Abstract
Background
Regadenoson is a novel pharmacological stress agent whose disposition during hemodialysis is not known. The purpose of this study was to determine the clearance of regadenoson under varying dialytic conditions using an in vitro hemodialysis model.
Methods and Results
Whole human blood was used to analyze the effect of hemodialysis on the clearance of regadenoson. Regadenoson transmembrane clearance (CLD) was assessed for both a standard permeability and a high permeability polysulfone hemodialyzer with blood/dialysate flow rates of 300/600 and 400/800 mL/min. A two-tailed, paired Student’s t test was used to compare regadenoson CLD between hemodialyzer types and flow rates. The mean ± SD regadenoson CLD values ranged between 62.5 ± 11.8 and 89.1 ± 24.0 mL/min for all dialytic conditions. There was no significant difference in regadenoson CLD between hemodialyzer types and flow rates (p > .05).
Conclusions
Hemodialysis enhances the clearance of regadenoson independent of hemodialyzer permeability and blood/dialysate flow rate. This clearance is modest relative to total body clearance and is unlikely to produce a clinically significant outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Regadenoson, a selective adenosine 2A receptor agonist, was approved by the United States Food and Drug Administration in April 2008 for use as a pharmacologic stress agent with radionuclide myocardial perfusion imaging (MPI), including single-photon emission computed tomography (SPECT) MPI.1,2 Regadenoson primarily acts on arteriolar smooth muscle cells to induce hyperemia via coronary vasodilation, aiding in the detection of coronary artery disease (CAD) and other perfusion abnormalities.3-5 Following intravenous administration of a single 0.4 mg bolus dose, regadenoson undergoes rapid distribution (peak plasma concentration within 1-3 minutes) followed by slower elimination with a half-life of approximately 2 hours. It is primarily eliminated via renal tubular secretion (58% excreted unchanged) and has a prolonged half-life of approximately 4 hours in patients with severe renal impairment (creatinine clearance <30 mL/min).6,7
Cardiovascular disease, including CAD, is a leading cause of mortality in chronic kidney disease (CKD) patients receiving dialysis (stage 5D).8,9 In 2013, over half the deaths among CKD stage 5D patients were attributed to this disease.9 Consequently, most CKD patients on dialysis, including those seeking renal transplantation, are routinely evaluated for CAD, often with regadenoson stress SPECT MPI.10-12 Despite its prevalent use, few studies on regadenoson have been conducted in patients with CKD on hemodialysis. Studies by Doukky and AlJaroudi et al used a subset of CKD stage 5D patients from the ASSUAGE and ASSUAGE-CKD trials and other databases to show the safety and prognostic value of regadenoson in this population.12-17 No studies, however, have yet evaluated the pharmacokinetics of regadenoson in patients with CKD stage 5D to show how hemodialysis may influence the clearance of regadenoson. Based on its small molecular weight (408 Da) and low plasma protein binding (30%), regadenoson has the potential to be removed by hemodialysis. However, its relatively large volume of distribution (63-75 L) may offset this potential.2,7 In this study, we assessed the effect of hemodialysis on the clearance of regadenoson under varying dialytic conditions using an in vitro hemodialysis model.
Methods
Our in vitro model used a commercially available Fresenius 2008K dialysis machine (Fresenius Medical Care, Waltham, MA) to assess regadenoson clearance during hemodialysis. This model used, as a patient surrogate, one liter of continuously stirred, sodium heparin-anticoagulated, whole human blood (BioreclamationIVT, Westbury, NY) placed in an Erlenmeyer flask and warmed to 37 °C in a water bath. The dialysis circuit was connected using a compatible Fresenius hemodialysis blood tubing set primed with 0.9% NaCl and one of two hemodialyzers (filters): a standard permeability (low flux) polysulfone hemodialyzer (Fresenius Hemoflow™ F8; ultrafiltration coefficient (K uf) = 7.5 mL/h/mmHg; surface area = 1.8 m2) and a high permeability (high flux) polysulfone hemodialyzer (Fresenius Optiflux® F160NR; K uf = 50 mL/h/mmHg; surface area = 1.5 m2). Dialysate was prepared using manufacturer-recommended Naturalyte® 4000 sodium bicarbonate concentrate (Fresenius Medical Care) and Centrisol® calcium-free acid concentrate (Minntech, Minneapolis, MN) diluted with deionized water in a 1:45 ratio.
Regadenoson (Lexiscan®, Astellas Pharma Inc., Northbrook, IL) was obtained and used in its commercially available form (0.4 mg/5 mL syringe for injection, Lot Nos. 49-048-EV and 50-028-EV). Based on findings from an initial dose-finding experiment, 24 µg (0.3 mL) of regadenoson was added to the flask of warmed blood to target the average peak plasma concentration of 17.5 ng/mL that is observed after a single 0.4 mg dose in patients with severe kidney dysfunction (creatinine clearance <30 mL/min).7 Urea (750 mg, Lot No. 30K0221; Sigma, St. Louis, MO) and creatinine (100 mg, Lot No. 072K0094; Sigma) were added to the blood as control markers. Solutes were allowed to mix continuously in the blood for 10 minutes to ensure even distribution of all solutes. The blood was recirculated through the dialysis circuit for an additional 20 minutes to allow for uniform coating of the tubing and hemodialyzer. Dialysis and ultrafiltration were turned off during recirculation.
Hemodialysis was performed in single-pass mode at blood flow rates (Q b) of 300 and 400 mL/min and dialysate flow rates (Q d) of 600 and 800 mL/min, respectively. Each hemodialyzer was tested for both flow rate pairs. Ultrafiltration flow rate was set to zero for all runs of hemodialysis. Blood samples were collected simultaneously from the prefilter and postfilter ports of the dialysis circuit approximately 90 seconds after initiation of hemodialysis. The filtered blood was collected in an empty flask for disposal. This procedure was repeated eight times for each hemodialyzer flow rate pair. A new hemodialyzer and blood tubing set was used for each run of hemodialysis.
Collected blood samples were centrifuged at 3000 rpm for 10 minutes, and the separated plasma was transferred to 2.0 mL polypropylene cryogenic vials (Fisher Scientific, Pittsburgh, PA), labeled, and stored at −80 °C until analysis.
Sample Analysis
Regadenoson concentration was determined using a validated high-performance liquid chromatography assay. Plasma samples containing regadenoson were extracted with ammonium acetate (solid phase extraction). The eluate was evaporated and reconstituted and an aliquot was analyzed on an API 5000 LC system with tandem mass spectrometric detection (AB Sciex LLC, Framingham, MA). Blood urea nitrogen and creatinine concentrations were analyzed on a Siemens Advia 1800 chemistry system (Tarrytown, NY). The lower limits of detection for BUN and creatinine were 5 and 0.1 mg/dL, respectively, with a coefficient of variation (precision) of ≤4.7%. Blood hematocrit was measured using a microcapillary centrifuge (Model MB, IEC, Needham Heights, MA) and a dial reader.
Calculations
The extraction ratio (E) and transmembrane clearance during hemodialysis (CLD) for regadenoson, urea, and creatinine were calculated for each hemodialyzer using the following equations:
where C a is the prefilter solute concentration, C v is the postfilter solute concentration, Q b is the blood flow rate in mL/min, and Hct is the blood hematocrit.
Statistical Analysis
A power analysis indicated that 8 experiments were required to detect a 20% difference in the dialytic clearance of regadenoson between filter types. Assumptions used in these calculations included: a power of 90% and a standard deviation of 10% with a significance level of p < .05. A two-tailed, paired Student’s t test was used to compare extraction ratio and solute clearance between hemodialyzer types and flow rates. A value of p < .05 was regarded as statistically significant.
Results
The mean ± standard deviation (SD) of the extraction ratio for regadenoson ranged between 0.30 ± 0.08 and 0.32 ± 0.06 for the F8 hemodialyzer and 0.36 ± 0.09 and 0.41 ± 0.06 for the F160NR hemodialyzer (Table 1). The larger regadenoson molecule had a significantly smaller extraction ratio than urea and creatinine in all hemodialyzer types and flow settings (p < .001).
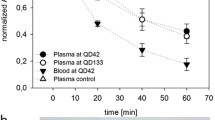
Observed regadenoson, urea, and creatinine transmembrane clearances are shown in Table 2. The mean CLD for regadenoson ranged between 62.5 ± 11.8 and 76.9 ± 19.7 mL/min for the F8 hemodialyzer and 75.1 ± 17.0-89.1 ± 24.0 mL/min for the F160NR hemodialyzer. Regadenoson clearance did not significantly change when Q b was increased from 300 to 400 mL/min with the F8 hemodialyzer (p = .12) or F160NR hemodialyzer (p = .22). There was no significant difference in regadenoson clearance between the two hemodialyzers at a Q b of 300 mL/min (p = .11) or 400 mL/min (p = .23) (Figure 1). Although urea and creatinine clearances could not be directly compared with values reported by the manufacturer due to varying flow rates and dialysis methods, results were consistent with expectations for the given conditions.18,19
Mean regadenoson transmembrane clearance for two hemodialyzers (F8 and F160NR) at blood flow rates of 300 and 400 mL/min. Error bars represent the standard deviation from the mean. There was no significant difference in regadenoson clearance between the two hemodialyzers and two blood flow rates (p > 0.05)
Discussion
Renal excretion is a major elimination pathway for regadenoson. Pharmacokinetic studies in subjects with renal impairment indicate regadenoson clearance decreases in parallel with a reduction in creatine clearance.7 Several studies have evaluated whether this reduced clearance adversely effects the safety profile and prognostic value of regadenoson in both dialysis-dependent and nondialysis patients with CKD. These studies have shown a generally favorable profile of regadenoson with an increased occurrence of headaches and gastrointestinal adverse effects,12-15,20 both of which were found to be effectively controlled with aminophylline, a nonselective adenosine receptor antagonist.16,17 Despite the abundance of these studies supporting its safe and effective use in patients with CKD on hemodialysis, no known studies have yet clarified whether regadenoson is actually removed by hemodialysis. In this study, we evaluated and assessed the effect of hemodialysis on the clearance of regadenoson. Results from this study indicate that regadenoson is cleared by hemodialysis at a rate of approximately 60-90 mL/min with hemodialyzer permeability (flux) and varying Q b of 300-400 mL/min having no significant effect on clearance. A previous pharmacokinetic study in subjects with severe renal impairment (creatinine clearance <30 mL/min) not on hemodialysis showed that the total body clearance of regadenoson (CLT) is approximately 250 mL/min, with nonrenal clearance (CLNR) accounting for the majority of this clearance at approximately 200 mL/min.7 Our findings indicate that hemodialysis would contribute approximately 30-45% to the overall regadenoson clearance, which would shorten the half-life by about 35%. When compared to the total clearance observed in patients with normal renal function (630 mL/min),6 it becomes evident that the additional clearance by hemodialysis is of relative insignificance (<25%). Typically, drug dosage adjustments are considered when extracorporeal clearance accounts for greater than 30% of total body clearance.21 However, due to its relatively limited clearance during hemodialysis and its relatively safe profile in CKD stage 5D, regadenoson dose adjustments in the dialysis-dependent population may not be warranted as hemodialysis will likely not have a substantial effect on the clinical outcome of a patient receiving regadenoson.
Many factors may affect the efficiency of hemodialysis and the removal of small solutes. A faster flow rate or a hemodialyzer with larger membrane pores will more efficiently clear solutes from blood and may significantly influence solute clearance. For this reason, regadenoson clearance was evaluated using two hemodialyzer types with varying membrane permeability and two common blood and dialysate flow rate pairs. The results reported here suggest that neither of these factors significantly influence regadenoson clearance. In the clinical setting, patient-specific factors such as residual renal function (RRF) and hemodialysis access recirculation may further influence regadenoson clearance. Although the additional clearance, if any, provided by RRF cannot easily be assessed, it would be expected to reduce the half-life to a value closer to that observed in patients with normal renal function and would not have any clinical implications. Recirculation, which occurs when some of the blood returning to the patient (postfilter) is immediately drawn back into the dialysis line (prefilter) without entering systemic circulation, may reduce the total amount of regadenoson removed without affecting the dialytic clearance.22 Any reduction in dialytic clearance due to recirculation would increase the half-life to a value closer to that observed in patients with CKD stage 5D, a population for which the safety and efficacy of regadenoson has already been established.11,13-17
There are several potential clinical applications of this new knowledge. First, although regadenoson may induce myocardial infarction and potentially fatal ventricular arrhythmias in rare cases,23-25 lesser degrees of myocardial ischemia may occur in response to regadenoson are not uncommon,26 particularly in patients with advanced coronary artery disease.27 While initial management generally includes medical therapies such as aminophylline, beta-adrenergic antagonists, and/or nitroglycerin, invasive management may also be required in some cases. These data suggest that there is no clinically relevant role for hemodialysis in cases of regadenoson induced myocardial ischemia, arrhythmia, or other severe side effects.
More commonly, clinicians are faced with uncertainty as to optimum timing of regadenoson stress in relation to hemodialysis. Many patients are relatively hypotensive after hemodialysis and may not tolerate vasodilator stress immediately afterward. Conversely, some laboratories have been hesitant to perform regadenoson stress on nondialysis days under the belief that regadenoson administration immediately prior to dialysis may limit potential adverse effects. These data suggest that timing of regadenoson stress in relation to dialysis can be safely liberalized.
Lastly, an analysis of the ASSUAGE trials suggested that patients with advanced renal disease may particularly benefit from aminophylline administration after regadenoson stress compared to those with preserved renal function.28 Unfortunately, aminophylline is contraindicated in patients with seizure disorder. In such patients, early dialysis is likely to have at most a modest effect on symptom control.
Strengths and Limitations
The in vitro study design we report in this paper allowed us to easily control for the many variables affecting dialytic clearance, including hemodialyzer type and flow rates. This allowed us to determine and compare the clearance of regadenoson under varying dialytic conditions that would otherwise be difficult to do in the clinical setting. This in vitro design has some important limitations as well. Since we used a hemodialysis model with whole human blood collected from relatively healthy patients supplemented with urea and creatinine, the findings reported here may not translate to patients with CKD stage 5D who have altered pharmacokinetics. However, similar in vitro hemodialysis models have been used for other drugs and found to be a good predictor of in vivo drug clearance.29-32
New Knowledge Gained
Regadenoson is a dialyzable solute that is removed by hemodialysis under common dialytic conditions, albeit at a rate much slower than the nonrenal clearance rate in patients with severe renal impairment. Therefore, hemodialysis is unlikely to hasten significantly the removal of regadenoson from the body.
Conclusion
Hemodialysis enhances the clearance of regadenoson independent of hemodialyzer permeability and blood/dialysate flow rate. This clearance is modest relative to total body clearance and is unlikely to produce a clinically significant outcome.
Abbreviations
- CAD:
-
Coronary artery disease
- MPI:
-
Myocardial perfusion imaging
- SPECT:
-
Single-photon emission computed tomography
References
Miller TD, Askew JW, Anavekar NS. Noninvasive stress testing for coronary artery disease. Cardiol Clin 2014;32:387-404.
Lexiscan prescribing information handbook. Lexiscan (regadenoson) prescribing package insert. Northbrook, IL: Astellas Pharma; 2014.
Buhr C, Gössl M, Erbel R, Eggebrecht H. Regadenoson in the detection of coronary artery disease. Vasc Health Risk Manag 2008;4:337-40.
Ananthasubramaniam K, Weiss R, McNutt B, Klauke B, Feaheny K, Bukofzer S. A randomized, double-blind, placebo-controlled study of the safety and tolerance of regadenoson in subjects with stage 3 or 4 chronic kidney disease. J Nucl Cardiol 2012;19:319-29.
Farhad H, Murthy VL. Pharmacologic manipulation of coronary vascular physiology for the evaluation of coronary artery disease. Pharmacol Ther 2013;140:121-32.
Gordi T, Frohna P, Sun HL, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet 2006;45:1201-12.
Gordi T, Blackburn B, Lieu H. Regadenoson pharmacokinetics and tolerability in subjects with impaired renal function. J Clin Pharmacol 2007;47:825-33.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 2003;108:2154-69.
United States Renal Data System. USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2015. p. 49-54.
Lentine KL, Costa SP, Weir MR, Robb JF, Fleisher LA, Kasiske BL, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol 2012;60:434-80.
Venkataraman R, Hage FG, Dorfman T, Heo J, Agel RA, de Mattos AM, et al. Role of myocardial perfusion imaging in patients with end-stage renal disease undergoing coronary angiography. Am J Cardiol 2008;102:1451-6.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0303-4.
AlJaroudi W, Hermann D, Hage F, Heo J, Iskandrian AE. Safety of regadenoson in patients with end-stage renal disease. Am J Cardiol 2010;105:133-5.
AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol 2016;23:560-9.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: The first prospective evaluation. J Nucl Cardiol 2013;20:205-13.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging “The ASSUAGE trial”. J Nucl Cardiol 2012;19:448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Marget B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease—the ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29:1029-37.
Fresenius Medical Care. Dialysers and filters product range. Waltham, MA: Fresenius Medical Care; 2007.
Fresenius Medical Care. Fresenius optiflux dialyzers. Waltham, MA: Fresenius Medical Care; 2011.
Palani G, Husain Z, Salinas RC, Karthikeyan V, Karthikeyan AS, Ananthasubramaniam K. Safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic kidney disease patients not on hemodialysis. J Nucl Cardiol 2011;18:605-11.
Levy G. Pharmacokinetics in renal disease. Am J Med 1977;62:461-5.
Tattersall JE, Chamney P, Aldridge C, Greenwood RN. Recirculation and the post-dialysis rebound. Nephrol Dial Transplant. 1996;11:75-80.
Hsi DH, Marreddy R, Moshiyakhov M, Luft U. Regadenoson induced acute ST-segment elevation myocardial infarction and multivessel coronary thrombosis. J Nucl Cardiol 2013;20:481-4.
Andrikopoulou E, Lloyd SG, Hage FG. Ventricular tachycardia during regadenoson SPECT myocardial perfusion imaging. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0339-5.
Rai M, Ahlberg AW, Marwell J, Chaudhary W, Savino JA 3rd, Alter EL, et al. Safety of vasodilator stress myocardial perfusion imaging in patients with elevated cardiac biomarkers. J Nucl Cardiol 2016. doi:10.1007/s12350-016-0448-9.
Johnson NP, Gould KL. Physiological basis for angina and ST-segment change PET-verified thresholds of quantitative stress myocardial perfusion and coronary flow reserve. JACC Cardiovasc Imaging 2011;4:990-8.
Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, et al. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med 2014;55:248-55.
Rangel MO, Morales Demori R, Voll ST, Wassouf M, Dick R, Doukky R. Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: A substudy of the ASSUAGE and ASSUAGE-CKD trials. J Nucl Cardiol 2015;22:1008-18.
Stevenson JM, Patel JH, Churchwell MD, Vilay AM, DePestel DD, Sörgel F, et al. Ertapenem clearance during modeled continuous renal replacement therapy. Int J Artif Organs 2008;31:1027-34.
Eyler RF, Vilay AM, Nader AM, Heung M, Pleva M, Sowinski KM, et al. Pharmacokinetics of ertapenem in critically ill patients receiving continuous venovenous hemodialysis or hemodiafiltration. Antimicrob Agents Chemother 2014;58:1320-6.
Churchwell MD, Pasko DA, Mueller BA. Daptomycin clearance during modeled continuous renal replacement therapy. Blood Purif 2006;24:548-54.
Vilay AM, Grio M, DePestel DD, Sowinski KM, Gao L, Heung M, et al. Daptomycin pharmacokinetics in critically ill patients receiving continuous venovenous hemodialysis. Crit Care Med 2011;39:19-25.
Acknowledgments
Dr Katherine Gharibian was an employee of the University of Michigan College of Pharmacy at the time this study was conducted. The authors would like to acknowledge the contributions of Weerachai Chaijamorn and Alexander Shaw in the conduct of this study.
Disclosure
The authors have no conflicts of interest to report.
Funding
This study was sponsored by Astellas Pharma Global Development, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gharibian, K.N., Murthy, V.L. & Mueller, B.A. Influence of hemodialysis on regadenoson clearance in an in vitro hemodialysis model. J. Nucl. Cardiol. 25, 234–239 (2018). https://doi.org/10.1007/s12350-016-0667-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0667-0