Abstract
Background
There are limited data on the prognostic utility of regadenoson SPECT myocardial perfusion imaging (MPI) in patients with end-stage renal disease (ESRD).
Methods and Results
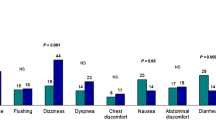
In a single-center, retrospective study, we analyzed consecutive ESRD patients who underwent regadenoson SPECT-MPI. The severity of MPI abnormalities and ischemic burden were determined quantitatively. The primary endpoint was major adverse cardiac events (MACE), defined as the composite of cardiac death or myocardial infarction. Among 1,227 subjects (mean age 54 ± 13 years, 47% men), 60 (5%) MACE were observed during a mean follow-up of 2.5 ± 1.8 years. The presence and severity of MPI abnormalities and ischemic burden were associated with a stepwise increase in MACE risk. Abnormal MPI (SSS ≥ 4) was associated with increased MACE risk, independent and incremental to relevant clinical covariates; adjusted hazard ratio, 1.95; 95% confidence interval, 1.15-3.32; Δχ2 = 5.97; P = .013. Myocardial ischemia (SDS ≥ 2) was associated with a trend towards increased MACE risk; adjusted hazard ratio, 1.63; 95% confidence interval, 0.96-2.77; Δχ2 = 3.12; P = .072.
Conclusion
In the largest cohort to date, we demonstrated the incremental prognostic value of abnormal MPI in predicting MACE risk in ESRD patients. Given its size, our study provides improved risk estimates in this population compared to previous reports.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion imaging (MPI) via single photon emission computed tomography (SPECT) is a well-established modality for the diagnosis and risk stratification of patients with suspected or known coronary artery disease (CAD).1,2 Regadenoson, a selective A2A adenosine receptor agonist, has been the most commonly used vasodilator agent for SPECT-MPI in the United States in virtue of its excellent safety and tolerability profile.3 Renal excretion accounts for 57% of regadenoson systemic elimination, which translates to delayed clearance in patients with impaired renal function.4,5 Nonetheless, previous studies have demonstrated the safe use of regadenoson in patients with advanced chronic kidney disease (CKD; stages III/IV), who are not yet on dialysis.6,7 Additionally, small observational studies validated its safety profile in patients with end-stage renal disease (ESRD).8,9,–10 Despite the high prevalence of CAD in ESRD patients and the importance of ischemic evaluation for cardiac risk stratification in renal transplant candidates,11,12,–13 there remains a paucity of data on the prognostic value of regadenoson SPECT-MPI in these patients. Hage et al previously concluded that regadenoson SPECT-MPI had excellent prognostic utility in a large retrospective study of all-comers, among whom 362 had ESRD.14 Subsequently, in a small prospective cohort of non-consecutive 303 ESRD patients enrolled in the ASSUAGE and ASSUAGE-CKD trials, our group demonstrated the prognostic utility of regadenoson SPECT-MPI in this population.15,16,–17 In this investigation, we sought to assert the prognostic utility of regadenoson SPECT-MPI in a large, consecutive ESRD patient cohort.
Methods
In a retrospective cohort study design, we analyzed consecutive ESRD patients who underwent regadenoson SPECT-MPI at Rush University Medical Center (Chicago, IL) in the period from July 1, 2009 to September 11, 2015. We excluded subjects with missing stress MPI data. Only the first regadenoson SPECT-MPI was analyzed in case there was more than one test performed during the study period. The detailed methodology of this cohort derivation was described elsewhere.18,19
Stress MPI Protocol and Analysis
All regadenoson SPECT-MPIs were performed per the American Society of Nuclear Cardiology guidelines.20,21 We have previously reported the specifics of stress testing, image acquisition, and processing.22,23 Standard 1-day rest/regadenoson stress protocol using 99mTc-tetrofosmin was done for almost all patients. However, dual-isotope protocol was occasionally used during periods of 99mTc shortage and 2-day protocol with 99mTc-tetrofosmin in morbidly obese individuals (body mass index ≥ 40 kg·m−2). Dual-head Siemens Ecam® camera (Siemens; Hoffman Estates, IL) was used to acquire the SPECT-MPI, without attenuation correction. Investigators, blinded to clinical and outcome data, assessed MPI scans quantitatively via Corridor 4DM software package (INVIA-Ann Arbor, MI), on a 17-segment model and the standard 5-point scale (0: normal, 1: mild, 2: moderate, 3: severe, 4: absent radiotracer activity). The total summed scores were used to generate summed stress score (SSS), summed rest score (SRS), and summed difference score (SDS). MPI studies were categorized, based on SSS, as normal (SSS = 0-3), mildly abnormal (SSS = 4-8), moderately abnormal (SSS = 9-13), and severely abnormal (SSS ≥ 14). Ischemic burden was categorized, based on SDS, into no ischemia (SDS = 0-1), mild ischemia (SDS = 2-4), and moderate to severe ischemia (SDS ≥ 5).1 Transient ischemic dilation (TID) was measured by calculating the ratio of stress to rest left ventricular (LV) volumes, derived from the ungated SPECT images. Abnormal TID ratio was considered for values of 1.31 and above.24,25 We quantitatively measured rest and post-stress LV ejection fraction (LVEF). The LVEF reserve was calculated from subtracting rest LVEF from post-stress LVEF.26 LV dysfunction was defined as an abnormal LVEF (< 50%).
Endpoints
We observed the patients for the following outcomes of interest: death, cardiac death (CD), myocardial infarction (MI), surgical or percutaneous coronary revascularization (CR), and renal transplantation. We defined late CR (LCR) as revascularization taking place over 90 days following the stress MPI, which were deemed as events not directly triggered by the results of MPI.15 We obtained death events using the social security death index or chart review done by investigators blinded to clinical and imaging data. Detailed chart review (whenever possible) or death certificates were used to determine the cause of death. CD was defined as death due fatal MI, fatal arrhythmias, or heart failure. Non-fatal MI was defined as an elevation in cardiac biomarkers ≥ 3 times above the upper limit of normal and the clinical determination of the managing cardiologist, guided by the global definition of MI. The primary endpoint was major adverse cardiac events (MACE), defined as the composite of CD or MI. The secondary endpoints were (i) composite of Death/MI, (ii) composite of CD/MI/LCR, and (iii) all-cause mortality.
Statistical Analysis
Continuous data were presented as mean ± standard deviation while categorial data were presented as frequencies and percentages. Kaplan-Meier plots and the log-rank test were used to compare event-free survival. Univariate and multivariate Cox regression models were used to assess the unadjusted and adjusted risk of adverse outcomes, with risk estimates expressed as hazard ratios (HR) and 95% confidence intervals (CI). We adjusted for the following clinically relevant covariates: age, sex, smoking, dyslipidemia, diabetes mellitus, and prior history of CAD. Covariates were limited to 1 degree of freedom for every 10 events. Hypertension was not included in multivariate adjustment since it was prevalent in over 90% of the study cohort. The date of stress MPI was considered time zero in the survival analysis, whereas follow-up time was defined by either a qualifying event, last event-free encounter, or a maximum follow-up duration of 6.5 years, whichever took place first. Since renal transplant is known to improve the outcomes of ESRD patients,12 we performed additional sensitivity survival analyses in which we terminated the follow-up at the date of transplant and censored all ensuing outcome events. Nested stepwise Cox regression models were used to determine the incremental prognostic value of abnormal MPI, myocardial ischemia, or LV dysfunction, using the absolute increase in global chi-square (χ2) statistic, calculated by likelihood ratio test, and the corresponding P value. Using the coordinates of the receiver operating characteristic (ROC) curve for TID ratio as a predictor of MACE, we aimed to identify an exploratory threshold that optimizes the discriminatory prognostic capacity of TID for the primary outcome. A two-tailed P value of < .05 was the criterion for statistical significance. We used SPSS software package, version 23 (IBM, Inc., Armonk, NY) to perform all statistical analyses.
Results
Among 1,250 ESRD patients who underwent regadenoson SPECT-MPI, 23 were excluded due to missing imaging data. Table 1 summarizes the baseline clinical and imaging characteristics of the 1,227 patients included in the final cohort. Briefly, the mean age was 54 ± 13 years and 47% were men. Renal transplant evaluation was the most common indication for MPI (N = 949, 77.3%). A total of 321 (26.2%) had an abnormal MPI and 299 (24.4%) had myocardial ischemia. The mean follow-up period for clinical and composite events was 2.5 ± 1.8 years. The duration of follow-up for all-cause mortality (as a single outcome) was slightly longer at 2.8 ± 1.8 years, since a clinical encounter is not needed to determine the last vital status. During follow-up, there were 204 (16.6%) deaths, 27 (2.2%) confirmed CD, 38 (3.1%) MI, 85 (6.9%) CR, and 47 (3.8%) LCR events. Notably, 365 (29.7%) patients underwent renal transplant during follow-up, at a mean of 2.4 ± 1.9 years after MPI.
Primary Endpoint
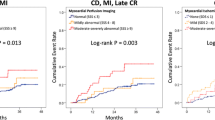
During the follow-up period, 60 (5%) MACE were observed. SSS, as a continuous variable, was independently predictive of MACE after adjusting for clinical covariates (age, sex, smoking, dyslipidemia, diabetes mellitus, prior history of CAD); adjusted HR, 1.03 per 1 SSS point increment; CI, 1.01-1.06; P = .013. The frequency of MACE rate was more than double in patients with an abnormal MPI (SSS ≥ 4) compared to patients with a normal MPI (8.4% vs 3.6%, P = .001). The presence and severity of MPI abnormalities and ischemic burden were associated with a stepwise increase in MACE (Figure 1A). Abnormal MPI was associated with an increased MACE risk, independent of clinical covariates; adjusted HR, 1.95; CI, 1.15-3.32; P = .013 (Figure 1A). Annualized MACE rate among patients with normal MPI was 1.4% and there was a stepwise increase in MACE rates with increasing severity of MPI abnormalities (Figure 2A). MPI findings provided further incremental prognostic value for predicting MACE beyond clinical covariates alone (Δχ2 = 5.97, P = .015), as shown in Figure 3.
Incremental prognostic value of regadenoson SPECT-MPI. Bar chart depicts global chi-square statistics derived from 3-step nested Cox proportional hazards models. MACE, major adverse cardiac events; CD, cardiac death; MI, myocardial infarction; MPI, SPECT myocardial perfusion imaging. Clinical variables include age, sex, diabetes mellitus, dyslipidemia, active smoking, and known coronary artery disease status. MPI is defined as normal vs. abnormal (summed stress score ≥ 4 vs ≤ 3). LV Function is defined as normal vs. abnormal (left ventricular ejection fraction ≥ 50% vs < 50%).
MACE rate was almost double in patients with myocardial ischemia (SDS ≥ 2) compared to those without myocardial ischemia (8.0% vs 3.9%, P = .004). As a continuous variable, unadjusted SDS was significantly associated with MACE; HR, 1.05 per 1-point increment; CI, 1.01-1.09; P = .026, but statistical significance was lost after adjusting for clinical covariates; HR, 1.03; CI, 0.98-1.09; P = .243. As a dichotomous variable, and after adjusting for clinical covariates, myocardial ischemia was associated with a trend towards an increase in MACE risk; adjusted HR, 1.63; CI, 0.96-2.77; P = .072. The presence and severity of myocardial ischemia were associated with a stepwise increase in MACE (Figure 1B) which translated to a stepwise increase in annualized MACE rates with increasing ischemic burden (Figure 2B). Myocardial ischemia provided a borderline incremental prediction of MACE risk to clinical covariates alone (Δχ2 = 3.12, P = .077).
In sensitivity survival analyses, in which we censored follow-up at the time of renal transplantation (if occurred during the study period), abnormal MPI was significantly associated with an increased MACE risk, after adjusting for clinical covariates (Supplemental Table 1). On the other hand, myocardial ischemia was associated with a trend towards an increase in MACE risk, after adjusting for clinical covariates (Supplemental Table 2).
In ROC analysis, TID provided a modest discriminatory capacity for predicting MACE (area under the curve, 0.62; CI, 0.54-0.69; P = .002). TID, as a continuous variable, was associated with an increased MACE risk, after adjusting for clinical covariates (adjusted HR, 1.18; CI, 1.07-1.30; P = .001). A previously published TID threshold of ≥ 1.31,24 provided a prognostic sensitivity and specificity for MACE of 8% and 96%, respectively. However, a dichotomous TID of ≥ 1.31 was not associated with a statistically significant increase in MACE risk, after adjusting for clinical covariates (adjusted HR; 1.91, CI, 0.76-4.81; P = .170). On further exploratory analyses of the TID/MACE ROC curve coordinates, we iteratively identified a TID ratio of ≥ 1.15 as a threshold that can provide an improved prognostic discriminatory capacity, with a sensitivity and specificity for MACE of 28% and 84%, respectively. TID ratio of ≥1.15 was associated with a significant increase in MACE risk, after adjusting for clinical covariates (adjusted HR, 1.82; CI, 1.03-3.22; P = .041).
LVEF, as a continuous variable, was associated with MACE risk after adjusting for clinical covariates; adjusted HR, 1.25 per 10-point decrement in LVEF; CI, 1.03-1.49; P = .022. Similarly, LV dysfunction (LVEF < 50%), was associated with an increased MACE risk after adjusting for clinical covariates; adjusted HR, 2.43; CI, 1.40-4.23; P = .002. LV function (normal vs abnormal) provided incremental prognostic value to clinical covariates and abnormal MPI, as shown in Figure 3.
Secondary Endpoints
During the study follow-up period, there were 229 (18.7%) composite Death/MI and 93 (7.6%) composite CD/MI/LCR events. The frequencies of composite Death/MI, composite CD/MI/LCR, and all-cause mortality were higher in patients with an abnormal MPI (SSS ≥ 4) compared to patients with normal MPI (25.9% vs 16.1%, 11.8% vs 6.1%, 21.8% vs 14.8%, all P < .01). After adjusting for clinical covariates, abnormal MPI (SSS ≥ 4) was independently associated with an increased risk of composite Death/MI (adjusted HR, 1.73; CI, 1.31-2.29; P < .001), composite CD/MI/LCR (adjusted HR, 1.56; CI, 1.02-2.40; P = .040), and all-cause mortality (adjusted HR, 1.43; CI, 1.06-1.93; P = .021). Among patients with normal MPI, annualized events rates were as follows: composite Death/MI 6.2%, composite CD/MI/LCR 2.3%, and all-cause mortality 5.2%. There was a stepwise increase in the rates of the secondary endpoints with increasing MPI abnormality (Figure 2A).
The frequencies of composite Death/MI, composite CD/MI/LCR, and all-cause mortality were higher in patients with myocardial ischemia (SDS ≥ 2) compared to patients without myocardial ischemia (24.4% vs 16.8%, 12.7% vs 5.9%, 22.1% vs 14.9%; all P < .05). After adjusting for clinical covariates, myocardial ischemia (SDS ≥ 2) was associated with an increased risk of the composite Death/MI (adjusted HR, 1.41; CI, 1.06-1.87; P = .019), the composite CD/MI/LCR (adjusted HR, 1.64; CI, 1.07-2.50; P = .022), and all-cause mortality (adjusted HR, 1.43; CI, 1.06-1.94; P = .019). Increasing severity of myocardial ischemia was associated with a stepwise increase in annualized event rates of all secondary outcomes (Figure 2B).
In sensitivity survival analyses, in which we censored follow-up at the time of renal transplantation (if occurred during the study period), abnormal MPI and myocardial ischemia were associated with significant increases in the risk of Death/MI and CD/MI/LCR, after adjusting for clinical covariates. On the other hand, abnormal MPI and myocardial ischemia were associated with a trend towards an increased risk of all-cause mortality (Supplemental Tables 1 and 2).
After adjusting for clinical covariates, TID, as a continuous variable, was associated with an increased risk of the composite Death/MI (adjusted HR, 1.13 per 0.1-point increment; CI, 1.07-1.19; P < .001), the composite CD/MI/LCR (adjusted HR, 1.10 per 0.1-point increment; CI, 1.01-1.20; P = .023), and all-cause mortality (adjusted HR, 1.14 per 0.1-point increment; CI, 1.07-1.21; P < .001). When abnormal TID was assessed as a dichotomous variable (ratio ≥ 1.31), and after adjusting for clinical covariates, it was only associated with a borderline significant increase in the composite Death/MI (adjusted HR, 1.68; CI, 1.00-2.79; P = .048), but it was not associated with a significant increase in the risk of the composite CD/MI/LCR (adjusted HR, 1.23; CI, 0.53-2.83; P = .630) or all-cause mortality (adjusted HR, 1.60; CI, 0.93-2.77; P = .091).
Discussion
To our knowledge, this is the largest study to date to report on the prognostic utility of SPECT-MPI in patients with ESRD. The study confirmed that the presence and severity of perfusion abnormalities with regadenoson SPECT-MPI were associated with an independent and incremental prognostic value for MACE of CD or MI, the composite endpoints of Death/MI and CD/MI/LCR, as well as all-cause mortality. The prognostic utility of regadenoson SPECT-MPI was generally consistent when we censored the survival analyses at renal transplantation. Notably, the annualized MACE rate of 1.4% for patients with normal regadenoson SPECT-MPI in the present cohort may have been underestimated on account of the retrospective nature of our study, yet is significantly lower than previously reported in ESRD patients (4.9%).15 However, the annualized composite of Death/MI among patients with normal MPI was 6.2% which is in line with historic data. Nonetheless, the observed annualized MACE rate is expectedly higher than that reported among all-comers with normal vasodilator SPECT-MPI (1.1%)27 or, more specifically, those with regadenoson SPECT-MPI (0.9-1.1%).14,25,28 Moreover, we affirmed that the presence and severity of regadenoson-induced myocardial ischemia with SPECT-MPI were associated with a stepwise increase in adverse cardiac events and all-cause mortality. Lastly, we demonstrated the independent association of LV dysfunction with MACE, highlighting its incremental prognostic value above and beyond clinical and imaging covariates.25
Although our study asserts the significant prognostic value of regadenoson SPECT-MPI in ESRD patients, it is important to note the modest effect sizes of abnormal MPI and myocardial ischemia in this cohort (i.e., HRs < 2), compared to historical data in all-comers. By the same token, the incremental prognostic value of MPI abnormalities, beyond clinical covariates, is rather minimal. It is plausible that outcomes of these patients are more strongly influenced by their ESRD/hemodialysis status and associated comorbidities than by perfusion abnormalities. This elevated baseline risk may result in minimizing the contribution of perfusion imaging in determining the overall prognosis of these patients.11,12,–13 The prognostic impact of baseline renal function is supported by the earlier findings of Hakeem et al29 who demonstrated that, in patients undergoing stress MPI (32% exercise and 68% adenosine), both MPI results as well as CKD are independent and incremental predictors of cardiac death and all-cause mortality.
Our main findings are concordant with other reports in the literature. For instance, Hage et al14 previously reported excellent prognostic implications of regadenoson SPECT-MPI in a large retrospective study of 1,400 patients of all-comers, albeit only 362 of whom had ESRD. In their analysis, ESRD was found to be an independent predictor of CD. However, the authors did not specifically study the prognostic value of regadenoson MPI in ESRD.15 Bhatti et al have shown an independent prognostic value for SPECT-MPI across various degrees of renal dysfunction, predominantly CKD not yet in ESRD status.30 Our study population was an all-ESRD cohort, many of whom were undergoing routine ischemic evaluation as part of the renal transplantation work-up while on the transplant waiting list. In previously published data from representative overlapping cohorts from our center, we reported that the mean duration of dialysis in our ESRD population was 3.6 ± 3.5 years, with 92% on hemodialysis and 8% on peritoneal dialysis.15 We also previously reported that 43% of ESRD patients undergoing renal transplant evaluation have unconfirmed etiology of ESRD, while 38% of patients were presumed to have hypertension, diabetes mellitus, or combined hypertension and diabetes as their etiology of ESRD. Glomerular disease and polycystic kidney disease, each comprised 5% of the ESRD population.13
It is well established that renal transplant has a favorable impact on the outcome of patients with ESRD.12 In the present report, we did not evaluate the impact of MPI findings on post-transplant outcomes. However, our group has previously reported on the impact of pre-transplant MPI, with various stress modalities, on post-transplant outcomes in a cohort of renal transplant recipients. The study demonstrated that the diagnostic and the prognostic utility of stress MPI is dependent on the pre-transplant clinical risk. In fact, the predictive value of MPI followed the Bayes’ Theorem, such that patients with an intermediate pre-transplant risk (3-4 transplant risk factors) derived the most value from pre-transplant MPI in prognosticating long-term, post-transplant MACE risk. Pre-transplant MPI findings did not provide a significant prognostic value in patients with lower and higher clinical risk, as their outcomes were primarily commensurate to their baseline clinical risk regardless of MPI findings.3,11,13
We have previously conducted the first prospective evaluation of the prognostic utility of regadenoson SPECT-MPI in patients with ESRD.15 This was done on 303 non-consecutive ESRD patient cohort enrolled in the ASSUAGE and ASSUAGE-CKD trials.16,17 The results were notable for a preserved prognostic utility in this patient population, which is in keeping with our findings herein. Interestingly, in our previous report,15 the annualized MACE rate in subjects with normal MPI was considerably higher than this cohort (4.9% vs 1.4%). This may be explained by the older age (mean age 62 vs 54 years), more comorbidities (e.g., DM 43% vs 28%), and known symptomatic CAD (e.g., chest pain or dyspnea accounted for ~ 68% of indications for stress MPI) in the prior study’s cohort. Furthermore, owing to the retrospective nature of the current study, we speculate that MACE may have been underestimated due to less ascertainment of CD as cause of mortality and possible missed MI events. However, all other outcomes seemed consistent between our previous prospective evaluation15 and the current report. We have previously reported on the robust prognostic value of blunted heart rate response in ESRD patients and in renal transplant recipients. In fact, heart rate response can refine risk prediction in ESRD patients, particularly among those with normal MPI.31,32,–33
TID, as a continuous variable, was associated with an increased risk of adverse cardiac events and all-cause mortality in our current cohort. However, when assessed as a dichotomous variable (ratio ≥ 1.31), this association was not statistically significant or with a marginal trend towards statistical significance. This may be related to the limited number of events, resulting in “type II error.” Golzar et al previously demonstrated that TID does not add useful diagnostic information for severe and extensive CAD.24 Conversely, Lester et al,34 who defined abnormal TID as ratio ≥ 1.33, concluded that it adds important prognostic information in patients with an abnormal MPI. In their analysis of 887 patients,34 they found a significant association between TID and the composite CD/MI/LCR, which was mostly driven by the LCR events. It is worth noting that the selection of subjects with normal MPI in the aforementioned cohort may have accentuated the predictive value of TID. This contrasts with our non-selected, consecutive patient cohort which may have included borderline or technically inferior studies, translating into “data noise,” which may have curtailed the predictive capacity of TID. Nevertheless, our unselected patient cohort more likely mimics the real-world scenarios. The diagnostic and prognostic value of TID has been somewhat conflicting in recent literature,24,35 perhaps due to decreasing prevalence of severe and extensive CAD in contemporary cohorts compared to historical data.36,37 Traditionally, abnormal TID threshold is determined in a population with low likelihood of CAD as a value greater than 2 standard deviations above the mean. Such methodology yields a threshold with low sensitivity, but high specificity, for severe CAD. However, with low prevalence of severe CAD in contemporary cohorts, it is likely that the low sensitivity renders such a threshold ineffective in identifying patients at risk. Therefore, redefining the TID threshold to optimize its diagnostic and prognostic performance may be necessary. In this report, we explored deriving an optimal TID threshold from an iterative examination of the coordinates of the TID/MACE ROC curve. Indeed, we identified the TID ratio of ≥ 1.15 as a threshold that can provide an improved prognostic discriminatory capacity. We caution, however, that this threshold was iteratively derived to optimize the prognostic discriminatory capacity in this particular cohort. Thus, external validation of this methodology and threshold is prudent.
Previous studies have reported on the prognostic value of pharmacologic stress MPI in the setting of renal dysfunction. A report from Australia demonstrated the utility of different stress MPI modalities (exercise, dobutamine, right atrial pacing, and dipyridamole) in 387 patients being evaluated for renal transplant.38 Al-Mallah et al39 studied a large consecutive patient cohort of 7,348 all-comers undergoing SPECT-MPI (exercise, adenosine, and dobutamine) and demonstrated the modest value it adds in predicting death across various degrees of renal dysfunction, although predominantly not declared ESRD. Our findings in this large, consecutive ESRD patient cohort are a continuum to these reports, specifically in terms of the modest incremental prognostic value that MPI findings provide in this patient population.
Limitations
Our findings are subject to all limitations inherent to a single-center, retrospective study design. MACE may have been underestimated since the ascertainment of cardiac death was only inclusive of confirmed cardiac death cases. It is also plausible that some MI events may have not been captured. Additionally, owing to its observational nature, the long-term outcomes in our study may have been influenced by MPI-guided CR and medical therapy. We attempted to mitigate this limitation by focusing on LCR rather than CR events. Lastly, the cause of death was occasionally determined via death certificates review, which may have been inaccurate.
New Knowledge Gained
Our report is the largest to date to assert the prognostic utility of regadenoson SPECT-MPI, as an independent and incremental predictor of cardiac-specific outcomes as well as all-cause mortality in ESRD patients. Given its size, our study provides improved risk estimates compared to previous reports. The prognostic utility of TID is inconsistent. Further examination of an optimal TID threshold remains warranted.
Conclusions
In the largest cohort to date, stress MPI provides independent and incremental prognostic value in predicting adverse cardiac events and all-cause mortality in patients with ESRD.
Abbreviations
- CAD:
-
Coronary artery disease
- CD:
-
Cardiac death
- CKD:
-
Chronic kidney disease
- CR:
-
Coronary revascularization
- ESRD:
-
End-stage renal disease
- LCR:
-
Late coronary revascularization
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiac events
- MI:
-
Myocardial infarction
- MPI:
-
Myocardial perfusion imaging
- ROC:
-
Receiver operating characteristic
- SDS:
-
Summed difference score
- SSS:
-
Summed stress score
- TID:
-
Transient ischemic dilation
References
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation 2013;128:1634-43.
Doukky R, Frogge N, Balakrishnan G, Hayes K, Collado FM, Rangel MO, et al. The prognostic value of cardiac SPECT performed at the primary care physician’s office. J Nucl Cardiol 2013;20:519-28.
Vij A, Golzar Y, Doukky R. Regadenoson use in chronic kidney disease and end-stage renal disease: A focused review. J Nucl Cardiol 2018;25:137-49.
Gordi T, Frohna P, Sun HL, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet 2006;45:1201-12.
Gordi T, Blackburn B, Lieu H. Regadenoson pharmacokinetics and tolerability in subjects with impaired renal function. J Clin Pharmacol 2007;47:825-33.
Ananthasubramaniam K, Weiss R, McNutt B, Klauke B, Feaheny K, Bukofzer S. A randomized, double-blind, placebo-controlled study of the safety and tolerance of regadenoson in subjects with stage 3 or 4 chronic kidney disease. J Nucl Cardiol 2012;19:319-29.
Palani G, Husain Z, Salinas RC, Karthikeyan V, Karthikeyan AS, Ananthasubramaniam K. Safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic kidney disease patients not on hemodialysis. J Nucl Cardiol 2011;18:605-11.
Aljaroudi W, Hermann D, Hage F, Heo J, Iskandrian AE. Safety of regadenoson in patients with end-stage renal disease. Am J Cardiol 2010;105:133-5.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: the first prospective evaluation. J Nucl Cardiol 2013;20:205-13.
Gharibian KN, Murthy VL, Mueller BA. Influence of hemodialysis on regadenoson clearance in an in vitro hemodialysis model. J Nucl Cardiol 2016. https://doi.org/10.1007/s12350-016-0667-0.
Golzar Y, Doukky R. Stress SPECT myocardial perfusion imaging in end-stage renal disease. Curr Cardiovasc Imaging Rep 2017;10:13.
Parikh K, Appis A, Doukky R. Cardiac imaging for the assessment of patients being evaluated for kidney or liver transplantation. J Nucl Cardiol 2015;22:282-96.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Kharouta M, Vij A, et al. Validation of a clinical pathway to assess asymptomatic renal transplant candidates using myocardial perfusion imaging. J Nucl Cardiol 2018;25:2058-68.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol 2015;22:1214-21.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2017;24:112-8.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “The ASSUAGE trial”. J Nucl Cardiol 2012;19:448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Margeta B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease—The ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29:1029-37.
Doukky R, Nigatu A, Khan R, Anokwute C, Fughhi I, Ayoub A, et al. Prognostic significance of ischemic electrocardiographic changes with regadenoson stress myocardial perfusion imaging. J Nucl Cardiol 2018. https://doi.org/10.1007/s12350-018-1415-4.
Iskander F, Iskander M, Gomez J, Doukky R. Prognostic value of regadenoson stress myocardial perfusion imaging in patients with left bundle branch block or ventricular paced rhythm. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01762-4.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016. https://doi.org/10.1007/s12350-015-0387-x.
Tilkemeier PL, Bourque J, Doukky R, Sanghani R, Weinberg RL. ASNC imaging guidelines for nuclear cardiology procedures: Standardized reporting of nuclear cardiology procedures. J Nucl Cardiol 2017;24:2064-128.
Chawla D, Rahaby M, Amin AP, Vashistha R, Alyousef T, Martinez HX, et al. Soft tissue attenuation patterns in stress myocardial perfusion SPECT images: A comparison between supine and upright acquisition systems. J Nucl Cardiol 2011;18:281-90.
Ballany W, Mansour K, Morales Demori R, Al-Amoodi M, Doukky R. The impact of regimented aminophylline use on extracardiac radioisotope activity in patients undergoing regadenoson stress SPECT myocardial perfusion imaging: A substudy of the ASSUAGE trial. J Nucl Cardiol 2014;21:496-502.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99m myocardial perfusion SPECT. J Nucl Cardiol 2015;22:526-34.
Kattoor AJ, Kolkailah AA, Iskander F, Iskander M, Diep L, Khan R, et al. The prognostic value of regadenoson SPECT myocardial perfusion imaging: The largest cohort to date. J Nucl Cardiol 2020. https://doi.org/10.1007/s12350-020-02135-y.
Gomez J, Golzar Y, Fughhi I, Olusanya A, Doukky R. The significance of post-stress decrease in left ventricular ejection fraction in patients undergoing regadenoson stress gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2018;25:1313-23.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, Raslan S, Heo J, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014-21.
Hakeem A, Bhatti S, Dillie KS, Cook JR, Samad Z, Roth-Cline MD, et al. Predictive value of myocardial perfusion single-photon emission computed tomography and the impact of renal function on cardiac death. Circulation 2008;118:2540-9.
Bhatti S, Hakeem A, Dhanalakota S, Palani G, Husain Z, Jacobsen G, et al. Prognostic value of regadenoson myocardial single-photon emission computed tomography in patients with different degrees of renal dysfunction. Eur Heart J Cardiovasc Imaging 2014;15:933-40.
AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol 2016;23:560-9.
AlJaroudi W, Anokwute C, Fughhi I, Campagnoli T, Wassouf M, Vij A, et al. The prognostic value of heart rate response during vasodilator stress myocardial perfusion imaging in patients with end-stage renal disease undergoing renal transplantation. J Nucl Cardiol 2019;26:814-22.
Gomez J, Fughhi I, Campagnoli T, Ali A, Doukky R. Impact of integrating heart rate response with perfusion imaging on the prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2017;24:1666-71.
Lester D, El-Hajj S, Farag AA, Bhambhvani P, Tauxe L, Heo J, et al. Prognostic value of transient ischemic dilation with regadenoson myocardial perfusion imaging. J Nucl Cardiol 2016;23:1147-55.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: A cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol 2013;20:774-84.
Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE, et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 2013;61:1054-65.
Duvall WL, Rai M, Ahlberg AW, O’Sullivan DM, Henzlova MJ. A multi-center assessment of the temporal trends in myocardial perfusion imaging. J Nucl Cardiol 2015;22:539-51.
Chew CG, Unger S, Shakib S. Value of myocardial perfusion imaging in renal transplant evaluation. Nephrology (Carlton) 2013;18:376-81.
Al-Mallah MH, Hachamovitch R, Dorbala S, Di Carli MF. Incremental prognostic value of myocardial perfusion imaging in patients referred to stress single-photon emission computed tomography with renal dysfunction. Circ Cardiovasc Imaging 2009;2:429-36.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Funding
The study was funded in part by Astellas Pharma Global Development (Northbrook, IL). The funding source had no input in the study design, execution, data analysis and interpretation, or manuscript preparation and approval.
Author’s social text
In the largest cohort to date, #regadenoson #MPI provides independent and incremental #prognostic_value for predicting #MACE in patients with #ESRD. @RamiDoukky @AKolkailah @CookCtyHealth @RushMedical #CVNuc @JNCjournal @MyASNC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kolkailah, A.A., Iskander, M., Iskander, F. et al. The prognostic utility of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease: The largest cohort to date. J. Nucl. Cardiol. 29, 101–110 (2022). https://doi.org/10.1007/s12350-020-02259-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02259-1