Abstract
Purpose of Review
Patients with end-stage renal disease (ESRD) have an increased risk of cardiovascular morbidity and mortality. Cardiac risk assessment, though challenging, is critical in these high-risk patients, particularly in the pre-transplant population. In this review, we discuss the burden of coronary artery disease in the ESRD population and review the literature on the diagnostic and prognostic performance, clinical value, and future directions of single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) in ESRD patients.
Recent Findings
Stress myocardial perfusion imaging provides incremental prognostic value to clinical data. The American Heart Association/American College of Cardiology Foundation consensus statement on the cardiac assessment of kidney transplant candidates provides some guidance on the selection of asymptomatic patients for further non-invasive risk stratification. Additionally, the novel selective A2A receptor-agonist vasodilator stress agent, regadenoson, is safe and effective in ESRD and has recently been approved by the Food and Drug Administration for use in this population. Ancillary stress MPI findings, namely heart rate response to vasodilator stress, can provide incremental risk stratification.
Summary
While myocardial perfusion imaging is widely used as a risk assessment tool, its utilization and clinical implications in the ESRD population are controversial. Though stress SPECT-MPI has imperfect diagnostic accuracy in this specific patient population, it is still a valuable non-invasive modality in cardiovascular risk assessment.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiovascular mortality accounts for more than 40% of deaths in patients with end-stage renal disease (ESRD) [1, 2]. Multiple prospective cohort studies have shown an inverse relationship between declining renal function and coronary artery disease (CAD) risk in patients with advanced (stages 3–5) chronic kidney disease (CKD) and those on dialysis. ESRD patients have cardiovascular event rates that are three times higher than those with normal renal function [2, 3]. Furthermore, the presence of ESRD portends a worse short- and long-term prognosis for many common cardiovascular conditions. In particular, dialysis patients who present with acute coronary syndrome have a twofold higher incidence of in-hospital mortality and recurrent myocardial infarction compared with the non-dialysis population [4]. Consequently, CKD has been recognized as an independent risk factor for cardiovascular disease, and several professional societies, including the American College of Cardiology Foundation (ACCF) and American Heart Association (AHA), have accepted it as a coronary disease risk equivalent [5].
For ESRD patients who undergo renal transplantation, their high cardiovascular risk follows them into the post-transplant period. Almost half of the deaths occurring within 30 days post-transplant are due to acute myocardial infarctions [6]. Additionally, in patients with functioning allografts, cardiovascular death is the most common cause of mortality at all times after transplantation, occurring in 36% of patients within 10 years of transplantation [6].
Given the high cardiovascular risk associated with ESRD, enhanced risk stratification is greatly needed not only for general assessment of CAD in ESRD patients but also in asymptomatic patients who are being evaluated for kidney transplantation. The body of literature regarding the utility of single-photon emission computed tomography-myocardial perfusion imaging (SPECT-MPI) in this population is evolving. ESRD patients represent a special population in terms of underlying cardiovascular risk, challenges in SPECT-MPI performance and interpretation, and the role this stress modality plays in future risk prediction.
Cardiovascular Risk Stratification for ESRD Patients
The high cardiovascular disease risk in patients with ESRD has largely been attributed to shared traditional risk factors such as diabetes mellitus, hypertension, sedentary lifestyle, smoking, family history, and dyslipidemia; however, these risk factors do not fully account for the frequency and severity of cardiovascular events in ESRD patients. Non-traditional risk and exacerbating factors such as increased inflammatory markers, endothelial dysfunction, volume overload, abnormalities in mineral metabolism, anemia, oxidative stress, autonomic imbalance, and the state of undergoing peritoneal or hemodialysis have been identified as possibly creating a milieu which promotes accelerated atherogenesis and adverse outcomes in ESRD patients [2, 7,8,9]. Unfortunately, most CAD risk prediction tools, including Framingham, Adult Treatment Panel-III (ATP-III), and Atherosclerotic Cardiovascular Disease (ASCVD), do not account for the high event rates in ESRD patients and may underestimate risk by as much as 50% in this patient population [10, 11].
The inability of traditional risk assessment indices to accurately estimate risk in ESRD patients is particularly relevant in the evaluation of renal transplant candidates. Though renal transplant has the highest associated survival of all renal replacement therapies, transplant recipients still have a high mortality rate when compared to the general population [12]. Since available organs are greatly limited, it is imperative that the selection of candidates takes into account an accurate estimation of perioperative and long-term cardiovascular risk. However, using stress testing, including stress MPI, for CAD surveillance in asymptomatic ESRD patients being considered for kidney transplantation is controversial. Acknowledging this controversy and the fact that the perioperative guidelines for non-cardiac surgery are not adequate for this unique population, the AHA/ACCF put forth a consensus scientific statement on the evaluation and management of cardiac disease in transplant candidates [13••]. The AHA/ACCF statement proposed that non-invasive testing is “reasonable” in asymptomatic kidney transplant candidates with “multiple” risk factors (Class IIb—level of evidence C). Risk factors specifically proposed for this population include age >60 years, hypertension, diabetes, dyslipidemia, smoking, cardiovascular disease, dialysis >1 year, and left ventricular hypertrophy. The statement indicates that “the specific number of risk factors that should be used to prompt testing remains to be determined, but the committee considers ≥3 to be reasonable” [13••]. A recent study validated the risk factors proposed by the AHA/ACCF statement and confirmed that having three or more of these risk factors in asymptomatic kidney transplant candidates is associated with increased risk of obstructive CAD as well as post-operative and long-term major adverse cardiac events (MACE) following transplant. The study also confirmed that three or more of these risk factors is an effective threshold to use in order to derive a significant incremental predictive value from stress MPI in this population [14].
Selection of Stress Modality in ESRD
Cardiovascular testing in ESRD patients is challenging due to limitations of available imaging modalities. ESRD patients tend to have a high burden of coronary artery calcification which can cause significant artifact affecting interpretation of coronary computed tomographic angiography (CTA). Though the risk of contrast-induced nephropathy is an important consideration in CKD patients, including those in stage 5 (glomerular filtration rate <15 ml/min/1.73 m2), this risk is not as relevant in ESRD patients on dialysis. On the other hand, the risk of gadolinium toxicity causing nephrogenic systemic fibrosis does restrict the use of cardiac magnetic resonance perfusion imaging in this patient population.
In terms of provocative stress testing, a significant proportion of ESRD patients cannot exercise due to baseline poor functional capacity and mobility-limiting comorbid conditions, such as peripheral arterial disease or diabetic or uremic neuropathy. Additionally, the frequent comorbidity of uncontrolled hypertension (primary or secondary) can limit the ability to complete a maximal symptom-limited exercise stress test. Moreover, left ventricular hypertrophy is highly prevalent in this population due to underlying primary or secondary systemic hypertension, thus limiting the diagnostic utility of ST-segment changes in discerning stress-induced myocardial ischemia [15, 16].
Vasodilator and catecholamine pharmacologic stress agents are most widely used in this patient population; however, though their use is thought to be safe in ESRD patients, both have limitations. As with exercise, dobutamine use is frequently limited by a hypertensive response which can hinder administering doses necessary to achieve a target heart rate. Thus, vasodilator stress with adenosine receptor agonists is commonly used in the ESRD population [17]. Older vasodilator agents, such as adenosine and dipyridamole, are not renally metabolized and can be safely used in ESRD patients. In recent years, regadenoson, a novel A2A receptor-agonist vasodilator, has become the most commonly used pharmacologic stress agent in the USA owing to favorable tolerability, ease of use as a fixed-dose bolus injection, and safety profile in patients with reactive airway disease [18, 19]. However, regadenoson is predominantly cleared by the kidneys (57%), and its triphasic half-life as well as a 2-h terminal elimination phase results in ESRD patients having reduced clearance and longer exposure to the drug [20]. More recently, in an in vitro dialysis model, it has been shown that hemodialysis enhances the clearance of regadenoson. However, this clearance is modest relative to total body clearance and is unlikely to produce a clinically significant effect [21]. Nonetheless, retrospective and prospective studies have shown that, other than an increase in gastrointestinal side effects, regadenoson is safe and tolerable in patients with ESRD (Fig. 1) [22, 23••]. Moreover, regadenoson-related side effects, including gastrointestinal symptoms, can be avoided or abated with the use of low-dose (75 mg) intravenous aminophylline administered at least 90–120 s after stress radioisotope injection [24,25,26]. Administering aminophylline to prevent or treat regadenoson-related adverse effects has been shown to have no demonstrable effect on the burden of regadenoson-induced myocardial ischemia detected by SPECT-MPI [27]. Therefore, regadenoson is safe and generally well-tolerated in ESRD patients, and in January 2017, was approved by the Food and Drug Administration (FDA) for use in patients with ESRD [28].
Rates of adverse effects within 24 h of regadenoson use in ESRD patients versus controls. SPECT single-photon emission computed tomography, ESRD end-stage renal disease. Controls were patients with glomerular filtration rate >30 ml/min/1.73 m2. Reproduced from Doukky et al. J Nucl Cardiol. 2013;20(2):205–201, with permission [23]
Diagnostic Accuracy of SPECT-MPI in ESRD
Much of the data related to diagnostic performance of SPECT-MPI in ESRD comes from patients being evaluated for kidney transplantation. As shown in Table 1, pooled data from multiple small studies assessing the diagnostic accuracy of stress SPECT-MPI in ESRD patients undergoing kidney transplant evaluation showed 67% sensitivity and 77% specificity for detection of significant CAD, defined as ≥70% diameter stenosis [29,30,31,32,33,34,35,36]. In a study of 138 pre-transplant candidates and using a more lenient definition of significant CAD, defined as ≥50% diameter stenosis, Winther et al. found the sensitivity and specificity of SPECT-MPI to be 53% and 82%, respectively [37]. The reason for the relatively low diagnostic performance of SPECT-MPI in this population is multifold. First, ESRD patients have a predisposition for particular hemodynamic and anatomic abnormalities which could impair diagnostic accuracy. For instance, the presence of significant left ventricular hypertrophy can compromise the detection of small or mild perfusion defects, decreasing the sensitivity of SPECT-MPI [38]. Also, left ventricular hypertrophy and a large left ventricular cavity, due to a chronic volume overload state caused by systemic shunting by an arteriovenous fistula created for hemodialysis access, can increase attenuation defects in the inferior wall. Figure 2 illustrates an example of SPECT-MPI from a patient with ESRD on long-standing hemodialysis highlighting left ventricular hypertrophy, enlarged left ventricular cavity, and prominent inferior wall attenuation, but normal left ventricular ejection fraction and myocardial perfusion.
Normal SPECT myocardial perfusion imaging in a patient with ESRD undergoing a transplant evaluation. SSS summed stress score, SDS summed rest score, TID transient ischemic dilation, LVEF post-stress gated SPECT left ventricular ejection fraction, LVEDVi left ventricular end-diastolic volume indexed to the body surface area, LVM left ventricular mass, LVMi left ventricular mass index. Rest-vasodilator stress 99mTc-tetrofosmin SPECT myocardial perfusion imaging for pre-transplant evaluation of a 39-year-old African-American man with ESRD on hemodialysis; his electrocardiogram met criteria for left ventricular hypertrophy. As shown, myocardial perfusion and left ventricular systolic function were normal. Note left ventricular dilatation (LVEDVi = 84 ml/m2; normal is <75 ml/m2 for a male) and increased left ventricular mass index (LVMi = 119 g/m2; normal ≤115 g/m2 for a male). The visualized inferior wall defect was likely caused by diaphragmatic attenuation and/or left ventricular enlargement caused by systemic shunting (arterial-venous fistula used for dialysis). Reproduced from Parikh et al. J Nucl Cardiol. 2015 Apr;22(2):282–296, with permission [17].
A hypertensive response to stress can also result in transient ischemic dilatation and perfusion defects in the absence of epicardial coronary stenosis [39, 40]. Additionally, endothelial dysfunction in the absence of epicardial coronary disease, a well-described finding in diabetic patients with ESRD, could decrease the specificity of SPECT-MPI [41]. Moreover, volume overload may lead to elevated background activity from increased lung uptake of the radioisotope which may degrade image quality from decreased signal-to-noise ratio. Notably, most published reports describing the diagnostic performance of SPECT-MPI in the ESRD population are older studies, predating recent advancements in SPECT technology and the introduction of modern attenuation correction tools which may now mitigate some of these barriers to diagnostic accuracy. Hybrid imaging techniques, such as coronary CTA/SPECT, have been shown to enhance diagnostic performance beyond either modality alone in renal transplant patients [37]. While the advantage of positron emission tomography (PET) as compared to SPECT-MPI has been well documented in the general population [42], the diagnostic accuracy of PET-MPI specifically in ESRD patients has not been reported in the literature.
Prognostic Value of SPECT-MPI in ESRD
The prognostic value of SPECT-MPI in ESRD patients has been demonstrated in multiple investigations. Several studies have shown renal dysfunction to be an important independent risk predictor of MACE, and stress SPECT-MPI, with exercise or vasodilator stress agents, has proven to provide robust prognostication across the entire spectrum of renal function, including ESRD [43••, 44,45,46]. Hage et al. [45] retrospectively studied the prognostic performance of regadenoson SPECT-MPI in 1400 patients, 26% of whom had ESRD. Findings not only showed that regadenoson SPECT-MPI provides powerful prognostic information that can aid in clinical decision-making, but also the burden of perfusion deficit on MPI was a predictor of adverse cardiac events, independent of ESRD status and other clinical covariates [45]. Similarly, Hakeem et al. [43••] found that in patients (N = 1652) who underwent stress MPI (36% exercise, 63% adenosine), worsening renal function, including ESRD, and perfusion defect burden on MPI were found to be independent predictors as well as have an additive value in risk prediction of cardiac death and all-cause mortality.
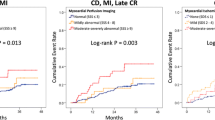
Though these investigations included ESRD patients, they did not exclusively study the value of SPECT-MPI in this specific patient population. There have been a few small studies which have looked into the value of SPECT-MPI in ESRD patients at the initiation of hemodialysis, and these studies have consistently shown the presence of myocardial perfusion defects to be an independent predictor of MACE [47,48,49]. Most existing data evaluating the prognostic performance of SPECT-MPI in ESRD patients are derived from investigations in those undergoing pre-transplant evaluation. Venkataraman et al. [50] demonstrated, in ESRD patients undergoing pre-transplant evaluation, a significant incremental prognostic value of dipyridamole stress SPECT-MPI, outperforming invasive coronary angiography data alone. More recently, in a prospective evaluation of 303 ESRD patients undergoing regadenoson SPECT-MPI, most of which were performed as part of a pre-transplant evaluation, worsening perfusion abnormalities and regadenoson-induced myocardial ischemia were associated with a stepwise increase in MACE rates (Fig. 3) [46]. Moreover, abnormal MPI and myocardial ischemia were associated with nearly twice the risk of MACE, even after adjusting for important clinical covariates [46].
Impact of regadenoson-induced perfusion abnormalities on cardiac outcomes in ESRD patients. The figure depicts Kaplan-Meier survival plots for cumulative event rates. ESRD end-stage renal disease, CD cardiac death, MI myocardial infarction, CR coronary revascularization, Late CR coronary revascularization occurring >90 days post-MPI, SSS summed stress score, SDS summed difference score. Reproduced from Doukky et al. J Nucl Cardiol 2015; DOI: 10.1007/s12350-015-0303-4 [46]
Notably, patients with normal MPI findings but with CKD, including ESRD, have been shown to have a significantly higher cardiac death rate than those with normal MPI and normal renal function (2.7 vs. 0.8% per year) [38]. Similarly, in an exclusive cohort of ESRD patients, the rate of cardiac death or MI in patients with a normal MPI was considerable at 4.9% per year [46]. This is certainly a deviation from the well-established low (<1%) annual MACE risk in patients with normal MPI reported in the general population [51, 52]. This is due to high baseline risk of MACE in the ESRD population, such that even those with normal MPI continue to have a relatively high risk in adherence with the principle of Bayes theorem. Elevated risk in patients with normal MPI has been demonstrated in other high-risk populations, such as those with known CAD, diabetics, the elderly, and patients unable to perform any level of exercise during stress MPI [53, 54]. Thus, ESRD patients who are at significant risk despite a normal exercise or vasodilator stress MPI may benefit from additional risk stratification derived from ancillary electrocardiographic or MPI findings such as heart rate response (HRR) to vasodilator stress and mechanical dyssynchrony.
Ancillary MPI Findings
Heart rate is expected to increase during vasodilator stress; HRR to stress is commonly calculated as [(peak heart rate − baseline heart rate) ÷ baseline heart rate] [55]. A blunted HRR to vasodilator stress (<28% for regadenoson and <20% for adenosine) during SPECT-MPI was shown to be a strong and independent predictor of death and cardiac events in ESRD patients [56, 57••]. Additionally, the integration of HRR and MPI findings improved risk stratification in a stepwise fashion, with a normal HRR and normal MPI identifying a truly low-risk group, while an abnormal HRR identified elevated risk even in patients with normal MPI, as shown in Fig. 4. These findings were consistent even after adjusting for relevant covariates [58]. In asymptomatic ESRD patients undergoing kidney transplant evaluation, the value of pre-transplant HRR in predicting perioperative and long term outcomes following kidney transplant needs to be investigated.
Impact of integrating HRR to regadenoson with MPI on adverse outcomes. Kaplan-Meier plots of cumulative event rates according to MPI and HRR MI, myocardial infarction. HR hazard ratio, CI confidence interval, MPI myocardial perfusion imaging. HRR heart rate response. Reproduced from Gomez et al. J Nucl Cardiol 2016; DOI: 10.1007/s12350-016-0497-0 [58].
Another emerging prognostic tool is left ventricular dyssynchrony by phase analysis of gated SPECT-MPI which, when studied in a cohort of pre-transplant ESRD patients, was shown to predict mortality independent of MPI abnormalities and left ventricular dysfunction [59, 60].
Serial Testing
While normal MPI in low-risk patients predicts low annual MACE rates for several years following MPI, high-risk patients, such as the elderly, patients with known CAD, diabetics, those undergoing vasodilator stress, and CKD/ESRD patients have been shown to have an accelerated increase in annual risk [38, 46, 53, 54]. In these populations, reassessment of risk with serial testing has been suggested, though controversial. In ESRD patients, ischemic symptoms may be confounded by symptoms which may be attributed to a state of chronic volume overload, such as decreased exercise tolerance and dyspnea on exertion; also, the frequent comorbidity of diabetes may result in “silent” ischemia or atypical symptoms. Moreover, multiple inflammatory factors and the altered hemodynamic state during hemodialysis and peritoneal dialysis can cause accelerated progression of CAD [61]. Therefore, the question has been posed as to whether surveillance ischemia evaluation would be beneficial in asymptomatic ESRD patients. This is particularly relevant to renal transplant candidates who have prolonged wait times for an organ (median 3.6 years). Considering that many of these patients have baseline high risk from multiple comorbidities combined with the risk of accelerated atherogenesis with maintenance dialysis, CAD severity may progress from their initial cardiovascular risk assessment to the time of organ availability [17]. Unfortunately, only a limited number of studies have addressed the utility of serial testing to better predict cardiovascular outcomes in this population.
El-Hajj et al. [62] investigated a cohort of high-risk patients (N = 698), 21% of whom had ESRD, and the indication for 20% of the initial MPI studies were pre-transplant or pre-operative evaluation. The authors found that changes in perfusion defect size and left ventricular ejection fraction (LVEF) in serial regadenoson MPI studies done within 16 ± 9 months provided incremental prognostic information [62]. Similarly, in a cohort of 656 asymptomatic ESRD patients who underwent two consecutive stress SPECT-MPI studies (mean interval 19 months), there was a stepwise increase in new or worsening MPI findings (increase in total perfusion deficit ≥5%) with prolonging time intervals between MPI studies. Moreover, an increase in total perfusion deficit by 5% or more was associated with the composite outcome of death or MI, irrespective of whether the initial MPI was normal or abnormal [63]. However, Gill et al. [64], who specifically studied ESRD patients awaiting renal transplantation (N = 604) in Canada, found that cardiovascular risk remained relatively unchanged over a 3-year period. Though cardiovascular risk did increase dramatically during the post-transplantation period, results of non-invasive testing prior to transplantation (mostly SPECT-MPI) were not predictive of post-operative cardiac events. Of note, the patient population was relatively young (48 ± 13 years) with relatively low rates of significant comorbidities (20% diabetes mellitus, 13% ischemic heart disease); therefore, these results may not be relevant in higher risk patients, particularly those “too sick” to be considered for transplantation [64]. Currently, the AHA/ACCF consensus statement states that the usefulness of periodically screening for myocardial ischemia in asymptomatic kidney transplantation candidates while on the transplant waiting list to reduce the risk of MACE is uncertain (Class IIb—level of evidence C) [13••]. Clearly, more research is needed in this domain.
Coronary Angiography
Acknowledging the lower diagnostic performance of non-invasive stress testing in ESRD patients, several studies have sought to answer the question as to whether coronary angiography would be a better predictor of cardiac events in certain high-risk subgroups of this population, particularly as it relates to post-transplant survival. De Lima et al. [30] studied moderate (age ≥50 years) or high-risk (presence of diabetes, angina, prior MI or stroke, left ventricular dysfunction, or extracardiac atherosclerosis) ESRD patients on dialysis (N = 126) who were renal transplant candidates. All patients underwent dipyridamole SPECT-MPI, dobutamine stress echocardiography, and coronary angiography. Not only did invasive testing have a higher diagnostic performance than non-invasive modalities, multivariate analysis showed that the sole predictor of cardiac events at a follow-up of 26 months was angiographic evidence of coronary stenosis ≥70% [30]. Based on these findings, Gowdak et al. [65] aimed to prospectively test certain high-risk clinical features to identify renal transplant candidates who may benefit from direct invasive coronary angiography rather than first undergoing non-invasive risk stratification. The presence of diabetes, peripheral arterial disease, and prior myocardial infarction were independently associated with angiographically significant CAD, and the composite incidence of fatal/nonfatal MACE increased almost twofold in patients with diabetes, fourfold in patients with peripheral arterial disease, and sixfold in patients with prior MI [65]. Recently, Mann et al. [66] studied high-risk renal transplant candidates (N = 225) defined by the presence of diabetes, known CAD, peripheral arterial disease, or ischemia on MPI. Coronary angiography revealed significant CAD in 47% of high-risk patients; furthermore, percutaneous or surgical revascularization in patients with ≥70% coronary stenosis resulted in reduced mortality both for those on the waiting list and for those who underwent renal transplantation [66].
While the findings in these studies suggest that coronary angiography in select, high-risk patients may provide a more accurate assessment of cardiac risk, results from other studies have failed to show benefit in a strategy of direct invasive testing. Hage et al. [67••] found that the presence and severity of angiographically defined CAD was not predictive of mortality in pre-transplant patients. Interestingly, in a recent study, De Lima et al. [68] found that while angiographically defined CAD identified patients at increased risk of post-transplant cardiac events, there was no difference in survival between patients with and those without significant CAD. Since these are observational non-controlled studies, the bias involved in selecting patients for coronary angiography and revascularization cannot be overstated. Only randomized, strategy-based clinical trials can adequately address the role of initial coronary angiography and revascularization.
Coronary Revascularization
While cardiovascular risk assessment strategies in ESRD patients and transplant candidates have been a focus of investigation, the inevitable questions follow—does coronary revascularization modify cardiovascular risk in ESRD patients? How should risk inform clinical decision-making, particularly when choosing candidates for renal transplantation?
When surgical or percutaneous coronary revascularization is indicated based on clinical practice guidelines, the outcomes for ESRD patients are associated with a more modest benefit and a higher complication rate than in patients with normal renal function [69].
Outcome studies on prophylactic coronary revascularization in the ESRD and pre-transplant population are scarce. In one study of high-risk, asymptomatic ESRD patients (N = 165) who underwent non-invasive cardiac risk stratification by stress MPI at the initiation of dialysis, revascularization failed to improve cardiac event-free survival at a follow-up of 47 months [47]. Similarly, outcomes for prophylactic revascularization in renal transplant candidates in several observational studies have not shown any survival benefit compared with those patients who do not undergo revascularization, except for significant left main or severe three-vessel CAD [67••, 70]. Alternatively, a single-center observational study of 657 transplant candidates found that patients with significant CAD who underwent revascularization followed by transplantation had a survival advantage over patients who declined revascularization. However, definitive conclusions cannot be drawn from this study due to confounding bias associated with selection to angiography and refusal of revascularization in a population perceived to be at high risk, thus selected for coronary angiography and recommended to have a revascularization [71].
In the absence of robust controlled prospective data evaluating the benefit of prophylactic revascularization in ESRD pre-transplant patients, conclusions can only be extrapolated from studies which have investigated a prophylactic revascularization strategy in other high-risk groups, such as patients with known CAD undergoing vascular surgery. Patients with asymptomatic ischemia do not appear to benefit from prophylactic pre-operative coronary revascularization in the absence of high-risk anatomy (significant left main disease or three-vessel disease with left ventricular dysfunction) in which revascularization may result in a survival advantage [72].
Future Directions
Considering the relatively limited diagnostic performance of SPECT-MPI in ESRD patients, there is scope for further investigation on optimizing risk assessment using modern imaging techniques and hybrid modalities. The role of PET-MPI, which has not been widely studied in the ESRD population, as well as enhancing diagnostic performance with hybrid modalities such as PET/CTA and SPECT/CTA are promising subjects of future studies. Moreover, improving clinical risk assessment in this population is also needed; as in any population, pre-test clinical assessment is paramount to identify appropriate candidates for MPI and determine post-test risk. Furthermore, currently available methods need to be built upon in order to better predict post-transplant survival. More data is needed to inform us of not only whether stress MPI is useful in diagnosis and risk stratification, but more importantly, whether it can guide decision-making in order to improve the outcome of ESRD patients, whether they undergo transplant or remain on maintenance dialysis therapy.
Conclusions
ESRD patients have a considerably increased risk of cardiac events including cardiovascular mortality compared to the general population; this fact is of particular significance in transplant candidates in the setting of scarcity of available organs. Stress MPI, particularly vasodilator stress, is well-suited to evaluate CAD in this population. The novel selective A2A receptor agonist vasodilator stress agent, regadenoson, is safe and effective in ESRD and is now FDA approved. Though stress SPECT-MPI has imperfect diagnostic accuracy in this specific patient population, it is still a valuable non-invasive modality in cardiovascular risk assessment. Moreover, ancillary stress MPI findings, namely HRR to vasodilator stress, can provide incremental risk stratification.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
USRDS. “Cardiovascular disease in patients with CKD.” 2016. https://www.usrds.org/2016/view/v1_04.aspx. Accessed 27 December 2016.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305.
Shroff GR, Frederick PD, Herzog CA. Renal failure and acute myocardial infarction: clinical characteristics in patients with advanced chronic kidney disease, on dialysis, and without chronic kidney disease. A collaborative project of the United States Renal Data System/National Institutes of Health and the National Registry of Myocardial Infarction. Am Heart J. 2012;163(3):399–406.
Gurm HS, Gore JM, Anderson Jr FA, Wyman A, Fox KA, Steg PG, et al. Comparison of acute coronary syndrome in patients receiving versus not receiving chronic dialysis (from the Global Registry Of Acute Coronary Events [GRACE] Registry). Am J Cardiol. 2012;109(1):19–25.
Briasoulis A, Bakris GL. Chronic kidney disease as a coronary artery disease risk equivalent. Curr Cardiol Rep. 2013;15(3):340.
Ojo AO, Hanson JA, Wolfe RA, Leichtman AB, Agodoa LY, Port FK. Long-term survival in renal transplant recipients with graft function. Kidney Int. 2000;57(1):307–13.
Miyamoto T, Carrero JJ, Stenvinkel P. Inflammation as a risk factor and target for therapy in chronic kidney disease. Curr Opin Nephrol Hypertens. 2011;20(6):662–8.
Bleyer AJ, Hartman J, Brannon PC, Reeves-Daniel A, Satko SG, Russell G. Characteristics of sudden death in hemodialysis patients. Kidney Int. 2006;69(12):2268–73.
Shlipak MG, Fried LF, Cushman M, Manolio TA, Peterson D, Stehman-Breen C, et al. Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. JAMA. 2005;293(14):1737–45.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS, et al. The Framingham predictive instrument in chronic kidney disease. J Am Coll Cardiol. 2007;50(3):217–24.
Arend SM, Mallat MJ, Westendorp RJ, van der Woude FJ, van Es LA. Patient survival after renal transplantation; more than 25 years follow-up. Nephrol Dial Transplant. 1997;12(8):1672–9.
•• Lentine KL, Costa SP, Weir MR, Robb JF, Fleisher LA, Kasiske BL, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation: endorsed by the American Society of Transplant Surgeons, American Society of Transplantation, and National Kidney Foundation. Circulation. 2012;126(5):617–63. The first of its kind, this AHA/ACCF consensus statement on the cardiac assessment of transplant candidates provides guidance on non-invasive risk stratification in this challenging population.
Doukky R, Fughhi I, Wassouf M, Vuj A, Campagnoli T, Kharouta M, et al. A clinical pathway to assess asymptomatic renal transplant candidates using myocardial perfusion imaging. J Nucl Cardiol. 2016;23(4):916–7. [Abstract 220-14]
Charytan D. Is left ventricular hypertrophy a modifiable risk factor in end-stage renal disease. Curr Opin Nephrol Hypertens. 2014;23(6):578–85.
Doukky R, Olusanya A, Vashistha R, Saini A, Fughhi I, Mansour K, et al. Diagnostic and prognostic significance of ischemic electrocardiographic changes with regadenoson-stress myocardial perfusion imaging. J Nucl Cardiol. 2015a;22(4):700–13.
Parikh K, Appis A, Doukky R. Cardiac imaging for the assessment of patients being evaluated for kidney or liver transplantation. J Nucl Cardiol. 2015;22(2):282–96.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol: Off Publ Am Soc Nuclear Cardiol. 2007;14(5):645–58.
Golzar Y, Doukky R. Regadenoson use in patients with chronic obstructive pulmonary disease: the state of current knowledge. Int J Chron Obstruct Pulmon Dis. 2014;9:129–37.
Gordi T, Blackburn B, Lieu H. Regadenoson pharmacokinetics and tolerability in subjects with impaired renal function. J Clin Pharmacol. 2007;47(7):825–33.
Gharibian KN, Murthy VL, Mueller BA. Influence of hemodialysis on regadenoson clearance in an in vitro hemodialysis model. J Nucl Cardiol. 2016; doi:10.1007/s12350-016-0667-0.
Aljaroudi W, Hermann D, Hage F, Heo J, Iskandrian AE. Safety of regadenoson in patients with end-stage renal disease. Am J Cardiol. 2010a;105(1):133–5.
•• Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: the first prospective evaluation. J Nucl Cardiol. 2013a;20(2):205–13. This was the first prospective study to confirm the safety and tolerability of regadenoson in patients with ESRD.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: a randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “the ASSUAGE trial”. J Nucl Cardiol. 2012;19(3):448–57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Margeta B. Attenuation of the side effect profile of regadenoson: a randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease—the ASSUAGE-CKD trial. Int J Cardiovasc Imaging. 2013b;29(5):1029–37.
Rangel MO, Morales Demori R, Voll ST, Wassouf M, Dick R, Doukky R. Severe chronic kidney disease as a predictor of benefit from aminophylline administration in patients undergoing regadenoson stress myocardial perfusion imaging: a substudy of the ASSUAGE and ASSUAGE-CKD trials. J Nucl Cardiol. 2015;22(5):1008–18.
Fughhi I, Campagnoli T, Ali A, Doukky R. Impact of a regimented aminophylline administration protocol on the burden of regadenoson-induced ischemia detected by SPECT myocardial perfusion imaging. J Nucl Cardiol. 2016; doi:10.1007/s12350-016-0506-3.
Ananthasubramaniam K, Weiss R, McNutt B, Klauke B, Feaheny K, Bukofzer S. A randomized, double-blind, placebo-controlled study of the safety and tolerance of regadenoson in subjects with stage 3 or 4 chronic kidney disease. J Nucl Cardiol. 19(2):319–29.
Boudreau RJ, Strony JT, duCret RP, Kuni CC, Wang Y, Wilson RF, et al. Perfusion thallium imaging of type I diabetes patients with end stage renal disease: comparison of oral and intravenous dipyridamole administration. Radiology. 1990;175(1):103–5.
De Lima JJ, Sabbaga E, Vieira ML, de Paula FJ, Ianhez LE, Krieger EM, et al. Coronary angiography is the best predictor of events in renal transplant candidates compared with noninvasive testing. Hypertension. 2003;42(3):263–8.
Garcia-Canton C, Culegras C, Hernandez-Briz MJ, Palomar R, Moreno A, et al. Dobutamine stress echocardiography and stress 99M-technetium methoxyisobutylisonitrile SPECT in the assessment of coronary artery disease in kidney transplant candidates [abstract]. Journal of the American Society of Nephrology : JASN. 1998;9:708A.
Gowdak LH DPF, De Oliveira AL, Arantes RL, Cesar LA, Ramires JA, et al. Non-invasive screening for coronary artery disease in renal transplant candidates with diabetes is influenced by gender. European Society of Cardiology. 2010; European Society of Cardiology Congress.
Marwick TH, Steinmuller DR, Underwood DA, Hobbs RE, Go RT, Swift C, et al. Ineffectiveness of dipyridamole SPECT thallium imaging as a screening technique for coronary artery disease in patients with end-stage renal failure. Transplantation. 1990;49(1):100–3.
Vandenberg BF, Rossen JD, Grover-McKay M, Shammas NW, Burns TL, Rezai K. Evaluation of diabetic patients for renal and pancreas transplantation: noninvasive screening for coronary artery disease using radionuclide methods. Transplantation. 1996;62(9):1230–5.
Worthley MI, Unger SA, Mathew TH, Russ GR, Horowitz JD. Usefulness of tachycardic-stress perfusion imaging to predict coronary artery disease in high-risk patients with chronic renal failure. Am J Cardiol. 2003;92(11):1318–20.
Wang LW, Fahim MA, Hayen A, Mitchell RL, Baines L, Lord S, et al. Cardiac testing for coronary artery disease in potential kidney transplant recipients. The Cochrane database of systematic reviews. 2011(12):Cd008691.
Winther S, Svensson M, Jorgensen HS, Bouchelouche K, Gormsen LC, Pedersen BB, et al. Diagnostic performance of coronary CT angiography and myocardial perfusion imaging in kidney transplantation candidates. JACC Cardiovasc Imaging. 2015;8(5):553–62.
Hakeem A, Bhatti S, Chang SM. Screening and risk stratification of coronary artery disease in end-stage renal disease. JACC Cardiovasc Imaging. 2014;7(7):715–28.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99m myocardial perfusion SPECT. J Nucl Cardiol. 2015;22(3):526–34.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: a cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol. 2013c;20(5):774–84.
Ragosta M, Samady H, Isaacs RB, Gimple LW, Sarembock IJ, Powers ER. Coronary flow reserve abnormalities in patients with diabetes mellitus who have end-stage renal disease and normal epicardial coronary arteries. Am Heart J. 2004;147(6):1017–23.
Mc Ardle BA, Dowsley TF, de Kemp RA, Wells GA, Beanlands RS. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease?: a systematic review and meta-analysis. J Am Coll Cardiol. 2012;60(18):1828–37.
•• Hakeem A, Bhatti S, Dillie KS, Cook JR, Samad Z, Roth-Cline MD, et al. Predictive value of myocardial perfusion single-photon emission computed tomography and the impact of renal function on cardiac death. Circulation. 2008;118(24):2540–9. This observational study showed that stress SPECT-MPI provides effective risk stratification across the spectrum of renal function; notably, CKD patients with a normal MPI had a worse prognosis when compared to patients with normal renal function and normal MPI.
Bhatti S, Hakeem A, Dhanalakota S, Palani G, Husain Z, Jacobsen G, et al. Prognostic value of regadenoson myocardial single-photon emission computed tomography in patients with different degrees of renal dysfunction. Eur Heart J Cardiovasc Imaging. 2014;15(8):933–40.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol. 2015;22(6):1214–21.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol. 2015b; doi:10.1007/s12350-015-0303-4.
Kim JK, Kim SG, Kim HJ, Song YR. Cardiac risk assessment by gated single-photon emission computed tomography in asymptomatic end-stage renal disease patients at the start of dialysis. J Nucl Cardiol. 2012;19(3):438–47.
Momose M, Babazono T, Kondo C, Kobayashi H, Nakajima T, Kusakabe K. Prognostic significance of stress myocardial ECG-gated perfusion imaging in asymptomatic patients with diabetic chronic kidney disease on initiation of haemodialysis. Eur J Nucl Med Mol Imaging. 2009;36(8):1315–21.
Hase H, Joki N, Ishikawa H, Fukuda H, Imamura Y, Saijyo T, et al. Prognostic value of stress myocardial perfusion imaging using adenosine triphosphate at the beginning of haemodialysis treatment in patients with end-stage renal disease. Nephrol Dial Transplant. 2004;19(5):1161–7.
Venkataraman R, Hage FG, Dorfman T, Heo J, Aqel RA, de Mattos AM, et al. Role of myocardial perfusion imaging in patients with end-stage renal disease undergoing coronary angiography. Am J Cardiol. 2008;102(11):1451–6.
Doukky R, Frogge N, Balakrishnan G, Hayes K, Collado FM, Rangel MO, et al. The prognostic value of cardiac SPECT performed at the primary care physician’s office. J Nucl Cardiol. 2013d;20(4):519–28.
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation. 2013e;128:1634–43.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol. 2003;41(8):1329–40.
Poulin MF, Alexander S, Doukky R. Prognostic implications of stress modality on mortality risk and cause of death in patients undergoing office-based SPECT myocardial perfusion imaging. J Nucl Cardiol. 2016;23(2):202–11.
Hage FG, Dean P, Iqbal F, Heo J, Iskandrian AE. A blunted heart rate response to regadenoson is an independent prognostic indicator in patients undergoing myocardial perfusion imaging. J Nucl Cardiol. 2011a;18(6):1086–94.
Hage FG, Dean P, Bhatia V, Iqbal F, Heo J, Iskandrian AE. The prognostic value of the heart rate response to adenosine in relation to diabetes mellitus and chronic kidney disease. Am Heart J. 2011b;162(2):356–62.
•• AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol. 2016;23(3):560–9. This prospective study showed that a blunted heart rate response (<28%) to regadenoson is a strong and independent predictor of death and cardiovascular events in patients with ESRD.
Gomez J, Fughhi I, Campagnoli T, Ali A, Doukky R. Impact of integrating heart rate response with perfusion imaging on the prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol. 2016; doi:10.1007/s12350-016-0497-0.
Aggarwal H, AlJaroudi WA, Mehta S, Mannon R, Heo J, Iskandrian AE, et al. The prognostic value of left ventricular mechanical dyssynchrony using gated myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol. 2014;21(4):739–46.
AlJaroudi W, Aggarwal H, Venkataraman R, Heo J, Iskandrian AE, Hage FG. Impact of left ventricular dyssynchrony by phase analysis on cardiovascular outcomes in patients with end-stage renal disease. J Nucl Cardiol. 2010b;17(6):1058–64.
Himmelfarb J, Stenvinkel P, Ikizler TA, Hakim RM. The elephant in uremia: oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int. 2002;62(5):1524–38.
El-Hajj S, AlJaroudi WA, Farag A, Bleich S, Manaoragada P, Iskandrian AE, et al. Effect of changes in perfusion defect size during serial regadenoson myocardial perfusion imaging on cardiovascular outcomes in high-risk patients. J Nucl Cardiol. 2016;23(1):101–12.
Anokwute C, Fughhi I, Wassouf M, Kharouta M, Campagnoli T, Vuj A, et al. The prognostic value of serial stress myocardial perfusion imaging in asymptomatic end-stage renal disease patients awaiting kidney transplantation [Abstract]. J Am Coll Cardiol. 2017; in press.
Gill JS, Ma I, Landsberg D, Johnson N, Levin A. Cardiovascular events and investigation in patients who are awaiting cadaveric kidney transplantation. J Am Soc Nephrol. 2005;16(3):808–16.
Gowdak LH, de Paula FJ, Cesar LA, Martinez Filho EE, Ianhez LE, Krieger EM, et al. Screening for significant coronary artery disease in high-risk renal transplant candidates. Coron Artery Dis. 2007;18(7):553–8.
Mann DM, Fernandez S, Mondal Z, Laskow D, Osband A, Debroy M, et al. Role of coronary angiography in the assessment of cardiovascular risk in kidney transplant candidates. Am J Cardiol. 2016;118(5):679–83.
•• Hage FG, Smalheiser S, Zoghbi GJ, Perry GJ, Deierhoi M, Warnock D, et al. Predictors of survival in patients with end-stage renal disease evaluated for kidney transplantation. Am J Cardiol. 2007;100(6):1020–5. This study showed that, in kidney transplant candidates, the presence and severity of CAD on coronary angiography was not predictive of survival; also, coronary revascularization did not alter survival except in patients with 3-vessel disease.
De Lima JJ, Gowdak LH, de Paula FJ, Muela HC, David-Neto E, Bortolotto LA. Coronary artery disease assessment and intervention in renal transplant patients: analysis from the KiHeart cohort. Transplantation. 2016;100(7):1580–7.
Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Thorac Cardiovasc Surg. 2012;143(1):4–34.
Patel RK, Mark PB, Johnston N, McGeoch R, Lindsay M, Kingsmore DB, et al. Prognostic value of cardiovascular screening in potential renal transplant recipients: a single-center prospective observational study. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2008;8(8):1673–83.
Kumar N, Baker CS, Chan K, Duncan N, Malik I, Frankel A, et al. Cardiac survival after pre-emptive coronary angiography in transplant patients and those awaiting transplantation. Clinical Journal of the American Society of Nephrology : CJASN. 2011;6(8):1912–9.
McFalls EOWH, Moritz T, Goldman S, Krupski W, Littooy F, Pierpont G, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351(27):2795–804.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rami Doukky served on an advisory board and receives research funding from Astellas Pharma Global Development (Northbrook, IL). Yasmeen Golzar has no conflict to report.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Topical Collection on Cardiac Nuclear Imaging
Rights and permissions
About this article
Cite this article
Golzar, Y., Doukky, R. Stress SPECT Myocardial Perfusion Imaging in End-Stage Renal Disease. Curr Cardiovasc Imaging Rep 10, 13 (2017). https://doi.org/10.1007/s12410-017-9409-1
Published:
DOI: https://doi.org/10.1007/s12410-017-9409-1