Abstract
Objectives
Given the increasing prevalence of osteoporosis and the important role dynamic balanced plays in the assessment of muscle function, we aimed to examine the joint and separate effects of osteoporosis and poor dynamic balance on the incidence of sarcopenia in Chinese elderly individuals.
Design
This study was conducted on 658 (44.4% male) Chinese suburban-dwelling participants with a mean age of 68.42 ± 5.43 years who initially had no sarcopenia and were aged >60 years. A quantitative ultrasound scan of each participant’s calcaneus with a T score less than −2.5 was used to identify the prevalence of osteoporosis. Sarcopenia was diagnosed according to the Asian Working Group for Sarcopenia criteria. We assessed dynamic balance using the Timed Up and Go Test (TUGT). Participants who scored in the top 20% on the TUGT were defined as having poor dynamic balance.
Results
After a follow-up of three years, the incidence of sarcopenia in the general population was 8.1% (9.6% in males, 6.8% in females). The incidence of sarcopenia was progressively greater in people suffering from both osteoporosis and poor dynamic balance (OR=2.416, 95%CI=1.124–5.195) compared to those who only had osteoporosis (OR=0.797, 95%CI=0.378–1.682) or poor dynamic balance (OR=1.226, 95%CI=0.447–3.363) in models without adjustments. Even after adjusting for potential confounders, the result still held true (OR=2.431, 95%CI=1.053–5.614).
Conclusions
In our study, we found individuals who suffered from both osteoporosis and poor dynamic balance simultaneously had a significantly higher incidence of sarcopenia than those who suffered from either one or the other.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At present, China faces serious challenges from an aging population (1, 2). The aging process promotes a decline in skeletal muscle mass and function and therefore contributes to sarcopenia, which is characterized by a degenerative loss of skeletal muscle mass and strength (3). Sarcopenia is associated with an increased risk of falls and fractures, an impaired ability to perform activities associated with daily living, physical disabilities, loss of independence, poor quality of life, and an increased risk of death (4, 5). Because of the debilitating symptoms and increased burden of healthcare costs on patients, finding the risk factors of sarcopenia and preventing it at an early stage are essential.
In the other side, aging is also associated with osteoporosis which affects more than one-third of people aged ≥ 50 years old in China (6, 7). Previous studies have investigated the associations between osteoporosis and sarcopenia. Many of these studies suggest that high lean mass and muscle strength are positively associated with bone mineral density, and linking sarcopenia to osteoporosis (8–12). While some studies found that the presence of osteoporosis is significantly associated with short-term sarcopenia, others have not observed this reciprocal relationship (8, 9).
On the other hand, the TUGT, as muscle function assessment tool used to identify sarcopenia, is included in the European Working Group on Sarcopenia in Older People (EWGSOP) (13), which is a dynamic balance assessment tool that is good at predicting recurrent falls (14). It can prevent and reduce fracture morbidity and mortality by assessing the risk of falls in patients with osteoporosis. However, the TUGT was not included in the definition of sarcopenia used by the Asian Working Group for Sarcopenia (AWGS) (15), which means that we may overlook the important role of dynamic balance in muscle function when we use the sarcopenia definition from the AWGS. Previous studies have suggested that, in addition to the existing indicators for identifying sarcopenia, the TUGT should also be an important indicator of sarcopenia which could strengthen its association with adverse outcomes, including poor prognosis, and prevent adverse events in the elderly (2, 16).
Because few longitudinal studies explore the impact of poor dynamic balance on the incidence of sarcopenia as defined by the AWGS, the relationship between the two is still unclear. Given the increasing prevalence of osteoporosis and the important role dynamic balanced plays in the assessment of muscle function, linking these two health risks is essential. Therefore, in the present study, we aimed to examine the joint and separate effects of osteoporosis and poor dynamic balance on the incidence of sarcopenia in elderly Chinese individuals.
Methods
Study participants
Our study population included residents from three areas (Hougu, East Chadian, and West Chadian) of Tianjin, China. A total of 976 older individuals (age ≥ 60) in these areas joined the national free physical examination program from 2013 to 2016; all 976 subjects were invited to participate in a comprehensive geriatric assessment. Participants with the following conditions were excluded from the study: (1) unable to communicate with interviewers or to grant informed consent; (2) unable to perform the handgrip strength test or the 4-meter walking test; (3)unable to stand for measurement of body composition, weight, and height; (4) who had a foot injury making the bone density test not feasible; and (5) who were taking a drug that may interfere with bone or calcium metabolism (e.g., estrogen, calcitionin, diphosphonate). 11 subjects were excluded, excluded persons included 2 people with underlying diseases that were likely to affect bone or calcium metabolism, and 9 people who failed to perform a physical examination. The final study population comprised 871 subjects with no sarcopenia after 94 sarcopenia subjects were excluded. The cohort was invited to attend repeat questionnaire interviews and physical measurements at 12, 24, and 36 months during the 3-year period following the baseline investigation. During the follow-up years, we excluded participants who died (n=3), bedridden (n=4) and those missing data (n=206). Our final sample included 658 participants. Our study was approved by the Ethics Committee of Tianjin medical university, and all subjects agreed to participate in the survey and gave informed written consent for data collection. The registration number of approval of the EC for this study is ChiCTR1800016308.
Covariates
We interviewed all participants in person using a questionnaire from our previous study (17). We collected data on the participants’ sociodemographics and behavioral characteristics, including age, sex, living conditions, history of falls and depression. Depressive symptoms were assessed using the Geriatric Depression Scale, participants with a score of ≥11 were considered to have depressive symptoms. We also reviewed whether participants had chronic medical conditions (e.g., osteoarthritis). Performance-based assessments, including the 4-m walking velocity test (WS) and the Timed Up and Go Test (TUGT), were also conducted. The prevalence of specific medical conditions about hypertension, hyperlipidemia, stroke, coronary heart disease (CHD), and kidney disease was established using standardized criteria that combined information from history of physical illness evaluated on the basis of participants’ response (yes or no) to questions, physician diagnosis, and taking corresponding medication or undergoing other treatment now or in the past.
Assessment of OS
The BMD was measured at calcaneus by the quantitative ultrasound (QUS; OsteoPro UBD2002A, BMTECH; World Wide Co. Ltd., Seoul, Korea), (18) utilizing T scores based on World Health Organization (WHO) criteria (19), which were obtained from the automated equipment. A T score less than −2.5 was considered to indicate OP.
Assessment of Sarcopenia
Sarcopenia was defined according to the AWGS criteria (15), in which a person who has low muscle mass, low muscle strength and/or low physical performance was identified as having sarcopenia. Low muscle mass was classified as relative skeletal muscle mass index (ASM/ht2) less than 7.0kg/m2 and 5.7kg/m2 in men and women, respectively; low muscle strength was defined as grip strength <26kg or <18kg for males and females, respectively; low physical performance was defined as walking speed <0.8m/s for both males and females. Details of measurement methods have been described in our previous cross-sectional study (20).
Poor dynamic balance definition
Poor dynamic balance was measured by TUGT (21). Participants were instructed to sit in a chair before receiving a start signal, after which they were to stand up, walk 3m, turn to walk back and sit down again. The time taken to complete the test was recorded twice for each participant to obtain an average, with a 10-seconds interval between consecutive measurements. Participants scoring in the top 20% on the TUGT were defined as poor dynamic balance.
Statistical Analysis
Baseline characteristics of the study population are according to osteoporosis (yes or no) and poor dynamic balance (yes or no) groups as mean and median values and standard deviations for continuous variables and proportions for categorical variables. All continuous variables were presented as mean and standard deviation; classification variables were reported as percentages. Differences in the characteristics according to different incidence of osteoporosis and balance status were analyzed using analysis of variance, Kruskal-Wallis rank tests and χ2 tests. Logistic regression analysis was used to analyze the association between incidence of osteoporosis or balance status with sarcopenia, Model 1 was adjusted for gender, age and BMI. Model 2 was adjusted for gender, age, BMI, educational level, smoking and drinking habits, IPAQ (international physical activity questionnaire), CVD (Cardiovascular Diseases), osteoarthritis, marital status, history of falls, and depression. All statistical analyses were performed using SPSS version 19.0, and P-values less than 0.05 were considered statistically significant.
Results
Baseline characteristics
The final study included 658 participants (44.4% male) with a mean age of 68.42 ± 5.43 years, baseline characteristics according to the presence of osteoporosis and poor dynamic balance of baseline clinical characteristics are shown in Table 1. Overall, 29.8% subjects only suffering osteoporosis (OPA), 10.6% subjects only have poor dynamic balance (PBA), 16.6% subjects have both osteoporosis and dynamic poor dynamic balance (OP+PB) at baseline.
Clinical Characteristics of the Study Population at 3-year follow-up
After three years of follow-up, the incidence of sarcopenia in the general population is 8.1% (9.6% in male, 6,8% in female). The OP+PB group have the highest incidence of sarcopenia (15.6%, P=0.013). The OPA group have more female proportions (55.2/ 44.8vs38.2/61.8, p=0.002), lower BMI (26.28±3.28vs25.00±3.30, P<0.001), grip strength (29.21±8.70vs26.29±8.55, P<0.001), ASM (20.54±4.39vs18.23±4.01, P<0.001), walking speed (1.10±0.16vs1.01±0.16, P<0.001) and more falling history (12%vs22.6, P=0.023) than normal people. The PBA group have higher age (67.41±4.76vs69.30±5.62, P<0.001), lower grip strength (29.21±8.70vs26.17±7.76, P<0.001) than normal people, more diabetes (P<0.001) than all other groups. The OP +PB group have more female proportions (55.2/44.8vs40.4/59.6, P=0.002), higher age (67.41±4.76vs70.85±6.45, P<0.001), lower BMI (26.28±3.28vs25.22±3.39, P<0.001), grip strength (29.21±8.70vs23.68±8.50, P<0.001) than normal people, higher age (67.94±5.07vs70.85±6.45, P<0.001), lower grip strength (26.29±8.55vs23.68±8.50, P<0.001) than OPA group, all data is shown in Table 1.
Risk of the incidence of sarcopenia
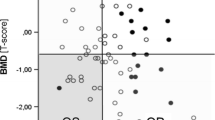
Compared with other groups, the OP+PB group had an increased incidence of new sarcopenia, and associations between osteoporosis and poor dynamic balance on the risk of developing sarcopenia are explored in Table 2. The incidence of sarcopenia was progressively greater in OP+PB group (OR=2.416, 95%CI=1.124–5.195) than OPA group (OR=0.797, 95%CI=0.378–1.682) or PBA group (OR=1.226, 95%CI=0.447–3.363) in models without adjustment, after adjusting for potential confounders the result still be true (OR=2.431, 95%CI=1.053–5.614). Figure 1 shows the incidence of sarcopenia according to different age group (60–69years:5.47%, 70–79 years:15.44%, ≥80 years:20%).
Discussion
In this study, we estimated the joint and separate effects of osteoporosis and poor dynamic balance on incidence of sarcopenia in a suburban-dwelling population of elderly persons aged 60 years and older in China. Those subjects who suffer from both osteoporosis and poor dynamic balance at baseline had the highest incidence of sarcopenia (15.6%, P=0.013) after a three-years follow-up. Osteoporosis or poor dynamic balance alone had no significant effect on the incidence of sarcopenia while people with both these two conditions had a significantly higher incidence of sarcopenia. After adjusting for potential confounders, osteoporosis and poor dynamic balance can predict the incidence of sarcopenia in Chinese community suburban-dwelling elderly individuals (OR=2.416, 95%CI=1.124–5.195).
The new incidence of sarcopenia
In our study, the incidence of sarcopenia in the general population is 8.1% (9.6% in males, 6.8% in females), which is similar to some previous studies which used a population whose average age was similar to ours and used the same definition of sarcopenia we did.(9, 20). However, when using a definition consistent with the EWGSOP, a systematic review showed that the prevalence of sarcopenia was 1–33% (and up to 68% in males) (22). These large differences in the prevalence of sarcopenia may be due to variable susceptibilities related to age, gender, and ethnicity. In a previous study of a Taiwanese population (23), the prevalence of sarcopenia (12.7% in males, 13.3% in females) was higher than our study. While the Taiwanese population is similar ethnically to the Chinese population, they were older in average age. These results were consistent with our research that showed older groups have higher morbidity (shown in figure 1). However, a Spanish study using a population with an average age similar to ours (69.21 ± 7.56 years) showed a higher incidence of sarcopenia (27.23% in female). This high variability to some extent can be attributed to differences in characteristics, gender, and living conditions of the study sample (24).
The influence of osteoporosis for sarcopenia
The definition of sarcopenia used in our study includes muscle mass, muscle strength, and walking speed. With aging, the decrease of muscle mass and muscle strength can result from multiple causes, including neuronal loss, decreased testosterone, IGF-I, insulin growth factor, and an increased level of inflammatory cytokines (25). Therefore, the incidence of sarcopenia can rise sharply with aging. On the other hand, with aging, the decline of human estrogen content is also a risk factor for the onset of sarcopenia (8), which also is an important risk factor for osteoporosis (26). The loss of muscle strength and mass during the aging process causes structural changes in the microarchitecture of the bones and decreases mineral density, resulting in the decline of bone quality and an increased rate of fractures (25). Our study shows that people with osteoporosis alone do not have a higher risk for sarcopenia after a three follow-up (OR=0.797, 95%CI=0.378–1.682). Some previous studies similar to ours, after adjusting for confounding factors, could not find a significant association between sarcopenia and osteoporosis (27, 28). A previous study showed that among the three assessment components of sarcopenia, the strongest link to osteoporosis was grip strength (8). However, in our study, the patients suffering only from osteoporosis group had a higher grip strength (26.29±8.55vs23.68±8.50, P<0.001) than those suffering from both osteoporosis and poor dynamic. Although their grip strength was lower than in the normal group, there was no difference in the change of grip strength between the osteoporosis-only group and the normal group during the three years of follow-up (1.50vs2.38, P=0.335), which means that despite the fact that high lean mass and muscle strength were positively associated with bone mineral density, osteoporosis alone is not sufficient to affect the incidence of sarcopenia in our subjects. However, some studies suggest that high lean mass and muscle strength are positively associated with BMD, and sarcopenia is associated with low BMD and osteoporosis (8–12). In summary, a larger sample size and more years of follow-up will clarify this issue.
The influence of poor dynamic balance for sarcopenia
Previous studies have shown that sarcopenia is more common in patients with disabilities, weakness, and those who have a higher risk of falling (29). There is already evidence that the TUGT can reliably predict the risk of falling (14). TUGT is likely related to the sequencing of several important dynamic stability skills, such as turning and sit-to-stand transitions as well as straight-ahead gait, which could be used to measure both gait speed and dynamic balance (30). So in order to better show the difference in the impact of walking speed and dynamic balance on the incidence of sarcopenia, we replaced the TUGT with the 4-m walking test which is used to indicate walking speed in our study. We analyzed the effects of poor walking speed alone and combined poor walking speed and osteoporosis at baseline on the incidence of sarcopenia, the slowest 20% for the 4-m walking test was defined as having poor walking speed (shown in the table below). We found that the baseline poor walking speed did not have a significant impact on the new incidence of sarcopenia (Poor walking speed only group VS normal group: OR=1.936, 95%CI=0.594–6.313; Osteoporosis with poor walking speed group VS normal group: OR=1.980, 95%CI=0.747–5.247). Dynamic stability during gait-related activities is essential for autonomy and was suitable for assessed by TUGT in our study (31), and the impact of dynamic stability on the incidence of sarcopenia is undoubtedly more obvious. However, the difference and priority of dynamic balance and walking speed assessed by TUGT is still needs more research to clarify. On the other hand, we found that suffering only from poor dynamic balance had no significant effect on the risk for sarcopenia after three years (OR=1.226, 95%CI=0.447–3.363). Similar to our study, another study found that patients with poor TUGT results do not have the same physical performance as those with sarcopenia (32). The possible reason is that the fast twist skeletal muscle capacity which dynamic balance requires is not included in the identification criteria for sarcopenia. However, some previous studies have shown that people with poor dynamic balance have both lower muscle mass and muscle strength, which increase the incidence of sarcopenia (10, 33).
However, this trend has not been shown in our population. Many studies suggested that due to multiple items included in the TUGT, a poor TUGT score represents worse muscle strength and muscle mass (14, 16). A decrease in muscle mass and muscle strength would reduce cortical bone strength and bone density (11, 34). Subjects with poor muscle strength and muscle mass may have osteoporosis at the same time due to bone-to-muscle interactions (27), since subjects with worse muscle function were in the combined group, and the poor balance group did not show a significant increase in morbidity. On the other hand, some studies suggested that poor TUGT scores may result from a great variety of underlying conditions, which is consistent with study (15). People with poor TUGT scores were older (67.41±4.76vs69.30±5.62, P<0.001), had lower grip strength (29.21±8.70vs26.17±7.76, P<0.001) than normal people, and were more likely to have diabetes (P<0.001) than all other groups. Previous studies have demonstrated that a loss of lean tissues and deterioration in muscle function have been described as one of the many complications of type 2 diabetes mellitus, (35) which is consistent with a previous study that suggested that a TUGT score is determined by multiple body functions (15).
Combined effect of osteoporosis and poor dynamic balance on sarcopenia
Sarcopenia is one of the most important contributing factors to frailty, disability, and mortality in older people (4, 5), and finding the risk factors of sarcopenia and preventing it at an early stage are essential. In our study, we found that osteoporosis and poor dynamic balance can predict the incidence of sarcopenia in Chinese community-dwelling elderly individuals (OR=2.416, 95%CI=1.124–5.195), and even after adjusting for potential confounders, the result still holds (OR=2.431, 95%CI=1.053–5.614). Many previous studies have demonstrated results consistent with our study that patients who suffer from osteoporosis and poor muscle capacity measured by TUGT are more susceptible to have sarcopenia (8–12, 33). We found that individuals who suffer from both osteoporosis and poor dynamic balance are typically older (67.41±4.76vs70.85±6.45, P<0.001), and have a lower BMI (26.28±3.28vs25.22±3.39, P<0.001), and grip strength (29.21±8.70vs23.68±8.50, P<0.001) than normal people in our data. Previous studies have shown that a higher age and a lower BMI are both important risk factors for sarcopenia which is consist with our study (36). On the other hand, with the increase of age, the loss of hormones such as testosterone and growth hormone is an important cause of sarcopenia (2), testosterone deprivation selectively decreases lower-limb muscle function, predominantly affecting muscles that support body weight, accelerate the body forwards during walking, and mediate balance (37). Although the poor dynamic balance group did not show significant effects on the morbidity of sarcopenia, after superimposing the performance of body bone mass on the basis of the dynamic balance assessment, the influence on the incidence of sarcopenia became very obvious, which represents a significantly higher incidence of sarcopenia in patients both with osteoporosis and poor dynamic balance.
Strengths and limitations
This study has a number of strengths. It was the first to examine a uniquely-defined group of suburban older men and women living in a discrete geographical area. Our participants were recruited from a suburban area and were leading a more physically active lifestyle than subjects in other geographical areas. Despite extensive efforts to curb the limits of our study, some limitations did exist. First, all participants in the present study were relatively healthy. We did not include participants who could not undergo a free annual national physical examination (e.g., those bedridden or with serious disease). Therefore, our results may actually underestimate the prevalence of osteoporosis or sarcopenia and its associated health impacts. Despite this limitation, statistical differences were still observed, implying that statistical power should not be a serious problem. Even so, we will increase future sample sizes and years of follow-up to increase power to evaluate risk factors in future research.
Conclusions
In our study, we found that individuals who suffer from osteoporosis or poor dynamic balance alone did not have an increased risk for sarcopenia, while patients who suffered from both had a significantly higher incidence of sarcopenia. This suggests that measures should be taken in subjects with both poor bone status and dynamic balance to prevent the onset of sarcopenia, thereby reducing the occurrence of frailty, disability, and mortality.
References
China. State Statistical B. Communique of the major statistics from the first national population census as released by the State Statistical Bureau of the People’s Republic of China (November 1, 1954). Chin Sociol Anthropol. 1984; 16:62–5.
Lauretani F, Bautmans I, De Vita F, Nardelli A, Ceda GP, Maggio M. Identification and treatment of older persons with sarcopenia. Aging Male. 2014; 17:199–204.
Evans WJ, Campbell WW. Sarcopenia and age-related changes in body composition and functional capacity. J Nutr. 1993; 123:465–8.
Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, et al. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007; 55:1216–23.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006; 61:1059–64.
Riis BJ, Hansen MA, Jensen AM, Overgaard K, Christiansen C. Low bone mass and fast rate of bone loss at menopause: equal risk factors for future fracture: a 15-year follow-up study. Bone. 1996; 19:9–12.
Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016; 16:1039.
Sjoblom S, Suuronen J, Rikkonen T, Honkanen R, Kroger H, Sirola J. Relationship between postmenopausal osteoporosis and the components of clinical sarcopenia. Maturitas. 2013; 75:175–80.
Yoshimura N, Muraki S, Oka H, Iidaka T, Kodama R, Kawaguchi H, et al. Is osteoporosis a predictor for future sarcopenia or vice versa? Four-year observations between the second and third ROAD study surveys. Osteoporos Int. 2017; 28:189–99.
da Silva AP, Matos A, Ribeiro R, Gil A, Valente A, Bicho M, et al. Sarcopenia and osteoporosis in Portuguese centenarians. Eur J Clin Nutr. 2017; 71:56–63.
He H, Liu Y, Tian Q, Papasian CJ, Hu T, Deng HW. Relationship of sarcopenia and body composition with osteoporosis. Osteoporos Int. 2016; 27:473–82.
Tarantino U, Baldi J, Scimeca M, Piccirilli E, Piccioli A, Bonanno E, et al. The role of sarcopenia with and without fracture. Injury. 2016; 47 Suppl 4:S3–S10.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–23.
Kang L, Han P, Wang J, Ma Y, Jia L, Fu L, et al. Timed Up and Go Test can predict recurrent falls: a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017; 12:2009–16.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014; 15:95–101.
Sim M, Prince RL, Scott D, Daly RM, Duque G, Inderjeeth CA, et al. Sarcopenia Definitions and Their Associations With Mortality in Older Australian Women. J Am Med Dir Assoc. 2019; 20:76–82 e2.
Zhang W, Shen S, Wang W, Zhou C, Xu L, Qiu J, et al. Poor lower extremity function was associated with pre-diabetes and diabetes in older chinese people. PLoS One. 2014; 9:e115883.
Ma Y, Fu L, Jia L, Han P, Kang L, Yu H, et al. Muscle strength rather than muscle mass is associated with osteoporosis in older Chinese adults. J Formos Med Assoc. 2018; 117:101–8.
Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. 1994; 4:368–81.
Han P, Kang L, Guo Q, Wang J, Zhang W, Shen S, et al. Prevalence and Factors Associated With Sarcopenia in Suburb-dwelling Older Chinese Using the Asian Working Group for Sarcopenia Definition. J Gerontol A Biol Sci Med Sci. 2016; 71:529–35.
Hwang HY, Choi JS, Kim HE. Masticatory efficiency contributing to the improved dynamic postural balance: A cross-sectional study. Gerodontology. 2018.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zuniga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014; 43:748–59.
Lin CC, Lin WY, Meng NH, Li CI, Liu CS, Lin CH, et al. Sarcopenia prevalence and associated factors in an elderly Taiwanese metropolitan population. J Am Geriatr Soc. 2013; 61:459–62.
Aibar-Almazan A, Martinez-Amat A, Cruz-Diaz D, Jimenez-Garcia JD, Achalandabaso A, Sanchez-Montesinos I, et al. Sarcopenia and sarcopenic obesity in Spanish community-dwelling middle-aged and older women: Association with balance confidence, fear of falling and fall risk. Maturitas. 2018; 107:26–32.
Frisoli A, Jr., Chaves PH, Ingham SJ, Fried LP. Severe osteopenia and osteoporosis, sarcopenia, and frailty status in community-dwelling older women: results from the Women’s Health and Aging Study (WHAS) II. Bone. 2011; 48:952–7.
Doherty TJ. Invited review: Aging and sarcopenia. J Appl Physiol (1985). 2003; 95:1717–27.
Walsh MC, Hunter GR, Livingstone MB. Sarcopenia in premenopausal and postmenopausal women with osteopenia, osteoporosis and normal bone mineral density. Osteoporos Int. 2006; 17:61–7.
Gillette-Guyonnet S, Nourhashemi F, Lauque S, Grandjean H, Vellas B. Body composition and osteoporosis in elderly women. Gerontology. 2000; 46:189–93.
Demontiero O, Boersma D, Suriyaarachchi P, Duque G. Clinical Outcomes of Impaired Muscle and Bone Interactions. Clinical Reviews in Bone and Mineral Metabolism. 2014; 12:86–92.
Salarian A, Zampieri C, Horak FB, Carlson-Kuhta P, Nutt JG, Aminian K. Analyzing 180 degrees turns using an inertial system reveals early signs of progression of Parkinson’s disease. Conf Proc IEEE Eng Med Biol Soc. 2009; 2009:224–7.
Bonnyaud C, Pradon D, Bensmail D, Roche N. Dynamic Stability and Risk of Tripping during the Timed Up and Go Test in Hemiparetic and Healthy Subjects. PLoS One. 2015; 10:e0140317.
Sim M, Prince RL, Scott D, Daly RM, Duque G, Inderjeeth CA, et al. Utility of four sarcopenia criteria for the prediction of falls-related hospitalization in older Australian women. Osteoporos Int. 2019; 30:167–76.
Waters DL, Qualls CR, Cesari M, Rolland Y, Vlietstra L, Vellas B. Relationship of Incident Falls with Balance Deficits and Body Composition in Male and Female Community-Dwelling Elders. J Nutr Health Aging. 2019; 23:9–13.
Szulc P, Beck TJ, Marchand F, Delmas PD. Low skeletal muscle mass is associated with poor structural parameters of bone and impaired balance in elderly men—the MINOS study. J Bone Miner Res. 2005; 20:721–9.
Guerrero N, Bunout D, Hirsch S, Barrera G, Leiva L, Henriquez S, et al. Premature loss of muscle mass and function in type 2 diabetes. Diabetes Res Clin Pract. 2016; 117:32–8.
Han P, Zhao J, Guo Q, Wang J, Zhang W, Shen S, et al. Incidence, Risk Factors, and the Protective Effect of High Body Mass Index against Sarcopenia in Suburb-Dwelling Elderly Chinese Populations. J Nutr Health Aging. 2016; 20:1056–60.
Cheung AS, Gray H, Schache AG, Hoermann R, Lim Joon D, Zajac JD, et al. Androgen deprivation causes selective deficits in the biomechanical leg muscle function of men during walking: a prospective case-control study. J Cachexia Sarcopenia Muscle. 2017; 8:102–12.
Acknowledgements
The authors thank Guiyan Shao from the Chadian public health center and Xiaofang Ren from Hangu welfare house for providing place and organization.
Funding
Funding: This work was supported by grant from National Natural Science Foundation of China (81601952) and Tianjin Municipal Science and Technology Commission (16ZXMJSY00070, Tianjin, China), and Health and Family Planning Commission of Binhai New Area (2017BWKZ005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate: This research was approved by the Ethics Committee at Tianjin Medical University. The methodological sessions were carried out in accordance with the approved guidelines and regulations. The participants were fully informed of the nature of research and signed an informed consent to participate.
Competing interests: The authors declare that they have no competing interests in this section.
Rights and permissions
About this article
Cite this article
Yu, X., Hou, L., Guo, J. et al. Combined Effect of Osteoporosis and Poor Dynamic Balance on the Incidence of Sarcopenia in Elderly Chinese Community Suburban-Dwelling Individuals. J Nutr Health Aging 24, 71–77 (2020). https://doi.org/10.1007/s12603-019-1295-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1295-6