Abstract
Objectives
Previous reported results of up to 12 months as well as 24-month follow-ups revealed superior and equivalent treatment outcomes for vital pulp therapy (VPT) using calcium-enriched mixture cement (CEM) in comparison with root canal therapy (RCT) for mature molars with established irreversible pulpitis, respectively. Present non-inferiority multicenter randomized clinical trial assesses the final long-term (5-year) results as well as the effects of patients’ age/gender and the presence of preoperative periapical lesion on the treatment outcomes.
Materials and methods
A total number of 407 patients were blindly allocated into two treatment groups [group 1 (VPT/CEM, n = 205) and group 2 (RCT, n = 202)] treated in 23 health-care centers by calibrated dentists. The treatment outcomes were assessed after 60 months.
Results
The 5-year results revealed no significant differences in the successes of both study arms (P = 0.29); a total number of 271 patients were available (~33 % were lost to follow-up). The patients’ age/gender did not affect the outcomes; the presence of preoperative periapical lesion also did not implement a significant effect in both groups (P > 0.05).
Conclusions
As an alternative for RCT, VPT/CEM can be considered as a valid treatment for vital mature permanent molars clinically diagnosed with irreversible pulpitis.
Clinical relevance
Considering the favorable outcomes of 6- to 60-month follow-ups, as an evidence-based/simple/affordable/effective/biologic approach in cases of irreversible pulpitis, VPT/CEM is highly recommended for universal clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The dental pulp can be exposed by accidental trauma or during preparation of a tooth for restoration which can be diagnosed as mechanical or carious exposure [1]. Moreover, each day, there are innumerable patients seeking for a dental visit to get rid of toothache steaming from symptomatic vital pulps [2]. In mature teeth, the treatments for inflamed exposed pulps include maintaining the tooth via root canal therapy (RCT) or tooth extraction; when compared to the first option, the later represents the non-optimal choice [3, 4]. The rationale for the RCT is based on the following: (i) the unreliability of vital pulp therapy (VPT) on these teeth, which is currently proved to be wrong by a high level of evidence (LoE) trials [5, 6], and (ii) the high probability for success in cases of optimally performed RCT on a tooth with vital pulp [7].
When deciding to condemn the vital pulp to extirpation, the most important issue to consider is the impossibility to determine the true status of the pulp in terms of whether it is in a reversible or irreversible state [2]; merely clinical sign/symptoms such as degree/characteristic of pain do not precisely reflect pulpal condition [1, 2]. On the other end of the spectrum, the rather high number of patients diagnosed with irreversible pulpitis also presents apical periodontitis [8], and this means that many potentially vital pulps are extirpated as a result of wrong diagnosis of necrosis due to the presence of apical lucency. The scenario is that in many developing or even developed countries, financial considerations or low dental IQ results in some patients choosing the less appropriate treatment for symptomatic inflamed pulps, which is tooth extraction [3–6].
Experts are of the opinion that for an informed, meticulously selected patient [1] who wills to avoid RCT [5, 6, 9] and under such circumstances where the tooth would be extracted otherwise, VPT should be attempted as the correct/ethical treatment choice [4, 10], specially in contemporary modern endodontics where pulp regeneration in necrotic teeth has become the top goal [11]. Ideally, VPT of adults’ permanent teeth includes direct/indirect pulp capping and partial/miniature/coronal pulpotomy using pulp-covering (bio)materials, which subsequently preserve the coronal pulp in situ, partially or totally removed to the level of canal orifice(s), and stimulate the formation of dentinal bridge as a natural barrier [12–14]. Considering the theory which states the inflammation of the pulp to be restricted to the irritation neighboring zones [15], the rationale behind pulpotomy approach is the removal of the inflamed portion of a pulp.
VPT can be concluded to have a high success rate provided that (i) the remaining pulp is either non-inflamed or capable of healing; (ii) hemorrhage is properly controlled; (iii) a biocompatible, bioregenerative capping material is applied; and (iv) a bacterial tight seal is present [1, 13, 14]. Despite being controversial, there are many reports of successful VPTs in patients with age ranging from 6 to 70 years [1, 10]; many clinicians hold the view that VPT for adult patients cannot be as successful as younger ones.
Calcium-enriched mixture (CEM) cement has been introduced as a hydrophilic tooth-colored biomaterial with favorable sealing ability. In terms of cytotoxicity, genotoxicity, osteogenic, dentinogenic, and cementogenic effects, CEM is biocompatible like mineral trioxide aggregate (MTA); many studies have shown the hard tissue (dentine, cementum, and bone) inductivity of CEM cement [16–18].
Decision making during the management of clinical problems should be based on the best currently available evidence [1, 19]. The randomized clinical trials with large sample sizes and long follow-up periods are graded the highest rank in LoE pyramid [19]. The successful long-term outcomes of primary molar pulpotomy using CEM cement have been already described [20]. Some randomized clinical trials have compared the efficacy of CEM cement in VPT of caries-exposed permanent molars, as well [5, 21]. The results revealed that CEM cement had similar successful outcomes in pulpotomy of permanent molars compared to MTA. It has also been shown that pulpotomy of teeth with irreversible pulpitis using CEM cement had a faster postoperative pain-relieving property compared to conventional RCT [9]. The present randomized clinical trial has been conducted for 5 years to compare the treatment outcomes of pulpotomy of permanent teeth with sign/symptoms of irreversible pulpitis using CEM cement; the 1- and 2-year results of the clinical trial revealed high clinical and radiographic success [6, 22]. This part of the trial aims to report the 5-year treatment outcomes of VPT/CEM or RCT for adults’ permanent molars with irreversible pulpitis. In addition, the influence of patient’s age/gender on long-term outcomes of VPT as well as effects of the presence of preoperative periapical lesion on the treatment outcomes is assessed.
Materials and methods
This project was evaluated and approved by the Iranian Ministry of Health and also the Ethics Committee of Iranian Center for Dental Research, Shahid Beheshti University of Medical Sciences, Tehran, Iran, and also registered at ClinicalTrials.gov (Identifier: NCT00748280). The protocol of patient retrieval was compatible with the principles of Declaration of Helsinki. This is the last report of the multicenter trial, with a randomized, parallel-grouped, and open-labeled design, representing the 5-year outcomes of treatment; the previous reports included outcomes of short- (postoperative pain) [9], intermediate- (6 months) [6], and long-term (12 and 24 months) recall [6, 22].
From a pool of patients of both genders referred to 23 health-care centers of five medical universities from four different states of Iran, the subjects of the study were recruited from 9–65-year-old patients who had a vital molar tooth (detected by clinical sign/symptoms) with a history of pain indicative of irreversible pulpitis (i.e., a spontaneous pain or a pain exacerbated with hot and cold stimuli that lasted for a few seconds to several hours which was interpreted as lingering type compared to the normal teeth and could be reproduced using cold/heat testing [2]) and those who had opted for extraction for pain relief and announced to be prepared for future recalls. Subjects with moderate or severe marginal periodontitis, a tooth non-restorable with amalgam or a tooth with internal/external resorption, and root canal calcification in periapical radiographs and medically compromised patients with systemic complication that would alter the treatment procedure were excluded. In addition, if a tooth was diagnosed with a non-common anatomy of root canal system during root canal therapy, it would be excluded. The volunteers had to sign an informed consent, and they were assured that in case they wished to quit, they would be excluded. Each patient was assigned with a code. All the demographic data, patients’ codes, and the treated teeth for each subject were recorded before treatment.
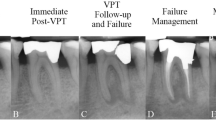
After 5 years, all the clinical and radiographic evaluations were done in the same way as described in two previous reports [6, 22]. In addition, the previous database was also checked for treatment cases with failure, those failed teeth in both arms that did not take part in the next evaluations (i.e., failed cases at 1-year follow-up who did not take part at 2- and 5-year recall). The 5-year results of each treatment group, with/without such failures, were assessed using the chi-square test. The chi-square test was also used for assessing the effect(s) of gender on treatment outcomes in each of the study arms.
The influence of patients’ age (three age groups of <20, 20–29, and ≥30 years) as well as the effect of preoperative periapical involvement (i.e., presence/absence of apical lucency) on success/failure of the study arms were assessed using the multiple binary logistic regression model.
The marginal homogeneity test was used to compare the distribution of treatment responses in each of the study arms at 1- and 5-year follow-ups.
Statistical analysis was set up using SPSS version 16. Statistical error type I was set at 0.05.
Results
After 5 years, a total number of 271 patients (66.6 %; 137 in VPT/CEM group and 134 in RCT group) were available for assessment of treatment outcomes. Using the independent sample t test, no significant difference in the follow-up duration was shown between the groups (P = 0.27).
When the data of available patients were assessed, the chi-square test revealed no significant difference in the treatment outcomes of both groups with the success rates of 78.1 and 75.3 % for the VPT/CEM and RCT groups, respectively (P = 0.61).
When the missing data related to the previous failures (n = 13 in VPT/CEM group and n = 20 in RCT group) were evaluated, the difference between the study arms was not significant (P = 0.29) with success rate being 71.3 % for VPT/CEM group and 65.8 % for RCT group.
In terms of the correlation between patients’ age and treatment outcomes in each of the two study arms, the multiple binary logistic regression model revealed that the outcome and patients’ age were not significantly related in each of the defined age groups (P = 0.72 and P = 0.61 for VPT/CEM and RCT arms, respectively; Table 1).
For assessing the impact of gender on outcomes of treatment in each of the study arms, the statistical analysis did not reveal a significant difference (P = 0.24 in VPT/CEM and P = 0.73 in RCT; Table 2).
In addition, the marginal homogeneity test did not reveal a significant difference between the 1- and 5-year results in the group treated by VPT/CEM (P = 0.09), while the difference for the RCT group was significant (P < 0.001) (Table 3).
For the interaction of treatment type and preoperative periapical involvement of the teeth on treatment success and failure, the multiple binary logistic regression model revealed no significant differences (P = 0.71) (Table 4).
Discussion
This was a 5-year, multicenter, randomized, non-inferiority clinical trial employing a large sample size in a wide age range, compared to the treatment outcomes of VPT/CEM as a new bioregenerative concept with RCT, in Iran. Immediate, 6-, 12-, and 24-month outcomes were previously reported [6, 9, 22], and this is the final report (60 months) presenting the last long-term outcomes. The 5-year success rate of VPT/CEM was comparable to that of RCT; in other words, for the treatment of irreversible pulpitis, VPT/CEM approach is not only non-inferior to RCT, but also, it ended up in equivalent results compared to RCT.
The ultimate goal of endodontics is the prevention/elimination of apical periodontitis (AP) [4, 23]. If we exclude the cases of AP in teeth with vital inflamed pulps [8], the term AP, will be used to describe the rest of the cases of lesions due to endodontic pathogens egressing form the apical foramen of necrotic teeth [4, 24]. Therefore, by maintaining the vital pulp (i.e., health), those cases of AP (i.e., disease) that occur due to necrosis can be prevented, and in fact, this is the best endodontics (i.e., providing health care) possible [4]. The results of the current study revealed that preoperative periapical involvement around the target teeth did not affect the outcomes of VPT, as many of the samples in the VPT/CEM group did show a preoperative periapical involvement, and the presence of these lesions did not influence the positive treatment outcomes.
It used to be generally accepted that a history of spontaneous or lingering provoked pain is indicative of extensive irreversible inflammatory changes of the pulp tissue, and a radical treatment such as RCT has to be performed [2]. From the traditional point of view, the rational for this choice is that pulpal inflammation has probably reached a level where its elimination is not possible without removal of entire pulp tissue. Vital pulpectomy gained general acceptance following several studies published in the period from 1940s to 1970s [4], stating the unreliability of VPT and the high success rate of performing RCT on vital teeth [1, 25]. However, many authors have stated that the survival prognosis of endodontically treated teeth is not as good as teeth with vital pulps, especially in molars with the hazard ratio of >7:1 [26], which can be due to the loss of tooth structure as well as defensive mechanisms provided by the vital pulp such as tooth sensitivity, proprioception [27, 28], and damping property [29]. Therefore, professionals hold the view that the vital pulp should be preserved, as far as possible. One should also consider that not all RCTs are technically perfect.
The 5-year success rate of root canal treatment in this trial was 75.3 %. Epidemiological studies have reported a high prevalence of radiographic failures of RCTs [30]. A recent systematic review has shown that the success rate of endodontic treatment has not improved over the last decades and among these, the RCTs of molar teeth present the worse survival rate [31]. This can be attributed to multiple procedural mishaps such as perforations, instrument separation, ledge formation, and canal transportation [31, 32]. On the other hand, although the success rates of up to 96–98 % have been reported for treatments done by endodontists [33], it is undeniable that most of the dental visits are provided by GPs worldwide; epidemiologic studies have demonstrated up to 66 % prevalence of AP after endodontic treatment performed by GPs which can be related to technically defective treatments [33, 34].
The results of a recent systematic review concluded that “Vital pulp therapy should be considered as an alternative treatment to pulpectomy in vital permanent teeth with cariously exposed pulps, and partial/full pulpotomy provide more predictable outcomes than direct pulp capping” [1]. This alternative treatment option could avoid the early loss of molars due to aforementioned iatrogenic reasons during RCT. In addition, VPT can be easily learned and performed by GPs, while RCT in molar teeth seems to be much more complicated and technique sensitive [35]. The results of the present 5-year outcome assessment revealed that VPT/CEM is not only statistically non-inferior to one-visit RCT in mature molars clinically diagnosed with irreversible pulpitis, but also, it offers the advantage of having simplicity and low time/financial/patient cost. The last but not least is the impossibility of conducting pulp tests on pulpotomized teeth [12, 36, 37], and this fact highlights that some teeth may have silently become necrotized and emphasize on the importance of radiographic follow-up. Although it is possible that, in some teeth, a clinically silent chronic inflammation or a sterile necrosis occurred, in cases of probable treatment failure in VPT, there is still a chance of performing RCT which is not the same scenario for pulpectomized teeth, as the failed endodontic treatment can potentially end up in more complicated strategies such as surgical/nonsurgical retreatment.
While it is easy to write about optimal treatment, many facts remain that need to be issued: with the contemporary knowledge, can the histological status of the pulp be judged by clinical symptoms and condemned for extirpation based on speculation? For many years, it is being stated that the signs/symptoms such as degree or characteristic of pain do not precisely reflect the pulp condition [38]. Considering the importance of vital pulp [27, 28] and recent efforts in pulp regeneration in (im)mature pulpless permanent teeth [11], extirpation of the already existing vital pulp merely based on clinical evaluation does not seem to have a place in modern endodontics, anymore.
From patients’ point of view, there is a well-documented cause and effect association between patients’ socioeconomic status and their health-care concerns, as even in developed countries, the socioeconomic status is a strong determinant of tooth loss [39]. This means that in every community, there is a social class of population who are less likely to obtain dental care due to financial issues or loss of education, and when they seek oral health care, they are more likely to experience tooth extraction and edentulism [39, 40]. Every day, endodontists visit many patients with low dental IQ who do not want to or cannot afford RCT as an expensive treatment on a tooth that shows diagnostic or clinical signs of irreversible pulpitis, and thus, they choose extraction [4]. Opting for alternative treatments other than tooth extraction, e.g., VPT seems to be basically logical. However, VPT in adult permanent teeth following carious exposure of the pulp is controversial; some authors state that VPT should be performed only in young patients because of the high healing capacity of the pulp compared to old ones [1, 41]. The results of the current study proved that patient’s age does not affect the success rate of VPT, neither does the patient’s gender.
To compare the VPT/CEM with RCT, a huge number of participants were employed in this trail (n = 407); however, at the end of the study, 138 patients were lost to follow-up (absolute overall loss to follow-up rate = 33 %). As the difficult nature of clinical trials and patient attendance, the majority of investigators have represented the short/intermediate-term end points. Few 1- and 2-year randomized clinical trials assessed the treatment outcomes after initial endodontic treatments on much lower sample size (n ≈ 100) with 12 and 35 % dropout, respectively [42, 43]. One of the best cohort studies in this field is the Toronto Study which started with 582 endodontically treated teeth, and in phase IV, 4–6-year outcomes after initial endodontic treatment were reported only based on 32 % recall [44]. Another important issue is the comparative loss rates in the experimental arms; when losses are related to differences in efficacy of the treatments, bias could arise [45]; however, our previous report with 18 % dropout at 2 years revealed that the treatment effectiveness of VPT/CEM was comparable with RCT (2 years). Moreover, in the present trial, the loss rate in both arms was identical (33 %).
Pulp is able to respond to external noxious agents. In theory, by doing partial or total pulpotomy, the most superficial part of the pulp containing inflammatory changes and even bacterial infiltration is removed, and the surgical wound would contain sound and reactive connective tissue [41]. Currently, several studies have reported a successful outcome of vital pulp therapy in vital teeth with cariously exposed pulps and signs/symptoms of irreversible pulpitis even with periapical lesions [10, 46, 47]. Taking into account the high demand for tooth extraction due to excruciating pain stemming from irreversible pulpitis, by those patients who cannot afford RCT or are not aware of the side effects of elective tooth extraction, VPT needs to be considered as an edentulism preventive treatment that meanwhile has pain relief ability comparable to RCT, as it has been proved in a recent randomized controlled clinical trial [9].
Conclusion
Considering the total results of the present non-inferiority multicenter randomized clinical trials with large sample size and short- to long-term follow-ups, treatment outcomes of VPT/CEM in mature permanent molars with established irreversible pulpitis is comparable with RCT; this evidence-based, simple, cost-effective, predictable, and bioregenerative treatment option is recommended as a realistic alternative for tooth extraction or RCT in general clinical practice worldwide.
References
Aguilar P, Linsuwanont P (2011) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod 37:581–587
Mejare IA, Axelsson S, Davidson T, Frisk F, Hakeberg M, Kvist T et al (2012) Diagnosis of the condition of the dental pulp: a systematic review. Int Endod J 45:597–613
McDougal RA, Delano EO, Caplan D, Sigurdsson A, Trope M (2004) Success of an alternative for interim management of irreversible pulpitis. J Am Dent Assoc 135:1707–1712
Swift EJ, Trope M, Ritter AV (2003) Vital pulp therapy for the mature tooth—can it work? Endod Top 5:49–56
Asgary S, Eghbal MJ (2013) Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: a multi-center randomized controlled trial. Acta Odontol Scand 71:130–136
Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S (2013) One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Investig 17:431–439
Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I et al (2004) Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:95–99
Abella F, Patel S, Duran-Sindreu F, Mercade M, Bueno R, Roig M (2012) Evaluating the periapical status of teeth with irreversible pulpitis by using cone-beam computed tomography scanning and periapical radiographs. J Endod 38:1588–1591
Asgary S, Eghbal MJ (2010) The effect of pulpotomy using a calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: a randomized clinical trial. Odontology 98:126–133
Matsuo T, Nakanishi T, Shimizu H, Ebisu S (1996) A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod 22:551–556
Nosrat A, Li KL, Vir K, Hicks ML, Fouad AF (2013) Is pulp regeneration necessary for root maturation? J Endod 39:1291–1295
Cvek M (1978) A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod 4:232–237
Witherspoon DE (2008) Vital pulp therapy with new materials: new directions and treatment perspectives—permanent teeth. J Endod 34:S25–S28
Asgary S, Ahmadyar M (2013) Vital pulp therapy using calcium-enriched mixture: an evidence-based review. J Conserv Dent 16:92–98
Yamasaki M, Kumazawa M, Kohsaka T, Nakamura H, Kameyama Y (1994) Pulpal and periapical tissue reactions after experimental pulpal exposure in rats. J Endod 20:13–17
Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H (2008) A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:609–614
Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S (2010) Repair of furcal perforation using a new endodontic cement. Clin Oral Investig 14:653–658
Naghavi N, Ghoddusi J, Sadeghnia HR, Asadpour E, Asgary S (2014) Genotoxicity and cytotoxicity of mineral trioxide aggregate and calcium enriched mixture cements on L929 mouse fibroblast cells. Dent Mater J 33:64–69
Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ (2008) Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther 88:156–175
Malekafzali B, Shekarchi F, Asgary S (2011) Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur J Paediatr Dent 12:189–193
Nosrat A, Seifi A, Asgary S (2013) Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. Int J Paediatr Dent 23:56–63
Asgary S, Eghbal MJ, Ghoddusi J (2014) Two-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter randomized clinical trial. Clin Oral Investig 18:635–641
Chugal NM, Clive JM, Spangberg LS (2001) A prognostic model for assessment of the outcome of endodontic treatment: effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91:342–352
Azuma MM, Samuel RO, Gomes-Filho JE, Dezan-Junior E, Cintra LT (2013) The role of IL-6 on apical periodontitis: a systematic review. Int Endod J. doi:10.1111/iej.12196
Ricucci D, Russo J, Rutberg M, Burleson JA, Spangberg LS (2011) A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:825–842
Caplan DJ, Cai J, Yin G, White BA (2005) Root canal filled versus non-root canal filled teeth: a retrospective comparison of survival times. J Public Health Dent 65:90–96
Chee WW, Donovan TE (1993) Use of radicular attachments with endodontically treated teeth. J Calif Dent Assoc 21:57–60
Randow K, Glantz PO (1986) On cantilever loading of vital and non-vital teeth. An experimental clinical study. Acta Odontol Scand 44:271–277
Ou KL, Chang CC, Chang WJ, Lin CT, Chang KJ, Huang HM (2009) Effect of damping properties on fracture resistance of root filled premolar teeth: a dynamic finite element analysis. Int Endod J 42:694–704
Pak JG, Fayazi S, White SN (2012) Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod 38:1170–1176
Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F et al (2007) Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Dent Traumatol 23:66–71
Weiger R, Hitzler S, Hermle G, Lost C (1997) Periapical status, quality of root canal fillings and estimated endodontic treatment needs in an urban German population. Endod Dent Traumatol 13:69–74
Friedman S, Mor C (2004) The success of endodontic therapy—healing and functionality. J Calif Dent Assoc 32:493–503
Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S (2003) Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J 36:181–192
Demarco FF, Rosa MS, Tarquinio SB, Piva E (2005) Influence of the restoration quality on the success of pulpotomy treatment: a preliminary retrospective study. J Appl Oral Sci 13:72–77
Barrieshi-Nusair KM, Qudeimat MA (2006) A prospective clinical study of mineral trioxide aggregate for partial pulpotomy in cariously exposed permanent teeth. J Endod 32:731–735
Sonmez D, Sari S, Cetinbas T (2008) A Comparison of four pulpotomy techniques in primary molars: a long-term follow-up. J Endod 34:950–955
Seltzer S, Bender IB, Ziontz M (1963) The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol 16:969–977
Edelstein BL (2002) Disparities in oral health and access to care: findings of national surveys. Ambul Pediatr 2:141–147
Dolan TA, Atchison KA (1993) Implications of access, utilization and need for oral health care by the non-institutionalized and institutionalized elderly on the dental delivery system. J Dent Educ 57:876–887
Fong CD, Davis MJ (2002) Partial pulpotomy for immature permanent teeth, its present and future. Pediatr Dent 24:29–32
Penesis VA, Fitzgerald PI, Fayad MI, Wenckus CS, BeGole EA, Johnson BR (2008) Outcome of one-visit and two-visit endodontic treatment of necrotic teeth with apical periodontitis: a randomized controlled trial with one-year evaluation. J Endod 34:251–257
Molander A, Warfvinge J, Reit C, Kvist T (2007) Clinical and radiographic evaluation of one- and two-visit endodontic treatment of asymptomatic necrotic teeth with apical periodontitis: a randomized clinical trial. J Endod 33:1145–1148
de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S et al (2008) Treatment outcome in endodontics: the Toronto study—phase 4: initial treatment. J Endod 34:258–263
Schulz KF, Grimes DA (2002) Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet 359:781–785
Mejare I, Cvek M (1993) Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol 9:238–242
Caliskan MK (1995) Pulpotomy of carious vital teeth with periapical involvement. Int Endod J 28:172–176
Acknowledgments
This work was supported by the Iranian Ministry of Health and Medical Education (Health Deputy, Oral Health Office) and Shahid Beheshti University of Medical Sciences (grant number p/25/17/1/tm/103). The authors thank the study participants and dentists (Dr. S. Niknam, Dr. H. Abdolmaleki, Dr. M. Shahriari, Dr. B. Sepehri, Dr. M. Zarei, Dr. H. Mohadesi, Dr. L. Kochmeshki, Dr. N. Shirzaei, Dr. S.H. Hoseini, Dr. M.R. Naderi, Dr. A.R. Torkamanzadeh, Dr. N. Sahranavard, Dr. J. Mohebi, Dr. A. Naseri, Dr. M. Forozanfar, Dr. A. Razavi, Dr. A. Izadi, Dr. H. Fadaei, Dr. K. Khorshidian, Dr. H.A. Taheri, Dr. M.H. Bagheri-Atabak, Dr. M. Zareshahi, and Dr. M. Pahlevan-Shamsi) for their enthusiastic contributions as well as Dr. K. Bagheri-Lankarani, Dr. S.H. Emami-Razavi, Dr. S.M. Alavian, Dr. A.R. Mesdaghinia, Dr. M.M. Goya, Dr. M.H. Khoshnevisan, Dr. S.M. Tabatabaei, Dr. K. Etemad, Dr. M.M. Vardi, Dr. M. Sourosh, and Dr. H. Hesary who provided the national supervision and support for this trial; Dr. S.M.R. Safavi for critical review; Dr. A.R. Zali, Dr. S. Mohamad-Sadeghi, Dr. M. Piriaei, and Dr. S. Kheirieh for administrative help; and Dr. R.A. Taheri, Dr. F. Rahnama, Dr. A. Heravi, Dr. G.A. Dehghani, and Dr. H. Fotohi who monitored the trial in different states.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asgary, S., Eghbal, M.J., Fazlyab, M. et al. Five-year results of vital pulp therapy in permanent molars with irreversible pulpitis: a non-inferiority multicenter randomized clinical trial. Clin Oral Invest 19, 335–341 (2015). https://doi.org/10.1007/s00784-014-1244-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1244-z