Abstract
The aim of this study was to establish whether there are any electromyographic (EMG) differences after two different surgical techniques in two years follow-up after anterior cruciate ligament (ACL) reconstruction. Study participants were divided into three groups. The control group included healthy athletes (C), the first study group (E1) consisted of injured athletes who were treated by ACL reconstruction using patellar tendon graft and the second study group (E2) comprised injured athletes treated by gracilis and semitendinosus tendon graft. The threshold of muscle activity was defined as 30% of maximum amplitude of EMG signal medial envelope of individual muscles in the control group. Two years after reconstruction, the E2 group achieved the maximum amplitude of biceps femoris muscle signal in the takeoff phase statistically significantly later than the E1 group (0.0166, p = 0.05 and 0.015152, p = 0.05/3 = 0.016), whereas the rectus femoris muscle in the flight phase in the E2 group improved statistically significantly earlier than in the C group (0.0393, p = 0.05 and 0.025974, p = 0.05/3 = 0.016). The results of this study show particularly statistically significant differences between observed surgery techniques, which led to the change of the neuromuscular pathway during simple and controlled knee movements even two years after ACL reconstructions in athletes who returned to active training. These disturbances of muscle work coordinations in the knee joint could be tied to the function and location from which the graft was taken rather than the quality of the transplant itself. This may result in an increased risk of repeated knee injury, including potential permanent health consequences in athletes. Based on the results of this research, we were unable to establish which of the presented ACL reconstruction techniques is more appropriate. This study may be useful for athletes and their coaches, who could plan, programme and adequately adjust their training process, thereby improving knee function in the best possible way, which in turn would maintain and extend athletes’ respective sports careers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most widespread sporting activity in the world is soccer, and the highest incidence of anterior cruciate ligament (ACL) injury has in fact been recorded in soccer, so it is not surprising that the most common injury forcing active soccer players to pause their sports activity is ACL rupture [1]. The goal of ACL reconstruction is clearly to reinstate the previous complete knee stability with proper muscle function and full knee mobility [17]. To achieve that, surgeons reconstruct the ruptured ACL, mostly applying one of two types of autografts: bone–patellar-tendon and bone and hamstring-tendon graft [7, 8, 22], although some other techniques are also in use [21]. In the 1970s and for next three decades, patellar tendon graft was the most popular choice. In the light of harvest site morbidity and postoperative stiffness associated with patellar tendon graft, many surgeons began to choose semitendinosus and gracilis graft [9, 16, 18]. The actual value of both methods is evaluated in various tests, mostly combining objective measurements and subjective patient opinions [2, 20, 23–25]. The most commonly used tests are the Single Assessment Numeric Evaluation Score, Lysholm Score, International Knee Documentation Committee Score and Knee Injury and Osteoarthritis Outcome Score [12]. Some authors, however, consider that conventional evaluation of ACL reconstruction with these tests is not good enough, as they cannot imitate the situations in modern sports that are extremely demanding of the knee. For a realistic evaluation of ACL reconstruction, it is necessary to introduce dynamic functional stability tests. In their biomechanical – kinematic study, Chouliaras et al. [5] described one such test: it was demonstrated that the knee reconstructed by the hamstring method cannot prevent excessive internal lower-leg rotation on landing and in strong upper-body rotation. It was previously established that reconstruction by the patellar method also fails to sufficiently stabilise the knee in similar situations. The authors therefore concluded that neither of these grafts provides sufficient stabilisation of tibial rotation and that further improvements in technique of ACL reconstruction are necessary to achieve better anatomical position and improve function. In our view, further biomechanical analyses are essential to determine the actual state of muscle function following ACL reconstruction, especially in the highly challenging situations of modern sports.
The aim of the research was to establish whether there are any qualitative neuromuscular changes and departures from healthy movement pattern shown in the surface electromyographic (EMG) signal and to what extent such changes and deviations differ in terms of the applied surgery technique two years after ACL reconstruction. The study considered two most commonly applied reconstruction techniques using grafts of either semitendinosus or gracilis muscles or the medial third of the patellar ligament. As opinions about which of the two grafts is more appropriate in highly physically demanding individuals or athletes still differ, the results of this study could be used to improve rehabilitation programmes and as additional criteria for selecting the reconstruction method (i.e. for defining the criteria for such selection). This would certainly contribute to the quality of recovery and enable athletes to resume their professional sports activities earlier [14, 19].
Methods
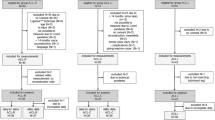
The measurement protocol comprised two points in time that are important in athletes’ rehabilitation and training. The initial measurement was conducted seven days prior to the reconstruction, during the preparation of the individual for surgery. The respective reconstruction method for individuals was chosen by random sampling. The second measurement took place two years after ACL reconstruction. In the period of the second measurement, the sports strains to which the individuals were exposed were identical to the strains prior to the injury. ACL reconstructions were performed under identical conditions, in the same clinic and by the same surgeon. The rehabilitation programme was also conducted under identical conditions, in the same polyclinic and under supervision of the same physical therapist [14]. Study participants were divided into three homogenous groups. The first study group consisted of injured athletes (soccer players) who were treated by ACL reconstruction technique including patellar tendon graft (E1). The second study group comprised injured soccer players treated by ACL reconstruction technique including gracilis and semitendinosus tendon graft (E2). The third group (control group) comprised healthy soccer players (C). The groups each consisted of ten individuals, and the basic descriptive statistics for anthropometric characteristics are shown in Table 1.
Signal samples were measured original surface (EMG) signals of the four dominant knee muscles (rectus femoris, vastus medialis, vastus lateralis and biceps femoris) measured whilst executing the motor task of single-leg vertical jump. In recording the EMG signal, the electrodes were positioned on the individual’s body in line with the SENIAM protocol [10, 11]. Single-leg vertical jump was chosen as it connects a large number of specific movements and techniques occurring in numerous sports or activities. In addition, this jump isolates muscular operation and activity of the individual knee joint where the impact of the other leg is not possible [13, 15].
Participants performed the task three times with one leg, but further analysis included only one measurement for each athlete, respectively. The motor task was divided into five characteristic phases identified through monitoring of the vertical component of the ground reaction force on a Kistler platform [19]. The crucial (and also the central) part of the signal was defined as the moment of re-established contact with the ground after the flight phase. In the time domain, the following phases of the single-leg vertical jump were defined, their duration being expressed as the percentage of jump-cycle duration: prejump, takeoff, flight, landing 1 and landing 2 (Fig. 1). The jump was analysed over its entire duration, and subsequent analysis of individual jump phases were conducted. Signal processing was done with MATLAB software.
Review of vertical jump phases defined by the vertical component of the ground reaction force and duration of these phases expressed as the percentage of overall cycle duration of 4 s. The phases include prejump from 0–16% (a), takeoff from 16–45% (b), flight from 45–51% (c), landing 1 from 51–61% (d) and landing 2 from 61–100% (e)
The surface EMG signal was recorded using the multichannel EMG device (TELEMG, BTS) and electrodes placed in compliance with the SENIAM protocol. The measuring period for single jumps was 4 s (2 s before and 2 s after the first contact with the landing base), with sampling frequency of 1,000 Hz. First, the signal was high-pass filtered with a fifth-order Butterworth filter with 15 Hz frequency in order to eliminate displacement artefacts. After the displacement artefacts were removed, signals dominated by various artefacts were excluded by visual inspection of the recorded signal and measurements of the same individuals were repeated. The remaining signals were full-wave-corrected and low-pass-filtrated with fifth-order Butterworth filter of 5 Hz frequency to obtain signal envelopes. Time normalisation of the signal was conducted, i.e. jump duration was shown in the range of 0–100%. The threshold of muscle activity was defined as 30% of maximum amplitude of EMG signal medial envelope of individual muscles in the control group. Sections of EMG signal with amplitude exceeding the defined threshold were considered to be muscle activity periods and were further analysed (Figs. 2 and 3).
Review of medial envelopes of electromyographic (EMG) signals in the patellar tendon graft (E1) group for the vastus medialis, vastus lateralis, rectus femoris and biceps femoris muscles. The x coordinate represents the duration of the jump time normalised to 0–1 (0–100% of the cycle). The y coordinate represents the medium envelope amplitude of the EMG signal (V). The entire envelope is marked black, and the periods of muscle activity are highlighted in red
Review of medial envelopes of electromyographic (EMG) signals in the gracilis and semitendinosus tendon graft (E2) group for vastus medialis, vastus lateralis, rectus femoris and biceps femoris muscles. The x coordinate represents the duration of the jump time normalised to 0–1 (0–100% of the cycle). The y coordinate represents the medium envelope amplitude of the EMG signal (V). The entire envelope is marked black, and the periods of muscle activity are highlighted in red
The following variables were defined for describing the signal envelopes obtained: the initial moment of muscle activation: tstart; the moment of the end of muscle activation: tend; the moment when the maximum amplitude of EMG signal is reached: tmax; and duration of activation expressed in the percentage of the duration of the observed jump section: tdur. Due to the specific features of the population and to the complex character of the study, resulting in a small number of samples per group, nonparametric statistical methods for data analysis were applied [4]. To detect differences between groups, Kruskal–Wallis test was used (α = 0.05). If statistically significant differences were found, further testing was conducted using the consecutive Mann–Whitney U test, applying Bonferroni [3, 6] correction (α = 0.05/3 = 0.0167). Statistical analysis was conducted with the StatSoft Statistica software.
Results
Statistical analysis of defined variables over the entire jump duration showed no statistically significant differences. We therefore conducted statistical analysis of the same variables defined per individual jump phases. The values obtained are presented in Table 2 and indicate muscle-function differences between groups. Kruskal–Wallis (0.0166, p = 0.05) and Mann Whitney (0.015152, p = 0.05/3 = 0.016) tests indicate a statistically significant delay of maximum amplitude in the E2 group but the same group reached the maximum amplitude significantly sooner in the flight phase. Also, Kruskal–Wallis (0.0433, p = 0.05) and Mann–Whitney U (0.025974, p = 0.05) tests indicated maximum amplitude statistically significantly sooner than in the E1 group.
Discussion
According to the latest study pursuing comparison of values of the two most common ACL reconstruction methods, none show any intrinsic differences in terms of subjective, objective and functional outcome [23]. The previous study, conducted a few years earlier, which included a seven year follow-up, showed significantly higher arthrosis rate in the patellar group, whilst all other parameters were the same. In their conclusion, the authors recommended the hamstrings autograft, although there was a tendency to rupture (not statistically significant) [20]. In their extensive study, Katabi et al. [16] emphasise the significantly higher occurrence of femoropatellar pain in the patellar group, but in view of the fact that at the same time knee stability was significantly higher in this patient group, the patellar method is recommended as the gold standard for ACL reconstruction in athletes, especially those practicing pivoting sports.
The analysis per jump phases conducted with nonparametric statistical analysis methods showed certain differences between groups. In the prejump (first phase) and landing 2 (last phase), no statistically significant differences were recorded. Two years after ACL reconstruction, statistically significant changes of muscle activity pattern were recorded; however, this time it was observed to be much greater on the back side of the upper leg. These differences are particularly evident in reaching the maximum amplitude of EMG signal of biceps femoris muscle in takeoff and flight phases. The group consisting of injured soccer players treated by ACL reconstruction with gracilis and semitendinosus tendon graft (E2) reached the maximum amplitude of the signal of biceps femoris muscle in the takeoff phase later than the group treated with patellar tendon graft. Reaching the maximum amplitude significantly sooner may be attributed to a certain muscle preactivation functioning as the prevention of overstraining the muscle in the most challenging phase, landing 1. Following the application of Bonferroni correction, there were no statistically significant differences, but taking into account the low sample count and the strictness of the criteria imposed by Bonferroni correction, we find these findings indicative; and despite the fact that no statistically significant changes in landing were observed, in our opinion, there was an overstrain of the biceps femoris muscle in this group. Maybe this phenomenon can be attributed to the lack of function of gracilis and semitendinosus muscles, which were the sources of autografts in this group. To compensate for the lack of one of the stabilisers in the joint, the biceps femoris muscle assumes the key role in stabilising lower-leg movement.
As opposed to results in the E2 group, ACL reconstruction with a patellar tendon graft (E1 group) was statistically significantly different from the control group in terms of the activity of frontal upper-leg musculature. According to the analysis the rectus femoris muscle was activated statistically significantly earlier in the flight phase. As in the E2 group, this difference may be attributed to autograft material harvest location, i.e. to a certain prevention of overstrain in the form of muscle preactivation prior to contact with the ground.
It is known that some phases of the vertical jump do not load the knee joint equally. Therefore, most neuromuscular differences were expected in the landing phase, when the ground forces are by far the greatest. No differences were recorded between groups during this phase, which leads to the conclusion that during the highest loads and demands on joint stability, both reconstruction techniques serve their purposes. The differences in neuromuscular activation are noticed in the previous, or flight, phase. This could be explained by the need for muscle pre-activation, which prepares the muscle for the stabilisation role, but it could also be taken as a sign that a particular muscle needs more time to perform the demanded activity. On the other hand, the most frequently mentioned muscle in the “Results” section is the biceps femoris, the function of which is still not restored or is somewhat modified at the time of measurement, which is noticeable in the maximal activation during takeoff time for the E1 group and in preparation for landing in the E2 group. The rectus femoris muscle in E1 in comparison with the healthy group starts activation in the flight phase significantly earlier, probably for the same reasons as biceps femoris.
The results of this study represent fine diagnostics and the current condition of the knee joint, which are not noticeable to the athlete or coach in any other way. According to the results of this diagnostic method, the coach is able to understand the entire neuromuscular pattern and the role of a particular muscle in simple and controlled moves, which allows the possibility of a far more precise control and loading of particular segments in the knee joint. Our results show the existence of particularly statistically significant differences between observed surgical techniques that led to the change of the neuromuscular pathway during simple and controlled knee movements even two years after ACL reconstruction in athletes who have returned to active training. These disturbances of muscle coordination in the knee joint could be tied to function and location from which the autotransplant is taken and not to transplant quality itself. Based on the results of this research, we could not determine which ACL reconstruction method is more appropriate. It is possible that this is the result of a small number of study participants and the strictness of applied statistically significant criteria. It would therefore be useful to conduct the study on a larger number of individuals treated with these types of ACL reconstruction in during the same time interval.
Conclusion
Results indicate neuromuscular changes as long as two years after ACL reconstruction, when the respective rehabilitation was completed and athletes resumed a full training load. This may result in an increased risk of repeated knee injury, including potential permanent consequences. This study may primarily be useful for athletes and their coaches, who could then plan, programme and adequately adjust their training process, thereby improving knee function in the best possible way, which in turn would maintain and extend the athletes’ respective sports careers.
References
Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lázaro-Haro C, Cugt R (2009) Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc 17:705–729
Anders JO, Venbrocks RA, Weinberg M (2009) Proprioceptive skills and functional outcome after anterior cruciate ligament reconstruction with a bone-tendon-bone graft. Int Orthop 32:627–633
Bland JM, Altman DG (1995) Multiple significance tests: the Bonferroni method. BMJ 310:170
Bluman AG (2004) Elementary Statistics: a step by step approach. McGraw-Hill, New York
Chouliaras V, Ristanis S, Moraiti C, Tzimas V, Stergiou N, Georgoulis AD (2009) Anterior cruciate ligament reconstruction with a quadrupled hamstrings tendon autograft does not restore tibial rotation to normative levels during landing from a jump and subsequent pivoting. J Sports Med Phys Fit 49:64–70
Columb MO, Sagadai S (2006) Multiple comparisons. Curr Anaesth Crit Care 17:233–236
Dauty M, Tortellier L, Rochcongar P (2005) Isokinetic and anterior cruciate ligament reconstruction with hamstrings or patella tendon graft: analysis of literature. Int J Sports Med 26:599–606
Ejerhed L, Kartus J, Sernert N, Köhler K, Karlsson J (2003) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 31:19–25
Gobbi A, Mahajan S, Zanazzo M, Tuy B (2003) Patellar tendon versus quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a prospective clinical investigation in athletes. Arthroscopy 19:592–601
Hermens HJ, Merletti R, Rix H, Freriks B (eds) (1999) The state of the art on signal processing methods for surface electromyography. Roessingh Research and Development, Enschede
Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, Rau G et al (eds) (1999) European recommendations for surface electromyography. Roessingh Research and Development, Enschede
Johnson DS, Smith RB (2001) Outcome measurement in the ACL deficient knee – what's the score? Knee 8:51–57
Kasović M, Medved V, Mejovšek M, Ergović V (2008) Biomechanical diagnostics of knee joint condition in sport. In: Milanović D, Prot F (eds) Proceedings of the 5th International Scientific Conference in Kinesiology. University of Zagreb, Faculty of Kinesiology, Zagreb pp 242–245
Kasović M, Potočanac Z, Mejovšek M (2009) Differences in ACL reconstruction techniques: EMG study. Proceedings of XXII Congress of the International Society of Biomechanics, Cape Town, South Africa (CD-ROM)
Kasović M, Pribanić T, Medved V (2002) Take-off and landing properties in top-level football players: a ground reaction force study. Kinesiology 34:182–189
Katabi M, Djian P, Christel P (2002) Anterior cruciate ligament reconstruction: patellar tendon autograft versus four-strand hamstring tendon autografts. A comparative study at one year follow-up. Rev Chir Orthop Traumatol Revue de chirurgie orthopédique et réparatrice de l'appareil moteur 88:139–148
Kobayashi A, Higuchi H, Terauchi M, Kobayashi F, Kimura M, Takagishi K (2004) Muscle performance after anterior cruciate ligament reconstruction. Int Orthop 28:48–51
Lin Z, Zhang X, Jiang J (2010) Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int Orthop 34:45–49
Mejovšek M, Kasović M, Lončar V (2007) New laboratory test for dynamic satability in ACL deficient knee joint. Program and Abstracts of the XXIth ISB Congress, Taipei, Taiwan, J Biomech 40 (Suppl 2):588
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33:1337–1345
Seon JK, Song EK, Bae BH, Park SJ, Yoon TR, Cho SG, Lee JJ, Kim MS (2007) Kinematic study following double-bundle, anterior cruciate ligament reconstruction. Int Orthop 31:623–628
Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr (2004) Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med 32:1986–1995
Taylor DC, Deberardino TM, Nelson BJ, Duffey M, Tenuta J, Stoneman PD, Sturdivant RX, Mountcastle S (2009) Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: A randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med 37:1946–1957
Tow BP, Chang PC, Mitra AK, Tay BK, Wong MC (2005) Comparing 2-year outcomes of anterior cruciate ligament reconstruction using either patella-tendon or semitendinosus-tendon autografts: a non-randomised prospective study. J Orthop Surg (Hong Kong) 13:139–146
Woo SL, Fisher MB (2009) Evaluation of knee stability with use of a robotic system. J Bone Joint Surg 91(Suppl 1):78–84
Acknowledgements
This study was supported by the Ministry of Science, Education and Sports of the Republic of Croatia (Project No. 034-0362979-2334 and 034-0000000-2340)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasović, M., Mejovšek, M., Matković, B. et al. Electromyographic analysis of the knee using fixed-activation threshold after anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 35, 681–687 (2011). https://doi.org/10.1007/s00264-010-1050-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1050-4