Abstract
Objective
The aim of this study was to evaluate the prognostic value of metabolic tumor volume (MTV) on pre-treatment F-18 fluorodeoxyglucose (FDG) PET/CT in patients with hepatocellular carcinoma (HCC).
Methods
A total of 59 HCC patients who underwent FDG PET/CT before transarterial chemoembolization (TACE) or transarterial chemotherapy infusion (TACI) were retrospectively enrolled. The region of interest was drawn in the HCC and normal liver tissue. MTV2SD, defined as the sum of the voxels with higher standardized uptake values (SUV) than the SUV of the 97.5th percentile of voxels of the normal liver for each patient, was calculated using an intensity–volume histogram (IVH). The ratio of the maximum SUV of the tumor to the mean SUV of normal liver (T max/L mean) was also calculated. The prognostic significance of MTV2SD and Tmax/Lmean for progression-free survival (PFS) and overall survival (OS) was evaluated along with other clinical factors.
Results
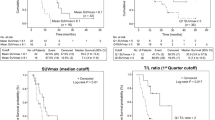
The tumor number, Tmax/Lmean, and MTV2SD were significant prognostic factors affecting PFS (p < 0.05), whereas tumor number, serum alpha-fetoprotein level, tumor stage, portal vein thrombosis, Tmax/Lmean, and MTV2SD were significant prognostic factors for OS (p < 0.05). In multivariate analysis, the tumor number and MTV2SD were independent prognostic factors for PFS (p < 0.05), whereas the independent prognostic factors for OS were tumor number, tumor stage, and MTV2SD (p < 0.05). The mean PFS and OS in patients with low MTV2SD (15.4 and 63.1 months, respectively) were significantly longer than those in patients with high MTV2SD (6.0 and 15.2 months, respectively; p = 0.005 and p < 0.0001, respectively).
Conclusions
Metabolic tumor volume was an independent prognostic factor for PFS and OS in patients with HCC. Therefore, FDG PET/CT can provide valuable prognostic information for HCC patients who undergo TACE or TACI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most frequently diagnosed cancer worldwide in men and the third most frequent cause of cancer-related death [1, 2]. Because most HCC patients are diagnosed at an intermediate-to-advanced stage, only 5–30 % of HCC patients undergo curative treatments such as surgical resection or liver transplantation [2]. For intermediate-to-advanced stage HCC patients without extrahepatic metastasis, transarterial chemoembolization (TACE) or transarterial chemotherapy infusion (TACI) has been used as a first-line therapy [2–4]. However, previous studies have shown diverse clinical outcomes after TACE or TACI [5–7]; hence, predicting clinical outcomes before treatment and selecting patients for whom TACE or TACI will provide long-term survival are important. Several clinicohistopathological factors including tumor stage, size, and number, the presence of portal vein thrombosis, extrahepatic metastasis, and the serum alpha-fetoprotein (AFP) level have been reported as significant factors for predicting clinical outcomes [3, 8–10].
Currently, F-18 fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) is widely used in various malignancies. Because of the variable FDG uptake of HCC and the relatively high uptake of normal liver tissue, the sensitivity of FDG PET for HCC is only 50–70 %, and the use of FDG PET/CT for diagnosis and staging in HCC is limited [2, 11–13]. Nevertheless, because the degree of FDG uptake in HCC lesions, which is expressed as the standardized uptake value (SUV) or tumor-to-liver uptake ratio, is related to tumor aggressiveness [13, 14], FDG uptake has been shown to be a significant predictor for tumor recurrence after surgical resection or liver transplantation [15, 16]. However, only a few studies have evaluated FDG uptake as a prognostic factor in HCC patients who underwent TACE or TACI [17, 18]. Furthermore, no study with HCC patients has assessed the prognostic value of volumetric parameters in FDG PET including metabolic tumor volume (MTV), which has been suggested to be a significant prognostic factor for other malignancies [19–21].
In the present study, we evaluated the prognostic value of MTV in pre-treatment FDG PET/CT and compared the predictive value of MTV with other conventional prognostic factors in HCC patients who underwent TACE or TACI. We also assessed the relationship between the time interval from treatment to disease progression and the pattern of disease progression and FDG PET/CT parameters in HCC patients who experienced disease progression.
Materials and methods
Patients
The Institutional Review Board of our medical center approved this retrospective study and the requirement to obtain informed consent was waived. The electronic medical records of 186 HCC patients who underwent pre-treatment FDG PET/CT and subsequent TACE or TACI between January 2008 and December 2011 were retrospectively reviewed. Among these patients, a total of 59 patients were enrolled in the present study. The following inclusion criteria were used: (1) confirmation of HCC diagnosis by histopathology or non-invasive diagnostic criteria of the American Association for the Study of Liver Disease guidelines; (2) absence of extrahepatic metastasis; (3) no treatment before the FDG PET/CT scan; (4) an Eastern Cooperative Oncology Group performance status of 0 or 1; and (5) a Child–Pugh class of A or B. Patients with a history of another malignancy and those with advanced liver disease were excluded from the study. The median interval between pre-treatment FDG PET/CT and TACE or TACI was 3.0 days (range 1.0–17.0 days). After TACE or TACI, all patients underwent clinical follow-up that included diagnostic imaging studies such as a contrast-enhanced liver CT scan, and measurement of the serum AFP level in every 3–6 months according to the clinical condition of the patients. The mean duration of clinical follow-up was 31.5 ± 23.8 months (range 4.7–96.5 months).
FDG PET/CT
All FDG PET/CT scans were performed using a dedicated PET/CT scanner (Gemini, Philips Medical Systems or Discovery STe, GE Healthcare). All patients fasted for at least 6 h prior to the PET/CT study. The PET/CT scan was performed 60 min after intravenous injection of FDG, and all patients revealed the blood glucose level of less than 150.0 mg/dL at the time of FDG injection. In patients who underwent PET/CT scanning with a Gemini scanner, 5.18 MBq/kg of FDG was injected, and for the Discovery STe, approximately 5.5 MBq/kg of FDG was administered. First, a low-dose CT scan for attenuation correction was obtained, followed by acquisition of emission images from the skull base to the mid-thigh in the 3D mode at 3 min per bed position for all PET/CT scanners. PET images were reconstructed iteratively with attenuation correction.
Image analysis
FDG PET parameters including the tumor-to-liver uptake ratio and MTV were calculated based on an intensity–volume histogram (IVH), which is represented in two forms, the cumulative IVH and the differential IVH [22, 23]. We used the cumulative IVH, which is a plot of the volume of a given structure as a function of the SUV that is equal to or higher than a certain value [23]. An example of the calculation of MTV is shown in Fig. 1. All FDG PET images were transferred using the Digital Imaging and Communications in Medicine protocol into the radiation therapy treatment planning software platform Computational Environment for Radiotherapy Research [22, 23]. Regions of interest (ROIs) were then manually drawn on the transaxial PET images that included the entire tumor lesions. In HCC lesions with low FDG uptake that were difficult to differentiate from the surrounding normal liver tissue, ROIs were drawn with careful correlation using contrast-enhanced liver CT and magnetic resonance imaging (MRI). Further, ROIs were drawn over normal liver tissue. Using ROIs of HCC lesions and normal liver tissue, cumulative IVHs of the HCC lesion and normal liver tissue were calculated (Fig. 1d), along with the maximum SUV of the tumor (Tmax), maximum SUV of normal liver tissue (Lmax), and mean SUV of normal liver tissue (Lmean). To calculate the MTV of HCC lesions, which is composed of only voxels with higher FDG uptake than normal liver tissue, two threshold values of normal liver tissue uptake were determined; one was Lmax, and the other was the SUV of the 97.5th percentile of the voxels of the normal liver tissue (L2SD), which is the SUV of the voxel that lies at a point of the mean plus two standard deviations (2SD) of the distribution of normal liver voxels. Using IVH, the MTV of HCC lesions which is defined as the sum of the voxels over the value of Lmax (MTVmax) or L2SD (MTV2SD) was calculated. The ratios of Tmax to Lmax (Tmax/Lmax), Tmax to L2SD (Tmax/L2SD), and Tmax to Lmean (Tmax/Lmean) were also calculated to represent the tumor-to-normal liver uptake ratio.
An example of the calculation of MTV based on IVH. On the maximum intensity projection (a), contrast-enhanced liver CT (b), and FDG PET (c) images of a 64-year-old man with a single HCC, the lesion shows moderately increased FDG uptake. The ROIs of the HCC (red) and normal liver tissue (blue) are manually outlined on the transaxial FDG PET images (d). The cumulative IVH plots for HCC (red) and normal liver tissue (blue) are shown in (e), and the left and right columns of the table show the ROI results of normal liver tissue and HCC, respectively. The SUV of the 97.5th percentile of the voxels of the normal liver tissue was 2.7 (blue box), and the fraction of the tumor volume with an SUV of 2.7 or more was 71.9 % (black box). Because the total tumor volume was 27.9 cm3 (red box), MTV2SD was 20.1 cm3 (color figure online)
Statistical analysis
The predictive values of five FDG PET/CT parameters (Tmax/Lmax, Tmax/L2SD, Tmax/Lmean, MTVmax, and MTV2SD) for progression-free survival (PFS) and overall survival (OS) were compared to conventional prognostic factors including age, sex, treatment modality, tumor number, tumor size, serum AFP, the Barcelona Clinic Liver Cancer (BCLC) stage, portal vein thrombosis, and the Child–Pugh class. For statistical analyses, all variables for survival analysis were classified into two categories, and the specific cut-off values for continuous variables were determined using receiver-operating characteristic (ROC) curve analysis. Kaplan–Meier survival analysis was performed to calculate cumulative PFS and OS rates according to the variables. The disease progression was defined as the progression of known HCC lesions or the occurrence of new intrahepatic or extrahepatic metastatic lesions on follow-up diagnostic studies. Survival time was defined as the time from TACE or TACI treatment to the date of the detection of progression of HCC (or death) or to the date of the last follow-up visit at our medical center. The significance of the predictive values of the variables was evaluated using a log-rank test in univariate analysis and using Cox proportional hazards regression test in multivariate analysis. In patients who experienced disease progression during follow-up, the correlations between FDG PET/CT parameters and the time interval from TACE or TACI treatment to progression of disease (time-to-progression) were evaluated by calculating Spearman’s rank correlation coefficient. Furthermore, the correlations between FDG PET/CT parameters and the pattern of HCC progression (intrahepatic progression and/or recurrence vs. extrahepatic metastasis) were evaluated using the Chi-square test and Fisher’s exact test. Statistical analyses were performed with SPSS 20.0 for Windows (SPSS Inc.) and p values <0.05 were considered statistically significant.
Results
Patient characteristics
The characteristics of the 59 enrolled patients are shown in Table 1. According to the BCLC staging classification, 24 patients (40.7 %) were classified as intermediate stage, and 20 patients (33.9 %) were classified as advanced stage because of the presence of portal vein thrombosis on pre-treatment imaging studies. The values of MTVmax and MTV2SD were 0.0 cm3 in five patients and one patient, respectively, because the value of Tmax was less than Lmax or L2SD. Of 59 patients, 45 (76.3 %) experienced progression of HCC, and 30 patients (50.1 %) died during follow-up. The median PFS time and OS time were 10.6 and 40.4 months, respectively. Among the 45 patients who experienced progression of HCC, 31 had intrahepatic recurrence or progression of HCC lesions, whereas the remaining 14 experienced extrahepatic metastasis.
Prognostic factors
Age, sex, treatment modality, tumor number, tumor size, serum AFP level, portal vein thrombosis, BCLC stage, Child–Pugh class, Tmax/Lmax, Tmax/L2SD, Tmax/Lmean, MTVmax, and MTV2SD were evaluated as variables in analysis of PFS and OS. For continuous variables, ROC curve analysis was performed to determine the optimal cut-off value. The cut-off values for age, tumor size, and serum AFP level were 60 years, 5.0 cm, and 400.0 ng/dL, respectively; the cut-off values for Tmax/Lmax, Tmax/L2SD, Tmax/Lmean, MTVmax, and MTV2SD were 1.2, 1.4, 1.5, 30 cm3, and 100 cm3, respectively. The significance of variables for predicting PFS and OS in univariate analysis is shown in Table 2. For PFS, tumor number, Tmax/Lmean (Fig. 2a), and MTV2SD (Fig. 2b) were significant predictive factors, and for OS, tumor number, serum AFP level, the presence of portal vein thrombosis, BCLC stage, Tmax/Lmean (Fig. 2c), MTVmax, and MTV2SD (Fig. 2d) were significant prognostic factors in univariate analysis. Among the variables evaluated in univariate analysis, those with a p value <0.05 were selected for multivariate analysis. Of the PET/CT parameters, Tmax/Lmean and MTV2SD, which showed the best predictive value among the tumor-to-liver uptake ratio and MTV, respectively, were selected for multivariate analysis. The results of multivariate analysis are shown in Table 3. For PFS, tumor number (p = 0.02) and MTV2SD (p = 0.04) were independent significant prognostic factors, and, for OS, tumor number (p = 0.005), BCLC stage (p = 0.01), and MTV2SD (p = 0.03) were significant.
Further subgroup survival analysis according to the BCLC stage (early-to-intermediate vs. advanced stage) was performed using MTV2SD, which was the only PET/CT parameter that showed statistical significance in multivariate analysis. With subgroup analysis, MTV2SD was also a significant predictive factor for OS, irrespective of BCLC stage (p = 0.009 for early-to-intermediate stage and p = 0.02 for advanced stage). For PFS, MTV2SD showed statistical significance in patients with early-to-intermediate stage HCC (p = 0.04); however, only borderline significance was shown in patients with advanced stage HCC (p = 0.08).
FDG uptake and time-to-progression and recurrence pattern
For the 45 patients who experienced progression of HCC, the relationship between Tmax/Lmean, MTV2SD, and time-to-progression was evaluated. We observed a significant inverse correlation between Tmax/Lmean and time-to-progression (p = 0.02, r = −0.344; Fig. 3a), showing that patients with high Tmax/Lmean had a shorter time-to-progression than patients with low Tmax/Lmean. In patients with Tmax/Lmean >4.0, all patients had disease progression less than 12 months after treatment. Borderline significance was shown between MTV2SD and time-to-progression (p = 0.06, r = −0.272; Fig. 3b).
The relationship among Tmax/Lmean, MTV2SD, and the pattern of progression of HCC (intrahepatic progression and/or recurrence vs. extrahepatic metastasis) was also evaluated in the 45 patients with progression (Table 4). We found no statistical difference in the frequency of extrahepatic metastasis according to Tmax/Lmean and MTV2SD (p > 0.05).
Discussion
To the best of our knowledge, this is the first clinical study to calculate MTV and assess the prognostic value of MTV derived from FDG PET/CT in HCC patients. Using the cumulative IVH, we calculated the volume of only tumor cells with higher FDG uptake than normal liver tissue. Our study demonstrated that the MTV of HCC is a significant independent prognostic factor for both PFS and OS.
Most previous studies evaluating MTV on FDG PET/CT used three methods for determining the threshold SUV to delineate metabolic tumor: (1) using a fixed threshold SUV such as 2.5 [21, 24] or 3.0 [25], (2) using a fixed ratio of Tmax as the threshold value, such as 40 % [26, 27] or 50 % of Tmax [28], or (3) using a threshold value of the mean plus 2SD of mediastinal blood pool SUV [19, 21]. However, for HCC patients, the high and variable FDG uptake of normal liver tissue prevents application of these three methods. Furthermore, because of heterogeneous and variable FDG uptake in HCC, accurately delineating HCC lesions from surrounding liver tissue is difficult. Hence, we devised a new method to measure the MTV of HCC using the IVH. The IVH was proposed as a novel method of characterizing intratumoral uptake heterogeneity [23, 29]. With the IVH, we used the personalized-threshold value, which was the SUV of the 97.5th percentile of the voxels of the normal liver tissue for each patient. Voxels with an SUV higher than the threshold value have a low chance of being normal liver tissue; hence, we could calculate the MTV of HCC consisting of voxels with higher FDG uptake than normal liver. MTV based on the personalized-threshold value using IVH was an independent prognostic factor.
The degree of FDG uptake has been widely used as an indicator of metabolic activity in many different malignancies. For HCC, the tumor-to-liver uptake ratio, especially the Tmax/Lmean, is an effective prognostic factor showing a more significant value than the SUV [16–18]. However, the tumor-to-liver uptake ratio represents only the point of the highest metabolic activity of the tumor and does not account for the tumor extent [30]. In contrast, MTV represents the extent of abnormally increased FDG uptake by tumor tissue beyond the intensity of FDG uptake in normal tissue [25]. In the present study, MTV2SD was composed of only voxels within the tumor that showed FDG uptake higher than that of normal liver tissue within the range of the mean plus 2SD. FDG uptake in HCC is positively related to tumor aggressiveness, and most well-to-moderately differentiated HCCs show an uptake of FDG similar to normal liver tissue, with a Tmax/Lmean <1.5, whereas most poorly differentiated HCCs show a Tmax/Lmean >2.0 [13, 31]. Thus, MTV2SD can be considered as the sum of the volume of tumor cells with aggressive features within the tumor and can be inferred as an indicator for prognosis. According our current results, MTV2SD was the only significant independent predictor among the FDG PET/CT parameters, and it had a higher predictive value than Tmax/Lmean. Additionally, MTV2SD showed statistical significance for OS in both patients with early-to-intermediate and advanced stages, indicating that further prognostic stratification can be made with MTV2SD, irrespective of the stage. For patients with high MTV, other intensive systemic treatment should be considered with or without local treatment, whereas long-term survival can be achieved by TACE or TACI in patients with low MTV. MTV on FDG PET/CT could guide the selection of HCC patients for TACE or TACI.
In the present study, although MTV2SD showed a more significant association with PFS and OS than Tmax/Lmean, the time interval between treatment and disease progression was significantly correlated with Tmax/Lmean. Because MTV2SD considers only the extent of tumor cells with increased metabolism, information about the intensity of FDG uptake, which reflects the intensity of glucose metabolism that is correlated with tumor aggressiveness [13, 14], is not included in MTV2SD. Tmax/Lmean, which represents the biological activity of the HCC, is correlated with time-to-progression. Therefore, additional treatment or close follow-up is needed in HCC patients with a high Tmax/Lmean.
We also assessed the relationship between FDG PET/CT parameters and the pattern of HCC progression. Because FDG uptake in HCC is related to tumor differentiation and poorly differentiated HCC tends to recur in extrahepatic sites [32], we hypothesized that HCC with high FDG uptake or MTV may tend to show extrahepatic metastasis. According to the results of our study, there was no statistical difference in the pattern of HCC progression according to FDG PET/CT parameters. However, because of the small number of patients in our study, further investigation is needed.
There are several limitations in our study. First, because of the retrospective nature of the study, selection bias is inevitable and the interpretation of the results could be limited. Second, although a recent study demonstrated comparable prognosis between TACI and TACE in intermediate-stage HCC patients [4], patients with heterogeneous clinical conditions were enrolled in the present study. Third, in patients with small HCC lesions, a partial-volume effect may have affected the FDG uptake, resulting in underestimation of MTV values. Furthermore, further study with more patients is needed to validate the IVH-based MTV measurement and compare with the conventional methods of MTV measurement. Finally, because the disease progression was retrospectively evaluated with diagnostic imaging studies, it might be underestimated in some of the patients.
In conclusion, using IVH, we measured the MTV of HCC lesions, which are composed of tumor cells with higher FDG uptake than normal liver tissue. In addition to tumor number and stage, MTV measured on pre-treatment FDG PET/CT is an independent significant prognostic factor for predicting PFS and OS in HCC patients who underwent TACE or TACI, and, showed a more significant association with PFS and OS than Tmax/Lmean. Furthermore, the time interval between treatment and disease progression can be predicted by the Tmax/Lmean of HCC lesions.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48:599–641.
Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30:61–74.
Nishikawa H, Osaki Y, Kita R, Kimura T, Ohara Y, Takeda H, et al. Comparison of transcatheter arterial chemoembolization and transcatheter arterial chemotherapy infusion for patients with intermediate-stage hepatocellular carcinoma. Oncol Rep. 2014;31:65–72.
Wang Y, Chen Y, Ge N, Zhang L, Xie X, Zhang J, et al. Prognostic significance of alpha-fetoprotein status in the outcome of hepatocellular carcinoma after treatment of transarterial chemoembolization. Ann Surg Oncol. 2012;19:3540–6.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003;37:429–42.
Takayasu K, Arii S, Ikai I, Kudo M, Matsuyama Y, Kojiro M, et al. Overall survival after transarterial lipiodol infusion chemotherapy with or without embolization for unresectable hepatocellular carcinoma: propensity score analysis. AJR Am J Roentgenol. 2010;194:830–7.
Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62–7.
Tateishi R, Yoshida H, Shiina S, Imamura H, Hasegawa K, Teratani T, et al. Proposal of a new prognostic model for hepatocellular carcinoma: an analysis of 403 patients. Gut. 2005;54:419–25.
Bonnetain F, Paoletti X, Collette S, Doffoel M, Bouche O, Raoul JL, et al. Quality of life as a prognostic factor of overall survival in patients with advanced hepatocellular carcinoma: results from two French clinical trials. Qual Life Res. 2008;17:831–43.
Trojan J, Schroeder O, Raedle J, Baum RP, Herrmann G, Jacobi V, et al. Fluorine-18 FDG positron emission tomography for imaging of hepatocellular carcinoma. Am J Gastroenterol. 1999;94:3314–9.
Torizuka T, Tamaki N, Inokuma T, Magata Y, Sasayama S, Yonekura Y, et al. In vivo assessment of glucose metabolism in hepatocellular carcinoma with FDG-PET. J Nucl Med. 1995;36:1811–7.
Khan MA, Combs CS, Brunt EM, Lowe VJ, Wolverson MK, Solomon H, et al. Positron emission tomography scanning in the evaluation of hepatocellular carcinoma. J Hepatol. 2000;32:792–7.
Shiomi S, Nishiguchi S, Ishizu H, Iwata Y, Sasaki N, Tamori A, et al. Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose for predicting outcome in patients with hepatocellular carcinoma. Am J Gastroenterol. 2001;96:1877–80.
Kitamura K, Hatano E, Higashi T, Seo S, Nakamoto Y, Yamanaka K, et al. Preoperative FDG-PET predicts recurrence patterns in hepatocellular carcinoma. Ann Surg Oncol. 2012;19:156–62.
Lee JW, Paeng JC, Kang KW, Kwon HW, Suh KS, Chung JK, et al. Prediction of tumor recurrence by 18F-FDG PET in liver transplantation for hepatocellular carcinoma. J Nucl Med. 2009;50:682–7.
Song MJ, Bae SH, Yoo Ie R, Park CH, Jang JW, Chun HJ, et al. Predictive value of (1)(8)F-fluorodeoxyglucose PET/CT for transarterial chemolipiodolization of hepatocellular carcinoma. World J Gastroenterol. 2012;18:3215–22.
Song MJ, Bae SH, Lee SW, Song do S, Kim HY, Yoo Ie R, et al. 18F-fluorodeoxyglucose PET/CT predicts tumour progression after transarterial chemoembolization in hepatocellular carcinoma. Eur J Nucl Med Mol Imaging. 2013;40:865–73.
Hyun SH, Choi JY, Kim K, Kim J, Shim YM, Um SW, et al. Volume-based parameters of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography improve outcome prediction in early-stage non-small cell lung cancer after surgical resection. Ann Surg. 2013;257:364–70.
Liao CY, Chen SW, Wu YC, Chen WT, Yen KY, Hsieh TC, et al. Correlations between 18F-FDG PET/CT parameters and pathological findings in patients with rectal cancer. Clin Nucl Med. 2014;39:e40–5.
Lee SJ, Choi JY, Lee HJ, Baek CH, Son YI, Hyun SH, et al. Prognostic value of volume-based (18)F-fluorodeoxyglucose PET/CT parameters in patients with clinically node-negative oral tongue squamous cell carcinoma. Korean J Radiol. 2012;13:752–9.
Deasy JO, Blanco AI, Clark VH. CERR: a computational environment for radiotherapy research. Med Phys. 2003;30:979–85.
El Naqa I, Grigsby P, Apte A, Kidd E, Donnelly E, Khullar D, et al. Exploring feature-based approaches in PET images for predicting cancer treatment outcomes. Pattern Recognit. 2009;42:1162–71.
Yoo SW, Kim J, Chong A, Kwon SY, Min JJ, Song HC, et al. Metabolic tumor volume measured by F-18 FDG PET/CT can further stratify the prognosis of patients with stage IV non-small cell lung cancer. Nucl Med Mol Imaging. 2012;46:286–93.
Oh JR, Seo JH, Chong A, Min JJ, Song HC, Kim YC, et al. Whole-body metabolic tumour volume of 18F-FDG PET/CT improves the prediction of prognosis in small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39:925–35.
Chung HH, Kwon HW, Kang KW, Park NH, Song YS, Chung JK, et al. Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis in patients with epithelial ovarian cancer. Ann Surg Oncol. 2012;19:1966–72.
Uto F, Shiba E, Onoue S, Yoshimura H, Takada M, Tsuji Y, et al. Phantom study on radiotherapy planning using PET/CT—delineation of GTV by evaluating SUV. J Radiat Res. 2010;51:157–64.
Yoon HJ, Paeng JC, Kwak C, Park YH, Kim TM, Lee SH, et al. Prognostic implication of extrarenal metabolic tumor burden in advanced renal cell carcinoma treated with targeted therapy after nephrectomy. Ann Nucl Med. 2013;27:748–55.
van Velden FH, Cheebsumon P, Yaqub M, Smit EF, Hoekstra OS, Lammertsma AA, et al. Evaluation of a cumulative SUV-volume histogram method for parameterizing heterogeneous intratumoural FDG uptake in non-small cell lung cancer PET studies. Eur J Nucl Med Mol Imaging. 2011;38:1636–47.
Fonti R, Larobina M, Del Vecchio S, De Luca S, Fabbricini R, Catalano L, et al. Metabolic tumor volume assessed by 18F-FDG PET/CT for the prediction of outcome in patients with multiple myeloma. J Nucl Med. 2012;53:1829–35.
Ho CL, Yu SC, Yeung DW. 11C-acetate PET imaging in hepatocellular carcinoma and other liver masses. J Nucl Med. 2003;44:213–21.
Sasaki K, Matsuda M, Ohkura Y, Kawamura Y, Inoue M, Hashimoto M, et al. In hepatocellular carcinomas, any proportion of poorly differentiated components is associated with poor prognosis after hepatectomy. World J Surg. 2014;38:1147–53.
Acknowledgments
This work was supported by research fund of Catholic Kwandong University International St. Mary’s Hospital.
Conflict of interest
No potential conflicts of interest were disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.W., Yun, M., Cho, A. et al. The predictive value of metabolic tumor volume on FDG PET/CT for transarterial chemoembolization and transarterial chemotherapy infusion in hepatocellular carcinoma patients without extrahepatic metastasis. Ann Nucl Med 29, 400–408 (2015). https://doi.org/10.1007/s12149-015-0956-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-015-0956-8