Abstract
Natalizumab is effective against relapsing-remitting multiple sclerosis (MS) but increases the risk of progressive multifocal leukoencephalopathy (PML), which is caused by the activation of the JCV polyomavirus. SF2/ASF (splicing factor2/alternative splicing factor) is a potent cellular inhibitor of JCV replication and large T-antigen (T-Ag) expression. We reported that SF2/ASF levels in blood cells increase during the first year of natalizumab therapy and decrease thereafter, inversely related to T-Ag expression, and suggested a correlation with JCV reactivation. Here, we report SF2/ASF levels of longitudinal blood samples of two patients undergoing natalizumab therapy, who developed PML while monitored, in comparison to natalizumab-treated controls and to one-off PML samples. After 6 months of therapy, SF2/ASF levels of the two cases were reduced, instead of increased, and their overall SF2/ASF levels were lower than those from natalizumab controls. Since SF2/ASF inhibits JCV, its early reduction might have a role in subsequent PML. We are aware of the limitations of the study, but the uniqueness of serial blood samples collected before and after PML onset in natalizumab-treated patients must be stressed. If confirmed in other patients, SF2/ASF evaluation could be a new and early biomarker of natalizumab-associated PML risk, allowing an 18–24-month interval before PML onset (presently ~ 5 months), in which clinicians could evaluate other risk factors and change therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Natalizumab is effective against relapsing-remitting multiple sclerosis (MS, Tintore et al. 2019) but increases the risk of progressive multifocal leukoencephalopathy (PML, Mill and Mao-Draayer 2018). Retrospectively, 78% of PML patients have a presymptomatic phase, recognizable at magnetic resonance imaging ~ 5 months before symptoms (Scarpazza et al. 2019). PML is caused by the JCV polyomavirus (Assetta and Atwood 2017), a ubiquitous opportunistic pathogen, which rarely infects lytically oligodendrocytes, causing PML. Natalizumab mobilizes pre-B and mature B cells from bone marrow to the periphery, possibly spreading JCV (Chalkias et al. 2014). Natalizumab alters transcriptional profiles of blood cells, especially of genes related to immune response, signaling, adhesion, and T and B cell metabolism (Lindberg et al. 2008). PML risk factors are the presence of anti-JCV antibody, previous immunosuppressant therapy, and natalizumab treatment duration > 24 months (Tintore et al. 2019; Mill and Mao-Draayer 2018).
Since JCV is ubiquitous and PML occurs rarely, multiple barriers must exist against disease development. PML occurs in the context of profoundly impaired cell-mediated immunity; natalizumab, preventing normal lymphocyte trafficking, is one of the most important factors contributing to the breakdown of neuroimmunosurveillance (Berger and Koralnik, 2005). The drug alters the expression of genes related to immune response, signal transduction, adhesion, and metabolism relevant for T and B lymphocytes, thus increasing the odds of JCV infection and/or replication in the brain (Lindberg et al. 2008).
The SF2/ASF (splicing factor 2/alternative splicing factor) is a key cellular regulator of alternative splicing (Zhao et al. 2015), which inhibits JCV replication, blocking the expression of large T-antigen (T-Ag, Uleri et al. 2013). Conversely, T-Ag suppresses SF2/ASF transcription, revealing a molecular SF2/ASF and T-Ag interplay in JCV control, and suggesting another mechanism of JCV reactivation in patients at PML risk (Craigie et al. 2015).
We reported that SF2/ASF levels in blood cells of MS patients vary during natalizumab therapy, increasing during the first year, and decreasing thereafter, inversely related to T-Ag (Uleri et al. 2017), and suggested its role in JCV reactivation.
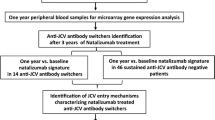
Here, we report data from longitudinal observation of two MS patients undergoing natalizumab therapy, who developed PML while monitored.
Methods
Cases
Case 1: female patient, with 22 years of MS at enrolment, and PML onset after 34 months of natalizumab therapy. Case 2: female patient, with 3 years of MS at enrolment, and PML onset after 25 months of therapy. Serial blood samples were collected within a longitudinal study of MS patients undergoing de novo natalizumab therapy. The five MS patients closest for enrolling in the same time interval and location were selected as natalizumab controls. Four one-off samples of PML cases were included as PML controls. Samples were treated as published (Uleri et al. 2017; Gerevini et al. 2019). Demographic and clinical-pathological data of the patients are reported in Table 1. The study has been performed on already stored samples of the two cases, who had been treated years ago, when the knowledge regarding natalizumab-associated risks and the advisability to discontinue the therapy after > 24 months on the drug, if previously treated with immunosuppressive agent, was not yet accessible. The study was approved by the Brescia Ethical Committee Board (protocols 2713 of 24/05/2017 and NP0 of 07/18/2018).
mRNA extraction, retro-transcription, and real-time RT-PCR
mRNAs were extracted, retro-transcribed, and amplified with SF2/ASF-specific and T-Ag-specific primers (Uleri et al. 2017). Parallel RNA samples were amplified without retro-transcription, to detect contaminant DNA. For each sample, the Ct values of the gene of interest were compared to those of the glyceraldehyde-3-phosphate dehydrogenase gene. The data were expressed according to the 2−ΔCt method (Uleri et al. 2017).
Results
Opposite patterns of SF2/ASF and T-Ag expression in natalizumab-treated patients
During therapy, SF2/ASF levels of blood cells of MS patients changed, showing a bell-shaped pattern, increasing during the first year (mean increase of 2.4-fold at 12 months), then declining (Fig. 1a). Conversely, the T-Ag levels showed a U-shaped pattern (Fig. 1b), fully in line with our findings in a Sardinian cohort (Uleri et al. 2017).
Levels of SF2/ASF and of T-Ag mRNAs in blood cells from MS patients exposed to natalizumab therapy and from PML cases. a, c, e, and g SF2/ASF transcripts; b, d, f, and h T-Ag transcripts. a and b Natalizumab-treated MS patients; mean values and standard deviations. c and d One-off control samples from already established PML cases. e and f Case 1, natalizumab-treated patient, who got PML, while monitored. The arrow indicates PML onset, and the black symbols indicate ongoing PML. g and h Case 2, natalizumab-treated patient, who got PML, while monitored. The arrow indicates PML onset, and the black symbols indicate ongoing PML. The data are expressed according to the 2−ΔCt method (Uleri et al. 2017). See text for details
The opposite behavior of SF2/ASF and T-Ag levels occurred also in the one-off PML control samples (Fig. 1c, d); their SF2/ASF levels were in the range of natalizumab controls, being T-Ag levels were lower in the PML patients with higher SF2/ASF.
Early decrease of SF2/ASF levels in the two patients who will develop PML
In both cases, SF2/ASF levels decreased within the first 6 months of therapy, instead of increasing, then partially recovered, until PML onset. Few weeks after PML onset, SF2/ASF levels of both patients decreased again (Fig. 1e, g).
Also in terms of step-wise comparison, the SF2/ASF levels of the cases were lower than those of natalizumab controls, and differences were highly significant (Fig. 2a). Along ~ 3 years of observation, their overall samples had much less SF2/ASF levels than overall samples from natalizumab controls (p = 0.0004). Interestingly, after 6 months of therapy, the two cases had only 1/14 of the SF2/ASF levels of natalizumab controls (p = 0.028).
Step-wise comparison of SF2/ASF and T-Ag levels during time of the two PML cases and the natalizumab-treated control patients. a SF2/ASF transcripts; b T-Ag transcripts. The statistical significance (p) was calculated by the unpaired two-tailed t test. Open bars, natalizumab-treated control patients; striped bars, PML cases. The data are expressed according to the 2−ΔCt method (Uleri et al. 2017). See text for details
The pre-natalizumab values of T-Ag mRNAs were highly different in the two cases, being > 50-fold higher in case 2, who developed PML at 25 months of therapy, than in case 1, who developed PML after 34 months. This suggests that JCV may have been activated already in case 2, before starting natalizumab therapy (Fig. 1f, h).
In line with the opposite behavior of SF2/ASF and T-Ag levels, the two cases had T-Ag levels higher than the natalizumab controls. However, T-Ag values were low, and a statistically significant difference was observed only at 6 months of therapy (Fig. 2b).
Discussion
The increased risk of developing PML is a major limitation to natalizumab use (Mill and Mao-Draayer 2018). To reduce PML risk and to decide therapy discontinuation, clinicians evaluate the anti-JCV sero-status, even though viremia and cell-mediated anti-JCV response were detected in seronegative individuals (Mill and Mao-Draayer 2018).
In this case report, we confirm, in another cohort, our previous finding (Uleri et al. 2017) that natalizumab therapy initially stimulates, then inhibits SF2/ASF, potent cellular inhibitor of JCV, with a bell-shaped pattern. Conversely, T-Ag levels show a U-shaped pattern (Fig. 1a, b). Therefore, a consequence of SF2/ASF reduction could be JCV reactivation, thus promoting PML onset.
We had the unique opportunity to analyze two MS patients, who developed PML while enrolled in a longitudinal study. The most apparent finding was a drop in SF2/ASF levels within 6 months from therapy start. Along the ~ 3 years of observation, their overall SF2/ASF levels were much lower than those of natalizumab controls. Accordingly, their T-Ag levels were higher than the controls. Importantly, in the two cases, SF2/ASF reduction occurred after 6 months of therapy and 19 and 28 months before PML onset, respectively.
We are aware of the limitations of a study of the two cases, but the uniqueness of serial samples collected before and after PML onset in natalizumab-treated patients must be stressed. Since 2009, 56 cases of natalizumab-associated PML occurred in Italy (Scarpazza et al. 2019). To the best of our knowledge, only our two cases received PML diagnosis while enrolled in a longitudinal study. If confirmed in other patients, SF2/ASF evaluation could be a new and early biomarker of natalizumab-associated PML risk. It would allow an 18–24-month interval before PML onset (much longer than the present 5-month presymptomatic phase, Scarpazza et al. 2019), in which clinicians could evaluate other risk factors and change therapy.
References
Assetta B, Atwood WJ (2017) The biology of JC polyomavirus. Biol Chem 398:839–855. https://doi.org/10.1515/hsz-2016-0345
Berger JR, Koralnik IJ (2005) Progressive multifocal leukoencephalopathy and natalizumab--unforeseen consequences. N Engl J Med 353:414–416. https://doi.org/10.1056/NEJMe058122
Chalkias S, Dang X, Bord E, Stein MC, Kinkel RP, Sloane JA, Donnelly M, Ionete C, Houtchens MK, Buckle GJ, Batson S, Koralnik IJ (2014) JC virus reactivation during prolonged Natalizumab monotherapy for multiple sclerosis. Ann Neurol 75:925–934. https://doi.org/10.1002/ana.24148
Craigie M, Regan P, Otalora YL, Sariyer IK (2015) Molecular interplay between T-antigen and splicing factor, arginine/serine-rich 1 (SRSF1) controls JC virus gene expression in glial cells. Virol J 12:196. https://doi.org/10.1186/s12985-015-0426-x
Gerevini S, Capra R, Bertoli D, Sottini A, Imberti L (2019) Immune profiling of a patient with alemtuzumab-associated progressive multifocal leukoencephalopathy. Mult Scler 25:1196-1201. https://doi.org/10.1177/1352458519832259
Lee P, Plavina T, Castro A, Berman M, Jaiswal D, Rivas S, Schlain B, Subramanyam M (2013) A second-generation ELISA (STRATIFY JCV™ DxSelect™) for detection of JC virus antibodies in human serum and plasma to support progressive multifocal leukoencephalopathy risk stratification. J Clin Virol 57:141–146. https://doi.org/10.1016/j.jcv.2013.02.002
Lindberg RLP, Achtnichts L, Hoffman F, Kuhle J, Kappos L (2008) Natalizumab alters transcriptional expression profiles of blood cell subpopulations of multiple sclerosis patients. J Neuroimmunol 194:153–164. https://doi.org/10.1016/j.jneuroim.2007.11.007
Mill EA, Mao-Draayer Y (2018) Understanding progressive multifocal leukoencephalopathy risk in multiple sclerosis patients treated with immunomodulatory therapies: a bird’s eye view. Front Immunol 9:138. https://doi.org/10.3389/fimmu.2018.00138
Scarpazza C, Signori A, Prosperini L, Sormani MP, Cosottini M, Capra R, Gerevini S, Italian PML Group (2019) Early diagnosis of progressive multifocal leucoencephalopathy: longitudinal lesion evolution. J Neurol Neurosurg Psychiatry 90:261–267. https://doi.org/10.1136/jnnp-2018-319208
Tintore M, Vidal-Jordana A, Sastre-Garriga J (2019) Treatment of multiple sclerosis - success from bench to bedside. Nat Rev Neurol 15:53–58. https://doi.org/10.1038/s41582-018-0082-z
Uleri E, Regan P, Dolei A, Sariyer IK (2013) SF2/ASF binding region within JC virus NCCR limits early gene transcription in glial cells. Virol J 10:147. https://doi.org/10.1186/1743-422X-10-147
Uleri E, Ibba G, Piu C, Caocci M, Leoni S, Arru G, Serra C, Sechi G, Dolei A (2017) JC polyomavirus expression and bell-shaped regulation of its SF2/ASF suppressor during the follow-up of multiple sclerosis patients treated with natalizumab. J Neurovirol 23:226–238. https://doi.org/10.1007/s13365-016-0492-x
Zhao Y, Zhu T, Zhang X, Wang Q, Zhang J, Ji W, Ma Y (2015) Splicing factor 2/alternative splicing factor contributes to extracellular signal regulated kinase activation in hepatocellular carcinoma cells. Mol Med Rep 12:3890–3894. https://doi.org/10.3892/mmr.2015.3851
Acknowledgments
GI and CP share the first authorship. The Authors thank Dr. C. Scarpazza (MS Centre, Spedali Civili, Brescia) for helping in the collection of clinical data.
Funding
This study was financially supported in part by Fondazione Italia Sclerosi Multipla (AD, FISM2016_R_12; LI, FISM2016_R_16).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Brescia Ethical Committee Board (protocols 2713 of 05/24/2017 and NP0 of 07/18/2018).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Claudia Piu and Gabriele Ibba share the first authorship
Rights and permissions
About this article
Cite this article
Piu, C., Ibba, G., Bertoli, D. et al. Early reduction of the splicing factor2/alternative splicing factor: a cellular inhibitor of the JC polyomavirus in natalizumab-treated MS patients long before developing progressive multifocal leukoencephalopathy. J. Neurovirol. 26, 133–137 (2020). https://doi.org/10.1007/s13365-019-00793-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-019-00793-4