Endod J. 2018;13(4):554–8.
Sahebi S, Nabavizadeh M, Dolatkhah V, Jamshidi D. Short term effect of calcium hydroxide, mineral trioxide aggregate and calcium-enriched mixture cement on the strength of bovine root dentin. Iran Endod J. 2012;7(2):68–73.
Moazami F, Sahebi S, Jamshidi D, Alavi A. The long-term effect of calcium hydroxide, calcium-enriched mixture cement and mineral trioxide aggregate on dentin strength. Iran Endod J. 2014;9(3):185–9.
Shokouhinejad N, Razmi H, Fekrazad R, Asgary S, Neshati A, Assadian H, Kheirieh S. Push-out bond strength of two root-end filling materials in root-end cavities prepared by Er, Cr: YSGG laser or ultrasonic technique. Aust Endod J. 2012;38(3):113–7.
Lotfi M, Ghasemi N, Rahimi S, Bahari M, Vosoughhosseini S, Saghiri MA, Zand V. Effect of smear layer on the push-out bond strength of two endodontic biomaterials to radicular dentin. Iran Endod J. 2013;9(1):41–4.
Ertas H, Kucukyilmaz E, Ok E, Uysal B. Push-out bond strength of different mineral trioxide aggregates. Eur J Dent. 2014;8(3):348–52.
Sobhnamayan F, Adl A, Sarbaz M, Sadat Shojaee N, Abhari G. Push-out bond strength of calcium enriched mixture exposed to alkaline environment. J Dent Biomater. 2015;2(3):92–6.
Ghasemi N, Reyhani MF, Milani AS, Mokhtari H, Khoshmanzar F. Effect of calcium hydroxide on the push-out bond strength of endodontic biomaterials in simulated furcation perforations. Iran Endod J. 2016;11(2):91–5.
Shokouhi MM, Abbaszadegan A, Ameri A, Sharifian SM, Nabavizadeh M. The effect of calcium chloride on push-out bond strength of calcium-enriched mixture cement and mineral trioxide aggregate. Iran Endod J. 2017;12(3):334–7.
Mohammadian F, Soufi S, Dibaji F, Sarraf P, Chiniforush N, Kharrazifard MJ. Push-out bond strength of calcium-silicate cements following Er:YAG and diode laser irradiation of root dentin. Lasers Med Sci. 2019;34(1):201–7.
Ghasemi N, Yavari H, Samiei M, Aminabadi NA, Tabriz FD, Taheri S, Davoudi P. Effect of three intracanal medicaments used in pulp regeneration on the push-out bond strength of mineral trioxide aggregate and calcium-enriched mixture: an in vitro study. J Dent Res Dent Clin Dent Prospects. 2022;16(1):40.
Datta G, Raghu R, Shetty A, Manjunath GP, Patel D, Rajasekhara S. An in vitro comparative evaluation of the effect of three intracanal medicaments–chlorhexidine gel, triple antibiotic paste, and calcium hydroxide paste on the push-out bond strength of MTA Plus, biodentine, and calcium-enriched mixture. Endodontology. 2023;35(1):60–4.
Bahadır HS, Türkyilmaz A, Bayraktar Y, Çelik Ç. Effect of laser-assisted retrograde cavity preparation on push-out-bond-strength of mineral trioxide aggregate and calcium-enriched-mixture-cement. Braz Dent Sci. 2022. https://doi.org/10.14295/bds.2022.e2736.
Darvish A, Amin M, Aboutorabi FHS, Aflaki S, Davoodi NS, Ghaffari A, Khodadade M, Asgarian S, Katebi T. Push-out bond strength of retrograde root-end filling materials in extracted human teeth: calcium enriched mixture cement versus biodentine. EurAsia J BioSci. 2019;13(1):619–24.
Tavasoli R, Saeidi A, Mahmoudi E, Barijani N, Gholinia H. Comparison of the push-out bond strength between root mineral trioxide aggregate (MTA) and calcium-enriched mixture (CEM) cement. Caspian J Dent Res. 2020;9(2):57–62.
Sheykhrezae MS, Sohrabi K, Khosraviani F, Mohammadi S, Chiniforush N, Sarraf P. Push-out bond strength of two calcium silicate–based cements used for repair of artificial furcal perforation following different power outputs of Nd: YAG laser. Lasers Med Sci. 2022;37(9):3503–8.
Oskoee SS, Kimyai S, Bahari M, Motahari P, Eghbal MJ, Asgary S. Comparison of shear bond strength of calcium-enriched mixture cement and mineral trioxide aggregate to composite resin. J Contemp Dent Pract. 2011;12(6):457–62.
Elmi M, Ehsani M, Esmaeili B, Khafri S. Comparison of bond strength of a composite resin with two different adhesive systems and a resin modified glass ionomer to calcium enriched mixture. J Conserv Dent. 2018;21(4):369.
Ajami AA, Jafari Navimipour E, Savadi Oskoee S, Abed Kahnamoui M, Lotfi M, Daneshpooy M. Comparison of shear bond strength of resin-modified glass ionomer and composite resin to three pulp capping agents. J Dent Res Dent Clin Dent Prospects. 2013;7(3):164–8.
Oskoee SS, Bahari M, Kimyai S, Motahhari P, Eghbal MJ, Asgary S. Shear bond strength of calcium enriched mixture cement and mineral trioxide aggregate to composite resin with two different adhesive systems. J Dent (Tehran). 2014;11(6):665.
Altunsoy M, Tanriver M, Ok E, Kucukyilmaz E. Shear bond strength of a self-adhering flowable composite and a flowable base composite to mineral trioxide aggregate, calcium-enriched mixture cement, and biodentine. J Endod. 2015;41(10):1691–5.
Doozaneh M, Koohpeima F, Firouzmandi M, Abbassiyan F. Shear bond strength of self-adhering flowable composite and resin-modified glass ionomer to two pulp capping materials. Iran Endod J. 2017;12(1):103–7.
Koohpeima F, Sobhnamayan F, Esfandiari M, Siabani SJ. Comparison of shear bond strength of silorane and nanohybrid composite resins to calcium enriched mixture cement in different time periods. J Dent Biomater. 2018;5(2):559–66.
Jaberi-Ansari Z, Mahdilou M, Ahmadyar M, Asgary S. Bond strength of composite resin to pulp capping biomaterials after application of three different bonding systems. J Dent Res Dent Clin Dent Prospects. 2013;7(3):152.
Milani AS, Rahimi S, Borna Z, Jafarabadi MA, Bahari M, Deljavan AS. Fracture resistance of immature teeth filled with mineral trioxide aggregate or calcium-enriched mixture cement: an ex vivo study. Dent Res J. 2012;9(3):299–304.
Ok E, Altunsoy M, Tanriver M, Capar ID, Kalkan A, Gok T. Fracture resistance of simulated immature teeth after apexification with calcium silicate-based materials. Eur J Dent. 2016;10(2):188–92.
Madani ZS, Harandi A, Geraily E, Bijani A, Gharekhani S. Fracture strength of teeth restored with fiber post and apical plug. Caspian J Dent Res. 2017;6(2):15–22.
Bolhari B, Nekoofar MH, Sharifian M, Ghabrai S, Meraji N, Dummer PM. Acid and microhardness of mineral trioxide aggregate and mineral trioxide aggregate-like materials. J Endod. 2014;40(3):432–5.
Tabrizizadeh M, Dabbagh MM, Badrian H, Davoudi A. Microhardness properties of mineral trioxide aggregate and calcium-enriched mixture cement plugs at different setting conditions. J Int Oral Health. 2015;7(9):36–9.
Shahi S, Rahimi S, Yavari HR, Ghasemi N, Rezaie Y, Mirzapour S. Effect of the bone graft on the surface microhardness of endodontic biomaterials. Iran Endod J. 2018;13(2):200.
Kazemipoor M, Tamizi M. Influence of immediate coronal restoration on microhardness of CEM Cement: an in vitro study. Iran Endod J. 2018;13(4):540.
Ansari ZJ, Ghasemi A, Norozi H, Baghban AA, Samiei M. Microhardness of calcium-enriched mixture cement and covering glass ionomers after different time periods of application. Iran Endod J. 2022;17(2):67.
Soheilipour E, Kheirieh S, Madani M, Baghban AA, Asgary S. Particle size of a new endodontic cement compared to Root MTA and calcium hydroxide. Iran Endod J. 2009;4(3):112.
Torabzadeh H, Aslanzadeh S, Asgary S. Radiopacity of various dental biomaterials. Res J Biol Sci. 2012;7(4):152–8.
Emadi N, Safi Y, Bagheban AA, Asgary S. Comparison of CT-number and gray scale value of different dental materials and hard tissues in CT and CBCT. Iran Endod J. 2014;9(4):283.
Eghbal MJ, Torabzadeh H, Bagheban AA, Shamszadeh S, Marvasti LA, Asgary S. Color stability of mineral trioxide aggregate and calcium enriched mixture cement. J Investig Clin Dent. 2016;7(4):341–6.
Arman M, Khalilak Z, Rajabi M, Esnaashari E, Saati K. In vitro spectrophotometry of tooth discoloration induced by tooth-colored mineral trioxide aggregate and calcium-enriched mixture cement. Iran Endod J. 2015;10(4):226–30.
Esmaeili B, Alaghehmand H, Kordafshari T, Daryakenari G, Ehsani M, Bijani A. Coronal discoloration induced by calcium-enriched mixture, mineral trioxide aggregate and calcium hydroxide: a spectrophotometric analysis. Iran Endod J. 2016;11(1):23–8.
Rouhani A, Akbari M, Farhadi-Faz A. Comparison of tooth discoloration induced by calcium-enriched mixture and mineral trioxide aggregate. Iran Endod J. 2016;11(3):175–8.
Sobhnamayan F, Adl A, Ghanbaran S. Effect of different irrigation solutions on the colour stability of three calcium silicate-based materials. J Dent Biomater. 2017;4(2):373–8.
Madani Z, Alvandifar S, Bizhani A. Evaluation of tooth discoloration after treatment with mineral trioxide aggregate, calcium-enriched mixture, and Biodentine® in the presence and absence of blood. Dent Res J. 2019;16(6):377–83.
Khalilak Z, Esnaashari E, Saati K, Bineshmarvasti D, Yousefshahi H, Nobakht M. An in vitro comparison of coronal discolouration caused by white mineral trioxide aggregate, theracal, calcium-enriched mixture and biodentine. Eur Endod J. 2022;7(1):47–51.
Farhang R, Hekmatfar S, Samadi V, Meraji A, Jafari K. Comparison of tooth discoloration induced by calcium-enriched mixture, mineral trioxide aggregate, and endocem. World J Dent. 2020;11(5):392–5.
Araghi S, Khavid A, Godiny M, Saeidipour M. In vitro evaluation of coronal discoloration following the application of calcium-enriched mixture cement, Biodentine, and mineral trioxide aggregate in endodontically treated teeth. Dent Res J. 2019;16(1):53–9.
Jamshidifar A, Madani Z. Comparison of teeth discolorations induced by mineral trioxide aggregate, calcium-enriched mixture and Biodentine using spectrophotometric analysis. Caspian J Dent Res. 2019;8(1):37–42.
Adel M, Aflaki S, Eghbal MJ, Darvish A, Golshiri AM, Moradi Majd N, Reda R, Tofangchiha M, Zanza A, Testarelli L. Comparison of coronal discoloration induced by White MTA and CEM cement. J Compos Sci. 2022. https://doi.org/10.3390/jcs6120371.
Abbaszadegan A, Sedigh Shams M, Jamshidi Y, Parashos P, Bagheri R. Effect of calcium chloride on physical properties of calcium-enriched mixture cement. Aust Endod J. 2015;41(3):117–21.
Sobhnamayan F, Adl A, Sadat Shojaee N, Zarei Z, Emkani A. Physical and chemical properties of CEM cement mixed with propylene glycol. Iran Endod J. 2017;12(4):474–80.
Shahi S, Samiei M, Bahari M, Yavari H, Rahbar Mahvarian M. Effect of incorporating titanium dioxide nanoparticles into white portland cement, white mineral trioxide aggregate, and calcium enriched mixture cement on the push-out bond strength to furcal area dentin. J Dent (Shiraz). 2023;24(4):422–8.
Sobhnamayan F, Adl A, Farmani S, Shojaee NS. Effect of propylene glycol on the bond strength of two endodontic cements. Iran Endod J. 2019;14(1):52.
Zavare FJ, Nojehdehian H, Moezizadeh M, Daneshpooy M. Chemical modification of MTA and CEM cement to decrease setting time and improve bioactivity properties by adding alkaline salts. J Dent Res Dent Clin Dent Prospects. 2020;14(1):1.
Asgary S, Eghbal MJ, Parirokh M, Torabzadeh H. Sealing ability of three commercial mineral trioxide aggregates and an experimental root-end filling material. Iran Endod J. 2006;1(3):101.
Faramarzi F, Vossoghi M, Shams B, Vossoghi M. Comparison of pro root mineral trioxide aggregate and calcium enriched mixture cement microleakage as root end filling material: an in vitro analysis of dye penetration. Avicenna J Dent Res. 2015;7(2):2.
Ghorbani Z, Kheirieh S, Shadman B, Eghbal MJ, Asgary S. Microleakage of CEM cement in two different media. Iran Endod J. 2009;4(3):87.
Asgary S, Eghbal MJ, Parirokh M. Sealing ability of a novel endodontic cement as a root-end filling material. J Biomed Mater Res A. 2008;87(3):706–9.
Shahriari S, Faramarzi F, Alikhani MY, Farhadian M, Hendi SS. Apical sealing ability of mineral trioxide aggregate, intermediate restorative material and calcium enriched mixture cement: a bacterial leakage study. Iran Endod J. 2016;11(4):336–40.
Sadeghi S, Khoshdel M. In-vitro sealing ability of calcium enriched mixture cement versus amalgam as retrograde filling materials. J Dent Mater Tech. 2018;7(4):152–5.
Kazem M, Eghbal MJ, Asgary S. Comparison of bacterial and dye microleakage of different root-end filling materials. Iran Endod J. 2010;5(1):17.
Shahbaz S, Iftekhar H, Alam S, Mishra SK. Comparative evaluation of the apical leakage of different bioceramic retrofilling materials with and without smear layer: a stereomicroscopic study. Indian J Dent Res. 2022;33(1):46.
Hasheminia M, Nejad SL, Asgary S. Sealing ability of MTA and CEM cement as root-end fillings of human teeth in dry, saliva or blood-contaminated conditions. Iran Endod J. 2010;5(4):151.
Milani AS, Shakouie S, Borna Z, Deljavan AS, Jafarabadi MA, Azar FP. Evaluating the effect of resection on the sealing ability of MTA and CEM cement. Iran Endod J. 2012;7(3):134–8.
Rahimi S, Asgary S, Samiei M, Bahari M, Pakdel SMV, Mahmoudi R. The effect of thickness on the sealing ability of CEM cement as a root-end filling material. J Dent Res Dent Clin Dent Prospects. 2015;9(1):6.
Moradi S, Disfani R, Ghazvini K, Lomee M. Sealing ability of orthograde MTA and CEM cement in apically resected roots using bacterial leakage method. Iran Endod J. 2013;8(3):109–13.
Shahi S, Jeddi Khajeh S, Rahimi S, Yavari HR, Jafari F, Samiei M, Ghasemi N, Milani AS. Effect of different mixing methods on the bacterial microleakage of calcium-enriched mixture cement. Minerva Stomatol. 2016;65(5):269–75.
Küçükkaya Eren S, Görduysus MÖ, Şahin C. Sealing ability and adaptation of root-end filling materials in cavities prepared with different techniques. Microsc Res Tech. 2017;80(7):756–62.
Sahebi S, Moazami F, Sadat Shojaee N, Layeghneghad M. Comparison of MTA and CEM Cement microleakage in repairing furcal perforation, an in vitro study. J Dent (Shiraz, Iran). 2013;14(1):31–6.
Haghgoo R, Arfa S, Asgary S. Microleakage of CEM cement and ProRoot MTA as furcal perforation repair materials in primary teeth. Iran Endod J. 2013;8(4):187.
Haghgoo R, Niyakan M, Moghaddam KN, Asgary S, Mostafaloo N. An in vitro comparison of furcal perforation repaired with pro-root MTA and new endodontic cement in primary molar teeth—a microleakage study. J Dent (Shiraz, Iran). 2014;15(1):28.
Ramazani N, Sadeghi P. Bacterial leakage of mineral trioxide aggregate, calcium-enriched mixture and biodentine as furcation perforation repair materials in primary molars. Iran Endod J. 2016;11(3):214–8.
Ayatollahi F, Tabrizizadeh M, Hazeri Baqdad Abad M, Ayatollahi R, Zarebidoki F. Comparison of microleakage of MTA and CEM cement apical plugs in three different media. Iran Endod J. 2016;11(3):198–201.
Adel M, Nima MM, Shivaie Kojoori S, Norooz Oliaie H, Naghavi N, Asgary S. Comparison of endodontic biomaterials as apical barriers in simulated open apices. Res Notices IS. 2012. https://doi.org/10.5402/2012/359873.
Rahimi S, Ghasemi N, Razi T, Rezaiepour A. Quality of the calcium-enriched mixture apical plug in simulated apexification model; effect of different mixing and placement methods. J Clini Exp Dent. 2017;9(10):e1237–41.
Ayatollahi F, Zarebidoki F, Razavi SH, Tabrizizadeh M, Ayatollahi R, Heydarigujani M. Comparison of microleakage of CEM Cement apical plug in different powder/liquid ratio in immature teeth using fluid filtration technique. J Dent. 2019;20(1):37.
Mirhadi H, Moazzami F, Safarzade S. The effect of acidic pH on microleakage of mineral trioxide aggregate and calcium-enriched mixture apical plugs. Iran Endod J. 2014;9(4):257–60.
Adl A, Sobhnamayan F, Shojaee NS, Azad FT, Bahmani M. Effect of propylene glycol on the sealing ability of mineral trioxide aggregate and calcium-enriched mixture cement apical barriers. Iran Endod J. 2017;12(3):318–22.
Refaei P, Jahromi MZ, Moughari AAK. Comparison of the microleakage of mineral trioxide aggregate, calcium-enriched mixture cement, and Biodentine orthograde apical plug. Dent Res J. 2020;17(1):66–72.
Ayatollahi F, Hazeri Baqdad Abad M, Razavi SH, Tabrizizadeh M, Ayatollahi R, Zarebidoki F. Evaluating the accuracy of two microleakage assessment methods for mineral trioxide aggregate and calcium-enriched mixture cement. Iran Endod J. 2017;12(4):497–501.
Bidar M, Disfani R, Asgary S, Forghani M, Gharagozlo S, Rouhani A. Effect of calcium hydroxide premedication on the marginal adaptation of calcium-enriched mixture cement apical plug. Dent Res J. 2012;9(6):706.
Yavari HR, Samiei M, Shahi S, Aghazadeh M, Jafari F, Abdolrahimi M, Asgary S. Microleakage comparison of four dental materials as intra-orifice barriers in endodontically treated teeth. Iran Endod J. 2012;7(1):25.
Sadeghi S, Tabari R, Hosseini S. The effect of thickness on sealing ability of calcium enriched cement as a coronal seal barrier. J Dent Mater Tech. 2017;6(4):166–9.
Zarenejad N, Asgary S, Ramazani N, Haghshenas MR, Rafiei A, Ramazani M. Coronal microleakage of three different dental biomaterials as intra-orifice barrier during nonvital bleaching. Dent Res J. 2015;12(6):581.
Ramezanali F, Aryanezhad S, Mohammadian F, Dibaji F, Kharazifard MJ. In vitro microleakage of mineral trioxide aggregate, calcium-enriched mixture cement and biodentine intra-orifice barriers. Iran Endod J. 2017;12(2):211–5.
Moghadam N, Abdollahi AA, Aghabalayi Fakhim H, Borna Z. In vitro sealing properties of calcium-enriched mixture and mineral trioxide aggregate orifice barriers during intra-coronal bleaching. Iran Endod J. 2017;12(2):231–5.
Zarean P, Zarean P, Ravaghi A, Zare Jahromi M, Sadrameli M. Comparison of MTA, CEM cement, and Biodentine as coronal plug during internal bleaching: an in vitro study. Int J Dent. 2020;2020:1–8.
Zafar M, Iravani M, Eghbal MJ, Asgary S. Coronal and apical sealing ability of a new endodontic cement. Iran Endod J. 2009;4(1):15.
Samiei M, Aghazade M, Farhadi F, Shahveghar N, Torab A, Vahid Pakdel SM. Sealing efficacy of single-cone obturation technique with MTA and CEM cement: an in vitro bacterial leakage study. J Dent Res Dent Clin Dent Prospects. 2014;8(2):77–83.
Godiny M, Hatam R, Khavid A, Khanlari S. Apical microleakage in root canals containing broken rotary instruments. Iran Endod J. 2017;12(3):360–5.
Tabrizzadeh M, Mirshahpanah M. Effects of calcium chloride, as an additional accelerator substance, on marginal adaptation of calcium-enriched mixture cement to dentin. J Int Oral Health JIOH. 2016;8(3):324–7.
Saberi E, Bijari S, Dinarvand R. Scanning electron microscopic evaluation of the effect of different root-end resection methods in the crack formation in root canals filled with mineral trioxide aggregate or calcium-enriched mixture cement. Dent Res J. 2022;19(1):110.
Asgary S, Kamrani FA, Taheri S. Evaluation of antimicrobial effect of MTA, calcium hydroxide, and CEM cement. Iran Endod J. 2007;2(3):105.
Asgary S, Kamrani FA. Antibacterial effects of five different root canal sealing materials. J Oral Sci. 2008;50(4):469–74.
Zarrabi MH, Javidi M, Naderinasab M, Gharechahi M. Comparative evaluation of antimicrobial activity of three cements: new endodontic cement (NEC), mineral trioxide aggregate (MTA) and Portland. J Oral Sci. 2009;51(3):437–42.
Bidar M, Naderinasab M, Talati A, Ghazvini K, Asgari S, Hadizadeh B, Gharechahi M, Mashadi NA. The effects of different concentrations of chlorhexidine gluconate on the antimicrobial properties of mineral trioxide aggregate and calcium enrich mixture. Dent Res J. 2012;9(4):466.
Reyhani MF, Ghasemi N, Safaralizadeh M, Safaralizadeh S, Barhaghi MHS. Effect of adding chlorhexidine to calcium enriched mixture (CEM) on its antimicrobial activity. Afr J Microbiol Res. 2014;8(24):2393–6.
Razmi H, Aminsobhani M, Bolhari B, Shamshirgar F, Shahsavan S, Shamshiri AR. Calcium enriched mixture and mineral trioxide aggregate activities against enterococcus faecalis in presence of dentin. Iran Endod J. 2013;8(4):191–6.
Jonaidi-Jafari N, Izadi M, Javidi P. The effects of silver nanoparticles on antimicrobial activity of ProRoot Mineral Trioxide Aggregate (MTA) and calcium enriched mixture (CEM). J Clini Exp Dent. 2016;8(1):e22–6.
Nourzadeh M, Amini A, Fakoor F, Asgary S. Antimicrobial activity of calcium-enriched mixture cement and biodentine on Enterococcus faecalis: an in vitro study. Iran Endod J. 2019;14(1):18.
Esteki P, Jahromi M, Tahmourespour A. In vitro antimicrobial activity of mineral trioxide aggregate, Biodentine, and calcium-enriched mixture cement against Enterococcus faecalis, Streptococcus mutans, and Candida albicans using the agar diffusion technique. Dent Res J. 2021;18:3.
Ayatollahi F, Tabrizizadeh M, Tafti HS, Rashidian S, Sheibani AA. Evaluating the impact of concentration on anti-fungal property of CEM cement. Rev Latinoamericana Hipertensión. 2019;14(5):514–7.
Kangarlou A, Sofiabadi S, Yadegari Z, Asgary S. Antifungal effect of calcium enriched mixture cement against candida albicans. Iran Endod J. 2009;4(3):101.
Hosseinzade M, Soflou RK, Valian A, Nojehdehian H. Physicochemical properties of MTA, CEM, hydroxyapatite and nano hydroxyapatite-chitosan dental cements. Biomed Res. 2016;27(2):442–8.
Javid B, Panahandeh N, Torabzadeh H, Nazarian H, Parhizkar A, Asgary S. Bioactivity of endodontic biomaterials on dental pulp stem cells through dentin. Restor Dent Endod. 2020;45(1):e3.
Ghoddusi J, Tavakkol Afshari J, Donyavi Z, Brook A, Disfani R, Esmaeelzadeh M. Cytotoxic effect of a new endodontic cement and mineral trioxide aggregate on L929 line culture. Iran Endod J. 2008;3(2):17–23.
Mozayeni MA, Milani AS, Marvasti LA, Asgary S. Cytotoxicity of calcium enriched mixture cement compared with mineral trioxide aggregate and intermediate restorative material. Aust Endod J. 2012;38(2):70–5.
Khedmat S, Dehghan S, Hadjati J, Masoumi F, Nekoofar MH, Dummer PM. In vitro cytotoxicity of four calcium silicate-based endodontic cements on human monocytes, a colorimetric MTT assay. Restor Dent Endod. 2014;39(3):149–54.
Saberi EA, Karkehabadi H, Mollashahi NF. Cytotoxicity of various endodontic materials on stem cells of human apical papilla. Iran Endod J. 2016;11(1):17–22.
Küçükkaya S, Görduysus MÖ, Zeybek ND, Müftüoǧlu SF. In vitro cytotoxicity of calcium silicate-based endodontic cement as root-end filling materials. Scientifica. 2016. https://doi.org/10.1155/2016/9203932.
Eshagh AS, Farhadmollashahi N, Ghotbi F, Karkeabadi H, Havaei R. Cytotoxic effects of mineral trioxide aggregate, calcium enrichedmixture cement, Biodentine and octacalcium pohosphate onhuman gingival fibroblasts. J Dent Res Dent Clin Dent Prospects. 2016;10(2):75–80.
Mohamed DA, Abdelfattah MI, Aboulezz EHA. The effect of three different biomaterials on proliferation and viability of human dental pulp stem cells (in-vitro study). Open Access Maced J Med Sci. 2017;5(5):657–63.
Torshabi M, Amid R, Kadkhodazadeh M, Shahrbabaki S, Tabatabaei F. Cytotoxicity of two available mineral trioxide aggregate cements and a new formulation on human gingival fibroblasts. J Conserv Dent. 2016;19(6):522–6.
Karkehabadi H, Shahriari S, Najafi R, Khoshbin E, Abbaspourrokni H, Pakseresht Z. Effect of Emdogain coated endodontic materials on viability of human dental pulp stem cells (HDPSCs). Giornale Italiano di Endodonzia. 2019;33(2):35–42.
Esmaeilzadeh M, Moradkhani S, Daneshyar F, Arabestani MR, Asl SS, Tayebi S, Farhadian M. Antimicrobial and cytotoxic properties of calcium-enriched mixture cement, Iranian propolis, and propolis with herbal extracts in primary dental pulp stem cells. Restor Dent Endod. 2023. https://doi.org/10.5395/rde.2023.48.e2.
Zafari J, Karkehabadi H, Nikzad F, Esmailnasab S, Abbasi Javan Z, Javani JF. Combination of dental capping agents with low-level laser therapy increases the cell ciability percent of stem cells from Apical Papilla (SCAPs). J Lasers Med Sci. 2022;13: e58.
Asgary S, Moosavi SH, Yadegari Z, Shahriari S. Cytotoxic effect of MTA and CEM cement in human gingival fibroblast cells. Scanning electronic microscope evaluation. N Y State Dent J. 2012;78(2):51–4.
Amid R, Torshabi M, Tabari K, Kadkhodazadeh M, Eslami S, Ghazizadeh AM. Assessment of gingival fibroblast attachment to root surfaces restored with three different dental materials: an in vitro study. J Periodontol Implant Dent. 2016. https://doi.org/10.15171/jpid.2016.005.
Samiei M, Asgary S, Farajzadeh M, Bargahi N, Abdolrahimi M, Kananizadeh U, Dastmalchi S. Investigating the mutagenic effects of three commonly used pulpotomy agents using the ames test. Adv Pharm Bull. 2015;5(1):121.
Naghavi N, Ghoddusi J, Sadeghnia HR, Asadpour E, Asgary S. Genotoxicity and cytotoxicity of mineral trioxide aggregate and calcium enriched mixture cements on L929 mouse fibroblast cells. Dent Mater J. 2014;33(1):64–9.
Asgary S, Nazarian H, Khojasteh A, Shokouhinejad N. Gene expression and cytokine release during odontogenic differentiation of human dental pulp stem cells induced by 2 endodontic biomaterials. J Endod. 2014;40(3):387–92.
Assadian H, Khojasteh A, Ebrahimian Z, Ahmadinejad F, Boroojeni HSH, Bohlouli M, Nekoofar MH, Dummer P, Nokhbatolfoghahaei H. Comparative evaluation of the effects of three hydraulic calcium silicate cements on odontoblastic differentiation of human dental pulp stem cells: an in vitro study. J Appl Oral Sci. 2022. https://doi.org/10.1590/1678-7757-2022-0203.
Hajizadeh N, Madani ZS, Zabihi E, Golpour M, Zahedpasha A, Mohammadnia M. Effect of MTA and CEM on mineralization-associated gene expression in stem cells derived from apical papilla. Iran Endod J. 2018;13(1):94–101.
Omidi S, Bagheri M, Fazli M, Ahmadiankia N. Effects of two calcium silicate cements on transforming growth factor-β1 secretion from human dental pulp stem cells. Iran Endod J. 2018;13(4):522.
Omidi S, Bagheri M, Fazli M, Ahmadiankia N. The effect of different pulp-capping materials on proliferation, migration and cytokine secretion of human dental pulp stem cells. Iran J Basic Med Sci. 2020;23(6):768–75.
Mohamed DA, Fayyad DMJ. The effect of different bioactive materials on the odontogenic differentiation potential of dental pulp stem cells using two different culture mediums. Tanta Dent J. 2017;14(3):120.
Tabarsi B, Zabihi E, Mostafazadeh A, Fazli A, Marvasti LA, Asgary S. Cytokine release of two endodontic biomaterials. Res J Biol Sci. 2012;7:260–4.
Ghasemi N, Rahimi S, Lotfi M, Solaimanirad J, Shahi S, Shafaie H, Milani AS, Shakuie S, Zand V, Abdolrahimi M. Effect of mineral trioxide aggregate, calcium-enriched mixture cement and mineral trioxide aggregate with disodium hydrogen phosphate on BMP-2 production. Iran Endod J. 2014;9(3):220–4.
Hengameh A, Reyhaneh D, Nima MM, Hamed H. Effects of two bioactive materials on survival and osteoblastic differentiation of human mesenchymal stem cells. J Conserv Dent. 2014;17(4):349–53.
Rafatjou R, Amiri I, Janeshin A. Effect of calcium-enriched Mixture (CEM) cement on increasing mineralization in stem cells from the dental pulps of human exfoliated deciduous teeth. J Dent Res Dent Clin Dent Prospects. 2018;12(4):233.
Saberi E, Farhad-Mollashahi N, Sargolzaei Aval F, Saberi M. Proliferation, odontogenic/osteogenic differentiation, and cytokine production by human stem cells of the apical papilla induced by biomaterials: a comparative study. Clin Cosmet Investig Dent. 2019;11:181–93.
Khoshbin E, Ghasemi L, Najafi R, Karkehabadi H. Effects of CEM cement and emdogain on proliferation and differentiation of human stem cells from the apical papilla: a comparative in vitro study. Biotechnol Lett. 2023;45(1):69–81.
Abbasipour F, Akheshteh V, Rastqar A, Khalilkhani H, Asgary S, Janahmadi M. Comparing the effects of mineral trioxide aggregate and calcium enriched mixture on neuronal cells using an electrophysiological approach. Iran Endod J. 2012;7(2):79.
Parirokh M, Mirsoltani B, Raoof M, Tabrizchi H, Haghdoost AA. Comparative study of subcutaneous tissue responses to a novel root-end filling material and white and grey mineral trioxide aggregate. Int Endod J. 2011;44(4):283–9.
Rahimi S, Mokhtari H, Shahi S, Kazemi A, Asgary S, Eghbal MJ, Mesgariabbasi M, Mohajeri D. Osseous reaction to implantation of two endodontic cements: mineral trioxide aggregate (MTA) and calcium enriched mixture (CEM). Med Oral Patol Oral Cir Bucal. 2012;17(5): e907.
Tabarsi B, Pourghasem M, Moghaddamnia A, Shokravi M, Ehsani M, Ahmadyar M, Asgary S. Comparison of skin test reactivity of two endodontic biomaterials in rabbits. Pak J Biol Sci. 2012;15(5):250–4.
Shokravi M, Tabarsi B, Moghaddamnia A, Sohanfaraji A, Pourghasem M. Comparison of skin reaction between MTA (produced in Iran) and CEM in rabbit. Int J Mol Cell Med. 2012;1(2):94–8.
Asgary S, Parirokh M, Eghbal MJ, Ghoddusi J. SEM evaluation of pulp reaction to different pulp capping materials in dog’s teeth. Iran Endod J. 2006;1(4):117–23.
Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H. A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):609–14.
Madani ZS, Haddadi A, Mesgarani A, Seyedmajidi M, Mostafazadeh A, Bijani A, Ashraphpour M. Histopathologic responses of the dental pulp to calcium-enriched mixture (CEM) and mineral trioxide aggregate (MTA) in diabetic and non-diabetic rats. Int J Mol Cell Med. 2014;3(4):263–71.
Tabarsi B, Parirokh M, Eghbal M, Haghdoost A, Torabzadeh H, Asgary S. A comparative study of dental pulp response to several pulpotomy agents. Int Endod J. 2010;43(7):565–71.
Zarrabi MH, Javidi M, Jafarian AH, Joushan B. Histologic assessment of human pulp response to capping with mineral trioxide aggregate and a novel endodontic cement. J Endod. 2010;36(11):1778–81.
Zarrabi MH, Javidi M, Jafarian AH, Joushan B. Immunohistochemical expression of fibronectin and tenascin in human tooth pulp capped with mineral trioxide aggregate and a novel endodontic cement. J Endod. 2011;37(12):1613–8.
Hoseinifar R, Eskandarizadeh A, Parirokh M, Torabi M, Safarian F, Rahmanian E. Histological evaluation of human pulp response to direct pulp capping with MTA, CEM Cement, and Biodentine. J Dent (Shiraz, Iran). 2020;21(3):177.
Nosrat A, Peimani A, Asgary S. A preliminary report on histological outcome of pulpotomy with endodontic biomaterials vs calcium hydroxide. Restor Dent Endod. 2013;38(4):227–33.
Mehrdad L, Malekafzali B, Shekarchi F, Safi Y, Asgary S. Histological and CBCT evaluation of a pulpotomised primary molar using calcium enriched mixture cement. Eur Arch Paediatr Dent. 2013;14:191–4.
Haghgoo R, Asgary S, Abbas FM, Hedeshi RM. Nano-hydroxyapatite and calcium-enriched mixture for pulp capping of sound primary teeth: a randomized clinical trial. Iran Endod J. 2015;10(2):107.
Haghgoo R, Asgary S, Montazeri R. Histopathological evaluation of primary teeth after pulp capping with calcium-enriched mixture and bioactive glass. Iran Endod J. 2018;13(4):457.
Rasheed M, Asghar H, Sana U, Moazzam M, Malik F, Farooq A. Histological analysis of human pulp by comparing propolis, mineral trioxide aggregate and calcium enriched mixture as a direct pulp capping agent in primary molars. P J M H S. 2021;15(8):1864–6.
Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36(5):837–41.
Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S. Repair of furcal perforation using a new endodontic cement. Clin Oral Invest. 2010;14:653–8.
AAE Position Statement on Vital Pulp Therapy. J Endod. 2021;47(9):1340–4.
Asgary S, Ansari G, Tavassoli-Hojjati S, Shirazi AS, Parhizkar A. Clinical applications of hydraulic calcium silicate-based biomaterials in paediatric endodontics. Endod Pract Today. 2020;14(3):229–41.
Ghoddusi J, Forghani M, Parisay I. New approaches in vital pulp therapy in permanent teeth. Iran Endod J. 2014;9(1):15–22.
Liu Q, Meng N, Gu J, Yang Y, Dong Q. Research progress and meta-analysis of calcium enriched mixture for vital pulp therapy. J Contem Med Pract. 2022;4(7):151–5.
Silva E, Pinto KP, Belladonna FG, Ferreira CMA, Versiani MA, De-Deus G. Success rate of permanent teeth pulpotomy using bioactive materials: A systematic review and meta-analysis of randomized clinical trials. Int Endod J. 2023;56(9):1024–41.
Torabzadeh H, Asgary S. Indirect pulp therapy in a symptomatic mature molar using calcium enriched mixture cement. J Conserv Dent. 2013;16(1):83.
Asgary S, Hassanizadeh R, Torabzadeh H, Eghbal MJ. Treatment outcomes of 4 vital pulp therapies in mature molars. J Endod. 2018;44(4):529–35.
Asgary S, Nosrat A, Homayounfar N. Periapical healing after direct pulp capping with calcium-enriched mixture cement: a case report. Oper Dent. 2012;37(6):571–5.
Ghajari MF, Jeddi TA, Iri S, Asgary S. Direct pulp-capping with calcium enriched mixture in primary molar teeth: a randomized clinical trial. Iran Endod J. 2010;5(1):27.
Fallahinejad Ghajari M, Asgharian Jeddi T, Iri S, Asgary S. Treatment outcomes of primary molars direct pulp capping after 20 months: a randomized controlled trial. Iran Endod J. 2013;8(4):149–52.
Kulkarni P, Tiwari S, Agrawal N, Kumar A, Umarekar P, Bhargava S. Clinical outcome of direct pulp therapy in primary teeth: a systematic review and meta-analysis. J Indian Soc Pedod Prev Dent. 2022;40(2):105–11.
Asgary S, Ahmadyar M. Can miniature pulpotomy procedure improve treatment outcomes of direct pulp capping? Med Hypotheses. 2012;78(2):283–5.
Asgary S, Fazlyab M. Management of complicated crown fracture with miniature pulpotomy: a case report. Iran Endod J. 2014;9(3):233.
Asgary S, Nourzadeh M, Eghbal MJ. Miniature pulpotomy of symptomatic mature permanent teeth: a report of two cases. Iran Endod J. 2016;11(1):75.
Ramazani M, Asgary S. Delayed miniature pulpotomy in a symptomatic mature molar. Dent Rese J. 2018;15(4):302–5.
Tavassoli-Hojjati S, Ameli N, Zeinabadi MS. Partial pulpotomy using calcium-enriched mixture cement: a case report. Int J Dent Clin. 2013;5(4):29.
Al-Kazzaz A, Ashour H, Barakat S, Alkhouli M. Evaluate the effectiveness of vital pulp therapy using bioceramic endosequense root repair material (ERRM) compared to enriched mixture cement (CEM) in symptomatic mature permanent posterior teeth: clinical and radiographical study. Int J Dent Oral Sci. 2021;8(10):4758–63.
Asgary S. Calcium-enriched mixture pulpotomy of a human permanent molar with irreversible pulpitis and condensing apical periodontitis. J Conserv Dent. 2011;14(1):90–3.
Asgary S, Verma P, Nosrat A. Treatment outcomes of full pulpotomy as an alternative to tooth extraction in molars with hyperplastic/irreversible pulpitis: a case report. Iran Endod J. 2017;12(2):261.
Asgary S. Micro-computed tomography assessment of full pulpotomy in a mature molar after five years: a case report. Iran Endod J. 2022;17(4):223–4.
Asgary S. Management of pink spot due to class iv invasive cervical root resorption using vital pulp therapy: a case report. Iran Endod J. 2023;18(2):110–2.
Asgary S. A successful pulpotomy-treated permanent molar withstood recurrent decay after 10 years of treatment. J Dent Sci. 2022;17(4):1827–8.
Asgary S, Eghbal MJ. The effect of pulpotomy using a calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: a randomized clinical trial. Odontology. 2010;98(2):126–33.
Eghbal MJ, Haeri A, Shahravan A, Kazemi A, Moazami F, Mozayeni MA, Saberi E, Samiei M, Vatanpour M, AkbarzadeBaghban A. Postendodontic pain after pulpotomy or root canal treatment in mature teeth with carious pulp exposure: a multicenter randomized controlled trial. Pain Res Manag. 2020. https://doi.org/10.1155/2020/5853412.
Asgary S, Eghbal MJ. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: a multi-center randomized controlled trial. Acta Odontol Scand. 2013;71(1):130–6.
Asgary S, Eghbal MJ, Bagheban AA. Long-term outcomes of pulpotomy in permanent teeth with irreversible pulpitis: a multi-center randomized controlled trial. Am J Dent. 2017;30(3):151–5.
Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S. One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Invest. 2013;17(2):431–9.
Asgary S, Eghbal MJ, Ghoddusi J. Two-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter randomized clinical trial. Clin Oral Invest. 2014;18(2):635–41.
Asgary S, Eghbal MJ, Fazlyab M, Baghban AA, Ghoddusi J. Five-year results of vital pulp therapy in permanent molars with irreversible pulpitis: a non-inferiority multicenter randomized clinical trial. Clin Oral Investig. 2015;19(2):335–41.
Nosrat A, Seifi A, Asgary S. Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. Int J Paediatr Dent. 2013;23(1):56–63.
Asgary S, Eghbal MJ, Shahravan A, Saberi E, Baghban AA, Parhizkar A. Outcomes of root canal therapy or full pulpotomy using two endodontic biomaterials in mature permanent teeth: a randomized controlled trial. Clin Oral Invest. 2022;26(3):3287–97.
Malekafzali B, Shekarchi F, Asgary S. Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur J Paediatr Dent. 2011;12(3):189–93.
Salehi SZ, Jabarifar SE, Borujeni MB. Evaluation of the clinical and radiographic outcomes of pulpotomy in primary molars using formocresol, CEM cement and sodium hypochlorite 5%. IJSciences. 2015;4(04):35–40.
Ansari G, Morovati SP, Asgary S. Evaluation of four pulpotomy techniques in primary molars: a randomized controlled trial. Iran Endod J. 2018;13(1):7.
Sajadi FS, Jalali F, Khademi M. Ferric sulfate versus calcium-enriched mixture cement in pulpotomy of primary molars: a randomized clinical trial. Pesqui Bras Odontopediatria Clín Integr. 2021;21:e0017.
Manohar S, Bazaz N, Neeraja G, Subramaniam P, Sneharaj N. A comparative evaluation of four regenerative materials for pulpotomy in primary molars: an in vivo study. Dent Res J. 2022;19(1):102.
Memarpour M, Fijan S, Asgary S, Keikhaee M. Calcium-enriched mixture pulpotomy of primary molar teeth with irreversible pulpitis. A clinical study. Open Dent J. 2016;10:43–9.
Asgary S, Sarraf Shirazi A, Sabbagh S. Management of primary molars with irreversible pulpitis employing tampon pulpotomy: report of three cases with 34-month mean follow-up. Clin Case Rep. 2021;9(4):2289–94.
Asgary S, Roghanizadeh L. tampon pulpotomy: long-term successful results of a molar with irreversible pulpitis and previous vital pulp therapy failure. Iran Endod J. 2023;18(3):165–7.
Asgary S, Çalışkan MK. Vital pulp therapy of a mature molar with concurrent hyperplastic pulpitis, internal root resorption and periradicular periodontitis: a case report. Iran Endod J. 2015;10(4):284.
Asgary S, Fazlyab M, Sabbagh S, Eghbal MJ. Outcomes of different vital pulp therapy techniques on symptomatic permanent teeth: a case series. Iran Endod J. 2014;9(4):295–300.
Yazdani S, Jadidfard MP, Tahani B, Kazemian A, Dianat O, Marvasti LA. Health technology assessment of CEM pulpotomy in permanent molars with irreversible pulpitis. Iran Endod J. 2014;9(1):23–9.
Nosrat A, Asgary S. Apexogenesis treatment with a new endodontic cement: a case report. J Endod. 2010;36(5):912–4.
Nosrat A, Asgary S. Apexogenesis of a symptomatic molar with calcium enriched mixture. Int Endod J. 2010;43(10):940–4.
Harandi A, Forghani M, Ghoddusi J. Vital pulp therapy with three different pulpotomy agents in immature molars: a case report. Iran Endod J. 2013;8(3):145–8.
Sabbagh S, Sarraf Shirazi A, Eghbal MJ. Vital pulp therapy of a symptomatic immature permanent molar with long-term success. Iran Endod J. 2016;11(4):347–9.
Ashraf H, Rahmati A, Amini N. Vital pulp therapy with calcium-silicate cements: report of two cases. Iran Endod J. 2017;12(1):112–5.
MacInnes A. What is the most effective endodontic medicament for pulpotomies in immature permanent teeth? Evid Based Dent. 2020;21(3):108–9.
Chen Y, Chen X, Zhang Y, Zhou F, Deng J, Zou J, Wang Y. Materials for pulpotomy in immature permanent teeth: a systematic review and meta-analysis. BMC Oral Health. 2019;19:1–9.
Nosrat A, Asgary S, Eghbal MJ, Ghoddusi J, Bayat-Movahed S. Calcium-enriched mixture cement as artificial apical barrier: a case series. J Conserv Dent. 2011;14(4):427.
Balan P, Parameswaran M, Ramesh K. Apexification of a traumatized anterior tooth with calcium enriched mixture with one year follow up—a case report. IOSR J Dent Med Sci. 2013;9:18–21.
Parirokh M, Farzaneh S, Hallajmofrad AR. Conservative management of unset mineral trioxide aggregate root-end filling: a case report. Iran Endod J. 2016;11(3):241–5.
Abazarpour R, Parirokh M, Farhadi A, Jalali Z, Kheirabadi N. Successful ultra-conservative management of a mandibular premolar with dens invaginatus. Iran Endod J. 2017;12(3):390–5.
Nosrat A, Seifi A, Asgary S. Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: a review and report of two cases with a new biomaterial. J Endod. 2011;37(4):562–7.
Asgary S, Fazlyab M, Nosrat A. Regenerative endodontic treatment versus apical plug in immature teeth: three-year follow-up. J Clin Pediatr Dent. 2016;40(5):356–60.
Mehrvarzfar P, Abbott PV, Akhavan H, Savadkouhi ST. Modified revascularization in human teeth using an intracanal formation of treated dentin matrix: a report of two cases. J Int Soc Prev Community Dent. 2017;7(4):218–21.
Roghanizadeh L, Fazlyab M. Revascularization and apical plug in an immature molar. Iran Endod J. 2018;13(1):139.
Kubba R, Al DZ. Revitalization of a necrotic immature permanent anterior tooth (case report). J Bagh Coll Dent. 2018;30(2):82–5.
Asgary S. Management of an unrepairable root perforation due to inflammatory root resorption: a case report. J Dent Sci. 2022;17(3):1409–10.
Asgary S, Ehsani S. Periradicular surgery of human permanent teeth with calcium-enriched mixture cement. Iran Endod J. 2013;8(3):140.
Moradi Majd N, Akhtari F, Araghi S, Homayouni H. Treatment of a vertical root fracture using dual-curing resin cement: a case report. Case Rep Dent. 2012;2012: 985215.
Asgary S, Fazlyab M. Surgical treatment of an immature short-rooted traumatized incisor with an extensive apical lesion using CEM cement. Iran Endod J. 2015;10(2):148–51.
Asgary S, Fayazi S. Endodontic surgery of a symptomatic overfilled mta apical plug: a histological and clinical case report. Iran Endod J. 2017;12(3):376–80.
Fazlyab M, Asgary S. Failure of cone-beam computed tomography in detection of fiber post perforation. Iran Endod J. 2017;12(3):396.
Asgary S, Roghanizadeh L, Haeri A. Surgical endodontics vs regenerative periodontal surgery for management of a large periradicular lesion. Iran Endod J. 2018;13(2):271.
Asgary S, Talebzadeh B. Surgical endodontics for management of progressive actinomycosis. Gen Dent. 2020;68(1):61–4.
Asgary S, Mirmohammadi H, Parhizkar A. Management of symptomatic horizontal mid-root fractures after unsuccessful orthograde endodontic retreatments. Cureus. 2019;11(8):e5473.
Asgary S, Roghanizadeh L. Grafting with bone substitute materials in therapy-resistant periapical actinomycosis. Case Rep Dent. 2021;2021:6619731.
Asgary S, Roghanizadeh L. Partial necrosis consequence of the infection spreading from an adjacent apical periodontitis: a case report. Iran Endod J. 2018;13(3):420–3.
Asgary S. Management of a hopeless mandibular molar: a case report. Iran Endod J. 2011;6(1):34–7.
Asgary S, Marvasti LA, Kolahdouzan A. Indications and case series of intentional replantation of teeth. Iran Endod J. 2014;9(1):71.
Kheirieh S, Fazlyab M, Torabzadeh H, Egfhbal MJ. Extraoral retrograde root canal filling of an orthodontic induced external root resorption using CEM cement. Iran Endod J. 2014;9(2):149–52.
Moradi Majd N, Arvin A, Darvish A, Aflaki S, Homayouni H. Treatment of necrotic calcified tooth using intentional replantation procedure. Case Rep Dent. 2014;2014: 793892.
Asgary S, Nosrat A. Concurrent intentional replantation of maxillary molars using a novel root-end filling. Gen Dent. 2014;62(3):30–3.
Moradi Majd N, Zohrehei H, Darvish A, Homayouni H, Adel M. Continued root formation after delayed replantation of an avulsed immature permanent tooth. Case Rep Dent. 2014;2014:832637.
Asgary S, Roghanizadeh L. Rapid bone healing after intentional replantation of a molar with apical actinomycosis. Iran Endod J. 2018;13(1):135–8.
Asgary S, Talebzadeh B. Intentional replantation of a molar with several endodontic complications. J Stomatol Oral Maxillofac Surg. 2019;120(5):489–92.
Francis T, Sakkir N, Kumar V, Joshi SB. Effectiveness of a novel calcium-enriched mixture root cement to decelerate replacement resorption in replanted teeth: a case report. World J Dent. 2019;10(6):457–60.
Asgary S, Ahmadyar M. Autotransplantation of a maxillary third molar with closed roots. Oral Surg. 2013;6(3):146–8.
Ghanbari HO, Taheri M, Abolfazli S, Asgary S, Gharechahi M. Efficacy of MTA and CEM cement with collagen membranes for treatment of class II furcation defects. J Dent. 2014;11(3):343.
Eghbal MJ, Fazlyab M, Asgary S. Repair of a strip perforation with calcium-enriched mixture cement: a case report. Iran Endod J. 2014;9(3):225.
Asgary S, Verma P, Nosrat A. Periodontal healing following non-surgical repair of an old perforation with pocket formation and oral communication. Restor Dent Endod. 2018;43(2):e17.
Asgary S, Eghbal MJ, Mehrdad L, Kheirieh S, Nosrat A. Surgical management of a failed internal root resorption treatment: a histological and clinical report. Restor Dent Endod. 2014;39(2):137–42.
Asgary S. Furcal perforation repair using calcium enriched mixture cement. J Conserv Dent. 2010;13(3):156.
Eghbal MJ, Fazlyab M, Asgary S. Repair of an extensive furcation perforation with CEM cement: a case study. Iran Endod J. 2014;9(1):79.
Asgary S, Parhizkar A. Healing of large endodontic lesions using a new combination of triple antibiotics: a case report. Clin Case Rep. 2023;11(1): e6879.
Mungekar-Markandey S, Mistry L, Jawdekar A. Clinical success of iatrogenic perforation repair using mineral trioxide aggregate and other materials in primary molars: a systematic review and meta-analysis. Int J Clin Pediatr Dent. 2022;15(5):610.
Asgary S, Nosrat A, Seifi A. Management of inflammatory external root resorption by using calcium-enriched mixture cement: a case report. J Endod. 2011;37(3):411–3.
Sabbagh S, Shirazi AS, Torabzadeh H. Double antibiotic paste for management of external inflammatory root resorption. Iran Endod J. 2018;13(4):569.
Asgary S, Parhizkar A. Management of external inflammatory root resorption following tooth autotransplantation using a modified combination of triple antibiotics. Case Rep Dent. 2022. https://doi.org/10.1155/2022/5178339.
Ramazani M, Asgary S, Zarenejad N, Mehrani J. Interdisciplinary approach for management of iatrogenic internal root resorption: a case report. Iran Endod J. 2016;11(1):71.
Tavassoli-Hojjati S, Kameli S, Rahimian-Emam S, Ahmadyar M, Asgary S. Calcium enriched mixture cement for primary molars exhibiting root perforations and extensive root resorption: report of three cases. Pediatr Dent. 2014;36(1):23E-E27.
Asgary S, Ahmadyar M. One-visit endodontic retreatment of combined external/internal root resorption using a calcium-enriched mixture. Gen Dent. 2012;60(4):e244–8.
Mirmohammadi H, Asgary S. Management of merged external/internal root resorption using cem cement: a case report. J Oral Res. 2018;7(8):318–22.
Asgary S, Fazlyab M. Surgical repair of invasive cervical root resorption with calcium-enriched mixture cement: a case report. Gen Dent. 2015;63(1):37–40.
Asgary S, Nosrat A. Conservative management of class 4 invasive cervical root resorption using calcium-enriched mixture cement. J Endod. 2016;42(8):1291–4.
Asgary S, Nosrat A, Fazlyab M. Intracanal management of a post-traumatic perforative invasive cervical root resorption using calcium enriched matrix cement. Saudi Endod J. 2013;3(3):139–43.
Asgary S, Nourzadeh M, Verma P, Hicks ML, Nosrat A. Vital pulp therapy as a conservative approach for management of invasive cervical root resorption: a case series. J Endod. 2019;45(9):1161–7.
Asgary S, Eghbal MJ. Root canal obturation of an open apex root with calcium enriched mixture. J Int J Case Rep Imaging. 2012;3:50–2.
Asgary S, Fazlyab M. Endodontic management of an infected primary molar in a child with agenesis of the permanent premolar. Iran Endod J. 2017;12(1):119–22.
Asgary S, Fazlyab M. A successful endodontic outcome with non-obturated canals. Iran Endod J. 2015;10(3):208–10.
Shourgashti Z, Keshvari H, Torabzadeh H, Rostami M, Bonakdar S, Asgary S. Physical properties, cytocompatibility and sealability of HealApex (a novel premixed biosealer). Iran Endod J. 2018;13(3):299–304.
Asgary S, Eghbal MJ, Fazlyab M, Baghban AA, Ghoddusi J. Five-year results of vital pulp therapy in permanent molars with irreversible pulpitis: a non-inferiority multi-center randomized clinical trial. Clin Oral Invest. 2015;19(2):335–41.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SA conceptualized the study, performed data analyses, and prepared the manuscript. MA and MF supported the conceptualization of the study and assisted in manuscript preparation and revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
SA is the inventor of CEM cement (Endodontic Filling Material; USA, 7,942,961, 2011 May 17).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Asgary, S., Aram, M. & Fazlyab, M. Comprehensive review of composition, properties, clinical applications, and future perspectives of calcium-enriched mixture (CEM) cement: a systematic analysis. BioMed Eng OnLine 23, 96 (2024). https://doi.org/10.1186/s12938-024-01290-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-024-01290-4