Abstract
Since its definition 65 years ago, progressive multifocal leukoencephalopathy (PML) has continued to devastate a growing population of immunosuppressed patients despite major advances in our understanding of the causative JC virus (JCV). Unless contained by the immune system, JCV lyses host oligodendrocytes collateral to its life cycle, leading to demyelination, neurodegeneration, and death. Novel treatments have stagnated in the absence of an animal model while current antiviral agents fail to address the now ubiquitous polyomavirus. In this review, we highlight the established pathogenesis by which JCV infection progresses to PML, highlighting major challenges that must be overcome to eliminate the underlying virus and, therefore, the debilitating disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
JC virus
At the time of its framing as a distinct disorder in 1958, the etiology of PML remained uncertain (Astrom et al. 1958). With a majority of cases affecting patients with advanced blood cancers (i.g., leukemias, lymphomas, myelomas) and severe inflammatory conditions (i.g., lupus erythematous, sarcoidosis), an early hypothesis proposed that it was the consequence of an opportunistic virus (Richardson 1961, 1974). This was confirmed by Zu Rhein and Chou in 1965, who identified an unknown “papova-like virus” when analyzing PML lesions with electron microscopy (Zurhein and Chou 1965). Six years later, Padgett et al. (1971) successfully isolated the PML-causing strain of JC virus (JCV) from the autopsy of the eponymous patient, JC. By 1976, JCV was identified in the sera of over twenty cases of PML and was the accepted cause of the demyelinating disease (Padgett et al. 1976). Shortly thereafter, Frisque, Bream, and Cannella published the complete genome and associated proteome of the first isolated JCV strain, Mad-1 (Frisque et al. 1984).
JCV is a double-stranded DNA polyomavirus with a circular, supercoiled genome packaged within an icosahedral capsid (Fig. 1A). The non-coding control region (NCCR) regulates the bicistronic genome consisting of two early and four late open reading frames (Fig. 1B). The early NCCR and six coding regions are largely conserved whereas the late NCCR varies across benign and pathologic strains (Fig. 2). Two early proteins, small and large tumor antigen (smtAg and LTAg), act as essential transactivators of the NCCR. In addition to increasing viral transcription by functioning as a helicase (unwinding and unzipping the hypercoiled dsDNA) and enhancer (recruiting host machinery to the promoter), the T antigens interact with housekeeping genes to create a pro-viral environment (Saribas and Safak 2020). Through interaction with E3 ubiquitin ligase, TRIM25, smtAg interrupts the cytokine signaling pathway of the innate immune response (Bollag et al. 2010; Chiang et al. 2021). LTAg inactivates tumor suppressors, p53 and pRb; inhibits the pro-apoptotic protein, survivin, and promotes proliferation through the c-Myc/Wnt pathway (Krynska et al. 1997; Gan et al. 2001) The resultant pro-survival state provides the two early peptides with their “tumor” namesake.
Overview of JC capsid, genome map, and interaction with host receptors. A Cartoonized depiction of the JC virus, which is 12% DNA and 88% protein by weight. The external icosahedral capsid consists of 72 VP1 pentamers organized around an inner capsid of approximately 72 VP2/VP3 proteins (not visible). The circular dsDNA genome is supercoiled within the capsid. B The genome is 5.2 kb, including a bicistronic non-coding control region and six open reading frames. The early genome (red) encodes small and large T-antigen; the late genome (blue) encodes agnoprotein and the three capsid proteins. C The VP1 proteins of the outer capsid directly bind to sialic acid residues and/or 5HT2A receptors on the host cell surface, initiating endocytosis
Arrangements of non-coding control regions of archetype (cy) and PML-type (Mad-1, Mad-4) JCV strains. Depiction of the archetype control region with noted deletions and rearrangements of the late promoter, producing common PML-type strains, Mad-1 and Mad-4. The early promoter (z) is largely conserved and regulates the expression of smtAg and LTAg whereas the late promoter (a–f) is prone to hypervariability and regulates the expression of Agno and VP1-3
Agnoprotein (Agno), the intermediate or “early-late” protein, hinders early LTAg and promotes late gene expression of additional Agno and the three capsid proteins, VP1-3 (Safak et al. 2001; Akan et al. 2006). Agno exits the host cell prior to cell death and interacts with adjacent cells, priming them for viral infiltration (Saribas et al. 2018). Within the infected cell, it also interacts with mitochondria to directly induce apoptosis of oligodendrocytes, enabling the lytic spread of JCV (Merabova et al. 2008; Saxena et al. 2021).
The external capsid includes 360 VP1 peptides arranged in 72 pentamers, forming an icosahedral capsid with T = 7 symmetry (Fig. 1A). Without an envelope, VP1 directly interacts with the environment, binding sialic acid residues on cell membranes to induce endocytosis (Fig. 1C) (Shishido-Hara et al. 2000; Ou et al. 2001; Kobayashi et al. 2013). Serotonin receptor 5HT2A, in particular, has been shown to interact with VP1, initiating the internalization of the entire virus into clathrin-coated pits (Querbes et al. 2004; Chapagain et al. 2008; Mayberry et al. 2019). The VP1 shell is capable of self-assembly but is stabilized around intrinsic minor proteins VP2 and VP3 (Ou et al. 2001; Shishido-Hara et al. 2004). Each five-VP1 capsomere is paired with an intrinsic VP2 or VP3 monomer, the latter being a truncated version of the former. The absence of either minor protein impairs the nuclear localization of JCV VP1 resulting in a reduction of viral progeny with key roles in nuclear localization and DNA packaging (Shishido-Hara et al. 2004; Gasparovic et al. 2006). The myristoylated VP2 has been identified in the role of uncoating in early infection whereas VP3 has been shown to inhibit the early promoter of the viral genome (Krauzewicz et al. 1990; Huang et al. 2003). Complexes of VP2 and VP3, together, enhance LTAg binding to the NCCR, promoting viral genome expression (Saribas et al. 2014).
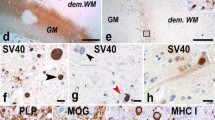
The exact ratio of VP2 to VP3 is unknown; other polyomaviruses, such as Merkel polyomavirus, lack VP3 altogether. Simian virus 40 (SV40) is a primate polyomavirus with a 69% homology to JCV (Deckhut et al. 1991). Its similar external shell of VP1 peptides surrounds a mixed core of 72 VP2 and VP3 monomers of an unspecified ratio (Nakanishi et al. 2006; Gasparovic et al. 2006). A complex of both VP2 and VP3 acts as a viroporin in the endoplasmic reticulum, enabling infection and packaging of viral DNA in the nucleus (Daniels et al. 2006). Given their similarities, it can be extrapolated that the roles of JCV VP2 and VP3 are similar to those of SV40, but the exact numbers remain unestablished for both.
The lifecycle of JCV: the adaptation hypothesis
Using viral isolate from patient samples and hemagglutination-inhibition testing, Padgett and Walker (1973) found 69% of the general population expressed antibodies against JCV, with 14% seropositivity in young children growing to 86% in senior adults. Asymptomatic individuals were identified as carriers as 20% of healthy subjects shed infectious JC virions in their urine (Hogan et al. 1980; Kitamura et al. 1990; Flaegstad et al. 1991). This peripheral strain has been referred to as “archetype” JCV (cy-JCV). Yogo and colleagues isolated cy-JCV and found it persists within the same, healthy participants over many years without mutations in the genome or decrement in concentrations (Yogo et al. 1990, 1991; Kato et al. 1994; Kitamura et al. 1997). Conversely, hypervariable “prototype” (hyp-JCV, also referred to as “neurotropic”) strains were isolated from PML patients, with rearrangements of the late NCCR differing across cases as well as within individuals (Grinnell et al. 1983; Martin et al. 1985; Iida et al. 1993; Ault and Stoner 1993; Yogo et al. 1994).
The “adaptation model” became the accepted theory of the JCV/PML life cycle wherein cy-JCV is spread through contamination of the environment before mutating to hvp-JCV within an immunocompromised host (Fig. 3). This theory is supported by the identification of cy-JCV in sewage and age-graded changes in anti-VP1 seropositivity (Bofill-Mas and Girones 2003; Bofill-Mas et al. 2003). Recent evidence from the novel coronavirus pandemic supports the gastrointestinal route of infection: regions with mask mandates show stable JCV seroconversion rates while viruses known to transmit through respiratory droplets (e.g., coronavirus, influenza, rhinovirus) declined (Cheng et al. 2021; Oh et al. 2021; Leech et al. 2022; Vigiser et al. 2022). LTAg has been implicated in multiple gastrointestinal cancers in the absence of systemic JCV, further supporting the proposed mechanism of infection via ingestion (Enam et al. 2002; Del Valle et al. 2005; Shin et al. 2006; Shavaleh et al. 2020; Querido et al. 2020; Fang et al. 2022).
Transmission of archetype JCV (cy-JCV) in the environment with latent reservoirs in an immune-competent host (black arrows) and pathogenesis during immune compromise (red arrows). Archetype JCV is ingested (1) and passed asymptomatically in urine with persistently low levels of replication in kidney tissue (2). Contamination of sewage (3a) and food products (3b) occurs secondary to poor hygiene, enabling spread to additional hosts through ingestion (1). During immune compromise, disinhibition of latent JCV increases proliferation (3). High proliferation rates increase the spontaneous rearrangements of cy-NCCR into PML-type strains (4a). Disinhibition and mutation enable the spread to additional organ reservoirs with preferential replication in glial cells of the brain (4b)
During immunosuppression, cy-JCV and its hvp-JCV progeny expand to include additional reservoirs, infiltrating lymphocytes and spreading hematogenously from the primary latency site in the kidney to include bone marrow and nervous tissue (Tornatore et al. 1992; White et al. 1992; d’Arminio Monforte et al. 1997; Du Pasquier et al. 2004; Van Loy et al. 2015). In the absence of immunosuppression, the blood–brain barrier successfully prevents the hematogenous spread of JCV, but evidence suggests even temporary immunosuppression can enable infiltration of nervous tissues through B-cell mediated extravasation. Both cy- and hvp-JCV proliferate strongest in glial cells, and both have been identified in the brains and peripheral tissues of PML and non-PML patients (White et al. 1992; O’Neill et al. 2003; Tan et al. 2010). Increased proliferation significantly increases the degree and rate of NCCR mutation, with deletions preceding translocations and variants increasing with viral load (Ault and Stoner 1993; Agostini et al. 1997; Pietropaolo et al. 2003). These mutations have clinical significance, with the number of repeats correlating with poorer PML outcomes (Pfister et al. 2001; Van Loy et al. 2015; Wilczek et al. 2022). The hypervariable prototype strains are not only less common, but less resistant to external stressors which influence the proposed route of transmission (i.e., extremes of pH) (Bofill-Mas et al. 2001, 2003; Bofill-Mas and Girones 2003). Particular rearrangements (e.g., Mad1, Mad4) promote the rate of replication more than cy-JCV and other, less common, hvp-JCV isoforms, supporting their convergent evolution in separate hosts (Daniel et al. 1996; Sock et al. 1996; Ault 1997; Elsner and Dörries 1998; Fedele et al. 2003; O’Neill et al. 2003). Mutations in coding regions, such as the late capsid proteins, are less commonly reported (Stoner and Ryschkewitsch 1995). Phenotype-altering mutations of the early (sm- and LTAg) and early-late proteins (Agno) significantly impaired viral propagation by removing the necessary recruitment of host polymerases (Okada et al. 2001). Similarly, alterations of the capsid proteins (VP1-3) altered the stability and infectivity of the virions. Alterations in these capsid proteins may alter the need for sialic acid binding for cellular invasion and, therefore, favor infection (Gorelik et al. 2011).
Latency and reactivation: the role of immune modulation in JCV pathogenesis
The mechanism by which an immune system promotes JCV latency is unknown, with several different mechanisms of immunosuppression resulting in reactivation (Du Pasquier et al. 2001; Iannetta et al. 2019). Flaws in both humoral and cell-mediated pathways have been implicated in PML pathogenesis, while reductions in pro-inflammatory markers have shown a correlation with JCV proliferation. Nuclear regulators, such as alternative splicing factor SF2/ASF, also change the capacity of a cell to maintain JCV levels at a low, unchanging level (Sariyer and Khalili 2011; Uleri et al. 2013; Piu et al. 2020). In addition to immunosuppression, certain external factors can enhance JCV replication including comorbid viruses and pollution (Dolci et al. 2018).
During the human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) epidemic, PML became significantly more common. The overall death rate of PML quadrupled, and 5–7% of individuals with HIV/AIDS developed PML (Holman et al. 1991). Although immunosuppression of HIV/AIDS increases risk, the incidence of PML was far greater than in other immune disorders (e.g., transplant recipients, lymphoma patients). With 80% of PML cases affecting patients with HIV/AIDS, clinical and epidemiological evidence hinted at a compounding relationship between human immunodeficiency and JC viruses (Wortman et al. 2000; Daniel et al. 2001). A complex of HIV transactivator, Tat, and cellular transcription factor, purα, was found to significantly increase the expression of JCV late genes by interacting with its promoter region. Other viruses have since shown cross-activation of the JCV late promoter with human T-lymphotropic virus type I acting through its tax protein and cytomegalovirus through IE2 (Okada et al. 2000; Winklhofer et al. 2000). Host proteins, including Bag1, NFκβ, YB-1 Sμbp-2, and Spi-B increase expression whereas c-Jun decreases it (Chen et al. 1997; Devireddy et al. 2000; Ravichandran et al. 2006; Marshall et al. 2010).
This interrelationship between HIV and JCV confounded the investigation of JC-specific antiviral agents. PML mortality peaked as the first protease inhibitor, saquinavir, was approved by the FDA in 1995. Within a year, HAART became widely available. The three-drug treatment drastically improved T-cell counts of HIV/AIDS patients, bringing a significant reduction in many HIV-associated diseases, including PML (Christensen et al. 2010). The resultant decline in PML-associated deaths was due to the improvement in predisposing immunosuppression and reduction in the co-promotional HIV. JC itself, however, was not treated. Improved outcomes were observed after the addition of cidofovir to HAART in patients with both HIV/AIDS and PML (De Luca et al. 1999; Brambilla et al. 1999; Jiang et al. 2010). However, as with other potential antivirals for PML, cidofovir has shown no benefit in clinical trials and is not recommended for the treatment of PML (Marra et al. 2002; De Luca et al. 2008).
In 2005, three simultaneously published case reports described the development of PML in patients treated with natalizumab (Tysabri) (Kleinschmidt-DeMasters and Tyler 2005; Langer-Gould et al. 2005; Van Assche et al. 2005). Natalizumab, a selective adhesion molecule inhibitor of α4β1 and α4β7 integrins prevents leukocyte entry into CNS via VCAM and gastrointestinal tissues via MadCAM (Ghosh et al. 2003; Miller et al. 2003). It was approved by the FDA for the treatment of multiple sclerosis and Crohn’s disease. The inhibition of α4β1 integrin is responsible for the heightened risk of PML in patients treated with natalizumab through not only impaired immunosurveillance, but also through the release of JCV-infected premature B cells from bone marrow stores and likely other currently unrecognized mechanisms (Berger and Koralnik 2005; Frohman et al. 2014). Proliferating within oligodendrocytes, JCV lyses to propagate its life cycle, and demyelination results as the source of myelin is destroyed. The risk of PML was calculated at 1:1000 after 18 months of natalizumab treatment (Yousry et al. 2006). In addition to altering the levels of natalizumab, studies show altered T-lymphocyte morphology, increasing the risk of JCV reactivation further than general immunosuppression alone (Iannetta et al. 2016; Zingaropoli et al. 2018). After a temporary recall, natalizumab returned to the American market in 2006 with the introduction of “Touch,” a mandatory program wherein natalizumab-treated patients underwent regular monitoring with seropositivity and/or PML symptoms indicating immediate cessation of treatment (Sheridan 2006). Four long-term observational studies were also initiated (STRATIFY-2, STRATA, TOP, and TYGRIS). A combined sample of over 37,000 patients revealed significant benefit from annual screening of the anti-JCV antibody index in the peripheral blood (Ho et al. 2017). JCV antibodies in peripheral blood and JCV DNA in urine correlate with previous exposure to JCV and, therefore, indicate an increased risk of natalizumab-induced PML.
Epidemiology: JCV prevalence and PML risk
The prevalence of JCV is consistently reported as 60–80% of the general population, citing the initial hemagglutination-inhibition studies by Padgett and Walker (1973). Their results were updated in 2009 by Egli et al. who observed anti-JCV antibodies by ELISA assay in 58% of healthy blood donors with notable age-graded seropositivity and uniform cy-JCV typing (Egli et al. 2009). A more recent 2018 metanalysis using anti-JCV ELISA found a mean seropositivity of 57.1% in patients with multiple sclerosis or neuromyelitis optica (Paz et al. 2018). Although hemagglutination-inhibition and anti-JCV antibody ELISA do suggest previous exposure to JCV, the serological tests do not equate to prevalence. A 2013 study found 37% of patients with multiple sclerosis who tested negative anti-JCV antibodies were positive for JCV viruria; this high false negative rate suggests a significant underestimation of JCV prevalence in the general population (Berger et al. 2013a, b).
Despite the consistently high levels of JCV, PML remains a rare disorder. Estimated annual incidence rates are on the order of about 1 in 1,000,000 persons, and in one population-wide study from Canada, the incidence of the disease was roughly one-half of that of Creutzfeldt Jakob disease (Bakal et al. 2021). As discussed above, the prevalence of the PML has changed over time to reflect the underlying prevalence of predisposing disorders. This change over time has been referred to as the “Epochs of PML” (Berger and Hartung 2023). These epochs were largely, although not exclusively, derived from the onset of the AIDS pandemic in 1981 and monoclonal antibody–associated PML in 2005. Prior to the AIDS pandemic, PML was predominantly observed in patients with underlying hematological malignancies, chiefly, B cell malignancies (Astrom et al. 1958). The prevalence of PML increased markedly in 1981 with the onset of the AIDS pandemic as 5–10% of all HIV-infected persons would develop PML (Berger 2014). Following the introduction of effective antiretroviral therapy in 1996, the prevalence of PML in the HIV-infected population began to decline; however, AIDS continues to be the most common predisposing cause for PML in the USA (Anand et al. 2019). Immunotherapies became a significant contributor to the prevalence of PML in 2005, after the first 3 cases of PML with natalizumab were reported (Kleinschmidt-DeMasters and Tyler 2005; Langer-Gould et al. 2005; Van Assche et al. 2005). To date, there are over 850 reported cases of natalizumab-associated PML (Dsilva et al. 2023). A wide range of immunosuppressive agents has been associated with the development of PML, although natalizumab and efalizumab (an LFA-1 monoclonal antibody that is now off the market) have rates orders of magnitude higher (Maas et al. 2016). Other conditions—in addition to AIDS and certain immunosuppressive therapies—which are predisposing to PML are lympho- and myeloproliferative disorders, carcinomas, primary immune deficiency diseases (e.g., idiopathic CD4 lymphopenia), and granulomatous inflammatory disorders (e.g., sarcoidosis). On rare occasion, no underlying explanation for PML is identified, and its development is believed to be simply a stochastic event.
PML: a clinically unmet challenge
In 1958, Astrom, Mancall, and Richardson defined PML by its unique histopathological features in three patients: two diagnosed with chronic lymphatic leukemia and one with Hodgkin’s B-cell lymphoma (Astrom et al. 1958). Over the course of the disease, shared symptoms included weakness, gait changes, slurred speech, vision changes, and cognitive alteration. Symptoms progressed in successive examinations. The cytological features differentiated PML from other demyelinating conditions as there was a characteristic triad of disseminated foci of demyelination, hypertrophy of astrocytes into “bizarre gigantic forms,” and oligodendrocytes with enlarged, round nuclei that stain darkly basophilic. Using this unique triad, they were able to reassess five historical cases for which histology was preserved: two undiagnosed patients in 1930, one proposed to be lymphogranulomatosis in 1941, and two cases presented as Schilder’s disease in 1945 and 1955. The description of PML from 65 years ago remains relevant today as challenges in diagnosis, treatment, and preclinical modeling have gone unmet.
Diagnosis
Brain biopsy remains the gold standard for diagnosis, with qPCR of cerebral spinal fluid (CSF) failing to meet its accuracy, instead functioning as an exclusionary screen (d’Arminio Monforte et al. 1997; Berger et al. 2013a, b; Ikeda et al. 2017). Because the screening procedure for a lumbar puncture is invasive, significant irreversible damage must occur and incite symptoms to arouse clinical suspicion and justify the procedure. Although a positive CSF screen is sufficient in the context of symptoms, repeatedly negative CSF PCRs may require a brain biopsy for diagnosis.
The presence of JCV in CSF in the absence of symptoms has a low sensitivity for predicting PML (Swinnen et al. 2019). The seropositive status of anti-JCV antibodies in the periphery does not equate to PML risk, as the prevalence of JCV is so extensive and the incidence of PML is so rare. (Ferretti et al. 2018; Cortese et al. 2021). Similarly, identification of JCV in the peripheral tissues does not translate to PML risk as it does not indicate mutation of cy-JCV to hvp-JCV nor does it reflect penetrance of the blood–brain barrier. An accepted and effective risk mitigation strategy is only currently available for natalizumab, with previous exposure to JCV (measured by anti-JCV antibodies) increasing the risk of drug-induced immunosuppression reactivating the virus (Ho et al. 2017). In these cases, patients are ineligible for certain PML-causing therapies. Other cases with non-iatrogenic or unavoidable immunosuppression have a dire need for a non-invasive, pre-symptomatic screen for PML-causing hvp-JCV.
Treatment
There is no effective treatment for JCV or PML (Berger et al. 2013a, b). Therapeutics are complicated by the heterogeneous patient population, with myriad subpopulations with different predisposing conditions underlying their immunosuppression. The common cause, the virus itself, is therefore the ideal target. A protein vaccine for polyomaviruses JC and BK is currently being studied in macaques; however, the training of the host immune system to recognize capsids as disease-associated is only valuable in an immune-competent environment (Peretti et al. 2023). Although the exact mechanism by which an immune system suppresses JCV is not established, cell-mediated immunity, especially JCV-specific T-cell responses, is clearly fundamental to the suppression of the disorder (Koralnik 2002). The role of the humoral immune system in preventing the development of PML in JCV-infected individuals remains uncertain but likely plays a role (Ray et al. 2015). Unlike many other viral infections, the presence of JCV-directed antibody is not protective. However, there may be neutralizing antibodies that have a role in the amelioration of the disorder.
No antivirals are recommended for any stage of infection, and many fail to show improvement in larger clinical trials (Gasnault et al. 2001; Jamilloux et al. 2016; Summers et al. 2019). Medications known to have high CNS penetrance and pre-existing FDA approval are often investigated, as their toxicities have been established for other conditions, making the lack of a translational animal model moot. Mefloquine, for example, is an anti-malarial agent with which Brickelmaier et al. significantly reduced JC replication within human glial cells (Brickelmaier et al. 2009). Small clinical studies and case reports showed mixed results on its benefit; however, it failed to improve viral load or clinical outcomes in cohort studies (Epperla et al. 2014; Kurmann et al. 2015; Nambirajan et al. 2017). Mefloquine has been paired with mirtazapine, a 5HT2A receptor antagonist approved for the treatment of major depressive disorder. Metanalyses have shown no benefit of mirtazapine, alone, on outcomes for PML patients (Jamilloux et al. 2016). The value of a combination therapy warrants consideration as the anti-malarial is proposed to reduce the genomic threat of JCV while the tricyclic antidepressant prevents capsid binding and, therefore, cell entry. The need for combination therapy is a mainstay of the sister virus, HIV, with highly active antiretroviral therapy (HAART) combining three drugs targeting different characteristics: a direct antagonist of reverse transcriptase, an indirect antagonist of reverse transcriptase, and a protease inhibitor preventing virion maturation. Redundancy in treatment will likely improve our targeting of both the JCV capsid/packaging—which is key to spread—as well as the JCV genome—which is key to expression and proliferation—to successfully eliminate the virus or suppress its viral load enough for management by a weakened immune system.
Targeting of the capsid through transfusion of T-cells primed against the major capsid protein VP1 and immune checkpoint inhibitors are appealing treatment possibilities but remain to show demonstratable efficacy (Muftuoglu et al. 2018; Cortese et al. 2019). The former mounts an immune response against the viral capsid; the latter increases the production of immune cells by obstructing anti-inflammatory PD-1, CTLA, or LAG-3. Unfortunately, altering the immune response can be problematic as reductions in viral load occur secondary to T-cell mediated culling of affected cells, advancing PML (Martins et al. 2019). Additionally, many PML patients rely on therapeutically low immune cells (i.e., transplant recipients, patients treated for autoimmune conditions) making them ineligible for the immune checkpoint inhibitors proposed.
Preclinical modeling
Progress in both diagnostics and therapeutics is limited by the absence of a pre-clinical, translational model. Animal analogs, including the murine (MuPyV) and simian (SV40) polyomaviruses, are homologous, but not identical, to JCV (White et al. 2015). While capable of duplicating PML-like conditions, the viruses themselves diverge too much to validate non-human preclinical research targeting JCV (Simon et al. 1999; Dang et al. 2005). JC virus preferentially affects human cells and inoculation with JCV uniformly produces tumors in neonatal hamsters, owl monkeys, squirrel monkeys, mice, and rats (Walker et al. 1973; London et al. 1978, 1983; Gordon et al. 2000; Del Valle and Khalili 2021). Multiple laboratories have produced humanized mice capable of harboring the JC virus (Matoba et al. 2008; Kondo et al. 2014). Matoba et al. engrafted JCV-infected cells from PML patients into mice, maintaining the cell line for 2 weeks prior to successfully suppressing the virus with an siRNA targeting agnoprotein. Kondo et al. introduced human glial progenitor cells into perinatal shiverer mice, which lack endogenous myelin, and achieved human myelination of mice axons. When JCV was injected into the brains of these chimeras, human astrocytes and oligodendrocytes were susceptible to infection; mouse cells were spared. Both models, proposed over a decade ago, reveal the potential to model JCV in vivo through humanization.
Future advancements
To eliminate PML, several translational concepts must, and can, be addressed: the development of JCV-targeting therapies, the creation of an animal model to test said therapies, and the creation of a non-invasive diagnostic screen that will enable effective treatment prior to the onset of irreversible demyelination.
Modern advances in gene editing have great value in the treatment of persistent and evasive viral infections. Although protein vaccines and immune modulators can prevent the entry of virions into cells, and reverse transcriptase and polymerase inhibitors can prevent genome expansion, these efforts are viro-static, rather than viro-cidal. CRISPR/Cas9 targets even latent DNA, curing a host of the virus entirely. The similarly persistent virus, HIV, has been successfully eliminated from T-lymphocytes in vitro, humanized mice, and SIV-analogous macaques and is currently in clinical trials (Datta et al. 2016; Kaminski et al. 2016; Dash et al. 2019; Mancuso et al. 2020). The RNA virus persists following integration into the host genome, making the excision of the viral genes essential to effective, lasting therapies. Other RNA viruses which vary significantly across strains, such as corona- and influenzaviruses, can be addressed en masse through conserved gene segments, as shown by Abbott et al. (2020) who produced a “pan-coronavirus” therapy utilizing six gRNAs to account for 90% of all coronaviruses, including SARS-CoV-2. Gene therapies utilizing CRISPR as a curative antiviral have shown success with notoriously latent herpesviruses (including cytomegalovirus, herpes simplex type 1, and Epstein Barr) which contain a dsDNA genome that permanently infects the host, like JCV (Yuen et al. 2015; van Diemen et al. 2016). CRISPR constructs against JCV have been successful, with Wollebo et al. (2015) completely excising the NCCR-LTAg span of the JCV genome in vitro, terminating the viral life cycle. Unfortunately, the absence of an animal model for JCV stalls such therapies at the preclinical stage.
Disease modeling has improved significantly in recent years with the production of multicellular human organoids and the xenotransplantation of said organoids into animal surrogates. Barreras et al. (2022) successfully propagated the JC virus within human cerebral organoids, a three-dimensional system containing neurons, oligodendrocytes, and astrocytes. The system not only produced myelinated axons, but it also hosted JCV infection and displayed associated demyelination. This is a monumental step toward the creation of a JCV model when considered in the context of xenotransplantation foreshadowed by the teams of Matoba and Kondo. A research “pocket” of xenotransplanted cerebral organoids could better reflect the multicellular environment of JCV-driven PML while borrowing the metabolism and blood–brain barrier of host mice, bridging the gap between basic science research and clinical investigations. In researching xenotransplantation, Dong et al. (2021) and Bao et al. (2021) successfully injected human organoids into murine brains. The human cells formed synaptic and angiogenic connections with their murine neighbors, producing an in vivo model with a more accurate human. Ex vivo infection of human organoids and their incorporation into mouse brains may, therefore, produce a humanized model, a necessary stage for assessing the safety and bioavailability of new JCV therapies and diagnostics prior to clinical trials.
Outside of neuroprotectants or neuro-regeneration, the only true treatment for PML is prevention, as neurodegeneration and central nervous system demyelination are irreversible. Agnoprotein has been proposed as a promising target, as cells actively producing JCV release the early-late protein into the environment prior to cell lysis (Otlu et al. 2014). Potentially acting as a viroporin primer for the anticipated release of virions, agnoprotein interacts with adjacent uninfected cells (Suzuki et al. 2010; Saribas et al. 2018). The ability to detect the 5kD agnoprotein prior to its triggering of apoptosis is complicated by the absence of a preclinical model and the patency of the blood–brain barrier. Highly sensitive diagnostics, like sandwich ELISA and RT-LAMP, have been validated for identifying minute levels of viral proteins and RNA (Morioka et al. 2014; Zai et al. 2018; Huang et al. 2020; Tanimoto et al. 2022). Targeting agnoprotein in the blood may now be possible for early identification of JC-reactivation and pre-symptom PML screening.
Advancements in JCV research have well exceeded those of PML, despite the polyomavirus being discovered nearly a decade after the disease’s definition. There is a distinct pathologic link between the infection and its disease, but no such link has entered the clinical sphere diagnostically or therapeutically with the exception of very specific iatrogenic prevention. We have the technology, today, to improve patient outcomes by developing realistic screens, translational preclinical models, and JC-targeting therapies, all necessary tools to better aid individuals of the heterogenous PML patient population.
References
Abbott TR, Dhamdhere G, Liu Y et al (2020) Development of CRISPR as an antiviral strategy to combat SARS-CoV-2 and influenza. Cell 181:865-876.e12. https://doi.org/10.1016/j.cell.2020.04.020
Agostini HT, Ryschkewitsch CF, Singer EJ, Stoner GL (1997) JC virus regulatory region rearrangements and genotypes in progressive multifocal leukoencephalopathy: two independent aspects of virus variation. J Gen Virol 78:659–664. https://doi.org/10.1099/0022-1317-78-3-659
Akan I, Sariyer IK, Biffi R et al (2006) Human polyomavirus JCV late leader peptide region contains important regulatory elements. Virology 349:66–78. https://doi.org/10.1016/j.virol.2006.01.025
Anand P, Hotan GC, Vogel A et al (2019) Progressive multifocal leukoencephalopathy: a 25-year retrospective cohort study. Neurol Neuroimmunol Neuroinflamm 6:e618. https://doi.org/10.1212/NXI.0000000000000618
Astrom KE, Mancall EL, Richardson EP (1958) Progressive multifocal leuko-encephalopathy; a hitherto unrecognized complication of chronic lymphatic leukaemia and Hodgkin’s disease. Brain 81:93–111. https://doi.org/10.1093/brain/81.1.93
Ault GS (1997) Activity of JC virus archetype and PML-type regulatory regions in glial cells. J Gen Virol 78(Pt 1):163–169. https://doi.org/10.1099/0022-1317-78-1-163
Ault GS, Stoner GL (1993) Human polyomavirus JC promoter/enhancer rearrangement patterns from progressive multifocal leukoencephalopathy brain are unique derivatives of a single archetypal structure. J Gen Virol 74(Pt 8):1499–1507. https://doi.org/10.1099/0022-1317-74-8-1499
Bakal JA, Charlton CL, Hlavay B et al (2021) Progressive multifocal leukoencephalopathy and Creutzfeldt-Jakob disease: population-wide incidences, comorbidities, costs of care, and outcomes. J Neurovirol 27:476–481. https://doi.org/10.1007/s13365-021-00983-z
Bao Z, Fang K, Miao Z et al (2021) Human cerebral organoid implantation alleviated the neurological deficits of traumatic brain injury in mice. Oxid Med Cell Longev 2021:6338722. https://doi.org/10.1155/2021/6338722
Barreras P, Pamies D, Monaco MC et al (2022) A human-derived 3D brain organoid model to study JC virus infection. J Neurovirol 28:17–26. https://doi.org/10.1007/s13365-022-01062-7
Berger JR (2014) Chapter 17 - Progressive multifocal leukoencephalopathy. In: Tselis AC, Booss J (eds) Handbook of Clinical Neurology. Elsevier, pp 357–376
Berger JR, Aksamit AJ, Clifford DB et al (2013a) PML diagnostic criteria: consensus statement from the AAN Neuroinfectious Disease Section. Neurology 80:1430–1438. https://doi.org/10.1212/WNL.0b013e31828c2fa1
Berger JR, Hartung H-P (2023) Commentary: progressive multifocal leukoencephalopathy genetic risk variants for pharmacovigilance of immunosuppressant therapies. Front Neurol 14:1146027. https://doi.org/10.3389/fneur.2023.1146027
Berger JR, Houff SA, Gurwell J et al (2013b) JC virus antibody status underestimates infection rates. Ann Neurol 74:84–90. https://doi.org/10.1002/ana.23893
Berger JR, Koralnik IJ (2005) Progressive multifocal leukoencephalopathy and natalizumab–unforeseen consequences. N Engl J Med 353:414–416. https://doi.org/10.1056/NEJMe058122
Bofill-Mas S, Clemente-Casares P, Major EO et al (2003) Analysis of the excreted JC virus strains and their potential oral transmission. J Neurovirol 9:498–507. https://doi.org/10.1080/13550280390218887
Bofill-Mas S, Formiga-Cruz M, Clemente-Casares P et al (2001) Potential transmission of human polyomaviruses through the gastrointestinal tract after exposure to virions or viral DNA. J Virol 75:10290–10299. https://doi.org/10.1128/JVI.75.21.10290-10299.2001
Bofill-Mas S, Girones R (2003) Role of the environment in the transmission of JC virus. J Neurovirol 9:54–58. https://doi.org/10.1080/13550280390195306
Bollag B, Hofstetter CA, Reviriego-Mendoza MM, Frisque RJ (2010) JC virus small T antigen binds phosphatase PP2A and Rb family proteins and is required for efficient viral DNA replication activity. PLoS One 5:e10606. https://doi.org/10.1371/journal.pone.0010606
Brambilla AM, Castagna A, Novati R et al (1999) Remission of AIDS-associated progressive multifocal leukoencephalopathy after cidofovir therapy. J Neurol 246:723–725. https://doi.org/10.1007/s004150050440
Brickelmaier M, Lugovskoy A, Kartikeyan R et al (2009) Identification and characterization of mefloquine efficacy against JC virus in vitro. Antimicrob Agents Chemother 53:1840–1849. https://doi.org/10.1128/AAC.01614-08
Chapagain ML, Sumibcay L, Gurjav U et al (2008) Serotonin receptor 2A blocker (risperidone) has no effect on human polyomavirus JC infection of primary human fetal glial cells. J Neurovirol 14:448–454. https://doi.org/10.1080/13550280802235916
Chen NN, Kerr D, Chang CF et al (1997) Evidence for regulation of transcription and replication of the human neurotropic virus JCV genome by the human S(mu)bp-2 protein in glial cells. Gene 185:55–62. https://doi.org/10.1016/s0378-1119(96)00630-0
Cheng Y, Ma N, Witt C et al (2021) Face masks effectively limit the probability of SARS-CoV-2 transmission. Science 372:1439–1443. https://doi.org/10.1126/science.abg6296
Chiang C, Dvorkin S, Chiang JJ et al (2021) The small t antigen of JC virus antagonizes RIG-I-mediated innate immunity by inhibiting TRIM25’s RNA binding ability. mBio 12:e00620–21. https://doi.org/10.1128/mBio.00620-21
Christensen KLY, Holman RC, Hammett TA et al (2010) Progressive multifocal leukoencephalopathy deaths in the USA, 1979–2005. Neuroepidemiology 35:178–184. https://doi.org/10.1159/000311014
Cortese I, Muranski P, Enose-Akahata Y et al (2019) Pembrolizumab treatment for progressive multifocal leukoencephalopathy. N Engl J Med 380:1597–1605. https://doi.org/10.1056/NEJMoa1815039
Cortese I, Reich DS, Nath A (2021) Progressive multifocal leukoencephalopathy and the spectrum of JC virus-related disease. Nat Rev Neurol 17:37–51. https://doi.org/10.1038/s41582-020-00427-y
Dang X, Axthelm MK, Letvin NL, Koralnik IJ (2005) Rearrangement of simian virus 40 regulatory region is not required for induction of progressive multifocal leukoencephalopathy in immunosuppressed rhesus monkeys. J Virol 79:1361–1366. https://doi.org/10.1128/JVI.79.3.1361-1366.2005
Daniel AM, Swenson JJ, Mayreddy RP et al (1996) Sequences within the early and late promoters of archetype JC virus restrict viral DNA replication and infectivity. Virology 216:90–101. https://doi.org/10.1006/viro.1996.0037
Daniel DC, Wortman MJ, Schiller RJ et al (2001) Coordinate effects of human immunodeficiency virus type 1 protein Tat and cellular protein Puralpha on DNA replication initiated at the JC virus origin. J Gen Virol 82:1543–1553. https://doi.org/10.1099/0022-1317-82-7-1543
Daniels R, Rusan NM, Wadsworth P, Hebert DN (2006) SV40 VP2 and VP3 insertion into ER membranes is controlled by the capsid protein VP1: implications for DNA translocation out of the ER. Mol Cell 24:955–966. https://doi.org/10.1016/j.molcel.2006.11.001
d’Arminio Monforte A, Cinque P, Vago L et al (1997) A comparison of brain biopsy and CSF-PCR in the diagnosis of CNS lesions in AIDS patients. J Neurol 244:35–39. https://doi.org/10.1007/pl00007727
Dash PK, Kaminski R, Bella R et al (2019) Sequential LASER ART and CRISPR treatments eliminate HIV-1 in a subset of infected humanized mice. Nat Commun 10:2753. https://doi.org/10.1038/s41467-019-10366-y
Datta PK, Kaminski R, Hu W et al (2016) HIV-1 latency and eradication: past, present and future. Curr HIV Res 14:431–441. https://doi.org/10.2174/1570162x14666160324125536
De Luca A, Ammassari A, Pezzotti P et al (2008) Cidofovir in addition to antiretroviral treatment is not effective for AIDS-associated progressive multifocal leukoencephalopathy: a multicohort analysis. AIDS 22:1759–1767. https://doi.org/10.1097/QAD.0b013e32830a5043
De Luca A, Fantoni M, Tartaglione T, Antinori A (1999) Response to cidofovir after failure of antiretroviral therapy alone in AIDS-associated progressive multifocal leukoencephalopathy. Neurology 52:891–892. https://doi.org/10.1212/wnl.52.4.891
Deckhut AM, Tevethia MJ, Haggerty S et al (1991) Localization of common cytotoxic T lymphocyte recognition epitopes on simian papovavirus SV40 and human papovavirus JC virus T antigens. Virology 183:122–132. https://doi.org/10.1016/0042-6822(91)90125-u
Del Valle L, Khalili K (2021) Induction of brain tumors by the archetype strain of human neurotropic JCPyV in a transgenic mouse model. Viruses 13:162. https://doi.org/10.3390/v13020162
Del Valle L, White MK, Enam S et al (2005) Detection of JC virus DNA sequences and expression of viral T antigen and agnoprotein in esophageal carcinoma. Cancer 103:516–527. https://doi.org/10.1002/cncr.20806
Devireddy LR, Kumar KU, Pater MM, Pater A (2000) BAG-1, a novel Bcl-2-interacting protein, activates expression of human JC virus. J Gen Virol 81:351–357. https://doi.org/10.1099/0022-1317-81-2-351
Dolci M, Favero C, Bollati V et al (2018) Particulate matter exposure increases JC polyomavirus replication in the human host. Environ Pollut 241:234–239. https://doi.org/10.1016/j.envpol.2018.05.044
Dong X, Xu S-B, Chen X et al (2021) Human cerebral organoids establish subcortical projections in the mouse brain after transplantation. Mol Psychiatry 26:2964–2976. https://doi.org/10.1038/s41380-020-00910-4
Dsilva L, McCarthy K, Lyons J et al (2023) Progressive multifocal leukoencephalopathy with natalizumab extended or standard interval dosing in the United States and the rest of the world. Expert Opinion on Drug Safety 0:1–8. https://doi.org/10.1080/14740338.2023.2221027
Du Pasquier RA, Clark KW, Smith PS et al (2001) JCV-specific cellular immune response correlates with a favorable clinical outcome in HIV-infected individuals with progressive multifocal leukoencephalopathy. J Neurovirol 7:318–322. https://doi.org/10.1080/13550280152537175
Du Pasquier RA, Kuroda MJ, Zheng Y et al (2004) A prospective study demonstrates an association between JC virus-specific cytotoxic T lymphocytes and the early control of progressive multifocal leukoencephalopathy. Brain 127:1970–1978. https://doi.org/10.1093/brain/awh215
Egli A, Infanti L, Dumoulin A et al (2009) Prevalence of polyomavirus BK and JC infection and replication in 400 healthy blood donors. J Infect Dis 199:837–846. https://doi.org/10.1086/597126
Elsner C, Dörries K (1998) Human polyomavirus JC control region variants in persistently infected CNS and kidney tissue. J Gen Virol 79(Pt 4):789–799. https://doi.org/10.1099/0022-1317-79-4-789
Enam S, Del Valle L, Lara C et al (2002) Association of human polyomavirus JCV with colon cancer: evidence for interaction of viral T-antigen and beta-catenin. Cancer Res 62:7093–7101
Epperla N, Medina-Flores R, Mazza JJ, Yale SH (2014) Mirtazapine and mefloquine therapy for non-AIDS-related progressive multifocal leukoencephalopathy. WMJ 113:242–245
Fang C-Y, Chen S-Y, Hsiao B-X et al (2022) Unusually high incidence of polyomavirus JC infection in the higher grade of colorectal cancer tissues in Taiwan. Eur J Med Res 27:127. https://doi.org/10.1186/s40001-022-00756-2
Fedele CG, Ciardi MR, Delia S et al (2003) Identical rearranged forms of JC polyomavirus transcriptional control region in plasma and cerebrospinal fluid of acquired immunodeficiency syndrome patients with progressive multifocal leukoencephalopathy. J Neurovirol 9:551–558. https://doi.org/10.1080/13550280390241188
Ferretti F, Bestetti A, Yiannoutsos CT et al (2018) Diagnostic and prognostic value of JC Virus DNA in plasma in progressive multifocal leukoencephalopathy. Clin Infect Dis 67:65–72. https://doi.org/10.1093/cid/ciy030
Flaegstad T, Sundsfjord A, Arthur RR et al (1991) Amplification and sequencing of the control regions of BK and JC virus from human urine by polymerase chain reaction. Virology 180:553–560. https://doi.org/10.1016/0042-6822(91)90069-n
Frisque RJ, Bream GL, Cannella MT (1984) Human polyomavirus JC virus genome. J Virol 51:458–469. https://doi.org/10.1128/JVI.51.2.458-469.1984
Frohman EM, Monaco MC, Remington G et al (2014) JC virus in CD34+ and CD19+ cells in patients with multiple sclerosis treated with natalizumab. JAMA Neurol 71:596–602. https://doi.org/10.1001/jamaneurol.2014.63
Gan D-D, Reiss K, Carrill T et al (2001) Involvement of Wnt signaling pathway in murine medulloblastoma induced by human neurotropic JC virus. Oncogene 20:4864–4870. https://doi.org/10.1038/sj.onc.1204670
Gasnault J, Kousignian P, Kahraman M et al (2001) Cidofovir in AIDS-associated progressive multifocal leukoencephalopathy: a monocenter observational study with clinical and JC virus load monitoring. J Neurovirol 7:375–381. https://doi.org/10.1080/13550280152537274
Gasparovic ML, Gee GV, Atwood WJ (2006) JC virus minor capsid proteins Vp2 and Vp3 are essential for virus propagation. J Virol 80:10858–10861. https://doi.org/10.1128/JVI.01298-06
Ghosh S, Goldin E, Gordon FH et al (2003) Natalizumab for active Crohn’s disease. N Engl J Med 348:24–32. https://doi.org/10.1056/NEJMoa020732
Gordon J, Del Valle L, Otte J, Khalili K (2000) Pituitary neoplasia induced by expression of human neurotropic polyomavirus, JCV, early genome in transgenic mice. Oncogene 19:4840–4846. https://doi.org/10.1038/sj.onc.1203849
Gorelik L, Reid C, Testa M et al (2011) Progressive multifocal leukoencephalopathy (PML) development is associated with mutations in JC virus capsid protein VP1 that change its receptor specificity. J Infect Dis 204:103–114. https://doi.org/10.1093/infdis/jir198
Grinnell BW, Martin JD, Padgett BL, Walker DL (1983) Naturally occurring and passage-induced variation in the genome of JC virus. Prog Clin Biol Res 105:61–77
Ho P-R, Koendgen H, Campbell N et al (2017) Risk of natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: a retrospective analysis of data from four clinical studies. Lancet Neurol 16:925–933. https://doi.org/10.1016/S1474-4422(17)30282-X
Hogan TF, Padgett BL, Walker DL et al (1980) Rapid detection and identification of JC virus and BK virus in human urine by using immunofluorescence microscopy. J Clin Microbiol 11:178–183. https://doi.org/10.1128/jcm.11.2.178-183.1980
Holman RC, Janssen RS, Buehler JW et al (1991) Epidemiology of progressive multifocal leukoencephalopathy in the United States: analysis of national mortality and AIDS surveillance data. Neurology 41:1733–1736. https://doi.org/10.1212/wnl.41.11.1733
Huang WE, Lim B, Hsu C-C et al (2020) RT-LAMP for rapid diagnosis of coronavirus SARS-CoV-2. Microb Biotechnol 13:950–961. https://doi.org/10.1111/1751-7915.13586
Huang Y-L, Wang M, Ou W-C et al (2003) Analysis of DNA-binding activity of the JC virus minor capsid protein VP2. J Neurovirol 9(Suppl 1):21–24. https://doi.org/10.1080/13550280390195289
Iannetta M, Zingaropoli MA, Bellizzi A et al (2016) Natalizumab affects T-cell phenotype in multiple sclerosis: implications for JCV reactivation. PLoS One 11:e0160277. https://doi.org/10.1371/journal.pone.0160277
Iannetta M, Zingaropoli MA, Latronico T et al (2019) Dynamic changes of MMP-9 plasma levels correlate with JCV reactivation and immune activation in natalizumab-treated multiple sclerosis patients. Sci Rep 9:311. https://doi.org/10.1038/s41598-018-36535-5
Iida T, Kitamura T, Guo J et al (1993) Origin of JC polyomavirus variants associated with progressive multifocal leukoencephalopathy. Proc Natl Acad Sci USA 90:5062–5065. https://doi.org/10.1073/pnas.90.11.5062
Ikeda J, Matsushima A, Ishii W et al (2017) Brain biopsy is more reliable than the DNA test for JC virus in cerebrospinal fluid for the diagnosis of progressive multifocal leukoencephalopathy. Intern Med 56:1231–1234. https://doi.org/10.2169/internalmedicine.56.7689
Jamilloux Y, Kerever S, Ferry T et al (2016) Treatment of progressive multifocal leukoencephalopathy with mirtazapine. Clin Drug Investig 36:783–789. https://doi.org/10.1007/s40261-016-0433-8
Jiang Z-G, Cohen J, Marshall LJ, Major EO (2010) Hexadecyloxypropyl-cidofovir (CMX001) suppresses JC virus replication in human fetal brain SVG cell cultures. Antimicrob Agents Chemother 54:4723–4732. https://doi.org/10.1128/AAC.00837-10
Kaminski R, Chen Y, Fischer T et al (2016) Elimination of HIV-1 genomes from human T-lymphoid cells by CRISPR/Cas9 gene editing. Sci Rep 6:22555. https://doi.org/10.1038/srep22555
Kato K, Guo J, Taguchi F et al (1994) Phylogenetic comparison between archetypal and disease-associated JC virus isolates in Japan. Jpn J Med Sci Biol 47:167–178. https://doi.org/10.7883/yoken1952.47.167
Kitamura T, Aso Y, Kuniyoshi N et al (1990) High incidence of urinary JC virus excretion in nonimmunosuppressed older patients. J Infect Dis 161:1128–1133. https://doi.org/10.1093/infdis/161.6.1128
Kitamura T, Sugimoto C, Kato A et al (1997) Persistent JC virus (JCV) infection is demonstrated by continuous shedding of the same JCV strains. J Clin Microbiol 35:1255–1257
Kleinschmidt-DeMasters BK, Tyler KL (2005) Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N Engl J Med 353:369–374. https://doi.org/10.1056/NEJMoa051782
Kobayashi S, Suzuki T, Igarashi M et al (2013) Cysteine residues in the major capsid protein, Vp1, of the JC virus are important for protein stability and oligomer formation. PLoS One 8:e76668. https://doi.org/10.1371/journal.pone.0076668
Kondo Y, Windrem MS, Zou L et al (2014) Human glial chimeric mice reveal astrocytic dependence of JC virus infection. J Clin Invest 124:5323–5336. https://doi.org/10.1172/JCI76629
Koralnik IJ (2002) Overview of the cellular immunity against JC virus in progressive multifocal leukoencephalopathy. J Neurovirol 8(Suppl 2):59–65. https://doi.org/10.1080/13550280290167894
Krauzewicz N, Streuli CH, Stuart-Smith N et al (1990) Myristylated polyomavirus VP2: role in the life cycle of the virus. J Virol 64:4414–4420. https://doi.org/10.1128/JVI.64.9.4414-4420.1990
Krynska B, Gordon J, Otte J et al (1997) Role of cell cycle regulators in tumor formation in transgenic mice expressing the human neurotropic virus, JCV, early protein. J Cell Biochem 67:223–230. https://doi.org/10.1002/(SICI)1097-4644(19971101)67:2%3c223::AID-JCB7%3e3.0.CO;2-Z
Kurmann R, Weisstanner C, Kardas P et al (2015) Progressive multifocal leukoencephalopathy in common variable immunodeficiency: mitigated course under mirtazapine and mefloquine. J Neurovirol 21:694–701. https://doi.org/10.1007/s13365-015-0340-4
Langer-Gould A, Atlas SW, Green AJ et al (2005) Progressive multifocal leukoencephalopathy in a patient treated with natalizumab. N Engl J Med 353:375–381. https://doi.org/10.1056/NEJMoa051847
Leech G, Rogers-Smith C, Monrad JT et al (2022) Mask wearing in community settings reduces SARS-CoV-2 transmission. Proc Natl Acad Sci USA 119:e2119266119. https://doi.org/10.1073/pnas.2119266119
London WT, Houff SA, Madden DL et al (1978) Brain tumors in owl monkeys inoculated with a human polyomavirus (JC virus). Science 201:1246–1249. https://doi.org/10.1126/science.211583
London WT, Houff SA, McKeever PE et al (1983) Viral-induced astrocytomas in squirrel monkeys. Prog Clin Biol Res 105:227–237
Maas RPPWM, Muller-Hansma AHG, Esselink RAJ et al (2016) Drug-associated progressive multifocal leukoencephalopathy: a clinical, radiological, and cerebrospinal fluid analysis of 326 cases. J Neurol 263:2004–2021. https://doi.org/10.1007/s00415-016-8217-x
Mancuso P, Chen C, Kaminski R et al (2020) CRISPR based editing of SIV proviral DNA in ART treated non-human primates. Nat Commun 11:6065. https://doi.org/10.1038/s41467-020-19821-7
Marra CM, Rajicic N, Barker DE et al (2002) A pilot study of cidofovir for progressive multifocal leukoencephalopathy in AIDS. AIDS 16:1791–1797. https://doi.org/10.1097/00002030-200209060-00012
Marshall LJ, Dunham L, Major EO (2010) Transcription factor Spi-B binds unique sequences present in the tandem repeat promoter/enhancer of JC virus and supports viral activity. J Gen Virol 91:3042–3052. https://doi.org/10.1099/vir.0.023184-0
Martin JD, King DM, Slauch JM, Frisque RJ (1985) Differences in regulatory sequences of naturally occurring JC virus variants. J Virol 53:306–311. https://doi.org/10.1128/JVI.53.1.306-311.1985
Martins F, Sofiya L, Sykiotis GP et al (2019) Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol 16:563–580. https://doi.org/10.1038/s41571-019-0218-0
Matoba T, Orba Y, Suzuki T et al (2008) An siRNA against JC virus (JCV) agnoprotein inhibits JCV infection in JCV-producing cells inoculated in nude mice. Neuropathology 28:286–294. https://doi.org/10.1111/j.1440-1789.2007.00878.x
Mayberry CL, Soucy AN, Lajoie CR et al (2019) JC polyomavirus entry by clathrin-mediated endocytosis is driven by β-arrestin. J Virol 93:e01948-e2018. https://doi.org/10.1128/JVI.01948-18
Merabova N, Kaniowska D, Kaminski R et al (2008) JC virus agnoprotein inhibits in vitro differentiation of oligodendrocytes and promotes apoptosis. J Virol 82:1558–1569. https://doi.org/10.1128/JVI.01680-07
Miller DH, Khan OA, Sheremata WA et al (2003) A controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med 348:15–23. https://doi.org/10.1056/NEJMoa020696
Morioka K, Fukai K, Sakamoto K et al (2014) Evaluation of monoclonal antibody-based sandwich direct ELISA (MSD-ELISA) for antigen detection of foot-and-mouth disease virus using clinical samples. PLoS One 9:e94143. https://doi.org/10.1371/journal.pone.0094143
Muftuoglu M, Olson A, Marin D et al (2018) Allogeneic BK virus–specific t cells for progressive multifocal leukoencephalopathy. N Engl J Med 379:1443–1451. https://doi.org/10.1056/NEJMoa1801540
Nakanishi A, Nakamura A, Liddington R, Kasamatsu H (2006) Identification of amino acid residues within simian virus 40 capsid proteins Vp1, Vp2, and Vp3 that are required for their interaction and for viral infection. J Virol 80:8891–8898. https://doi.org/10.1128/JVI.00781-06
Nambirajan A, Suri V, Kataria V et al (2017) Progressive multifocal leukoencephalopathy in a 44-year old male with idiopathic CD4+ T-lymphocytopenia treated with mirtazapine and mefloquine. Neurol India 65:1061–1064. https://doi.org/10.4103/neuroindia.NI_535_16
Oh D-Y, Buda S, Biere B et al (2021) Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January - September 2020: Analysis of national surveillance data. Lancet Reg Health Eur 6:100112. https://doi.org/10.1016/j.lanepe.2021.100112
Okada Y, Endo S, Takahashi H et al (2001) Distribution and function of JCV agnoprotein. J Neurovirol 7:302–306. https://doi.org/10.1080/13550280152537148
Okada Y, Sawa H, Tanaka S et al (2000) Transcriptional activation of JC virus by human T-lymphotropic virus type I Tax protein in human neuronal cell lines. J Biol Chem 275:17016–17023. https://doi.org/10.1074/jbc.275.22.17016
O’Neill FJ, Greenlee JE, Dörries K et al (2003) Propagation of archetype and nonarchetype JC virus variants in human fetal brain cultures: demonstration of interference activity by archetype JC virus. J Neurovirol 9:567–576. https://doi.org/10.1080/13550280390241223
Otlu O, De Simone FI, Otalora Y-L et al (2014) The agnoprotein of polyomavirus JC is released by infected cells: evidence for its cellular uptake by uninfected neighboring cells. Virology 0:88–95. https://doi.org/10.1016/j.virol.2014.07.054
Ou W-C, Chen L-H, Wang M et al (2001) Analysis of minimal sequences on JC virus VP1 required for capsid assembly. J Neurovirol 7:298–301. https://doi.org/10.1080/13550280152537139
Padgett BL, Zurhein GM, Walker DL et al (1971) Cultivation of papova-like virus from human brain with progressive multifocal leucoencephalopathy. The Lancet 297:1257–1260. https://doi.org/10.1016/S0140-6736(71)91777-6
Padgett BL, Walker DL (1973) Prevalence of antibodies in human sera against JC virus, an isolate from a case of progressive multifocal leukoencephalopathy. J Infect Dis 127:467–470. https://doi.org/10.1093/infdis/127.4.467
Padgett BL, Walker DL, ZuRhein GM et al (1976) JC Papovavirus in progressive multifocal leukoencephalopathy. J Infect Dis 133:686–690. https://doi.org/10.1093/infdis/133.6.686
Paz SPC, Branco L, Pereira MA, de C et al (2018) Systematic review of the published data on the worldwide prevalence of John Cunningham virus in patients with multiple sclerosis and neuromyelitis optica. Epidemiol Health 40:e2018001. https://doi.org/10.4178/epih.e2018001
Peretti A, Scorpio DG, Kong W-P et al (2023) A multivalent polyomavirus vaccine elicits durable neutralizing antibody responses in macaques. Vaccine 41:1735–1742. https://doi.org/10.1016/j.vaccine.2023.02.002
Pfister LA, Letvin NL, Koralnik IJ (2001) JC virus regulatory region tandem repeats in plasma and central nervous system isolates correlate with poor clinical outcome in patients with progressive multifocal leukoencephalopathy. J Virol 75:5672–5676. https://doi.org/10.1128/JVI.75.12.5672-5676.2001
Pietropaolo V, Videtta M, Fioriti D et al (2003) Rearrangement patterns of JC virus noncoding control region from different biological samples. J Neurovirol 9:603–611. https://doi.org/10.1080/13550280390246507
Piu C, Ibba G, Bertoli D et al (2020) Early reduction of the splicing factor2/alternative splicing factor: a cellular inhibitor of the JC polyomavirus in natalizumab-treated MS patients long before developing progressive multifocal leukoencephalopathy. J Neurovirol 26:133–137. https://doi.org/10.1007/s13365-019-00793-4
Querbes W, Benmerah A, Tosoni D et al (2004) A JC virus-induced signal is required for infection of glial cells by a clathrin- and eps15-dependent pathway. J Virol 78:250–256. https://doi.org/10.1128/JVI.78.1.250-256.2004
Querido S, Fernandes I, Weigert A et al (2020) High-grade urothelial carcinoma in a kidney transplant recipient after JC virus nephropathy: the first evidence of JC virus as a potential oncovirus in bladder cancer. Am J Transplant 20:1188–1191. https://doi.org/10.1111/ajt.15663
Ravichandran V, Sabath BF, Jensen PN et al (2006) Interactions between c-Jun, nuclear factor 1, and JC virus promoter sequences: implications for viral tropism. J Virol 80:10506–10513. https://doi.org/10.1128/JVI.01355-06
Ray U, Cinque P, Gerevini S et al (2015) JC polyomavirus mutants escape antibody-mediated neutralization. Sci Transl Med 7:306ra151. https://doi.org/10.1126/scitranslmed.aab1720
Richardson EP (1961) Progressive multifocal leukoencephalopathy. N Engl J Med 265:815–823. https://doi.org/10.1056/NEJM196110262651701
Richardson EP Jr (1974) Our evolving understanding of progressive multifocal leukoencephalopathy*. Ann N Y Acad Sci 230:358–364. https://doi.org/10.1111/j.1749-6632.1974.tb14469.x
Safak M, Barrucco R, Darbinyan A et al (2001) Interaction of JC virus agno protein with T antigen modulates transcription and replication of the viral genome in glial cells. J Virol 75:1476–1486. https://doi.org/10.1128/JVI.75.3.1476-1486.2001
Saribas AS, Mun S, Johnson J et al (2014) Human polyoma JC virus minor capsid proteins, VP2 and VP3, enhance large T antigen binding to the origin of viral DNA replication: evidence for their involvement in regulation of the viral DNA replication. Virology 449:1–16. https://doi.org/10.1016/j.virol.2013.10.031
Saribas AS, White MK, Safak M (2018) Structure-based release analysis of the JC virus agnoprotein regions: A role for the hydrophilic surface of the major alpha helix domain in release. J Cell Physiol 233:2343–2359. https://doi.org/10.1002/jcp.26106
Saribas S, Safak M (2020) A comprehensive proteomics analysis of the JC virus (JCV) large and small tumor antigen interacting proteins: large T primarily targets the host protein complexes with V-ATPase and ubiquitin ligase activities while small t mostly associates with those having phosphatase and chromatin-remodeling functions. Viruses 12:1192. https://doi.org/10.3390/v12101192
Sariyer IK, Khalili K (2011) Regulation of human neurotropic JC virus replication by alternative splicing factor SF2/ASF in glial cells. PLoS One 6:e14630. https://doi.org/10.1371/journal.pone.0014630
Saxena R, Saribas S, Jadiya P et al (2021) Human neurotropic polyomavirus, JC virus, agnoprotein targets mitochondrion and modulates its functions. Virology 553:135–153. https://doi.org/10.1016/j.virol.2020.11.004
Shavaleh R, Kamandi M, Feiz Disfani H et al (2020) Association between JC virus and colorectal cancer: systematic review and meta-analysis. Infect Dis (lond) 52:152–160. https://doi.org/10.1080/23744235.2019.1692145
Sheridan C (2006) Tysabri back on market. Nat Biotechnol 24:874–874. https://doi.org/10.1038/nbt0806-874
Shin SK, Li M-S, Fuerst F et al (2006) Oncogenic T-antigen of JC virus is present frequently in human gastric cancers. Cancer 107:481–488. https://doi.org/10.1002/cncr.22028
Shishido-Hara Y, Hara Y, Larson T et al (2000) Analysis of capsid formation of human polyomavirus JC (Tokyo-1 strain) by a eukaryotic expression system: splicing of late RNAs, translation and nuclear transport of major capsid protein VP1, and capsid assembly. J Virol 74:1840–1853. https://doi.org/10.1128/jvi.74.4.1840-1853.2000
Shishido-Hara Y, Ichinose S, Higuchi K et al (2004) Major and minor capsid proteins of human polyomavirus JC cooperatively accumulate to nuclear domain 10 for assembly into virions. J Virol 78:9890–9903. https://doi.org/10.1128/JVI.78.18.9890-9903.2004
Simon MA, Ilyinskii PO, Baskin GB et al (1999) Association of simian virus 40 with a central nervous system lesion distinct from progressive multifocal leukoencephalopathy in macaques with AIDS. Am J Pathol 154:437–446. https://doi.org/10.1016/S0002-9440(10)65290-X
Sock E, Renner K, Feist D et al (1996) Functional comparison of PML-type and archetype strains of JC virus. J Virol 70:1512–1520. https://doi.org/10.1128/jvi.70.3.1512-1520.1996
Stoner GL, Ryschkewitsch CF (1995) Capsid protein VP1 deletions in JC virus from two AIDS patients with progressive multifocal leukoencephalopathy. J Neurovirol 1:189–194. https://doi.org/10.3109/13550289509113965
Summers NA, Kelley CF, Armstrong W et al (2019) Not a disease of the past: a case series of progressive multifocal leukoencephalopathy in the established antiretroviral era. AIDS Res Hum Retroviruses 35:544–552. https://doi.org/10.1089/AID.2018.0232
Suzuki T, Orba Y, Okada Y et al (2010) The Human polyoma JC virus agnoprotein acts as a viroporin. PLOS Pathogens 6:e1000801. https://doi.org/10.1371/journal.ppat.1000801
Swinnen B, Saegeman V, Beuselinck K et al (2019) Predictive value of JC virus PCR in cerebrospinal fluid in the diagnosis of PML. Diagnostic Microbiology and Infectious Disease 95:114859. https://doi.org/10.1016/j.diagmicrobio.2019.06.011
Tan CS, Ellis LC, Wüthrich C et al (2010) JC virus latency in the brain and extraneural organs of patients with and without progressive multifocal leukoencephalopathy. J Virol 84:9200–9209. https://doi.org/10.1128/JVI.00609-10
Tanimoto Y, Mori A, Miyamoto S et al (2022) Comparison of RT-PCR, RT-LAMP, and antigen quantification assays for the detection of SARS-CoV-2. Jpn J Infect Dis 75:249–253. https://doi.org/10.7883/yoken.JJID.2021.476
Tornatore C, Berger JR, Houff SA et al (1992) Detection of JC virus DNA in peripheral lymphocytes from patients with and without progressive multifocal leukoencephalopathy. Ann Neurol 31:454–462. https://doi.org/10.1002/ana.410310426
Uleri E, Regan P, Dolei A, Sariyer IK (2013) SF2/ASF binding region within JC virus NCCR limits early gene transcription in glial cells. Virol J 10:147. https://doi.org/10.1186/1743-422X-10-147
Van Assche G, Van Ranst M, Sciot R et al (2005) Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn’s disease. N Engl J Med 353:362–368. https://doi.org/10.1056/NEJMoa051586
van Diemen FR, Kruse EM, Hooykaas MJG et al (2016) CRISPR/Cas9-mediated genome editing of herpesviruses limits productive and latent infections. PLoS Pathog 12:e1005701. https://doi.org/10.1371/journal.ppat.1005701
Van Loy T, Thys K, Ryschkewitsch C et al (2015) JC virus quasispecies analysis reveals a complex viral population underlying progressive multifocal leukoencephalopathy and supports viral dissemination via the hematogenous route. J Virol 89:1340–1347. https://doi.org/10.1128/JVI.02565-14
Vigiser I, Piura Y, Kolb H et al (2022) JCV seroconversion rate during the SARS COVID-19 pandemic. Multiple Sclerosis and Related Disorders 68:104244. https://doi.org/10.1016/j.msard.2022.104244
Walker DL, Padgett BL, ZuRhein GM et al (1973) Human papovavirus (JC): induction of brain tumors in hamsters. Science 181:674–676. https://doi.org/10.1126/science.181.4100.674
White FA, Ishaq M, Stoner GL, Frisque RJ (1992) JC virus DNA is present in many human brain samples from patients without progressive multifocal leukoencephalopathy. J Virol 66:5726–5734
White MK, Gordon J, Berger JR, Khalili K (2015) Animal models for progressive multifocal leukoencephalopathy. J Cell Physiol 230:2869–2874. https://doi.org/10.1002/jcp.25047
Wilczek MP, Pike AMC, Craig SE et al (2022) Rearrangement in the hypervariable region of JC polyomavirus genomes isolated from patient samples and impact on transcription factor-binding sites and disease outcomes. Int J Mol Sci 23:5699. https://doi.org/10.3390/ijms23105699
Winklhofer KF, Albrecht I, Wegner M, Heilbronn R (2000) Human cytomegalovirus immediate-early gene 2 expression leads to JCV replication in nonpermissive cells via transcriptional activation of JCV T antigen. Virology 275:323–334. https://doi.org/10.1006/viro.2000.0503
Wollebo HS, White MK, Gordon J et al (2015) Persistence and pathogenesis of the neurotropic polyomavirus JC. Ann Neurol 77:560–570. https://doi.org/10.1002/ana.24371
Wortman MJ, Krachmarov CP, Kim JH et al (2000) Interaction of HIV-1 Tat with Puralpha in nuclei of human glial cells: characterization of RNA-mediated protein-protein binding. J Cell Biochem 77:65–74. https://doi.org/10.1002/(sici)1097-4644(20000401)77:1%3c65::aid-jcb7%3e3.0.co;2-u
Yogo Y, Guo J, Iida T et al (1994) Occurrence of multiple JC virus variants with distinctive regulatory sequences in the brain of a single patient with progressive multifocal leukoencephalopathy. Virus Genes 8:99–105. https://doi.org/10.1007/BF01703608
Yogo Y, Iida T, Taguchi F et al (1991) Typing of human polyomavirus JC virus on the basis of restriction fragment length polymorphisms. J Clin Microbiol 29:2130–2138. https://doi.org/10.1128/jcm.29.10.2130-2138.1991
Yogo Y, Kitamura T, Sugimoto C et al (1990) Isolation of a possible archetypal JC virus DNA sequence from nonimmunocompromised individuals. J Virol 64:3139–3143. https://doi.org/10.1128/JVI.64.6.3139-3143.1990
Yousry TA, Major EO, Ryschkewitsch C et al (2006) Evaluation of patients treated with natalizumab for progressive multifocal leukoencephalopathy. N Engl J Med 354:924–933. https://doi.org/10.1056/NEJMoa054693
Yuen K-S, Chan C-P, Wong N-HM et al (2015) CRISPR/Cas9-mediated genome editing of Epstein-Barr virus in human cells. J Gen Virol 96:626–636. https://doi.org/10.1099/jgv.0.000012
Zai J, Yi K, Xie L et al (2018) Dual monoclonal antibody-based sandwich ELISA for detection of in vitro packaged Ebola virus. Diagn Pathol 13:96. https://doi.org/10.1186/s13000-018-0773-1
Zingaropoli MA, Iannetta M, Pontecorvo S et al (2018) JC virus-DNA detection is associated with CD8 effector accumulation in peripheral blood of patients with multiple sclerosis under natalizumab treatment, independently from JC virus serostatus. Biomed Res Int 2018:5297980. https://doi.org/10.1155/2018/5297980
Zurhein G, Chou SM (1965) Particles resembling papova viruses in human cerebral demyelinating disease. Science 148:1477–1479. https://doi.org/10.1126/science.148.3676.1477
Acknowledgements
The authors wish to thank past and present members of the Department of Microbiology, Immunology and Inflammation and Center for Neurovirology and Gene Editing for sharing reagents and ideas.
Funding
This study utilized services offered by core facilities of the Comprehensive NeuroHIV Center (CNHC NIMH Grant Number P30MH092177-11). AR was supported by the training grant "Interdisciplinary and Translational Research Training in NeuroHIV (T32MH079785). Figures were created with Biorender.com.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rocchi, A., Sariyer, I.K. & Berger, J.R. Revisiting JC virus and progressive multifocal leukoencephalopathy. J. Neurovirol. 29, 524–537 (2023). https://doi.org/10.1007/s13365-023-01164-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-023-01164-w