Abstract
Objectives
Oral healthcare expenses are increasing rapidly as a result of the growth of high-cost health technologies worldwide. In many developing/developed countries, low-cost tooth extraction is the alternative treatment option for a high-cost root canal therapy (RCT) for management of human molars with irreversible pulpitis. Vital pulp therapy with calcium-enriched mixture cement (VPT/CEM) as a new alternative treatment option has demonstrated excellent treatment outcomes up to 1 year; if 2-year radiographic/clinical effectiveness as well as cost-effectiveness of the VPT/CEM is also non-inferior compared with RCT, it can serve as a viable treatment for mature molars with irreversible pulpitis.
Materials and methods
In this prospective, multicenter (n = 23), non-inferiority clinical trial, 407 patients were randomized to either one-visit RCT (n = 202) or VPT/CEM (n = 205) for 27 months. In this part of study, the primary outcome measure was the 2-year clinical and radiographic treatment outcomes. Cost-effectiveness was also analyzed.
Results
Mean follow-up times were 24.62 ± 0.72 and 24.61 ± 0.69 months in RCT (n = 166) and VPT/CEM (n = 166) arms, respectively. Clinical success rates in the two study arms were equal (98.19 %); however, radiographic success rates were 79.5 and 86.7 % in RCT and VPT/CEM arms, respectively, with no statistical difference (P = 0.053). The treatment time span mean was approximately three times greater in the RCT than in the VPT/CEM arm (94.07 vs. 31.09 min; P < 0.001). RCT had a cost of 171.5K per molar tooth compared with 44.5K for VPT.
Conclusions
VPT/CEM reduced time and cost spent. When considering clinical as well as cost-effectiveness of VPT/CEM, this treatment option is not only non-inferior but also superior to RCT in mature permanent molar teeth with established irreversible pulpitis.
Clinical relevance
Vital pulp therapy with CEM is a cost-effective and reliable biological technique for endodontic treatment of permanent molar teeth with irreversible pulpitis and can be recommended for general clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral health is an integral part of general health as well as quality of life. The cause and effect association between socioeconomic status (SES) and oral/general health status is well documented. Even in developed countries in the new millennium, SES is a strong determinant of tooth loss [1, 2]. The rate of dental utilization is lower for lower-SES people; though they reported a greater number of new dental symptoms, they were less likely to obtain dental care. When they did seek oral healthcare, they were more likely to experience tooth extraction and edentulism [1, 3]. Tooth loss is the final common endpoint for most dental diseases and conditions, the most frequent being irreversible pulpitis [4, 5]. However, it can considerably influence chewing ability, quality of life, and nutrition [1, 6].
It is a universal consensus that if there is no economic limitation, root canal therapy (RCT) is the treatment of choice for irreversible pulpitis. However, the survival rate of endodontically treated teeth in comparison to vital teeth, specifically molars, is alarmingly low [7]. Realistic outcome of RCT in the general population from epidemiological study reported high prevalence of radiographic failures (61 %) [8]. Case–control studies show that RCT of vital cases can yield favorable outcomes [9]. However, a recent systematic review reported that the success rates of RCT had not improved over the last five decades, again, molars had the worse survival rates [10]; moreover, satisfactory radiographic criteria for quality of endodontic treatment were significantly lower for molars than for other teeth [11]. A further systematic review reported that vital permanent teeth with cariously exposed pulp/irreversible pulpitis can be treated successfully with vital pulp therapy (VPT) [12]. It was shown to be a biologic, conservative, economic, and simple method, with a more favorable success rate [12, 13]. Currently, the number of people who can afford RCT has possibly reduced; therefore VPT has a relevant socioeconomic aspect too [14]. This alternative treatment option could avoid the early loss of molars. In addition, VPT could be performed by general dentists, while RCT may require an endodontist in molar teeth [14].
In dentistry, it is universally accepted that vital pulp tissue should be preserved if possible, with no questions asked. However, clinicians are reluctant to conduct VPT once the diagnosis of irreversible pulpitis is reached due to the inherent meaning of irreversible and are forced to carry out RCT. This clinical diagnosis is basically carried out on an experimental basis [4]. No consistent relationship between clinical symptoms and histopathological status of the pulp has been established [15]. Sound clear evidence to demonstrate the cutoff point from reversible to irreversible pulpitis does not exist. An interesting recent systematic review reported that “the overall evidence was insufficient to assess the value of toothache or abnormal reaction to heat/cold stimulation for determining the pulp condition” [16]. Besides, there are reports of successful VPT in vital teeth with signs/symptoms of irreversible pulpitis with periapical lesions [12, 17], highlighting the high capacity of dental pulp as a connective tissue to heal. Recently, pulp capping materials have shifted from being not only biocompatible but also bioactive; the focus has been redirected from repair to regeneration of the remaining pulp tissue [18, 19].
While numerous pulp capping agents have been advocated, the investigation for a perfect biomaterial has continued. Ideally, the biomaterial should control infection, adhere to dentin/restorative material (to provide hermetic seal), be nontoxic, be radiopaque, be simple to handle clinically, maintain pulpal vitality, and finally have a superficial effect on the pulp, thereby inducing a biologic encapsulation process resulting in dentine bridge formation. Bacteria are significant inhibiting factors for the healing process. Results from previous pulp capping studies with calcium-enriched mixture (CEM) cement suggest that stimulation of dentin bridge formation occurs not only because of its antibacterial effects [20] via high alkalinity [21] but also owing to release of Ca2+ and OH− [22]. In addition, CEM provides an endogenous source of PO4 that accelerates hydroxyapatite formation even in saline solution [23]. Like mineral trioxide aggregate (MTA), the sealing ability of CEM is superior to IRM [24]. A recent study revealed that shear bond strength of CEM to adhesive resin is favorable due to its cohesive mode of failure [25]. In terms of cytotoxicity and biocompatibility, CEM showed similar encouraging results to MTA [26–28]. CEM cement offers some advantages over MTA including improved handling, shorter setting time, decreased film thickness, and improved flow [21], resulting in simple clinical handling. In addition, several histological studies have reported that CEM cement has the ability to induce formation of a continuous dentin bridge [29–31]. CEM promotes osteogenesis [32], dentinogenesis [33], cementogenesis [34, 35], and maturogenesis [36, 37] as well as revascularization of necrotic pulp in immature teeth [38].
We hypothesized that the treatment outcomes of VPT with CEM cement (VPT/CEM) would be non-inferior to RCT in mature human molar teeth with established irreversible pulpitis. The results of pain relief during 7 days as well as 6- and 12-month follow-ups revealed superior treatment outcomes for VPT/CEM in comparison to RCT [39, 40]. The aim of this part of the present multicenter, randomized, non-inferiority clinical trial was to assess the 2-year treatment outcomes of VPT/CEM in comparison with one-visit RCT. In addition, the radiographic outcomes at 2 years after treatment were compared with those of the 6-month follow-up to evaluate the prognostic value of a 6-month control. This report aims to compare cost-effectiveness of VPT/CEM and RCT as well.
Materials and methods
The project was evaluated/approved by the Iranian Ministry of Health and the Ethics Committee of Iran Center for Dental Research, SBMU, Tehran, Iran. This clinical trial was conducted in compliance with the ethical principles of the Helsinki Declaration. This was a 27-month multicenter, randomized, parallel-grouped, and open-labeled design.
This report is part of a larger ongoing study, which has been registered at ClinicalTrials.gov (identifier: NCT00748280). Subjects were recruited according to previously reported inclusion/exclusion criteria; the sample size determination and randomization, general dentists’ attendance, one-visit root canal therapy technique (reference treatment) as well as vital pulp therapy with calcium-enriched mixture cement method (alternative treatment), and outcome measures (clinical assessments and radiographic scoring) were also the same as previously reported [40]. In this study, we will carry out comparative analysis of the intermediate- (6-month) and long-term (24-month) follow-up results.
Cost measures
As no standardized cost prices were available for RCT and VPT, national tariffs from the Relative Value in Dental Services book were used to estimate all treatment costs [41]. In cases where two tariffs for three and four rooted molars existed, the mean was estimated. Cost prices have been presented in K coefficient; in 2009, K was equal to 1,600 Iranian rial (IRR) (1 US dollar = 9,600 IRR).
We defined the total treatment time to be from administration of local anesthesia to the placement of temporary restoration. The time span was recorded by general dentists for each patient in the two study arms.
Statistical analysis was performed by a chi-square test. Statistical error type I was considered as 0.05. Statistical analysis was set up using SPSS version 13.
Results
Seventy-five patients (RCT, n = 36; VPT/CEM, n = 39) did not attend 24-month follow-up resulting in 332 (81.57 %) cases for long-term control; a statistical difference was not observed between study arms (P = 0.75).
Mean follow-up times at 2 years were 24.61 ± 0.69 and 24.62 ± 0.72 months in RCT and VPT/CEM arms, respectively; a statistical difference was not observed.
Treatment time spans were 94.07 min [coefficient of variation (CV) = 29.01 %] and 31.09 min (CV = 29.38 %) in the RCT and VPT/CEM, respectively (P < 0.001).
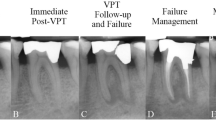
The results of radiographic evaluation by the four examiners illustrated that overall consensus treatment outcome of radiographic evaluation between the study arms at 2 years did not show statistically significant difference (Table 1, Fig. 1). Clinical success rates in the two study arms at 2-year follow-up were the same (98.19 %); outcomes in cases with preoperative periapical involvement were similar in the two study arms (P = 0.117) (Table 2).
Preoperative, postoperative, and follow-up radiographs in RCT and VPT/CEM groups: A, B healed, with normal contour and width of PDL before the treatments and at follow-up; C, D failed, with normal PDL before the treatments and a new periapical radiolucency at follow-up; E, F healed, with apical periodontitis before the treatments and normal PDL at follow-up; and G, H failed, with apical periodontitis before the treatments and persistent apical radiolucency at follow-up
Table 3 demonstrates no statistical difference between the alterations in distribution pattern of treatment outcomes related to the study arms within the time between the two follow-ups.
Cost-effectiveness
The costs of RCT were 148K and 195K (K = 1,600 IRR and 0.166 USD) for three and four canalled teeth, respectively (mean = 171.5K). The cost of VPT was 44.5K. Other costs categories were equivalent: postoperative radiology (7.4K) and coronal restorations costs (one-surface restorations = 43K, multi-surface restorations = 65K). The cost of nonsurgical endodontic retreatment for failure cases of RCT was 280K, while the average cost of endodontic treatment for failure cases of VPT/CEM was 171.5K.
Discussion
When severe pain is experienced in vital teeth or when mild to moderate pain is present with a prior history of pain, irreversible pulpitis is diagnosed. Management involves either RCT or extraction [5]. Historically, there were no other permanent treatment options. We hypothesized that treatment outcomes of VPT/CEM are non-inferior to RCT. Two-year results of the trial revealed that the treatment outcomes of VPT/CEM were statistically non-inferior to one-visit RCT, confirming our hypothesis as well as previous results [39, 40].
High-cost RCT replaces the vital tissues with endodontic materials instead of living pulp tissue. Survival rates of such a tooth are not comparable with teeth with vital pulps, especially when it involves molars [7]; endodontically treated teeth cannot continue their function without loss of proprioceptive function, tooth sensitivity, and damping properties [12]. A multitude of procedural accident, i.e., furcal/root perforation, instrument separation, alveolar nerve paraesthesia, and irrigation complications, canal transportation, and ledge formation as iatrogenic errors were more often identified in molars, making further treatment more problematic [42, 43]. Whether to preserve and treat the tooth or to insert high-cost implant technology becomes a challenge for the clinician [44]. In terms of aesthetics, RCT can cause tooth discoloration [45]. Endodontically treated molars, weakened by intentional enamel/dentine removal, can be lost at a much quicker rate if they are not supported with high-cost crowns [46, 47]. On the other hand, preserving the dental pulp reduces the episode of apical periodontitis [48]. The patient may be more willing to accept VPT with CEM as compared to tooth extraction or RCT due to the patient’s refusal/fear. Based on these facts, the ability to preserve dental pulp vitality via a low-cost VPT/CEM is a highly favorable treatment option in modern endodontology.
Obtained results showed that VPT/CEM is more time and cost effective in all situations compared with RCT; moreover, results showed a trend of higher success rates up to the 2-year recall. Under such conditions, there is no need to determine a cost-effectiveness ratio because the analysis is clear: a new biotechnology that costs less and produces equivalent/better results is desirable [49]. Thus, VPT/CEM may become a dominant method over RCT with respect to economic evaluation.
It is recommended that prospective trials reveal the accurate long-term prognosis of endodontically treated molars [50]; recall time can influence analysis of the outcome. Our trial was design to predict the treatment outcome of one-visit RCT as well as VPT/CEM in terms of the best reliable follow-up interval by using intermediate- (6-month) and long-term (1-, 2-, and 5-year) follow-ups. Our obtained results until now demonstrated that radiographic success rates after VPT/CEM were comparable at intermediate and 2-year follow-ups. Recently, we have reported that there is no difference between 6- and 12-month results [40]; therefore, it appears that 6-month follow-up is a reasonable/sufficient interval for evaluating the results of VPT. However, the probability of success increases continuously over time for RCT, agreeing with other reports [51]. Recent studies demonstrated that the follow-up period of 2 years is adequate [52]; however, complete healing following RCT might need an extended period of time [53]; we aim to carry out a 5-year follow-up.
The high clinical success rate of 98.19 % in this trial is based on patients reporting very few symptoms. Nonsurgical root canal treatment outcomes showed that the long-term tooth survival was 95 % [54], agreeing with our results. However, endodontic literature reveals that the majority of prognostic studies examined outcomes based on the radiographic resolution or the continued existence or progression of an apical periodontitis according to Strindberg’s criteria [50]. Since apical periodontitis may be clinically asymptomatic in many cases, we examined radiographic periapical status. Thus, the outcomes extrapolated from the radiographic evaluation had lower success rates (∼12–18 % less than clinical success). On the other hand, current endodontic concepts dictate that the major biologic factor influencing the treatment outcome is the presence of preoperative apical periodontitis. In the presence of apical periodontitis, the lower success is predicted [55]. The overall success rate of vital teeth with apical periodontitis in both study arms was considerably lower compared with teeth with normal periodontal ligament (PDL) (∼17.5 %), i.e., it was 10 and 25 % lower for VPT/CEM and RCT arms, respectively. However, VPT/CEM demonstrated better trend of success in such cases during 2-year follow-ups.
Initially, we employed 412 participants to compare the RCT with VPT/CEM; we had only 18 % drop out at 2-year follow-up. Because of the difficult nature of clinical trials and patient attendance, the majority of researchers have used short- and intermediate-term follow-ups as the endpoint. In the new millennium, there are numerous short-term randomized clinical trials that evaluated the clinical effectiveness of different treatment protocol on post-endodontic pain [56, 57]. In contrast, there are a few long-term randomized clinical trials to demonstrate treatment outcomes after one- and two-visit endodontic treatments [58, 59]. These trials were carried out on sizeable number of teeth/patients (n ≈ 100) with low and medium rate of drop out (12 and 35 %), comparable to our dropout rates.
The variation between the treatment outcomes in the two study arms during the trial interestingly reveals that our “expected power” at the beginning of the study was similar to “observed power” at the end of the study.
When RCT is performed by endodontic specialists or under/postgraduate students under strict operating conditions, i.e., aseptic setting, the success rate is generally high. However, epidemiologic studies reported that up to 64.5 % of endodontically treated teeth, mainly by general dentists, are associated with apical periodontitis [60] in both industrialized and developing nations [8, 61]. An effective evidence-based procedure is required and should be pursued to solve this shocking problem and improve the endodontic treatment outcome worldwide. Our results revealed that VPT/CEM is highly affordable for most clinicians/patients as it is clinically simple and quick and has acceptable results in inexperienced hands. Moreover, VPT failures can be treated by a general dentist (first time RCT). However, RCT failures are more difficult to treat and are likely to require an endodontist.
Conclusion
Two-year treatment outcomes of VPT/CEM are statistically non-inferior to one-visit RCT in human mature molar teeth with established irreversible pulpitis. However, in terms of cost-effectiveness, VPT/CEM significantly reduces expenditure compared with RCT. Outcomes of VPT/CEM were comparable at 6-month and 1- and 2-year follow-ups; therefore, it appears that 6-month recall is a reasonable time. Low-cost VPT/CEM is a predictable simple bio-regenerative method with an excellent prognosis; it can be considered an evidence-based alternative option to extraction and RCT.
References
Gilbert GH, Duncan RP, Shelton BJ (2003) Social determinants of tooth loss. Health Serv Res 38:1843–1862
Edelstein BL (2002) Disparities in oral health and access to care: findings of national surveys. Ambul Pediatr 2:141–147
Dolan TA, Atchison KA (1993) Implications of access, utilization and need for oral health care by the non-institutionalized and institutionalized elderly on the dental delivery system. J Dent Educ 57:876–887
Levin LG, Law AS, Holland GR, Abbott PV, Roda RS (2009) Identify and define all diagnostic terms for pulpal health and disease states. J Endod 35:1645–1657
Bender IB (2000) Reversible and irreversible painful pulpitides: diagnosis and treatment. Aust Endod J 26:10–14
Gilbert GH, Duncan RP, Heft MW, Dolan TA, Vogel WB (1998) Multidimensionality of oral health in dentate adults. Med Care 36:988–1001
Caplan DJ, Cai J, Yin G, White BA (2005) Root canal filled versus non-root canal filled teeth: a retrospective comparison of survival times. J Public Health Dent 65:90–96
Weiger R, Hitzler S, Hermle G, Lost C (1997) Periapical status, quality of root canal fillings and estimated endodontic treatment needs in an urban German population. Endod Dent Traumatol 13:69–74
Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, Nakagaki H, Nakamura H (2004) Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:95–99
Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K (2007) Outcome of primary root canal treatment: systematic review of the literature—part 1. Effects of study characteristics on probability of success. Int Endod J 40:921–939
Alsaleh I, Cousson PY, Nicolas E, Hennequin M (2012) Is endodontic treatment performed under general anaesthesia technically acceptable? Clin Oral Investig 16:1599–1606
Aguilar P, Linsuwanont P (2011) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod 37:581–587
Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J (2009) MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J 35:4–8
Demarco FF, Rosa MS, Tarquinio SB, Piva E (2005) Influence of the restoration quality on the success of pulpotomy treatment: a preliminary retrospective study. J Appl Oral Sci 13:72–77
Seltzer S, Bender IB, Ziontz M (1963) The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol 16:969–977
Mejare IA, Axelsson S, Davidson T, Frisk F, Hakeberg M, Kvist T, Norlund A, Petersson A, Portenier I, Sandberg H, Tranaeus S, Bergenholtz G (2012) Diagnosis of the condition of the dental pulp: a systematic review. Int Endod J 45:597–613
Asgary S (2011) Calcium-enriched mixture pulpotomy of a human permanent molar with irreversible pulpitis and condensing apical periodontitis. J Conserv Dent 14:90–93
Goldberg M, Schmalz G (2011) Toward a strategic plan for pulp healing: from repair to regeneration. Clin Oral Investig 15:1–2
Ulker HE, Hiller KA, Schweikl H, Seidenader C, Sengun A, Schmalz G (2012) Human and bovine pulp-derived cell reactions to dental resin cements. Clin Oral Investig 16:1571–1578
Asgary S, Kamrani FA (2008) Antibacterial effects of five different root canal sealing materials. J Oral Sci 50:469–474
Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S (2008) The properties of a new endodontic material. J Endod 34:990–993
Amini Ghazvini S, Abdo Tabrizi M, Kobarfard F, Akbarzadeh Baghban A, Asgary S (2009) Ion release and pH of a new endodontic cement, MTA and Portland cement. Iran Endod J 4:74–78
Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J (2009) Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J 35:147–152
Asgary S, Eghbal MJ, Parirokh M (2008) Sealing ability of a novel endodontic cement as a root-end filling material. J Biomed Mater Res A 87:706–709
Oskoee SS, Kimyai S, Bahari M, Motahari P, Eghbal MJ, Asgary S (2011) Comparison of shear bond strength of calcium-enriched mixture cement and mineral trioxide aggregate to composite resin. J Contemp Dent Pract 12:457–462
Malekafzali B, Shekarchi F, Asgary S (2011) Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur J Paediatr Dent 12:189–193
Asgary S, Eghbal MJ (2013) Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: a multi-center randomized controlled trial. Acta Odontol Scand 71:130–136
Asgary S, Moosavi SH, Yadegari Z, Shahriari S (2012) Cytotoxic effect of MTA and CEM cement in human gingival fibroblast cells. Scanning electronic microscope evaluation. N Y State Dent J 78:51–54
Zarrabi MH, Javidi M, Jafarian AH, Joushan B (2011) Immunohistochemical expression of fibronectin and tenascin in human tooth pulp capped with mineral trioxide aggregate and a novel endodontic cement. J Endod 37:1613–1618
Asgary S, Ehsani S (2009) Permanent molar pulpotomy with a new endodontic cement: a case series. J Conserv Dent 12:31–36
Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H (2008) A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:609–614
Rahimi S, Mokhtari H, Shahi S, Kazemi A, Asgary S, Eghbal MJ, Mesgariabbasi M, Mohajeri D (2012) Osseous reaction to implantation of two endodontic cements: mineral trioxide aggregate (MTA) and calcium enriched mixture (CEM). Med Oral Patol Oral Cir Bucal 17:e907–e911
Tabarsi B, Parirokh M, Eghbal MJ, Haghdoost AA, Torabzadeh H, Asgary S (2010) A comparative study of dental pulp response to several pulpotomy agents. Int Endod J 43:565–571
Asgary S, Eghbal MJ, Ehsani S (2010) Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod 36:837–841
Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S (2010) Repair of furcal perforation using a new endodontic cement. Clin Oral Invest 14:653–658
Nosrat A, Asgary S (2010) Apexogenesis treatment with a new endodontic cement: a case report. J Endod 36:912–914
Nosrat A, Seifi A, Asgary S (2013) Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. Int J Paediatr Dent 23:56–63
Nosrat A, Seifi A, Asgary S (2011) Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: a review and report of two cases with a new biomaterial. J Endod 37:562–567
Asgary S, Eghbal MJ (2010) The effect of pulpotomy using a calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: a randomized clinical trial. Odontology 98:126–133
Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S (2013) One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Investig 17:431–439
Ministry of Refah (2009) Relative value in dental services. 85–89
Eleftheriadis GI, Lambrianidis TP (2005) Technical quality of root canal treatment and detection of iatrogenic errors in an undergraduate dental clinic. Int Endod J 38:725–734
Editorial Board JOE (2008) Procedural accidents: an online study guide. J Endod 34:e65–e70
Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R (2009) Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J 42:757–774
Glickman GN, Koch KA (2000) 21st-century endodontics. J Am Dent Assoc 131(Suppl):39S–46S
Tikku AP, Chandra A, Bharti R (2010) Are full cast crowns mandatory after endodontic treatment in posterior teeth? J Conserv Dent 13:246–248
Akman S, Akman M, Eskitascioglu G, Belli S (2012) The use of endodontically treated and/or fiber post-retained teeth as abutments for fixed partial dentures. Clin Oral Investig 16:1485–1491
Lin LM, Di Fiore PM, Lin J, Rosenberg PA (2006) Histological study of periradicular tissue responses to uninfected and infected devitalized pulps in dogs. J Endod 32:34–38
Laupacis A, Feeny D, Detsky AS, Tugwell PX (1992) How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ 146:473–481
Setzer FC, Boyer KR, Jeppson JR, Karabucak B, Kim S (2011) Long-term prognosis of endodontically treated teeth: a retrospective analysis of preoperative factors in molars. J Endod 37:21–25
Orstavik D (1996) Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J 29:150–155
Siqueira JF Jr, Rocas IN, Riche FN, Provenzano JC (2008) Clinical outcome of the endodontic treatment of teeth with apical periodontitis using an antimicrobial protocol. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:757–762
Fristad I, Molven O, Halse A (2004) Nonsurgically retreated root filled teeth—radiographic findings after 20–27 years. Int Endod J 37:12–18
Ng YL, Mann V, Gulabivala K (2011) A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J 44:610–625
Chugal NM, Clive JM, Spangberg LS (2001) A prognostic model for assessment of the outcome of endodontic treatment: effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91:342–352
Menhinick KA, Gutmann JL, Regan JD, Taylor SE, Buschang PH (2004) The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J 37:531–541
Menke ER, Jackson CR, Bagby MD, Tracy TS (2000) The effectiveness of prophylactic etodolac on postendodontic pain. J Endod 26:712–715
Molander A, Warfvinge J, Reit C, Kvist T (2007) Clinical and radiographic evaluation of one- and two-visit endodontic treatment of asymptomatic necrotic teeth with apical periodontitis: a randomized clinical trial. J Endod 33:1145–1148
Penesis VA, Fitzgerald PI, Fayad MI, Wenckus CS, BeGole EA, Johnson BR (2008) Outcome of one-visit and two-visit endodontic treatment of necrotic teeth with apical periodontitis: a randomized controlled trial with one-year evaluation. J Endod 34:251–257
Yan MT (2006) The management of periapical lesions in endodontically treated teeth. Aust Endod J 32:2–15
Asgary S, Shadman B, Ghalamkarpour Z, Shahravan A, Ghoddusi J, Bagherpour A, Akbarzadeh Baghban A, Hashemipour M, Ghasemian Pour M (2010) Periapical status and quality of root canal fillings and coronal restorations in Iranian population. Iran Endod J 5:74–82
Acknowledgments
The authors thank the study participants and dentists (Drs. S. Niknam, H. Abdolmaleki, M. Shahriari, B. Sepehri, M. Zarei, H. Mohadesi, L. Kochmeshki, N. Shirzaei, S.H. Hoseini, M.R. Naderi, A.R. Torkamanzadeh, N. Sahranavard, J. Mohebi, A. Naseri, M. Forozanfar, A. Razavi, A. Izadi, H. Fadaei, K. Khorshidian, H.A. Taheri, M.H. Bagheri-Atabak, M. Zareshahi, and M. Pahlevan-Shamsi) for their enthusiastic contributions, as well as Drs. K. Bagheri-Lankarani, S.H. Emami-Razavi, S.M. Alavian, A.R. Mesdaghinia, M.M. Goya, M.H. Khoshnevisan, S.M. Tabatabaei, K. Etemad, M.M. Vardi, M. Sourosh, and H. Hesary who provided the national supervision of and support for this trial; Dr S.M.R. Safavi for critical review; Drs. A.R. Zali, S. Mohamad-Sadeghi, M. Piriaei, and S. Kheirieh for administrative help; Drs. A. Akbarzadeh and M.J. Kharazi-Fard who helped to develop the original statistical design/analysis; Drs. R.A. Taheri, F. Rahnama, A. Heravi, G.A. Dehghani, and H. Fotohi who monitored the trial in different states; Dr. E. Soheilipour, M. Ghorbanpour, B. Shadman, O. Hosseini, and Z. Khademi who entered and checked the data; Drs. H. Nazarinia and S. Goorang who interpreted the X-rays; and Dr. L. Alim Marvasti for the English editing of the manuscript. This work was supported by the Iranian Ministry of Health and Medical Education (Health Deputy, Oral Health Office) and Shahid Beheshti University of Medical Sciences [grant number p/25/17/1/tm/103].
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asgary, S., Eghbal, M.J. & Ghoddusi, J. Two-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter randomized clinical trial. Clin Oral Invest 18, 635–641 (2014). https://doi.org/10.1007/s00784-013-1003-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1003-6