Abstract
Introduction
Osteoporosis and sarcopenia are significant health problems that mainly affect older adults. This study aimed to investigate the relationship between sarcopenia and osteoporosis.
Materials and methods
The study included 444 participants who had undergone a dual-energy X-ray absorptiometry scan, handgrip test, 4-m walking speed test, and bioimpedance analysis within the past year. Participants were classified into control, osteopenia, or osteoporosis groups according to the World Health Organization classification. Sarcopenia was diagnosed according to the European Working Group on Sarcopenia in Older People-2 criteria.
Results
The mean age of the participants was 75.88 ± 7.20 years, and 80.9% were females. There were 144, 230, and 70 participants in the osteoporosis, osteopenia, and control groups, respectively. Probable sarcopenia was identified in 94 subjects, sarcopenia in 61, and severe sarcopenia in 72 participants. After adjusting for age, gender, and body mass index, probable sarcopenia and severe sarcopenia were associated with osteoporosis (p < 0.05). Low muscle strength, and low physical performance were associated with osteoporosis (p < 0.02). When osteoporosis was evaluated only according to the femoral neck T score, low muscle strength and low physical performance were found to be related not only to osteoporosis (p < 0.001), but also to osteopenia (p < 0.05). Additionally, probable sarcopenia was associated with femoral neck osteopenia (p < 0.01).
Conclusions
In this study, probable sarcopenia and severe sarcopenia were associated with osteoporosis in older adults. Furthermore, we found that low muscle strength, or dynapenia, which is the determining criterion of sarcopenia, was related to femoral neck osteopenia and osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductıon
As the world’s population ages, research into age-related pathological and physiological changes in the body has become more critical [1]. Decreased bone density and bone microarchitecture deterioration, which occur with advancing age, can lead to osteoporosis, a progressive metabolic bone disease associated with increased bone fragility [2]. Osteoporosis is related to many negative health outcomes, one of which is fractures, which can occur in patients with osteoporosis even in the absence of trauma. Of all the osteoporotic fractures, hip fractures are associated with the highest economic burden and mortality rates [3, 4]. The mortality rate of older adults with femoral fractures has been reported to be 15–20% in 1 year, and 50% of people lose their independence [4, 5].
On the other hand, sarcopenia, a geriatric syndrome, causes falls, fractures, physical disability, and mortality through generalized skeletal muscle disorder, which involves a decrease in muscle mass and/or muscle strength [6]. Moreover, a close relationship between bone and muscle tissue, both chemically and metabolically is reported. While skeletal muscle is kept in balance by protein synthesis and degradation, bone formation is regulated by reabsorption [7]. Both tissues show an adaptive response to mechanical loading and interact mechanically, known as the “mechanostat hypothesis” [8]. Nevertheless, in recent years, many studies have shown that this mechanic stimulus is not the only form of interaction between the tissues. Substances called myokines and osteokines are released from muscle and bone tissues, allowing them to communicate with each other [9].
Apart from these substances, many common genetic polymorphisms such as glycine-N‐acyltransferase like 1 (GLYATL1), myostatin (MSTN), and α-actinin-3 (ACTN3), have been found to lead to bone and muscle tissue loss [8]. In both sarcopenic and osteopenic individuals, serum concentrations of inflammatory cytokines, predominantly IL-6 and TNF-alpha, have been found to be high [8]. In addition, several risk factors including diabetes, malnutrition, obesity, abnormal thyroid function, low vitamin D levels, and levels of sex steroids, growth hormone, IGF-1, and corticosteroids have been reported to play a role in the development of both osteoporosis and sarcopenia [8].
Osteoporosis and sarcopenia are two critical problems that need to be evaluated due to their common risk factors and etiologic pathways, adverse health consequences, and health care and cost burden. Thus, osteosarcopenia was recently defined to draw attention to the importance of combined assessment of osteoporosis and sarcopenia [10], which comes to mind the question of whether the osteosarcopenia definition is enough to determine the complex interrelationships between the two conditions in older adults. For this reason, we aimed to investigate the possible relationship between sarcopenia, criteria of sarcopenia and dual-energy X-ray absorptiometry (DEXA) measurement sites in terms of osteoporosis. Moreover, this is one of the first studies to compare sarcopenia, which determined according to the European Working Group on Sarcopenia in Older People-2 (EWGSOP-2) criteria, osteopenia, and osteoporosis in different body parts.
Materials and methods
Participants
The records of 1127 participants over 65 years of age who visited the geriatric outpatient clinic with any reason between July 2016 and July 2017 were retrospectively reviewed.Handgrip strength test, 4-m gait speed test, bioimpedance analysis performed and had laboratory findings on the same day. In the end, 684 patients who had DEXA within 3 months before and after from AGD were included in this study. Of these, 198 people were excluded from the study because they met the exclusion criteria, and 42 refused to participate after being informed about the study. In the end, a total of 444 people were enrolled in the study (Fig. 1).
The investigation conformed to the Declaration of Helsinki and was approved by the ethics committee of Dokuz Eylul University, Turkey. Each participant or a legal guardian provided informed consent before participating in the study.
Exclusion criteria
Participants were excluded if they met the following criteria: under 65 years of age; refused to participate; pacemaker (because of contraindication to electrical bioimpedance); diagnosed with cancer (due to the effect of cancer-associated cachexia on muscle mass); diagnosis of dementia according to the Clinical Dementia Rating scale (CDR)-2 (because the reliability of handgrip strength is low for older participants with dementia due to difficulty in judgment and conception, which can cause them to fail to comprehend and complete tasks thoroughly); any disease that may affect bone metabolism (e.g., hyperparathyroidism, osteomalacia, Paget’s disease, hyperthyroidism); or a history of severe illness that may impair general health status (e.g., an acute cerebrovascular event, gastrointestinal bleeding, sepsis, acute renal failure, acute coronary syndrome, acute liver failure, acute respiratory failure).
Participant characteristics
We assessed characteristics of the subjects from medical records in this retrospective study. Age, gender, education level, concomitant systemic diseases, and the number of medications were recorded in clinical application. Participants were asked if they had experienced a fall or balance disorder in the last year in their application. The participants’ history of hypertension, diabetes mellitus, congestive heart failure, thyroid disease, dementia, and depression were individually investigated. Participants’ comorbid conditions were evaluated using the Charlson’s Comorbidity Index (CCI).
Comprehensive geriatric assessment
All patients underwent comprehensive geriatric evaluation including the Mini-Mental State Examination (MMSE) and the Clinical Dementia Rating (CDR) scale for neurocognitive assessment, the Lawton–Brody Instrumental Daily Living Activity Scale (IADL) and the Barthel Index for Activities of Daily Living (BADL) for the evaluation of daily living activities, the Timed Up and Go (TUG) test and the Tinetti Performance-Oriented Mobility Assessment (POMA) for the assessment of balance and gait, and the Mini Nutritional Assessment (MNA) for nutritional evaluation [11].
Laboratory findings
Laboratory tests, including thyroid-stimulating hormone (TSH), vitamin B12, and folic acid, were performed using a Diagnostic Modular Systems Autoanalyzer (E170 and P-800; Roche, Switzerland). Serum 25-OH vitamin D level was measured using the Cobas e601 autoanalyzer (Mannheim, Germany) via the radioimmunoassay method.
Diagnosis of sarcopenia
Bioimpedance analysis was established using a TANITA scale (MC-780U Multi Frequency Segmental Body Composition; Tokyo, Japan). Body mass index (BMI), fat-free mass, fat, bone, and muscle mass, and basal metabolic rate were obtained via bioimpedance analysis. Using data obtained through the bioimpedance analysis, the calculation was made according to the following formula: skeletal muscle (kg) = [(height2/R) × 0.401] + (gender × 3.825) + (age × (− 0.071)) + 5.102 [12]. The units for height, age, female gender, male gender, and resistance (R) in the formula were centimeters (cm), years, 0, 1, and 50 Hz, respectively. Skeletal muscle mass index (SMI; muscle mass/height2) was calculated by dividing the muscle mass by the square of the height in meters. Values of < 8.87 kg/m2 for males and 6.42 kg/m2 for females were regarded as low muscle mass [6].
A JAMAR brand hand dynamometer was used to evaluate muscle strength. Participants were seated and positioned with their elbows in 90° of flexion and wrists in 0–30° of dorsiflexion. They were asked to grip the dynamometer using maximum strength for about 5 s. The result was measured in kilograms. The participant was asked to repeat the procedure three times, and the average of these three measurements was recorded. Grip strength values of less than 16 kg in women and 27 kg in men were considered low muscle strength, also known as dynapenia [6, 13] A 4-m walking speed test was used to evaluate gait speed, which was measured in meters/second. A walking speed of ≤ 0.8 m/s was considered slow gait speed and defined as low physical performance. Robust, probable sarcopenia, sarcopenia, and severe sarcopenia groups were identified according to EWGSOP-2 criteria [6].
Diagnosis of osteoporosis
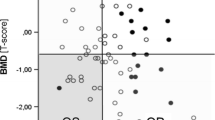
For the diagnosis of osteoporosis, the lumbar spine and femoral neck were submitted to DEXA and bone mineral density (BMD) scans, and T scores for these areas were calculated. The scans included lumbar spine and femoral neck sites. The scan procedure for each site was performed separately according to the manufacturer’s recommendations. According to the results obtained from DEXA, participants with T scores ranging from − 1.0 to − 2.5 in the femoral neck and lumbar spine were diagnosed with osteopenia, whereas, those with a BMD value of − 2.5 or below were diagnosed with osteoporosis [14].When participants were evaluated based on femoral neck T scores only, they were described as femoral neck osteopenia and osteoporosis. Similarly, when participants were evaluated based on lumbar spine T scores only, they were described as lumbar spine osteopenia and lumbar spine osteoporosis [14].
Statistical analyses
Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) version 22.0 for Windows (SPSS Inc, Chicago, IL) and Power Analysis and Sample Size (PASS) 2008 statistical software (Utah, USA). Nominal variables were assessed by Pearson’s chi-square test. Continuous variables with a normal distribution were analyzed by one-way ANOVA followed by a post hoc test, and the Kruskal–Wallis test was used to assess the presence of a non-normal distribution (Table 1). Adjustment according to age, gender, and BMI was carried out by multinomial logistic regression analysis (Table 2). Multinominal logistic regression analysis was used to assess the relationship between groups and calculated odds ratios in Tables 3 and 4. The sample size required for the study was calculated to be at least 256 participants for a 95% confidence interval and a 5% margin of error. Results with a p value of < 0.05 were considered statistically significant.
Results
A total of 444 participants (359 females, 85 males) were included in the study. The mean age was 75.88 ± 7.20 years. Of the participants, 230 (51.8%) were diagnosed with osteopenia and 144 (32.4%) were diagnosed with osteoporosis; whereas, 70 (15.8%) were not diagnosed with either osteopenia or osteoporosis. Of the patients, 217 (48.9%), 94 (21.1%), 61 (13.7%), and 72 (16.2%) were classified in the robust, probable sarcopenia, sarcopenia, and severe sarcopenia groups, respectively. Low muscle strength, low muscle mass, and low physical performance were observed in 227 (51.1%), 228 (51.3%), and 146 (32.9%) participants, respectively. Considering the sociodemographic characteristics of the participants, the incidence of osteopenia and osteoporosis was significantly higher in females than males (p < 0.001). The highest education level was observed in the healthy group (8.01 ± 4.31 years); whereas, the lowest educational level was found in participants with osteoporosis (5.85 ± 4.71 years), followed by those with osteopenia (7.23 ± 4.51 years; p < 0.001). Table 1 summarizes the demographic characteristics, comorbidities, and laboratory findings of the individuals participating in the study.
No difference was observed between the osteoporosis, osteopenia, and control groups in terms of the prevalence of hypertension, diabetes, heart failure, and dementia (p > 0.05). Furthermore, no difference was observed between the groups in terms of CCI scores used in the comorbidity assessment (p = 0.809).
A significant difference in mean BMI was observed between the groups (p < 0.001). The mean BMI of the osteoporosis group (27.60 ± 5.29 kg/m2) was found to be lower than both the osteopenia group (29.42 ± 5.57 kg/m2) and the control group (30.94 ± 5.43 kg/m2; p < 0.001). Comparison of the osteopenia, osteoporosis, and control groups showed a relationship with vitamin D levels, but no associations with the other parameters obtained at the time of diagnosis (vitamin B12, folate, and TSH values) were observed (p < 0.05). The difference in IADL between the control and osteoporosis groups was significant (p = 0.003) after adjusting for age, sex, and BMI, but no significant differences were observed in BADL, MNA, or POMA (p > 0.05; Table 2).
When we evaluated the relationship between sarcopenia and osteoporosis, we found that probable sarcopenia and severe sarcopenia increased the risk of osteoporosis by 3.17 (p = 0.018) and 3.81 (p = 0.049) times, respectively. Probable sarcopenia increased the risk of femoral neck osteopenia by 2.75 times (p = 0.008) and the risk of femoral neck osteoporosis by 3.19 times (p = 0.014). The most definite relationship was found between severe sarcopenia and femoral neck osteoporosis (OR = 7.63, p = 0.003). No relationship was found between the other groups (p > 0.05; Table 3).
The assessment of sub-parameters (low muscle strength, low muscle mass, low physical performance) in patients with sarcopenia and osteoporosis showed that low muscle strength and low physical performance were associated with osteoporosis when the confounding effects of age, gender, and BMI were eliminated (p < 0.05 for each comparison). Low muscle strength was associated with both femoral neck osteopenia (OR = 2.00 p = 0.017) and femoral neck osteoporosis (OR = 3.56, p < 0.001). Likewise, a low physical performance increased the risk of femoral neck osteopenia and femoral neck osteoporosis by 2.21 (p < 0.05) and 4.49 (p < 0.001) times, respectively (Table 4).
Discussion
This retrospective cross-sectional study showed that probable sarcopenia and severe sarcopenia were associated with osteoporosis in older adults. Probable sarcopenia was also associated with femoral neck osteopenia. Furthermore, low muscle strength, or dynapenia, and low physical performance were closely related to osteoporosis and femoral neck osteopenia.
The prevalence of osteoporosis was in higher in females, especially during the postmenopausal period due to a deficiency in estrogen. The prevalence of osteoporosis increases with aging. In a recent study, the prevalence of osteoporosis was 8% in adults aged 60–69, compared with 16.4% in older adults aged 70–79 years and 26.2% in older adults aged 80 years and more, respectively [15]. In the FRAX-TURK study, it was found that the prevalence of OP in men and women aged 50 years and over was 22.2 and 27.2%, respectively [16]. Of the participants 32.4% were diagnosed with osteoporosis as consistent with similar age groups in the literature.Low BMI is another critical risk factor for osteoporosis [17]. Accordingly, age, female gender, and BMI were found to be related to osteopenia and osteoporosis in our study. On the other hand, even though optimal vitamin D levels are essential to prevent osteoporosis, vitamin D levels were higher in the osteopenia and osteoporosis groups than in the control group in the current study. This may be related to the periodic screening and treatment of vitamin D levels in our clinical practice, or possibly due to a blunted vitamin D receptor response, even if vitamin D is enhanced to a sufficient level [18].
Sarcopenia is a condition characterized by a progressive loss of muscle quantity and quality. In advanced age, with reasons such as the increased risk of malnutrition, immobility, hormonal deficiencies, increased cytokine levels, the frequency of sarcopenia increases[6, 19]. By the reason of racial and ethnic differences the prevalence of sarcopenia ranges between 5–13% in 60–70 years and 11–50% over the 80 years age in the literature [20, 21]. Our sarcopenia prevalence was compatible with previous studies from Turkey. Bulut et al. was determined the prevalence of sarcopenia as 24.8% in Turkey. Since we evaluated sarcopenia with EWGSOP-2 which has lower cut-off values especially for muscle strength, in accordance with our previous studies our sarcopenia prevalence was 29.9% in this study. [22]. Moreover, Yazar et al. was identified sarcopenia prevalence in the life decades 60–69, 70–79 and 80 years and older age groups as 15.4, 21.2 and 36.5%, respectively, with EWGSOP[23].
Until now, many studies have reported that bone and muscle tissues interact in many different ways, prompting researchers to wonder if there is a relationship between sarcopenia and osteoporosis [8]. Although osteosarcopenia is predetermined, some inconsistencies in the relationship between sarcopenia and osteoporosis were observed in the current study. In one study, Reiss et al. showed an association between sarcopenia and osteoporosis, especially in women [24]; whereas in another one, Lima et al. found no relationship between severe sarcopenia and osteoporosis [25]. Therefore, to the best of our knowledge, this is the first study to compare sarcopenia (determined according to the EWGSOP-2 criteria), osteopenia, and osteoporosis in different body parts.
In this study, we found that the risk of osteoporosis was increased 3.17 times in the probable sarcopenia group and 3.81 times in the severe sarcopenia group. When we evaluated the sarcopenia criteria individually, the risk of osteoporosis was increased 3.14 times in participants with low muscle strength and 2.71 times in participants with low physical performance. Nevertheless, muscle mass was not associated with osteoporosis. These results suggest that the main issue between bone and muscle tissue may be muscle strength and functionality rather than muscle mass. Muscle forces exert higher forces on bones than gravitational ones associated with weight [26]. Besides, it is known that muscle strength is affected before than muscle mass in development of sarcopenia. Moreover, loss of muscle strength could not be completely explained by the loss of muscle mass [27]. On the other hand, the muscle strength and mechanical load on the bone stimulates bone cells by producing factors that lead to bone formation, such as myokines [28, 29]. However, there are contradictory results regarding the relationship of muscle mass to osteoporosis. Ma et al. showed no association between muscle mass and osteoporosis; whereas, Kim SY et al. showed that it is positively correlated with bone density. However, this study defined low muscle mass with a lower cut-off value than that stated in the EWGSOP-2 [30, 31]. Since the cross-sectional design, this study could not define a cause-and-effect relationship. Thus, further prospective studies are needed.
We found that the risk of femoral neck osteoporosis was increased 3.188 times in the probable sarcopenia group and 7.63 times in the severe sarcopenia group. Also, probable sarcopenia increased the risk of femoral neck osteopenia by 2.75 times. Similarly, Kim SW et al. showed a relationship between handgrip strength and femoral neck BMD in older adults [32]. Handgrip strength is a useful measurement to predict slow gait speed, and also lower extremity strength [33]. Moreover, in computerized experimental models used to create femoral neck implants, the morphology of the femoral shaft could not be simulated without adding muscle forces [34]. Additionally, many studies have shown how muscle forces affect femoral shaft and proximal femur morphological characteristics in different ways during bone growth. All these data can explain why femoral neck bone mineral density is also associated with muscle force and strength [35]. Meanwhile, a slow gait speed increased the risk of femoral neck osteopenia and femoral neck osteoporosis by 2.21 times (p < 0.05) and 4.49 times, respectively (p < 0.001). Considering that walking speed is a reflection of leg muscle strength and gait speed is related to bone health [36], this is an expected result. Besides, slow gait speed is an independent risk factor for falls in older adults [37]. It can be seen how important this relationship is in terms of the risk of hip fracture. Considering that hip fractures with possible harmful consequences are the most critical complications of osteoporosis, it is vital to determine the risk factors for sarcopenia and osteoporosis and to take precautions in older adults.
The study has several strengths. First, all participants underwent a comprehensive geriatric assessment, and thus, other factors that could affect the results were eliminated. To elaborately investigate the relationship between sarcopenia and osteopenia/osteoporosis, we individually evaluated all three factors that play a role in the diagnosis of sarcopenia: muscle strength, muscle mass, and physical activity. As far as we are concerned, this study is one of the first studies to use the EWGSOP-2 criteria to investigate the relationship between sarcopenia and osteoporosis. We have some limitations in this study. The study has a retrospective and cross-sectional design. We had no data for anti-osteoporosis drug usage. On the other hand, we participate the subjects who applied geriatric outpatient clinic, that may make it hard to generalize the results of the study for whole population. Besides that, in this retrospective study we included the patients who had DEXA measurements. Even though osteoporosis is a major problem in both genders, it has been investigated mostly in females in daily practice because of DEXA measurements are recommended in earlier ages for female patients. Thus, while we had 359 female participants in this study, we had only 85 male participants. Moreover, in our study, adjustments were made for age, gender and BMI to determine the relationship between osteoporosis and dynapenia, or sarcopenia to eliminate this problem.
Conclusion
Low muscle strength, or dynapenia, and low physical performance seem to be associated with osteoporosis, and probable and severe sarcopenia are associated with osteoporosis in older adults. Moreover, probable sarcopenia, low muscle strength, and low physical performance were associated with femoral neck osteopenia and femoral neck osteoporosis in the current study. Therefore, osteodynapenia [10] may highlight this complex interrelationship better than osteosarcopenia. Furthermore, it is essential to evaluate osteoporosis and sarcopenia together as they have common modifiable risk factors, including low muscle strength and physical inactivity, as well as common adverse outcomes such as fractures, falls, and economic burden.
References
Kanasi E, Ayilavarapu S (2000) Jones J (2016) The aging population: demographics and the biology of aging. Periodontol 72:13–18. https://doi.org/10.1111/prd.12126
Cosman F, Randall S, de Beur SJ et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Christensen L, Iqbal S, Macarios D et al (2010) Cost of fractures commonly associated with osteoporosis in a managed-care population. J Med Econ 13:302–313. https://doi.org/10.3111/13696998.2010.488969
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521. https://doi.org/10.1001/jama.2009.50
Melton LJ, Achenbach SJ, Atkinson EJ et al (2013) Long-term mortality following fractures at different skeletal sites: a population-based cohort study. Osteoporos Int 24:1689–1696. https://doi.org/10.1007/s00198-012-2225-1
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Khosla S, Riggs BL (2005) Pathophysiology of age-related bone loss and osteoporosis. Endocrinol Metab Clin North Am 34(4):1015–1030
Hirschfeld HP, Kinsella R, Duque G (2017) Osteosarcopenia: where bone, muscle, and fat collide. Osteoporos Int 28:2781–2790. https://doi.org/10.1007/s00198-017-4151-8
Paintin J, Cooper C, Dennison E (2018) Osteosarcopenia. Br J Hosp Med 79:253–258
Balogun S, Winzenberg T, Wills K et al (2019) Prospective associations of osteosarcopenia and osteodynapenia with incident fracture and mortality over 10 years in community-dwelling older adults. Arch Gerontol Geriatr 82:67–73. https://doi.org/10.1016/j.archger.2019.01.015
Unutmaz GD, Soysal P, Tuven B, Isik AT (2018) Costs of medication in older patients: before and after comprehensive geriatric assessment. Clin Interv Aging 13:607–613. https://doi.org/10.2147/CIA.S159966
Janssen I, Heymsfield SB, Baumgartner RN, Ross R (2000) Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol 89:465–471. https://doi.org/10.1152/jappl.2000.89.2.465
Clark BC, Manini TM (2008) Sarcopenia ≠ Dynapenia. J Gerontol A. 63:829–834. https://doi.org/10.1093/gerona/63.8.829
(2004) Who scientific group on the assessment of osteoporosis at primary health. 5–7. https://who.int/chp/topics/Osteoporosis.pdf
Wright N, Looker A, Saag K et al (2014) The recent prevalence of osteoporosis and low bone mass in the United States. J Bone Miner Res 29:2520–2526. https://doi.org/10.1002/jbmr.2269.The
Tuzun S, Eskiyurt N, Akarirmak U et al (2012) Incidence of hip fracture and prevalence of osteoporosis in Turkey: the FRACTURK study. Osteoporos Int 23:949–955. https://doi.org/10.1007/s00198-011-1655-5
Anthamatten A, Parish A (2019) Clinical update on osteoporosis. J Wifery Womens Heal 64:265–275. https://doi.org/10.1111/jmwh.12954
Sahin Alak ZY, Ates Bulut E, Dokuzlar O et al (2020) Long-term effects of vitamin D deficiency on gait and balance in the older adults. Clin Nutr. https://doi.org/10.1016/j.clnu.2020.04.003
Thomas DR (2007) Loss of skeletal muscle mass in aging: Examining the relationship of starvation, sarcopenia and cachexia. Clin Nutr 26:389–399. https://doi.org/10.1016/j.clnu.2007.03.008
Patel H, Syddall H, Jameson K et al (2013) Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People ( EWGSOP ) definition : findings from the Hertfordshire Cohort Study ( HCS ). Age Ageing 42:378–384. https://doi.org/10.1093/ageing/afs197
Morley JE (2008) Sarcopenia: Diagnosis and treatment. J Nutr Heal Aging 12:452–456. https://doi.org/10.1007/BF02982705
Bulut EA, Soysal P, Aydin AE et al (2017) Vitamin B12 deficiency might be related to sarcopenia in older adults. Exp Gerontol 95:136–140. https://doi.org/10.1016/j.exger.2017.05.017
Yazar T, Olgun Yazar H (2019) Prevalance of sarcopenia according to decade. Clin Nutr ESPEN 29:137–141. https://doi.org/10.1016/j.clnesp.2018.11.005
Reiss J, Iglseder B, Alzner R et al (2019) Sarcopenia and osteoporosis are interrelated in geriatric inpatients. Z Gerontol Geriatr 52:688–693. https://doi.org/10.1007/s00391-019-01553-z
Lima RM, de Oliveira RJ, Raposo R et al (2019) Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos 14:1–8. https://doi.org/10.1007/s11657-019-0591-4
Burr DB (1997) Muscle strength, bone mass, and age-related bone loss. J Bone Min Res 12:1547–1551. https://doi.org/10.1359/jbmr.1997.12.10.1547
Kim YH, Il KK, Paik NJ et al (2016) Muscle strength: A better index of low physical performance than muscle mass in older adults. Geriatr Gerontol Int 16:577–585. https://doi.org/10.1111/ggi.12514
Morseth B, Emaus N, Jørgensen L (2011) Physical activity and bone: The importance of the various mechanical stimuli for bone mineral density. A review. Nor Epidemiol 20:173–178. https://doi.org/10.5324/nje.v20i2.1338
Souza D, Barbalho M, Ramirez-Campillo R et al (2020) High and low-load resistance training produce similar effects on bone mineral density of middle-aged and older people: a systematic review with meta-analysis of randomized clinical trials. Exp Gerontol 138:110973. https://doi.org/10.1016/j.exger.2020.110973
Ma Y, Fu L, Jia L et al (2018) Muscle strength rather than muscle mass is associated with osteoporosis in older Chinese adults. J Formos Med Assoc 117:101–108. https://doi.org/10.1016/j.jfma.2017.03.004
Kim S, Won CW, Kim BS et al (2014) The association between the low muscle mass and osteoporosis in elderly Korean people. J Korean Med Sci 29:995–1000. https://doi.org/10.3346/jkms.2014.29.7.995
Kim SW, Lee HA, Cho EH (2012) Low handgrip strength is associated with low bone mineral density and fragility fractures in postmenopausal healthy Korean women. J Korean Med Sci 27:744–747. https://doi.org/10.3346/jkms.2012.27.7.744
Fragala MS, Alley DE, Shardell MD et al (2016) Comparison of handgrip and leg extension strength in predicting slow gait speed in older adults. J Am Geriatr Soc 64:144–150. https://doi.org/10.1111/jgs.13871
Mittlmeier T, Mattheck C, Dietrich F (1994) Effects of mechanical loading on the profile of human femoral diaphyseal geometry. Med Eng Phys 16:75–81. https://doi.org/10.1016/1350-4533(94)90014-0
Yadav P, Shefelbine SJ, Pontén E, Gutierrez-Farewik EM (2017) Influence of muscle groups’ activation on proximal femoral growth tendency. Biomech Model Mechanobiol 16:1869–1883. https://doi.org/10.1007/s10237-017-0925-3
Sun W, Watanabe M, Tanimoto Y et al (2007) Ultrasound parameters of bone health and related physical measurement indicators for the community-dwelling elderly in Japan. Geriatr Gerontol Int 7:154–159. https://doi.org/10.1111/j.1447-0594.2007.00390.x
Dokuzlar O, Koc Okudur S, Smith L et al (2019) Assessment of factors that increase risk of falling in older women by four different clinical methods. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01220-8
Acknowledgements
None.
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no financial or non-financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ontan, M.S., Dokuzlar, O., Ates Bulut, E. et al. The relationship between osteoporosis and sarcopenia, according to EWGSOP-2 criteria, in outpatient elderly. J Bone Miner Metab 39, 684–692 (2021). https://doi.org/10.1007/s00774-021-01213-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-021-01213-6