Abstract
Background
Hamstrings neuromuscular function is a crucial component of functional movement, and changes after anterior cruciate ligament (ACL) injury contribute to risk factors for secondary injury and long-term sequelae. To effectively treat muscular impairments, an accurate understanding of hamstrings neuromuscular function in patients with ACL reconstruction (ACLR) is needed.
Objective
A systematic review and meta-analysis were undertaken to describe and quantify hamstrings neuromuscular function in individuals with ACLR compared to controls.
Methods
We searched PubMed, Web of Science, SPORTDiscus, CINAHL, and EBSCOhost databases in October of 2020 for studies evaluating the difference between hamstrings electromyography (EMG) between individuals with ACLR and controls. Two independent reviewers assessed each paper for inclusion and quality. Means and standard deviations were extracted from each included study to allow random-effect size (ES) meta-analysis calculations for comparison of results.
Results
Thirty-four studies were included for final review. From these, 5 categories of neuromuscular outcomes were identified, and studies were grouped accordingly: (1) muscle activation levels (EMG amplitude), (2) co-activation, (3) onset timing, (4) electromechanical delay, and (5) time-to-peak activity. Moderate to strong evidence indicates that individuals with ACLR demonstrate higher hamstrings EMG amplitude (normalized to % maximum voluntary isometric contraction) and hamstrings-to-quadriceps co-activation during gait and stair ambulation compared to controls. In addition, there was moderate evidence of longer electromechanical delay during knee flexion and greater hamstrings-to-quadriceps co-activation during knee extension compared to controls.
Conclusions
Greater hamstrings EMG amplitude and co-activation during gait and ambulation tasks and longer electromechanical delay of the hamstrings in individuals with ACLR align with clinical impairments following ACLR and have implications for re-injury risk and long-term joint health, thus warranting attention in rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Compared to controls, individuals with ACLR demonstrate greater hamstrings EMG amplitude (normalized to activity during MVIC) and hamstrings-to-quadriceps co-activation during gait and stair-related tasks. |
Individuals with ACLR demonstrated longer electromechanical delay of the hamstrings during knee flexion and greater hamstrings-to-quadriceps co-activation during knee extension compared to controls. |
Overall, these results align with known clinical impairments following ACLR with implications for re-injury risk and long-term joint health, thus warranting attention in rehabilitation. |
1 Introduction
Anterior cruciate ligament reconstruction (ACLR) and rehabilitation is the gold standard treatment to restore knee joint stability and function following ACL injury in active individuals [1]. However, the high rates of incomplete return to competitive sport (55%) [2, 3], secondary ACL injury (23–35% within first two years) [4, 5], and long-term sequelae, such as post-traumatic osteoarthritis (33–51%) [6, 7], suggest multifactorial shortcomings of rehabilitation. As rehabilitation professionals, we now understand that long-term reductions in knee extensor moments (e.g. quadriceps avoidance) and neuromuscular activation during activities of daily living (e.g. gait, stair ambulation) and sport (e.g. jump landing, cutting) are contributing to increased compressive forces [8, 9] and joint degeneration over time [10,11,12]. Likewise, as anatomical ACL agonists and dynamic stabilizers against knee valgus and anterior tibial translation [13], impairments in hamstrings neuromuscular control may be predictive of graft rupture after ACLR [14].
Neuromuscular control is generally defined as unconscious muscular activity in the preservation of dynamic joint stability [15]. Surface electromyography (EMG) has been widely used to understand post-traumatic changes in neuromuscular function during functional tasks. Electromyographic signal directly reflects motor unit recruitment and firing characteristics from which we can infer the role of muscles in producing movement or maintaining joint stability [16, 17]. Using EMG recordings, neuromuscular function has often been operationalized in terms of amplitude, onset timing, electromechanical delay (EMD), hamstrings-to-quadriceps co-activation, and time to peak muscle activity (Table 1).
Following ACL injury, quadriceps neuromuscular dysfunction (e.g. muscle weakness, activation failure, a lower rate of torque development) is well described [18, 19], and contributes to self-reported disability [20], and long-term sequelae (e.g. post-traumatic osteoarthritis) [21]. Although not as widely reported, similar disruptions of the neuromuscular system may threaten the hamstrings’ capacity to attenuate and counteract anterior and rotational tibial shear forces during knee loading in activities of daily living and sport [13, 22]. Hamstrings neuromuscular function is a crucial component of functional movement (e.g. walking, jumping, cutting), and changes after ACL injury may contribute to risk factors for secondary injury and post-traumatic osteoarthritis [14, 22, 23]. In particular, hamstrings muscle facilitation (e.g. greater muscle activity and co-contraction) occurs despite relative hamstrings muscle weakness after ACL injury [24] and ACLR [25]. Although protective against subsequent injury (theoretically by reducing shear forces at the knee) [14], this neuromuscular behavior may be detrimental to joint health through reciprocal inhibition of quadriceps activation and increased compressive joint forces [8, 9]. Hamstrings EMG amplitude and onset timing are modifiable with strength [26] and neuromuscular training [27] in healthy individuals, making them a possible clinical target for interventions in such individuals following ACLR. Surprisingly, evidence-based treatment approaches to guide hamstrings recovery are sparse, as the scientific literature has historically focused on the quadriceps.
An accurate understanding of hamstrings neuromuscular function in individuals with ACLR is important to better target impairments to optimize muscular recovery in rehabilitation. Thus, we undertook a systematic review with meta-analysis to describe and quantify the neuromuscular function of the hamstring muscle complex after ACLR to elucidate global thigh neuromuscular consequence of injury. Specifically, this review sought to investigate EMG-derived metrics of hamstrings neuromuscular function compared to uninjured controls.
2 Methods
2.1 Registration
This systematic review was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and was registered with PROSPERO prior to completion of the initial search (registration No: CRD42018110824, approval date: Oct 15th 2018). PROSPERO was searched to ensure no similar reviews were ongoing at time of registration.
2.2 Search Strategy
Studies were included if (a) the study population included adults following primary unilateral ACLR, (b) graft types included autograft (e.g. bone-patellar tendon-bone or hamstring tendon), and (c) any EMG derived outcomes of the hamstrings were published. Studies were excluded if (a) the study population included adolescent (under 18 years of age) or elderly (over 70 years or age) individuals, or (b) individuals who underwent ACL revision surgery. Studies that also included a comparison group of individuals who were ACL deficient were included, but those data were not considered.
We searched databases from inception to October 22nd, 2020. We searched the electronic bibliographical databases of PubMed, Web of Science, SPORTDiscus, CINAHL, and EBSCOhost (MEDLINE).
The search strategy included key terms relating to the population (e.g. anterior cruciate ligament injury OR anterior cruciate ligament reconstruction OR anterior cruciate ligament injuries) and describing variables of interest (e.g. electromechanical delay OR time to peak activity OR coefficient of variation OR muscle activity, etc.). Since there is no universal definition of neuromuscular control [15], this search strategy comprised a wide spectrum of EMG-derived outcomes to capture all potentially relevant studies. The search terms were adapted for database-specific filters and language as appropriate. An example search for PubMed is shown in Electronic Supplementary Material Appendix S1.
The search was restricted to English language studies. Unpublished research was not considered as it was deemed impractical to identify all unpublished work on EMG activity associated with hamstrings muscle activity in individuals with ACLR.
2.3 Study Selection
A single investigator (DAS) exported all studies identified by the search strategy to Endnote X9 (Clarivate Analytics, Jersey). Any duplicates were then deleted using the deduplication feature. The titles and abstracts of all publications were then screened by a single investigator (DAS) to remove irrelevant studies. Full text was acquired for all retained studies. Two independent reviewers (DAS and NRG) determined final eligibility and inclusion. Any discrepancies were resolved at a consensus meeting.
2.4 Quality Assessment
Two independent reviewers (DAS and NRG) assessed the quality of all the included studies using the modified Newcastle–Ottawa Scale (mNOS), which is provided in Electronic Supplementary Material Appendix S2. All criteria were operationally defined, discussed in detail, and approved by all investigators during a consensus meeting prior to qualitative assessment. Although not developed specifically for ACL research, the mNOS is increasingly recommended for the qualitative assessment of observational studies [28]. The mNOS was applied using pen and paper. Discrepancies were resolved at a consensus meeting. Lack of agreement was resolved by a third reviewer (GEN) by a majority vote.
The mNOS contains eight categories (total of 9 possible points) relating to methodological quality. A score of 0–3 points was considered a low quality (LQ) study, a score of 4–6 points was considered a moderate quality (MQ) study, and a score of 7–9 points was considered a high quality (HQ) study.
2.5 Outcome Measures
The outcome measures considered in this review are generally considered metrics of neuromuscular function, operationally defined here as EMG-derived measures of amplitude, onset timing, EMD, co-activation, and time to peak muscle activity. For a description and justification of each, see Table 1.
2.6 Data Extraction
The following information was extracted from each of the publications by the primary investigator (DAS):
-
• publication information.
-
• patient descriptors: sample size, sex, age, height, weight, source of graft, sport, level of participation.
-
• study methods: study design, muscles assessed with EMG, task(s) completed.
-
• filtering and processing of EMG data.
-
• outcome measures: EMG amplitude, onset timing, EMD, co-activation, and time to peak muscle activity.
In individuals with ACLR, only data from the involved ACLR limb were extracted. Likewise, in control individuals, only data from the matched control limb were extracted. Corresponding authors were contacted for original data where publications did not report these in the text. Engauge Digitizer software (Open Source, Version 11.2) [29] was used to extract data from figures when authors were unable to recover the original data files or did not respond to requests [9, 30,31,32,33]. In five cases [34,35,36,37,38], data were not able to be extracted or obtained for meta-analysis.
2.7 Statistical Methods
Statistical analysis was completed using Review Manager 5 (The Cochrane Collaboration, Copenhagen, Denmark). Analyses were completed by one investigator (DAS). Standardized mean difference (SMD) and 95% confidence interval (CI) are reported. Individual and pooled SMD were calculated using Hedges’ g and categorized as small (≤ 0.50), medium (0.51–0.79), or large (≥ 0.80) [39]. To maximize clinical interpretability, raw mean differences (RMD, with 95% CIs) are reported for significant effects.
For studies reporting results for medial and lateral hamstrings musculature separately, data were analyzed separately. Semitendinosus and semimembranosus were reclassified as medial hamstring (MH), and biceps femoris was reclassified as lateral hamstring (LH). Studies not specifying or reporting MH and LH as pooled were reclassified as unspecified (US). For studies reporting results for males and females separately, or hamstrings tendon (HT) or patellar tendon (PT) graft types separately, data were pooled and have been presented as a heterogeneous cohort. The data for healthy control groups were also extracted in this way. Where methods, outcome measure, and task were comparable between studies, a random-effects meta-analysis was performed and the level of statistical heterogeneity for pooled data was established using the I2 statistics (p < 0.05). Heterogeneity (I2) was defined as low (0–40%), moderate (30–60%), substantial (50–90%), and considerable (75–100%) [40].
3 Results
3.1 Search Results
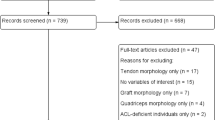
For detail of search results, including deduplication, exclusion, and full-text review, see Fig. 1. Following the screening of titles and abstracts, 163 publications were retained, and full text reviewed. Thirty-four studies were included for final review. Twenty-five studies evaluated the MH, 26 evaluated the LH, and 22 evaluated both MH and LH. One study [33] did not specify which hamstrings muscles were assessed, and three studies [31, 38, 41] reported bilateral hamstrings as pooled results. In these cases, they were classified as unspecified in the meta-analysis [31, 42].
Study characteristics, such as population sources, sample size, and demographic descriptors, are shown in Table 2. In total, the data from 1299 individuals were considered (700 ACLR, 599 controls) with at least 37% of the total sample being female. Of the individuals with ACLR, 35.9% (n = 251) underwent autograft with PT, 48.6% (n = 340) autograft with HT, 0.4% (n = 3) autograft with quadriceps tendon, 1.7% (n = 12) allograft, and 13.4% (n = 94) were not defined. Study design, task, muscles, EMG variables, and normalization procedures are reported in Table 3.
3.2 Methodological Quality Assessment
Results from the modified Newcastle Ottawa Scale (mNOS) are shown in Table 4. The median score was 5.5 (range 2–8) out of 9. Of the 34 studies, 8 (23.5%) were rated as high quality [14, 30, 31, 42,43,44,45,46], 22 (64.7%) were rated as moderate quality [9, 32,33,34, 37, 38, 41, 47,48,49,50,51,52,53,54,55,56,57,58,59,60,61], and 4 (11.8%) were rated as low quality [35, 36, 62, 63].
3.3 EMG Amplitude
Twenty studies evaluated hamstrings muscle activation, 17 of which were meta-analyzed.
Fourteen studies normalized muscle activity as percent maximum voluntary isometric contraction (% MVIC) for 8 different tasks (Fig. 2). In this comparison, individuals with ACLR demonstrated no difference in strength-based activation (i.e. knee flexion), single-limb stance, in-step kicking, or lateral push on a slide board compared to controls. However, individuals with ACLR demonstrated higher EMG amplitude than controls in the more dynamic tasks of gait (1 study, LH: g = 1.13 [95% CI 0.73, 1.54], RMD = 7.17% [95% CI 0.24, 14.11]), stair ambulation (3 studies, MH: g = 0.53 [95% CI 0.31, 0.75]; RMD = 1.87% [95% CI 0.93, 2.80]; LH: g = 0.86 [95% CI 0.29, 1.43], RMD = 3.01% [95% CI 0.96, 5.07]), and double-limb (1 study, US: g = 1.96 [95% CI 0.30, 0.3.61], RMD = 7.63% [95% CI 1.15, 14.11]) and single-limb jumping and jump landings (2 studies, MH: g = 0.86 [95% CI 0.43, 1.30], RMD = 10.76% [− 0.05, 21.58]). No consistent pattern of difference was seen between MH and LH activation, as all 95% confidence intervals overlapped.
EMG amplitude normalized to maximum voluntary isometric contraction by medial hamstrings, lateral hamstrings, and task. (1) Nordic hamstring exercise, (2) hamstring curl exercise, (3) concentric phase of squat, (4) eccentric phase of squat, (5) propulsion, (6) heel-strike, (7) stair ascent, (8) stair descent, (9) single-limb anterior reach, (10) step down, (11) step down with unstable platform perturbation, (12) step down with dual-task challenge, (13) step down with dual-task challenge and unstable platform perturbation, (14) concentric phase, (15) landing phase, (16) lift-off, (17) reactive, following contact, and (18) preparatory, prior to contact. ACLR anterior cruciate ligament reconstruction, EMG electromyography, SD standard deviation, Std standard, CI confidence interval
Two studies in the comparison were of high methodological quality. One study [30] reported higher MH (g = 1.18 [95% CI 0.46, 1.89]) but not LH EMG amplitude (g = 0.05 [95% CI − 0.60, 0.71]) in individuals with ACLR compared to controls during a single limb crossover hop test. Using pooled hamstring activity, another study [42] reported higher EMG amplitude in individuals with ACLR compared to controls during double limb jumping at ascent (g = 2.99 [95% CI 1.70, 4.27]), take-off (g = 0.48 [95% CI − 0.37, 1.33]), and landing (g = 2.56 [95% CI 1.38, 3.74]).
Three studies normalized activity as percent peak activity during the dynamic trial (% peak) for double limb or single limb jump landing tasks (Fig. 3). All were of high methodological quality. In the double limb comparison, there was no difference between hamstrings EMG amplitude between groups during double-limb jump landing (1 study, US: g = − 0.34 [95% CI − 1.06, 0.38], RMD = − 3.19% [95% CI − 9.53, 3.15]). Similarly, the LH and US single-limb jump landing comparisons showed no effect between groups (3 studies, LH: g = − 0.72 [95% CI − 1.51, 0.07], RMD = − 10.48% [95% CI − 18.38, − 2.58]; US: g = 0.10 [95% CI − 0.62, 0.81], RMD = 0.81% [95% CI − 5.03, 6.65]), as 95% confidence intervals crossed zero. However, a single study reporting MH activity during single limb jump landing found individuals with ACLR to be lower compared to control (MH: g = − 0.96 [95% CI − 1.83, − 0.07], RMD = − 14.00% [95% CI − 25.73, − 2.27]).
EMG amplitude normalized to maximum muscle activity in a dynamic trial by medial hamstring, lateral hamstring, and task. (1) reactive, following contact, (2) preparatory, prior to contact. ACLR anterior cruciate ligament reconstruction, EMG electromyography, SD standard deviation, Std standard, CI confidence interval
3.4 Co-activation
Eleven studies evaluated hamstrings-to-quadriceps muscle co-activation indices (peak or average EMG amplitude) (Fig. 4) [9, 31, 32, 38, 41, 44, 52, 55, 58, 60, 61]. Individuals with ACLR demonstrated no difference in co-activation during in-step kicking, or double-limb and single-limb jump landings compared to controls. However, individuals with ACLR demonstrated higher hamstrings co-activation than controls during strength-based activation (i.e. knee extension, 3 studies, MH: g = 0.85 [95% CI 0.53, 1.18], RMD = 1.03% [95% CI 0.29, 1.76]; LH: g = 0.93 [95% CI 0.22, 1.64], RMD = 1.35% [95% CI 0.38, 2.31]; US: g = 1.34 [95% CI 0.65, 2.03], RMD = 12.90% [95% CI 7.06, 18.74]), gait (1 study, MH: g = 3.57 [95% CI 3.04, 4.09], RMD = 10.72% [95% CI 9.45, 11.98]; LH: g = 1.45 [95% CI 0.90, 2.01], RMD = 3.84% [95% CI 2.60, 5.08]), and stair ambulation (2 studies, MH: g = 0.43 [95% CI 0.16, 0.69], RMD = 2.75% [95% CI 0.97, 4.53]; LH: g = 1.04 [95% CI 0.63, 1.44], RMD = 5.90% [95% CI 2.69, 9.11]). During gait, MH co-activation was characterized by a larger effect than LH in all phases (terminal swing, load-acceptance, and heel-strike). However, there were no further patterns of difference between MH and LH co-activation during strength-based or stair tasks, as all 95% confidence intervals overlapped.
Hamstrings to quadriceps co-activation by medial hamstrings, lateral hamstrings, and task. (1) load-acceptance, (2) heel-strike, (3) preparatory, prior to contact, (4) descent, (5) ascent, (6) step down, (7) step down with dual-task challenge, (8) step down with unstable platform perturbation, (9) step down with dual-task challenge and unstable platform perturbation, (10) reactive, following contact, (11) single-limb landing, and (12) double-limb landing. ACLR anterior cruciate ligament reconstruction, SD standard deviation, Std standard, CI confidence interval
3.5 Onset Timing
Four studies [35, 43, 56, 59] evaluated hamstrings EMG onset timing, 3 of which were meta-analyzed (Fig. 5) [43, 56, 59]. In this comparison, there were no differences between groups in either preparatory (i.e. feedforward, 1 study, MH: g = 0.16 [95% CI − 0.41, 0.72], LH: g = 0.11[95% CI − 0.46, 0.67]) or reactive (i.e. destabilizing platform, 2 studies, MH: g = 0.41[95% CI − 1.29, 2.10], LH: g = − 0.40 [95% CI − 0.86, 0.06]) hamstrings activation onset timing.
3.6 Electromechanical Delay
Two studies evaluated hamstrings EMD (Fig. 6) [47, 51]. Overall, individuals with ACLR demonstrated longer EMD than controls (MH: g = 1.78 [95% CI 0.81, 2.75], RMD = 27.31 ms [95% CI 19.85, 34.77]; LH: g = 0.85 [95% CI 0.29, 1.41], RMD = 20.50 ms [95% CI − 10.47, 51.48]).
3.7 Time to Peak Muscle Activity
Three studies evaluated hamstrings EMG time to peak muscle activity during a jump landing task (Fig. 7) [31, 43, 49]. Overall, there was no difference in hamstrings time to peak muscle activity between groups (MH: g = 0.06 [95% CI − 0.76, 0.88], LH: g = 0.41 [95% CI − 0.21, 1.03], US: g = − 0.06 [95% CI − 0.82, 0.70]).
3.8 Heterogeneity of Studies
Overall comparisons for each outcome of interest demonstrated moderate (amplitude [% peak], EMD, time to peak activity) or substantial (amplitude [% MVIC], onset timing) heterogeneity upon meta-analysis. Additionally, there was high variability in tasks within the EMG amplitude, onset timing, co-activation, and time to peak muscle activity studies. As a result, emphasis on interpretation is placed on task comparisons (sub-comparisons) in each outcome.
4 Discussion
This systematic review and meta-analysis presents a wide spectrum of EMG-derived hamstrings neuromuscular impairments in individuals with ACLR compared to uninjured controls. Those with ACLR demonstrated higher (moderate to large effect) hamstrings EMG amplitude (% MVIC) and co-activation during gait and stair ambulation compared to controls. Interestingly, MH EMG amplitude during single limb jump landing activities differs based on the normalization procedure (higher in ACLR group normalized to % MVIC, and lower in studies normalized to % peak activity). Additionally, there is a large prolongation of EMD during knee flexion and a large increase in hamstrings co-activation during knee extension in individuals with ACLR. Although MH co-activation demonstrated a larger magnitude effect than LH during gait, there were no other significant differences between muscles for any outcome or task. Most meta-analyzed studies comparing EMG amplitude between individuals with ACLR and controls varied in the task assessed, owing to the heterogeneity of results. Overall, the included studies varied in methodological quality, muscles evaluated, and task, resulting in some outcomes of interest having fewer included studies. The results and the clinical implications of the findings, including percent activation differences, are discussed by category.
4.1 EMG Amplitude
EMG amplitude results varied by normalization technique, as well as task subgrouping (Table 3). Most notably, with double-limb and single-limb jumping tasks, the differences in normalization technique (whether to % MVIC or % peak) resulted in contrasting effects. In these comparisons, it appears hamstrings activity is higher (as % MVIC) during double-limb landing in an individual with ACLR yet is no different when normalized to the peak of the dynamic trial. Further, MH activity is higher when normalized to MVIC but lower during single-limb landing in individuals with ACLR compared to the rest of the dynamic trial (i.e. other phases of the jump). Although speculative, this dichotomy conveys that EMG amplitude must be interpreted with respect to the normalization procedure. For example, a weaker individual (with lower MVIC or volitional activation) may use a greater proportion of their maximal muscle activation than a stronger person to complete a standardized task. Thus, the weaker individual would exhibit higher percent activation during the task when normalized to MVIC compared to relative activation. Impairments in hamstrings strength are prevalent in individuals following ACLR [64] so differences in normalization may help explain the difference between groups. As normalization to MVIC was most common in these results and is reported to be more reliable than the alternative [65], differences should be considered while interpreting the remaining amplitude results.
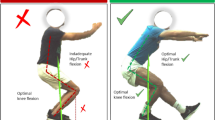
The LH of individuals with ACLR demonstrated higher EMG amplitude during gait (large effect, g = 1.13, RMD = 7.17%) and stair ambulation (large effect, g = 0.86, RMD = 3.01%). The MH demonstrated only a moderate effect during stair-related tasks (moderate effect, g = 0.53, RMD = 1.87%) although the confidence intervals did overlap, indicating the difference between hamstring muscles is inconclusive. There is a pattern of greater hamstrings activity after ACLR as dynamic joint stability demands increase (e.g. gait, stairs, and jump landing), but not during static tasks (e.g. isolated knee flexion, single limb stance, kicking). Greater amplitude during tasks that demand greater dynamic stability may indicate demands for a greater proportion of hamstrings neural drive (as % of theoretical maximum during MVIC) or an adaptive upregulation of hamstrings activity in an effort to preserve dynamic joint stability following ACLR [16, 17, 22]. Considering the nuances of the normalization technique (e.g., whether differences in raw amplitude [1.87–10.76%] between groups represent the same activity), intra-limb normalization via co-activation may be more clinically interpretable.
4.2 Co-activation
Individuals with ACLR demonstrated greater co-activation during isometric knee extension, gait, and stair ambulation. Specifically, voluntary quadriceps activation during knee extension was characterized by higher hamstrings co-activation in MH, LH, and US comparisons (large effects, g = 0.85–1.34, RMD = 1.03–12.90%), indicating that hamstrings co-contraction may dampen the mechanical efficiency of the quadriceps in those with ACLR. The effect was also presented during gait, with the MH (g = 3.57, RMD = 10.72%) demonstrating higher co-activation than the LH (g = 1.45, RMD = 3.84%), and stair ambulation (moderate to large effects, g = 0.43–1.04, RMD = 2.75–5.90%). Hamstring-to-quadriceps co-activation is important to provide stability to the knee and reduce the amount of tensile force placed on the ACL or graft tissue. Through simulated work in cadaveric knees [66], we can appreciate that greater hamstrings co-activation is associated with decreased strain in the ACL. Therefore, these results may indicate that greater levels of co-activation occur as an adaptive strategy to better resist anterior tibial shear and rotation during functional tasks to maintain dynamic knee stability. Recent work [14] provides evidence to this effect, reporting that individuals with greater co-activation were less likely to suffer graft rupture. Other authors [67] found similar associations between intralimb muscle strength (hamstring-to-quadriceps ratio) and risk of graft rupture, which collectively implicate intralimb muscle function and imbalance in secondary injury prevention.
Interestingly, co-activation was 2.75–10.72% higher during activities of daily living (e.g. walking and stairs), but not more dynamic athletic tasks (e.g. double-limb or single-limb jumping), suggesting those with ACLR may fail to effectively carry-over this compensation to a sport where it may be desirable for improved knee stability. Conversely, greater co-activation results in increased compressive forces about the knee and lesser knee flexion–extension excursion during gait [9, 13], representing a negative consequence of this strategy during highly repetitive activities of daily living as these impairments have been linked to cartilage degeneration and incidence of post-traumatic knee osteoarthritis [9, 68]. Furthermore, greater MH co-activation has been associated with greater medial tibiofemoral joint loading, which may contribute to reports of higher incidence of medial compartment post-traumatic osteoarthritis [22, 69].
4.3 Onset Timing
Hamstrings muscle onset timing was not different between groups regardless of reactive (e.g. reflexive) or preparatory (e.g. planned) paradigm [43, 56]. As a dynamic stabilizer, the time from perturbation to the onset of hamstrings muscle activity is important for active stabilization against anterior tibial shear and rotation [22, 59]. It is theorized that altered joint afference following ACL injury contributes to the delayed reaction of the lower extremity musculature [70, 71]. Here, large delays in reactivity were seen with a larger degree of platform perturbation (30° inversion + 10° plantarflexion [56] vs. 20° degree inversion [59]) despite both samples being similarly removed from ACLR surgery (approximately 9 months). The absence of an overall effect may suggest that reactive muscle activation is a modifiable neuromuscular impairment in individuals with ACLR. However, specific interventions to achieve this remain unclear. Considering the complexity of both reactive and preparatory aspects of the sport, the functional implications of this nuanced relationship are hard to define and should be the subject of future research.
4.4 Electromechanical Delay
Both included studies demonstrated longer EMD in individuals with ACLR compared to controls, with larger delay in the MH (g = 1.78, RMD = 27.31 ms) compared to LH (g = 0.85, RMD = 20.50 ms). In vivo evidence suggests that peak ACL strain occurs in the first 100 ms of joint loading during dynamic tasks (e.g. cutting, landing) [72], suggesting the need to rapidly develop muscle activity and subsequent force production to protect the ACL. Increased time between the onset of EMG activity and force production is associated with a lower rate of force production and a delay in muscular stabilization about a joint (e.g. dynamic joint stabilization). Considering both studies utilized isolated knee flexion exercise to assess this outcome, it is not clear whether these deficits translate to more dynamic activities relevant to ACL re-injury (e.g. jump landing). Despite this, longer EMD might be implicated in high graft failure rates seen in individuals with ACLR. This is especially true considering the largest effect in the MH, which helps resist external tibial rotation and knee valgus associated with ACL strain [22]. There is a need to identify clinical interventions which may target this impairment. Additionally, future studies utilizing finite element modeling with EMG may help to derive this outcome during functional tasks.
4.5 Time to Peak Muscle Activity
These findings indicated no difference in hamstrings time to peak muscle activity between groups. Clinically, this may represent a normal time to peak muscle activity during jump landing maneuvers in individuals with ACLR. However, time to peak activity is nuanced by potential differences in EMG amplitude between groups. For example, Ortiz et al. [31] reported similar hamstrings amplitude between groups during single limb jump landing, but those with ACLR demonstrated significantly faster time to peak hamstrings activity, which suggests more rapid progression of activation (i.e. higher relative activation in same elapsed time). As discussed previously, with peak ACL strain occurring in the first 100 ms of knee joint loading [72], this neural facilitation strategy may be indicated to protect the joint. Future research should normalize time to peak muscle activity to rate of activation to better appreciate the effectiveness of muscle activation strategies that preserve time to peak muscle activity.
4.6 Methodological Quality, Limitations, and Directions for Future Research
There were many methodological limitations identified using the mNOS, with only eight of the included studies having adequately described the selection of controls (mNOS item 3). Most notably, this could result in inappropriate matching of participants across groups, which may have had an influence on the results. This limitation should be addressed in future research. Further, five studies could not be included in the meta-analysis; however, their reported results did not differ from the noted findings.
All six overall comparisons within this meta-analysis were characterized by moderate to substantial heterogeneity, which indicates a large degree of variability in the results. This is likely a representation of the wide range of functional tasks and inclusion of both MH and LH results represented in the collective sample. We have attempted to address this limitation by reporting the more conservative random effects for all comparisons. We have included subgrouping by hamstring musculature and functional task in an effort to demonstrate the drivers of this heterogeneity for each outcome of interest. However, this reduces the number of studies in each sub comparison. Van Tulder et al. [73] recommends incorporating methodological quality, I2 statistic, and number of studies to establish the level of evidence. In so doing, sub comparisons of EMG amplitude and co-activation during stair ambulation and double and single limb jumping, as well as EMG onset timing during preparatory reactions, can be classified as moderate evidence (i.e., pooled results including at least one of high quality or multiple homogenous studies of moderate or low quality). EMD and time to peak activity results can also be classified as moderate evidence. Conversely, all other sub comparisons are classified as limited (i.e., results from multiple heterogeneous moderate or low-quality studies) or very limited evidence (i.e., results from one moderate or low-quality study), and as such, caution should be used in interpreting these comparisons.
Demographic factors such as sex, age, and graft-type are reported to influence recovery with ACLR [74]. However, the influence of these factors on hamstrings neuromuscular function is not fully understood. To this end, the included sample is largely male (approximately 63%), which is not representative of the reported prevalence between sexes and threatens the generalizability of these findings. Regarding graft type, we set out to primarily include individuals who underwent ACLR with autograft in this review. However, five studies [9, 38, 41, 42, 53] included several individuals who received an allograft. Due to the small number (n = 12, 1.7% of total ACLR sample) with reference to the included sample, we felt this was an acceptable exception; exclusion of these data would have also resulted in the removal of a large number of individuals with autograft (n = 111, 15.8% of total ACLR sample). Additionally, individuals with HT autograft are known to have larger deficits in hamstrings muscle strength after ACLR compared to those with PT autograft [75]. Here, neuromuscular impairments were observed despite a heterogeneous sample (35.9% PT, 48.6% HT). Sex and graft-type subgroup analyses were not undertaken as part of the review and remain an area of further research.
Although outside the scope of this report, neuromuscular abnormalities may be present prior to and thus contribute to initial ACL injury. As all but two studies [14, 35] identified in this search were cross-sectional, longitudinal studies describing the neuromuscular impact of initial ACL injury and evaluating the role of clinical interventions which address these hamstrings muscle dysfunctions are still needed to further our understanding in this regard. On this note, the primary findings of Palmieri-Smith et al. [14] suggest that higher hamstrings activity during single-limb jump landing may be protective against subsequent injury in those with ACLR. Secondly, due to a lack of data in the literature, comparison to the contralateral limb was not included in this review. Inter-limb comparisons within individuals would be useful to determine if hamstrings neuromuscular function is impaired bilaterally with ACLR. Lastly, future work should determine the interaction between co-activation (intralimb ratio of EMG amplitude) and hamstrings-to-quadriceps ratio (intralimb ratio of muscle strength) to clarify the clinical implications of intralimb function.
5 Conclusion
Moderate quality evidence suggests that individuals with ACLR demonstrate higher EMG amplitude (1.87–10.76%) and hamstrings-to-quadriceps co-activation (2.75–10.72%) during gait and stair-related tasks compared to controls. Additionally, hamstrings co-activation was higher during knee extension (1.03–12.90%), suggesting less efficient isolated quadriceps activation. Moderate quality evidence also suggests that individuals with ACLR demonstrate longer EMD (20.50–27.31 ms) of the hamstrings musculature with a greater negative impact in the MH than the LH. Collectively, these neuromuscular adaptations align with known clinical impairments (e.g. decreased quadriceps and hamstrings muscle strength) and are theorized to contribute to poor outcomes seen in this population, such as re-injury and post-traumatic osteoarthritis. These impairments warrant attention in rehabilitation from ACLR.
References
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–70. https://doi.org/10.1177/0363546514542796.
Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–52. https://doi.org/10.1136/bjsports-2013-093398.
Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–43. https://doi.org/10.1177/0363546510384798.
Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–32. https://doi.org/10.1177/0363546516651845.
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–76. https://doi.org/10.1177/0363546515621554.
Harris KP, Driban JB, Sitler MR, Cattano NM, Balasubramanian E, Hootman JM. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: a systematic review. J Athl Train. 2017;52(6):507–17. https://doi.org/10.4085/1062-6050-49.3.89.
Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806–19. https://doi.org/10.4085/1062-6050-49.3.35.
Palmieri-Smith RM, McLean SG, Ashton-Miller JA, Wojtys EM. Association of quadriceps and hamstrings cocontraction patterns with knee joint loading. J Athl Train. 2009;44(3):256–63. https://doi.org/10.4085/1062-6050-44.3.256.
Blackburn T, Pietrosimone B, Goodwin JS, Johnston C, Spang JT. Co-activation during gait following anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2019;67:153–9. https://doi.org/10.1016/j.clinbiomech.2019.05.010.
Pietrosimone B, Pfeiffer SJ, Harkey MS, Wallace K, Hunt C, Blackburn JT, et al. Quadriceps weakness associates with greater T1rho relaxation time in the medial femoral articular cartilage 6 months following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2632–42. https://doi.org/10.1007/s00167-018-5290-y.
Pietrosimone B, Seeley MK, Johnston C, Pfeiffer SJ, Spang JT, Blackburn JT. Walking ground reaction force post-ACL reconstruction: analysis of time and symptoms. Med Sci Sports Exerc. 2019;51(2):246–54. https://doi.org/10.1249/MSS.0000000000001776.
Palmieri-Smith RM, Thomas AC. A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev. 2009;37(3):147–53. https://doi.org/10.1097/JES.0b013e3181aa6669.
MacWilliams BA, Wilson DR, DesJardins JD, Romero J, Chao EY. Hamstrings cocontraction reduces internal rotation, anterior translation, and anterior cruciate ligament load in weight-bearing flexion. J Orthop Res. 1999;17(6):817–22. https://doi.org/10.1002/jor.1100170605.
Palmieri-Smith RM, Strickland M, Lepley LK. Hamstring muscle activity after primary anterior cruciate ligament reconstruction-a protective mechanism in those who do not sustain a secondary injury? A preliminary study. Sports Health. 2019;11(4):316–23. https://doi.org/10.1177/1941738119852630.
Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–9.
Basmajian JV, de Luca CJ. Muscles alive: their functions revealed by electromyography. 5th ed. Baltimore: Williams & Wilkins; 1985.
NIOSH. Selected topics in surface electromyography for use in the occupational setting: expert perspectives 1999. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 91-1001999.
Scheurer SA, Sherman DA, Glaviano NR, Ingersoll CD, Norte GE. Corticomotor function is associated with quadriceps rate of torque development in individuals with ACL surgery. Exp Brain Res. 2020;238(2):283–94. https://doi.org/10.1007/s00221-019-05713-w.
Norte GE, Hertel J, Saliba SA, Diduch DR, Hart JM. Quadriceps neuromuscular function in patients with anterior cruciate ligament reconstruction with or without knee osteoarthritis: a cross-sectional study. J Athl Train. 2018;53(5):475–85. https://doi.org/10.4085/1062-6050-102-17.
Kuenze C, Hertel J, Saliba S, Diduch DR, Weltman A, Hart JM. Clinical thresholds for quadriceps assessment after anterior cruciate ligament reconstruction. J Sport Rehabil. 2015;24(1):36–46. https://doi.org/10.1123/jsr.2013-0110.
Oiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthr Cartil. 2015;23(2):171–7. https://doi.org/10.1016/j.joca.2014.10.008.
Flaxman TE, Alkjaer T, Simonsen EB, Krogsgaard MR, Benoit DL. Predicting the functional roles of knee joint muscles from internal joint moments. Med Sci Sports Exerc. 2017;49(3):527–37. https://doi.org/10.1249/MSS.0000000000001125.
Flaxman TE, Smith AJ, Benoit DL. Sex-related differences in neuromuscular control: Implications for injury mechanisms or healthy stabilisation strategies? J Orthop Res. 2014;32(2):310–7. https://doi.org/10.1002/jor.22510.
Kim HJ, Lee JH, Ahn SE, Park MJ, Lee DH. Influence of anterior cruciate ligament tear on thigh muscle strength and hamstring-to-quadriceps ratio: a meta-analysis. PLoS ONE. 2016;11(1):e0146234. https://doi.org/10.1371/journal.pone.0146234.
Norte GE, Knaus KR, Kuenze C, Handsfield GG, Meyer CH, Blemker SS, et al. MRI-based assessment of lower-extremity muscle volumes in patients before and after ACL reconstruction. J Sport Rehabil. 2018;27(3):201–12. https://doi.org/10.1123/jsr.2016-0141.
Delahunt E, McGroarty M, De Vito G, Ditroilo M. Nordic hamstring exercise training alters knee joint kinematics and hamstring activation patterns in young men. Eur J Appl Physiol. 2016;116(4):663–72. https://doi.org/10.1007/s00421-015-3325-3.
Bencke J, Aagaard P, Zebis MK. Muscle activation during ACL injury risk movements in young female athletes: a narrative review. Front Physiol. 2018. https://doi.org/10.3389/fphys.2018.00445.
Hootman JM, Driban JB, Sitler MR, Harris KP, Cattano NM. Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011;2(2):110–8. https://doi.org/10.1002/jrsm.41.
Open-Source. Engauge digitizer software. In: Mitchell M, Muftakhidinov B, Winchen T, van Schaik B, Wilms A, Kensington et al., editors.: GitHub; 2015. p. Windows 10.
Briem K, Ragnarsdottir AM, Arnason SI, Sveinsson T. Altered medial versus lateral hamstring muscle activity during hop testing in female athletes 1–6 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):12–7. https://doi.org/10.1007/s00167-014-3333-6.
Ortiz A, Capo-Lugo CE, Venegas-Rios HL. Biomechanical deficiencies in women with semitendinosus-gracilis anterior cruciate ligament reconstruction during drop jumps. PM R. 2014;6(12):1097–106. https://doi.org/10.1016/j.pmrj.2014.07.003.
Telianidis S, Perraton L, Clark RA, Pua Y-H, Fortin K, Bryant AL. Diminished sub-maximal quadriceps force control in anterior cruciate ligament reconstructed patients is related to quadriceps and hamstring muscle dyskinesia. J Electromyogr Kinesiol. 2014;24(4):513–9.
Rudroff T. Functional capability is enhanced with semitendinosus than patellar tendon ACL repair. Med Sci Sports Exerc. 2003;35(9):1486–92. https://doi.org/10.1249/01.MSS.0000084425.07852.7D.
Swanik CB, Lephart SM, Giraldo JL, Demont RG, Fu FH. Reactive muscle firing of anterior cruciate ligament-injured females during functional activities. J Athl Train. 1999;34(2):121–9.
Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28(3):336–44. https://doi.org/10.1177/03635465000280030901.
Demont RG, Lephart SM, Giraldo JL, Swanik CB, Fu FH. Muscle preactivity of anterior cruciate ligament-deficient and -reconstructed females during functional activities. J Athl Train. 1999;34(2):115–20.
Ciccotti MG, Kerlan RK, Perry J, Pink M. An electromyographic analysis of the knee during functional activities. II. The anterior cruciate ligament-deficient and -reconstructed profiles. Am J Sports Med. 1994;22(5):651–8. https://doi.org/10.1177/036354659402200513.
Ortiz A, Olson S, Trudelle-Jackson E, Rosario M, Venegas HL. Landing mechanics during side hopping and crossover hopping maneuvers in noninjured women and women with anterior cruciate ligament reconstruction. PM R. 2011;3(1):13–20. https://doi.org/10.1016/j.pmrj.2010.10.018.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: L. Erlbaum Associates; 1988.
Higgins JPT, Green S, Cochrane C. Cochrane handbook for systematic reviews of interventions. Chichester, Hoboken: Wiley-Blackwell; 2008.
Pamukoff DN, Pietrosimone BG, Ryan ED, Lee DR, Blackburn JT. Quadriceps function and hamstrings co-activation after anterior cruciate ligament reconstruction. J Athl Train. 2017;52(5):422–8. https://doi.org/10.4085/1062-6050-52.3.05.
Jordan MJ, Aagaard P, Herzog W. Asymmetry and thigh muscle coactivity in fatigued anterior cruciate ligament-reconstructed elite skiers. Med Sci Sports Exerc. 2017;49(1):11–20. https://doi.org/10.1249/MSS.0000000000001076.
Bryant AL, Newton RU, Steele J. Successful feed-forward strategies following ACL injury and reconstruction. J Electromyogr Kinesiol. 2009;19(5):988–97. https://doi.org/10.1016/j.jelekin.2008.06.001.
Bryant AL, Pua YH, Clark RA. Morphology of knee extension torque-time curves following anterior cruciate ligament injury and reconstruction. J Bone Jt Surg Am. 2009;91(6):1424–31. https://doi.org/10.2106/JBJS.H.01335.
Kasovic M, Mejovsek M, Matkovic B, Jankovic S, Tudor A. Electromyographic analysis of the knee using fixed-activation threshold after anterior cruciate ligament reconstruction. Int Orthop. 2011;35(5):681–7. https://doi.org/10.1007/s00264-010-1050-4.
Rush JL, Norte GE, Lepley AS. Limb differences in hamstring muscle function and morphology after anterior cruciate ligament reconstruction. Phys Ther Sport. 2020;45:168–75. https://doi.org/10.1016/j.ptsp.2020.06.012.
Ristanis S, Tsepis E, Giotis D, Stergiou N, Cerulli G, Georgoulis AD. Electromechanical delay of the knee flexor muscles is impaired after harvesting hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(11):2179–86. https://doi.org/10.1177/0363546509340771.
Árnason S, Birnir B, Guðmundsson T, Guðnason G, Briem K. Medial hamstring muscle activation patterns are affected 1–6 years after ACL reconstruction using hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1024–9.
Coats-Thomas MS, Miranda DL, Badger GJ, Fleming BC. Effects of ACL reconstruction surgery on muscle activity of the lower limb during a jump-cut maneuver in males and females. J Orthop Res. 2013;31(12):1890–6. https://doi.org/10.1002/jor.22470.
Cordeiro N, Cortes N, Fernandes O, Diniz A, Pezarat-Correia P. Dynamic knee stability and ballistic knee movement after ACL reconstruction: an application on instep soccer kick. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1100–6. https://doi.org/10.1007/s00167-014-2894-8.
Freddolini M, Battaglioli A, Chiechi F, Placella G, Georgoulis A, Cerulli G, et al. Electromechanical delay of the knee flexor muscles after anterior cruciate ligament reconstruction using semitendinosus tendon. Sports Biomech. 2015;14(4):384–93. https://doi.org/10.1080/14763141.2015.1086425.
Hall M, Stevermer CA, Gillette JC. Muscle activity amplitudes and co-contraction during stair ambulation following anterior cruciate ligament reconstruction. J Electromyogr Kinesiol. 2015;25(2):298–304. https://doi.org/10.1016/j.jelekin.2015.01.007.
Harput G, Howard JS, Mattacola C. Comparison of muscle activation levels between healthy individuals and persons who have undergone anterior cruciate ligament reconstruction during different phases of weight-bearing exercises. J Orthop Sports Phys Ther. 2016;46(11):984–92. https://doi.org/10.2519/jospt.2016.5896.
Heller BM, Pincivero DM. The effects of ACL injury on lower extremity activation during closed kinetic chain exercise. J Sports Med Phys Fit. 2003;43(2):180–8.
Perraton L, Clark R, Crossley K, Pua YH, Whitehead T, Morris H, et al. Impaired voluntary quadriceps force control following anterior cruciate ligament reconstruction: relationship with knee function. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1424–31. https://doi.org/10.1007/s00167-015-3937-5.
Pincheira PA, Silvestre R, Armijo-Olivo S, Guzman-Venegas R. Ankle perturbation generates bilateral alteration of knee muscle onset times after unilateral anterior cruciate ligament reconstruction. PeerJ. 2018;6(7):e5310. https://doi.org/10.7717/peerj.5310.
Flaxman TE, Alkjaer T, Smale KB, Simonsen EB, Krogsgaard MR, Benoit DL. Differences in EMG-moment relationships between ACL-injured and uninjured adults during a weight-bearing multidirectional force control task. J Orthop Res. 2019;37(1):113–23. https://doi.org/10.1002/jor.24145.
Lepley LK, Thomas AC, McLean SG, Palmieri-Smith RM. Fatigue’s lack of effect on thigh-muscle activity in anterior cruciate ligament-reconstructed patients during a dynamic-landing task. J Sport Rehabil. 2013;22(2):83–92. https://doi.org/10.1123/jsr.22.2.83.
San Martín-Mohr C, Cristi-Sánchez I, Pincheira PA, Reyes A, Berral FJ, Oyarzo C. Knee sensorimotor control following anterior cruciate ligament reconstruction: a comparison between reconstruction techniques. PLoS ONE. 2018;13(11):e0205658. https://doi.org/10.1371/journal.pone.0205658.
Smeets A, Verschueren S, Staes F, Vandenneucker H, Claes S, Vanrenterghem J. Athletes with an ACL reconstruction show a different neuromuscular response to environmental challenges compared to uninjured athletes. Gait Posture. 2021;83:44–51. https://doi.org/10.1016/j.gaitpost.2020.09.032.
Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):2–14. https://doi.org/10.1007/s00167-007-0427-4.
Pereira HM, Nowotny AH, Santos AB, Cardoso JR. Electromyographic activity of knee stabilizer muscles during six different balance board stimuli after anterior cruciate ligament surgery. Electromyogr Clin Neurophysiol. 2009;49(2–3):117–24.
Mantashloo Z, Letafatkar A, Moradi M. Vertical ground reaction force and knee muscle activation asymmetries in patients with ACL reconstruction compared to healthy individuals. Knee Surgery Sports Traumatol Arthrosc. 2020;28(6):2009–14. https://doi.org/10.1007/s00167-019-05743-5.
Cristiani R, Mikkelsen C, Forssblad M, Engström B, Stålman A. Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3461–70. https://doi.org/10.1007/s00167-019-05396-4.
Knutson LM, Soderberg GL, Ballantyne BT, Clarke WR. A study of various normalization procedures for within day electromyographic data. J Electromyogr Kinesiol. 1994;4(1):47–59. https://doi.org/10.1016/1050-6411(94)90026-4.
Withrow TJ, Huston LJ, Wojtys EM, Ashton-Miller JA. Effect of varying hamstring tension on anterior cruciate ligament strain during in vitro impulsive knee flexion and compression loading. J Bone Jt Surg Am. 2008;90(4):815–23. https://doi.org/10.2106/JBJS.F.01352.
Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–51. https://doi.org/10.1136/bjsports-2015-095908.
Khandha A, Manal K, Wellsandt E, Capin J, Snyder-Mackler L, Buchanan TS. Gait mechanics in those with/without medial compartment knee osteoarthritis 5 years after anterior cruciate ligament reconstruction. J Orthop Res. 2017;35(3):625–33. https://doi.org/10.1002/jor.23261.
Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–57. https://doi.org/10.1177/0363546514526139.
Ward S, Pearce AJ, Pietrosimone B, Bennell K, Clark R, Bryant AL. Neuromuscular deficits after peripheral joint injury: a neurophysiological hypothesis. Muscle Nerve. 2015;51(3):327–32. https://doi.org/10.1002/mus.24463.
Nyland J, Gamble C, Franklin T, Caborn DNM. Permanent knee sensorimotor system changes following ACL injury and surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1461–74. https://doi.org/10.1007/s00167-017-4432-y.
Weinhandl JT, Earl-Boehm JE, Ebersole KT, Huddleston WE, Armstrong BS, O’Connor KM. Anticipatory effects on anterior cruciate ligament loading during sidestep cutting. Clin Biomech (Bristol, Avon). 2013;28(6):655–63. https://doi.org/10.1016/j.clinbiomech.2013.06.001.
van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review G. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–9. https://doi.org/10.1097/01.BRS.0000065484.95996.AF.
Kuenze C, Pietrosimone B, Lisee C, Rutherford M, Birchmeier T, Lepley A, et al. Demographic and surgical factors affect quadriceps strength after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):921–30. https://doi.org/10.1007/s00167-018-5215-9.
Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD. The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):768–80. https://doi.org/10.1007/s00167-010-1357-0.
Harput G, Soylu AR, Ertan H, Ergun N, Mattacola CG. Effect of gender on the quadriceps-to-hamstrings coactivation ratio during different exercises. J Sport Rehabil. 2014;23(1):36–43. https://doi.org/10.1123/jsr.2012-0120.
Blackburn JT, Bell DR, Norcross MF, Hudson JD, Engstrom LA. Comparison of hamstring neuromechanical properties between healthy males and females and the influence of musculotendinous stiffness. J Electromyogr Kinesiol. 2009;19(5):e362–9. https://doi.org/10.1016/j.jelekin.2008.08.005.
Acknowledgements
The authors would like to acknowledge all participants who contributed to the original research reviewed in this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
David Sherman, Neal Glaviano and Grant Norte declare that they have no conflicts of interest relevant to the content of this review.
Standards of reporting
PRISMA.
Ethics approval
This is a systematic review. The University of Toledo Institutional Review Board for Biomedical Research has confirmed that no ethical approval is required.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
All authors (DAS, NRG, and GEN) have contributed equally and demonstrated significant involvement in the planning and carrying out of this review and manuscript. Material preparation and data extraction were performed by DAS. Methodological quality review was performed by DAS and NRG. Data analysis was performed by DAS. The first draft of the manuscript was written by DAS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sherman, D.A., Glaviano, N.R. & Norte, G.E. Hamstrings Neuromuscular Function After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med 51, 1751–1769 (2021). https://doi.org/10.1007/s40279-021-01433-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01433-w