Abstract
Purpose
The purpose of this study was to assess activation patterns of medial (MH) versus lateral (LH) hamstrings in female athletes who had undergone ACL reconstruction (ACLR) using a hamstrings-graft during single-limb functional testing.
Methods
Eighteen athletes (1–6 years since ACLR) and 18 healthy controls were recruited from the Icelandic women’s top divisions in football, handball, and basketball. Activation of the MH and LH was monitored bilaterally using surface electromyography. Peak activation of the normalized signal was identified for two phases of the single-limb crossover (SLC) hop test and performance (distance jumped) registered. Self-reported knee symptoms and function were evaluated with the Knee injury and Osteoarthritis Outcome Score (KOOS). A repeated measures general linear model was used for main statistical data analyses, comparing variables of interests between limbs (within-subjects factor) and between groups.
Results
ACLR athletes had worse KOOS-symptoms scores (p < 0.05) than controls, while hop distance was equal. Overall, MH and LH muscle activation levels differed between the two phases of the SLC hop test (p < 0.05). Moreover, inter-limb differences in MH and LH activity were identified between groups (p < 0.05), mainly explained by greater LH than MH activation in the uninjured limb of ACLR athletes.
Conclusion
One to 6 years after ACLR, female athletes performed on par with uninjured controls, but demonstrated inter-limb differences in muscle activation patterns of the hamstrings that were not evident in controls. This may be an important factor to consider during postsurgical rehabilitation in order to lower the risk of a second injury.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An injury to the anterior cruciate ligament (ACL) of the knee is a serious one with short- as well as probable long-term consequences for the individual’s knee function, which may negatively affect his or her activity, participation, and quality of life. Female athletes are at greater risk of injury than their male counterparts who practice and compete in the same sport [22, 28], and they are also more likely to suffer a second injury to either the ipsilateral or contralateral limb [7, 25]. Concomitant injuries are common and typically involve menisci, collateral ligaments, and cartilage [12, 23]. This may, in part, explain early onset and progression of knee osteoarthritis (OA) recognized in this population [16].
The purpose of ACL reconstruction (ACLR) is to regain joint stability and thereby function of the lower limb. While joint stability may be adequately restored, arthrokinematics of the joint and kinematics of the lower limb are affected and may influence the rate of progression of knee OA [9, 10, 15, 34]. In Scandinavia, the graft is most commonly harvested from the ipsilateral semitendinosus (with or without additional strands from gracilis) [14]. In many instances, regeneration of the tendon does not ensue [17] and a resulting proximal migration of the muscle–tendon junction of the semitendinosus is often found [8, 17, 37]. This and postsurgical muscle atrophy may explain seemingly selective, persistent muscle weakness of the medial knee flexors that is found in tests performed in deep knee flexion [2, 8, 38, 41] and tibial internal rotation [3, 35]. The hamstrings, from a functional anatomy perspective, augment the ACL’s resistance to anterior translation of the tibia, and the muscle’s recovery following ACLR is therefore of clinical importance. Recent longitudinal analyses indicate that autografts harvested from the hamstrings [hamstring graft (HG)] are more often associated with re-rupture than when retrieved from the patellar tendon [27]. No studies, however, have elucidated whether this is related to the graft, fixation method, or postsurgical alterations in musculotendineal structure and/or function affecting knee joint arthrokinematics.
The overall goal of rehabilitation after ACLR was for the individual to regain knee and lower limb function and thus the ability to return to his/her desired activities [1, 39, 47]. The goal is generally achieved by progressively improving range of motion, strength, neuromuscular function, and sport-specific performance [1, 44, 45]. Specific training and testing for the medial (MH) versus lateral hamstring (LH) components are not routine, although muscle strength of knee flexors collectively is typically well monitored during rehabilitation [42]. This may, however, be of particular importance within the context of preventing re-injury in light of the mechanism of non-contact ACL injuries in sports, as the MH component has the potential to counter the external outward rotating knee moments associated with ACL rupture [5].
Athletes who have returned to previous levels of sports participation may have symmetrical lower limb performance upon functional testing, while continuing to demonstrate measurable biomechanical differences that reflect the quality of performance [24, 43]. Identifying specific alterations in muscle activation may inform postsurgical rehabilitation, with potential improvements in successful return to competition and lowered risk of re-injury. With respect to specific hamstring muscle activation, Ristanis et al. [32] used electromyography (EMG) to investigate whether timing of hamstring muscle activation was affected after ACLR using HG. They found significant electromechanical delay in the ipsilateral knee flexors compared with the contralateral limb and controls. Differences in the relative contribution of knee flexor components have further been demonstrated during controlled exercises in athletes who had undergone ACLR compared with matched controls [4, 43]. The mechanism of non-contact ACL rupture, however, typically involves predominantly unilateral dynamic maneuvers. To our knowledge, specific hamstring muscle activation patterns during single-limb cutting tasks have not been investigated post-ACLR.
Therefore, the purpose of this controlled laboratory trial was to assess MH and LH muscle activation levels in each lower limb during the single-limb crossover (SLC) hop test, which is frequently utilized to assess lower limb function after injury [19, 31]. The primary aim was to contrast muscle activation patterns of individuals who had undergone ACLR using a HG and matched healthy athletes. The ‘a-priori’ hypothesis was that inter-limb differences in MH and LH peak activation would only be found in participants, who had undergone ACLR. Secondary aims included group comparisons of variables that might identify differences in knee joint function and activity limitations (measured hop performance and self-reported). These are domains recognized within the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) [46].
Materials and methods
Eighteen eligible female athletes who had all undergone surgery 1–6 years previously volunteered to participate (ACLR group). They were recruited via advertisement from teams competing in the top leagues in three sports [team handball (n = 5), basketball (n = 4), and football (n = 9)]. In 12 instances, the surgical limb was the individual’s dominant one, while in six participants, this was not the case. The 18 controls (CTRL group) were recruited from the same teams and were matched for age, height, and weight (Table 1). The designated ‘surgical’ limb was in 11 instances the dominant side, while in seven cases, it was not. All ACLR participants had returned to competition with their teams. Five participants had undergone surgery 1–2 years previously, another five had undergone surgery 3–4 years previously, and eight participants had surgery 5–6 years previously. Exclusion criteria were current musculoskeletal injury, history of lower limb muscle strain within the previous 3 months, and any orthopedic condition precluding them from performing single-limb hop testing of either lower extremity. In order to avoid negative effects of excess adipose tissue on the EMG signal amplitude, and thereby the signal-to-noise ratio of the recorded signal, only participants with a body mass index (BMI) lower than 30 kg/m2 were accepted into the study.
Age, height, and weight were registered, and in addition, each participant completed the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire. The KOOS consists of five subscales assessing: (1) knee pain, (2) other knee symptoms, (3) knee function during activities of daily living, (4) ability during sports and recreation, and (5) factors relating to quality of life. The instrument is valid and reliable and contains items that are important to patients [6, 33, 40]. No group differences were found with respect to age, height, weight, or BMI (Table 1).
Wireless surface EMG (Kine Pro, Hafnarfjordur, Iceland) was used to monitor muscle activity of MH and LH during hop testing of each lower limb. A signal bandwidth of 16–500 Hz was used, sampling at 1,600 Hz. Electrodes were placed according to SENIAM guidelines in order to identify the optimal position [36]. In order to verify placement, muscles were palpated and a visual assessment of the signal performed prior to testing.
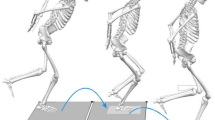
After a 5-min warm up on a stationary bicycle, participants performed the SLC hop test for distance, during which three consecutive maximal hops (triple jump) were performed while alternately crossing over a 15-cm strip on the floor (Fig. 1). The participants stood on the test limb with the toe behind a start line, with the 15-cm strip to the lateral side of the foot. The test was thereby always performed in such a manner that the first and third hops involved an anterolateral projection and anteromedial during the second hop. The overall distance (meters) covered was measured with a tape measure from the start line to the heel of the foot as it landed at the completion of the task. The test is a reliable and a valid measure of functional performance often used after knee injury [19, 31]. Following two practice trials, the EMG signal and the distance jumped were then recorded during a single maximal test trial and the same procedure followed for each limb. ACLR participants started jumping on the non-surgical limb, and each matched control with their matched limb. Two distinct phases of the triple jump were of interest: (1) the first landing and subsequent take-off and change in direction and (2) the second landing and subsequent take-off and change in direction. Raw EMG signals were high-pass filtered at 25 Hz, full-wave rectified, and the root-mean square of the signal was derived using a moving 250 ms window. Peak values for each of the two phases of the test jump were normalized to the maximum signal collected during two 5-s trials of maximal voluntary isometric muscle contraction. The study was approved by the National Bioethics Committee in Iceland (VSNb2012110023/03.07), and informed consent was obtained from participants prior to data collection.
Statistical analysis
Data were analyzed using IBM SPSS Statistics version 20. A repeated measures general linear model was used to evaluate each lower limb’s distance jumped (within-subjects factor) between groups. For muscle activity, within-subjects factors included limb (involved/uninvolved), phase of jump (first/second), and muscle (MH/LH), between the ACLR and CTRL groups. Independent t tests were used to analyze demographic variables and KOOS-scores between groups. Sample size was determined with reference to previous EMG studies conducted in our laboratory, where observed power of two groups with 20 subjects each ranged from 0.7 to over 0.9 for two- and three-way interactions. The alpha level was set at 0.05.
Results
A significant interaction was found due to differences in mean muscle activation levels of the medial and lateral hamstring components during phase one compared with phase two across both lower limbs for both groups (p = 0.001). Furthermore, a three-way interaction was found as inter-limb differences in MH versus LH activation levels were different between groups (p = 0.042; Fig. 2). Medial versus lateral activation levels were similar within both limbs of the CTRL group and within the surgical limb of ACLR athletes, but not the uninjured limb, where high activation levels of LH were coupled with relatively low activation of MH. Neither inter-limb nor group differences were demonstrated in performance of the SLC hop test. The mean (SD) distance was 3.54 (0.57) and 3.55 (0.64) m for the involved versus uninvolved limb of ACLR participants and 3.55 (0.63) and 3.49 (0.63) m for the matched limbs of the CTRL group. Although mean KOOS scores were generally slightly lower for ACLR participants, a statistically significant difference was only found for the KOOS-symptoms subscale (p < 0.05; Table 2, Fig. 3).
Discussion
The most important finding of this study was that inter-limb differences in activity of MH versus LH were identified in female athletes who had undergone ACLR, whereas performance (distance) was not affected during single-limb hop testing. Secondary outcomes showed greater complaints of knee symptoms of female athletes with history of ACLR.
Knee joint arthrokinematics during loading of the knee, in particular during cutting maneuvers, are of importance with respect to the injury mechanism of non-contact ACL tears. The interaction of muscle component and hop phase demonstrated clearly how the medial and lateral hamstring components play different roles depending on the change in direction. Net knee joint moments in the frontal and transverse planes would be expected to differ when cutting to the inside versus outside of the stance limb. The muscle components have distal insertions on either side of the knee and tibial rotation [11, 20], and frontal plane moments [29, 30] are known to affect their relative activation levels. Outwards versus inwards change in direction during the crossover hop would therefore be expected to affect them differently, as demonstrated by the results of the present study.
Interestingly, the between-groups interaction of limb and muscle group was mainly due to the difference in MH versus LH activation levels of the uninjured limb of the ACLR participants. The lateral component demonstrated high activation levels relative to the medial, across jump phases, whereas the surgical limb and both CTRL limbs had relatively similar LH versus MH activation levels on average. The result is of clinical significance, as female athletes with history of ACLR have a 16-fold greater risk of a second ACL injury than healthy athletes [25]. A second ACL injury of the contralateral limb is reportedly twice as likely to be sustained in the contralateral limb, and this is more common in female than male athletes [26, 48]. Greater relative LH activation levels may induce greater knee abduction and external rotation of the tibia, recognized components of the multifactorial mechanism of non-contact ACL injury [18].
The ACLR athletes had successfully returned to full participation of high-level sports and therefore had likely achieved acceptable limb symmetry for lower limb muscle strength. Moreover, no difference was found in hop performance between the two groups, as is to be expected given that limb symmetry is generally evaluated as one of the criteria for returning to high-level sport participation [42]. However, the contribution of MH versus LH toward the net flexor strength is not measured and therefore unknown. Studies have shown that tibial internal rotation strength is affected by harvesting semitendinosus [3, 35], which indicates that their function as knee flexors may also be compromised. A compensatory shift in muscle volume (MH atrophy and LH hypertrophy) has also been demonstrated in imaging studies [21, 37]. Hypertrophy and greater strength of LH combined with atrophy and decreased strength of MH after ACLR might lead to the changes in activation levels seen in the surgical limb compared with the uninjured limb of the ACLR participants. The weak MH would be activated at a greater percentage of its maximum, while the strong LH would demonstrate relatively low activation levels. However, no strength measures were performed in the present study, which limits our ability to interpret the clinical significance of the inter-limb differences in activation levels measured in ACLR participants. Another limitation involves motion of electrodes as the skin moves over the muscles. This is inevitable during a task where a change in direction is involved and, despite high-pass filtering of the signal to eliminate movement artifacts, may introduce cross talk from other than the target muscles.
Although mean KOOS-scores were generally slightly lower in ACLR athletes than controls, this was only statistically significant for the symptoms subscale, where the difference may also be considered clinically significant [6]. Notably, CTRL participants registered symptoms that affected their sports participation and quality of life, and this is recognized within amateur soccer, in particular in athletes with history of even minor knee injuries [13].
Conclusion
In summary, female athletes who had a history of ACLR surgery demonstrated inter-limb differences in relative medial versus lateral hamstring muscle activity not found in uninjured controls, reflecting high activation levels of LH in the uninjured limb. In light of the high rate of reinjury seen in this population and known mechanisms of non-contact ACL injury, in particular to the contralateral limb, rehabilitation after primary ACL injury should address muscle function of medial and lateral hamstring components of both lower limbs.
References
Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L (2012) Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther 42(7):601–614
Ahlen M, Liden M, Bovaller A, Sernert N, Kartus J (2012) Bilateral magnetic resonance imaging and functional assessment of the semitendinosus and gracilis tendons a minimum of 6 years after ipsilateral harvest for anterior cruciate ligament reconstruction. Am J Sports Med 40(8):1735–1741
Armour T, Forwell L, Litchfield R, Kirkley A, Amendola N, Fowler PJ (2004) Isokinetic evaluation of internal/external tibial rotation strength after the use of hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 32(7):1639–1643
Arnason SM, Birnir B, Gudmundsson TE, Gudnason G, Briem K (2014) Medial hamstring muscle activation patterns are affected 1–6 years after ACL reconstruction using hamstring autograft. Knee Surg Sports Traumatol Arthrosc 22(5):1024–1029
Bencke J, Curtis D, Krogshede C, Jensen LK, Bandholm T, Zebis MK (2013) Biomechanical evaluation of the side-cutting manoeuvre associated with ACL injury in young female handball players. Knee Surg Sports Traumatol Arthrosc 21(8):1876–1881
Briem K (2012) Reliability, validity and responsiveness of the Icelandic version of the knee injury and osteoarthritis outcome score (KOOS). Laeknabladid 98(7–8):403–407
Brophy RH, Schmitz L, Wright RW, Dunn WR, Parker RD, Andrish JT, McCarty EC, Spindler KP (2012) Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med 40(11):2517–2522
Choi JY, Ha JK, Kim YW, Shim JC, Yang SJ, Kim JG (2012) Relationships among tendon regeneration on MRI, flexor strength, and functional performance after anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med 40(1):152–162
Decker LM, Moraiti C, Stergiou N, Georgoulis AD (2011) New insights into anterior cruciate ligament deficiency and reconstruction through the assessment of knee kinematic variability in terms of nonlinear dynamics. Knee Surg Sports Traumatol Arthrosc 19(10):1620–1633
Delince P, Ghafil D (2012) Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20(1):48–61
Fiebert IM, Spielholz NI, Applegate EB, Fox C, Jaro J, Joel L, Raper L (2001) Comparison of EMG activity of medial and lateral hamstrings during isometric contractions at various cuff weight loads. Knee 8(2):145–150
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. New Engl J Med 363(4):331–342
Frobell RB, Svensson E, Gothrick M, Roos EM (2008) Self-reported activity level and knee function in amateur football players: the influence of age, gender, history of knee injury and level of competition. Knee Surg Sports Traumatol Arthrosc 16(7):713–719
Granan LP, Bahr R, Lie SA, Engebretsen L (2009) Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med 37(5):955–961
Hoshino Y, Fu FH, Irrgang JJ, Tashman S (2013) Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res 471:2924–2931
Janssen RP, du Mee AW, van Valkenburg J, Sala HA, Tseng CM (2013) Anterior cruciate ligament reconstruction with 4-strand hamstring autograft and accelerated rehabilitation: a 10-year prospective study on clinical results, knee osteoarthritis and its predictors. Knee Surg Sports Traumatol Arthrosc 21(9):1977–1988
Janssen RP, van der Velden MJ, Pasmans HL, Sala HA (2013) Regeneration of hamstring tendons after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21(4):898–905
Kobayashi H, Kanamura T, Koshida S, Miyashita K, Okado T, Shimizu T, Yokoe K (2010) Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1,700 athletes. J Sports Sci Med 9(4):669–675
Logerstedt D, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, Axe MJ, Snyder-Mackler L (2012) Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med 40(10):2348–2356
Lynn SK, Costigan PA (2009) Changes in the medial-lateral hamstring activation ratio with foot rotation during lower limb exercise. J Electromyogr Kinesiol 19(3):e197–e205
Macleod TD, Snyder-Mackler L, Axe MJ, Buchanan TS (2013) Early regeneration determines long-term graft site morphology and function after reconstruction of the anterior cruciate ligament with semitendinosus-gracilis autograft: a case series. Int J Sports Phys Ther 8(3):256–268
Myklebust G, Maehlum S, Holm I, Bahr R (1998) A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports 8(3):149–153
Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38(11):2201–2210
Orishimo KF, Kremenic IJ, Mullaney MJ, McHugh MP, Nicholas SJ (2010) Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(11):1587–1593
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2012) Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 22(2):116–121
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2014) Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med 42(7):1567–1573
Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM (2014) Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med 42(2):285–291
Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K (2007) A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy 23(12):1320–1325
Ramsey DK, Briem K, Axe MJ, Snyder-Mackler L (2007) A mechanical theory for the effectiveness of bracing for medial compartment osteoarthritis of the knee. J Bone Joint Surg Am 89(11):2398–2407
Ramsey DK, Snyder-Mackler L, Lewek M, Newcomb W, Rudolph KS (2007) Effect of anatomic realignment on muscle function during gait in patients with medial compartment knee osteoarthritis. Arthritis Rheum 57(3):389–397
Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR (2007) Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 87(3):337–349
Ristanis S, Tsepis E, Giotis D, Stergiou N, Cerulli G, Georgoulis AD (2009) Electromechanical delay of the knee flexor muscles is impaired after harvesting hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 37(11):2179–2186
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Scanlan SF, Chaudhari AM, Dyrby CO, Andriacchi TP (2010) Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech 43(9):1817–1822
Segawa H, Omori G, Koga Y, Kameo T, Iida S, Tanaka M (2002) Rotational muscle strength of the limb after anterior cruciate ligament reconstruction using semitendinosus and gracilis tendon. Arthroscopy 18(2):177–182
SENIAM Surface electromyography for the non-invasive assessment of muscles: recommendations for sEMG sensors, sensor placement and location. www.seniam.org
Snow BJ, Wilcox JJ, Burks RT, Greis PE (2012) Evaluation of muscle size and fatty infiltration with MRI nine to eleven years following hamstring harvest for ACL reconstruction. J Bone Joint Surg Am 94(14):1274–1282
Tadokoro K, Matsui N, Yagi M, Kuroda R, Kurosaka M, Yoshiya S (2004) Evaluation of hamstring strength and tendon regrowth after harvesting for anterior cruciate ligament reconstruction. Am J Sports Med 32(7):1644–1650
Tagesson S, Oberg B, Good L, Kvist J (2008) A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med 36(2):298–307
Tanner SM, Dainty KN, Marx RG, Kirkley A (2007) Knee-specific quality-of-life instruments: which ones measure symptoms and disabilities most important to patients? Am J Sports Med 35(9):1450–1458
Tashiro T, Kurosawa H, Kawakami A, Hikita A, Fukui N (2003) Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction. A detailed evaluation with comparison of single- and double-tendon harvest. Am J Sports Med 31(4):522–529
Thomee R, Kaplan Y, Kvist J, Myklebust G, Risberg MA, Theisen D, Tsepis E, Werner S, Wondrasch B, Witvrouw E (2011) Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 19(11):1798–1805
Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM (2008) Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 16(1):2–14
van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ (2010) Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(8):1128–1144
White K, Di Stasi SL, Smith AH, Snyder-Mackler L (2013) Anterior cruciate ligament- specialized post-operative return-to-sports (ACL-SPORTS) training: a randomized control trial. BMC Musculoskelet Disord 14:108
WHO World Health Organization. International classification of functioning, disability and health (ICF). http://www.who.int/classifications/icf/en/. http://www.who.int/classifications/icf/en/
Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR (2012) Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther 42(3):153–171
Wright RW, Magnussen RA, Dunn WR, Spindler KP (2011) Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am 93(12):1159–1165
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Briem, K., Ragnarsdóttir, A.M., Árnason, S.I. et al. Altered medial versus lateral hamstring muscle activity during hop testing in female athletes 1–6 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 24, 12–17 (2016). https://doi.org/10.1007/s00167-014-3333-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3333-6