Abstract
Background and Aims
18F-fluorocholine positron emission tomography/computed tomography (18F-FCH PET/CT) is an emerging functional imaging technique in the diagnosis and management of hepatocellular carcinoma (HCC). The aim of this study was to assess the ability of a pre- and post-treatment 18F-FCH PET/CT to predict prognosis and treatment response in early-stage HCC.
Methods
Patients with early- or intermediate-stage HCC planned for locoregional therapy were prospectively enrolled. Baseline demographic and tumor information was collected and baseline and post-treatment 18F-FCH PET/CT performed. Maximum standardized uptake values (SUVmax) were determined for each HCC lesion, and the difference between baseline and post-treatment SUVmax values were compared with progression-free survival outcomes.
Results
A total of 29 patients with 39 confirmed HCC lesions were enrolled from a single clinical center. Patients were mostly men (89.7%) with hepatitis C or alcohol-related cirrhosis (65.5%) and early-stage disease (89.7%). Per-patient and per-lesion sensitivity of 18F-FCH PET/CT was 72.4% and 59.0%, respectively. A baseline SUVmax < 13 was associated with a superior median progression-free survival compared with an SUVmax of > 13 (17.7 vs. 5.1 months; p = 0.006). A > 45% decrease in SUVmax between baseline and post-treatment 18F-FCH PET/CT (“responders”) was associated with a superior mean progression-free survival than a percentage decrease of < 45% (“non-responders,” 36.1 vs. 11.6 months; p = 0.034).
Conclusions
Baseline and post-treatment 18F-FCH PET/CT predicts outcomes in early-stage HCC undergoing locoregional therapy. This technique may identify patients with an objective response post-locoregional therapy who would benefit from further therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary liver cancer, of which hepatocellular carcinoma (HCC) is the most common type, is responsible for the second greatest number of cancer deaths worldwide per year [1, 2]. Diagnosis and management are complex and require a multidisciplinary approach, multiple imaging and diagnostic techniques, and both locoregional and systemic therapies [3]. Despite many recent advances in the management of HCC, median survival remains between 9 and 12 months in developed nations [4,5,6], and less than 5% 5-year survival in the developing world [7].
Recent European Association for the Study of the Liver (EASL) guidelines have identified refinement of prognosis evaluation as an area for improvement in the management of HCC [8]. Well-established prognostic markers include both patient (performance status, Child–Pugh status) and tumor characteristics (size and number, degree of differentiation, vascular invasion, alpha fetoprotein level {AFP}). Tumor differentiation, presence of microvascular invasion, and AFP have an emerging role in selecting ideal patients for liver transplantation; however, they are limited due to the requirement for a liver biopsy and low sensitivity of AFP [9, 10]. Treatment response to both locoregional and systemic therapies is an important predictor of prognosis. The modified Response Evaluation Criteria in Solid Tumors (mRECIST) assessment tool has been developed specifically for use in HCC due to the unique response of these tumors to treatment [11]. A meta-analysis of seven trials assessing survival post-locoregional therapy for HCC confirmed that objective response by mRECIST (complete response or partial response) is a strong predictor of superior survival compared with non-response (stable disease or progressive disease) [12]. However, application of the mRECIST criteria may be challenging in certain groups such as heterogenous tumors and after selective internal radiotherapy (SIRT) [13, 14]. In addition, it requires longitudinal assessments, precluding it from stratifying treatment intensity.
Positron emission tomography/computed tomography (PET/CT), typically with 18F-fluorodeoxyglucose (18F-FDG), has wide oncological applications [15, 16] but has historically had a limited role in HCC owing primarily to its poor sensitivity [17, 18]. Routine clinical use of 18F-FDG PET/CT is not recommended in HCC guidelines [8], although it may be useful in selecting liver transplantation patients due to its ability to detect poorly differentiated tumors [19]. Alterations in choline metabolism are common in cancer, and associated enzymes have been proposed as novel targets for cancer therapy [20]. PET/CT with 18F-fluorocholine (18F-FCH) has demonstrated sensitivity approaching 90% in HCC [21, 22] and more recently been shown to accurately detect extrahepatic disease [23], and improve staging and treatment allocation [24]. It therefore represents an attractive imaging technique for further study in HCC.
The aims of this pilot study were to (1) assess the prognostic ability of baseline 18F-FCH PET/CT in early- and intermediate-stage HCC and (2) examine the utility of baseline and post-treatment 18F-FCH PET/CT in predicting treatment response by mRECIST criteria and progression-free survival following locoregional therapy.
Methods
Study Design and Patient Selection
We performed an investigator-driven, prospective, single-center, pilot study of the utility of 18F-FCH PET/CT in prognosis and treatment response prediction in early- or intermediate-stage HCC treated with locoregional therapy. The study was approved by the Sir Charles Gairdner Hospital Human Research Ethics Committee, and all enrolled patients provided written informed consent. Sir Charles Gairdner Hospital provides Western Australia’s only liver transplant service and is a quaternary referral center for the management of HCC. All patients with HCC are managed via a weekly multidisciplinary team meeting consisting of transplant hepatologists, interventional radiologists, radiation oncologists, and hepatobiliary and liver transplant surgeons. Patients with a new HCC, as defined by American Association for the Study of Liver Diseases (AASLD) radiological criteria [25], or with a histological confirmation of diagnosis were eligible for inclusion if they had early- or intermediate-stage disease as defined by the Barcelona Clinic Liver Cancer criteria (BCLC 0, A or B), had three or less lesions, were 18 years or over, were able to give written consent, and were planned for locoregional therapy (ablation, transarterial chemoembolization {TACE}, SIRT, or stereotactic body radiotherapy {SBRT; CyberKnife}). Patients with a history of HCC with recurrent disease were eligible if the original lesion(s) had ongoing evidence of complete devascularization and were remote from the new lesions. All patients had magnetic resonance imaging (MRI) at baseline and post-treatment. Staging CT of the thorax and a bone scan were also performed; confirmed metastatic disease was an exclusion criterion. All MR scans were performed on a 1.5T (Siemens Magnetom Aera) with diffusion-weighted spin echo planar, in- and out-of-phase gradient echo T1, ultra-fast spin echo T2, fat-suppressed T2-weighted, and volume-interpolated T1 gradient echo imaging before and following gadolinium (Gadovist) administration with timing for arterial, portal venous, and delayed phases at 3, 5, and 7 min. Response to treatment was assessed on post-treatment MR images using mRECIST criteria [11]. Baseline 18F-FCH PET/CT was performed within 4 weeks of the MRI scan. A prospectively planned two-stage recruitment was undertaken, with an initial cohort of patients in phase 1 having only baseline 18F-FCH PET/CT performed (15 of the eventual 29 total patients enrolled across both phases), with the aim of confirming 18F-FCH activity at sites of HCC. Subsequently, phase 2 of the study commenced, which involved patients undergoing both baseline and post-treatment 18F-FCH PET/CT (14 patients) performed within 1 week of the post-treatment MRI, which as per our institution protocol was 6 weeks after ablation, TACE, or SBRT and 12 weeks after SIRT. Patients from both phases 1 and 2 of the study were used for calculating sensitivity of baseline 18F-FCH PET/CT in diagnosing HCC. Baseline patient clinical and demographic data were collected, and HCC staging was performed using the BCLC classification. Patients undergoing ablation had a biopsy of the target lesion performed concurrently if possible. Treatment strategy was determined in the multidisciplinary team meeting. Patients were followed until death, liver transplant, or date of last clinic visit, whichever came first. Follow-up ceased at August 30, 2018. Overall survival was defined as time from treatment initiation to death from any cause. Time to site progression was defined as the time between treatment and disease recurrence or progressive disease at the site of treatment for each individual lesion (herein referred to as progression-free survival). Across the study period, approximately 200 patients who underwent locoregional therapy at our institution were screened and offered enrollment if they met inclusion criteria.
18F-FCH PET/CT Technique and Analysis
18F-FCH was synthesized in-house. No carrier-added 18F fluoride was produced by 18 MeV proton irradiation of 18O-enriched water using an IBA Cyclone 18/9 medical cyclotron (IBA Molecular). 18F-FCH was produced on a GE TRACERLab MX synthesizer (GE Healthcare), using commercial cassettes and reagents (ABX GmbH). Patients were fasted for 6 h and administered 4 MBq/kg of 18F-FCH intravenously 10 min prior to image acquisition on a Siemens Biograph 16 PET/CT camera (CTI Inc., Knoxville, TN). PET/CT images were acquired using 3D mode, with 6–7 bed positions at 3 min per bed position and covering a field of view of vertex to proximal thighs. A low-dose non-contrast CT was performed for anatomical localization and attenuation correction. PET, fusion PET/CT, and CT images were displayed in 5-mm slices. 18F-FCH PET/CT studies were read independently by two experienced nuclear medicine physicians who were aware of patient clinical history and correlative imaging. 18F-FCH PET/CT was considered visually positive when uptake in the HCC lesion was higher than background liver activity. Unexpected extrahepatic uptake was recorded and investigated with imaging and if required, with biopsy. If there was disagreement in PET/CT interpretation between the 2 physicians, a consensus reading was reached. Semi-quantitative analysis was undertaken by drawing a volume of interest (VOI) over the lesion using the PET manufacturer’s standard software (Siemens SyngoVia), to determine 18F-FCH maximum intensity of uptake (SUVmax). For the purpose of the second phase of the study, if a previously 18F-FCH PET/CT positive lesion was undetectable on the post-treatment scan then the SUVmax of that lesion was considered as zero.
Statistical Analysis
All statistical analysis was performed with SPSS version 25.0 (IBM Corporation, Armonk, NY). p < 0.05 was considered statistically significant. Categorical variables were presented as number (percentage) and continuous variables as median (minimum–maximum or 95% confidence interval {95% CI}). Sensitivity of 18F-FCH PET/CT to detect HCC compared to MRI or histology as the reference was calculated per patient and per lesion. Predictors of pre-treatment 18F-FCH PET/CT positivity were assessed by Fisher’s exact tests and Student’s t tests. Continuous variables were transformed into categorical variables based upon clinical significance, laboratory reference ranges, or medians. Univariate predictors of progression-free survival were compared by the Kaplan–Meier method followed by multivariable analysis using the Cox proportional hazard model.
Results
A total of 29 patients were enrolled across the study period from May 2013 to November 2016 (Fig. 1). Patient characteristics are presented in Table 1. Patients were mostly male (89.7%) with a median age of 62 years. The dominant underlying liver disease was hepatitis C and/or alcoholic cirrhosis (65.5%) followed by nonalcoholic liver disease (NAFLD) (20.7%). The majority of patients had well-compensated cirrhosis (Child–Pugh A, 89.0%) and early- (BCLC A, 89.7%) or intermediate-stage HCC (BCLC B, 10.3%), and all patients had good performance status (ECOG 0, 100.0%). Nineteen patients had one lesion, and 10 patients had two lesions making a total of 39 lesions with a median maximum diameter of 32 mm (range 10–140 mm). Seventeen (43.6%) lesions had tissue available for histopathological assessment. Sixteen of these lesions (94.1%) were well or moderately well differentiated, and only one was poorly differentiated. Just over half the patients underwent local ablation (51.7%) with the remainder being treated with SIRT (20.7%), TACE (13.8%), SBRT (6.9%) and ablation plus TACE (6.9%). Fourteen patients (48.3%) were enrolled in the second phase of the study and underwent both baseline and post-treatment 18F-FCH PET/CT. Ten patients died during the follow-up period, and 22 patients had progressive disease. Median overall survival was 35 months (95% CI 27.3–42.7 months), and median progression-free survival for the 39 lesions was 14.5 months (95% CI 10.0–19.0 months).
Study flowchart. Twenty-nine patients were enrolled in the study and underwent baseline 18F-FCH PET/CT prior to treatment commencing. Of these 29 patients, 14 patients underwent both baseline and post-treatment 18F-FCH PET/CT, and 3 of these patients had a negative baseline 18F-FCH PET/CT and were not included in the survival analyses. 18F-FCH PET/CT, 18F-fluorocholine positron emission tomography/computed tomography
Pre-treatment 18F-FCH PET/CT Sensitivity
Per-patient 18F-FCH PET/CT sensitivity in detection of HCC was 72.4% (21/29). In the remaining patients (8/29), 5 had HCC lesions with activity similar to background liver and 3 with activity lower than background liver. These lesions were considered 18F-FCH PET/CT negative as they could not be reliably identified or assessed for treatment response. In the per-lesion analysis, 23 of 39 lesions were positive on 18F-FCH PET/CT (sensitivity 59.0%). The only significant predictor of a positive pre-treatment 18F-FCH PET/CT on a per-lesion basis was AFP > 20 compared with AFP < 20 (p = 0.02). Of the 16 well or moderately well-differentiated tumors, 11 had a positive 18F-FCH PET/CT (68.8%) and 5 were negative (31.1%) (Table 2). There was no association between overall survival or progression-free survival and a positive pre-treatment 18F-FCH PET/CT. Two patients had unexpected extrahepatic activity at 18F-FCH PET which was not found to be metastatic HCC. One patient had an asymptomatic brain abscess identified with 18F-FCH PET/CT which was treated successfully with a craniotomy, evacuation of the abscess, and antibiotics [26], and one patient had a previously undetected small lung adenocarcinoma identified which was managed with a partial lobectomy. Both patients were alive and disease-free at the end of follow-up.
Baseline 18F-FCH PET/CT SUVmax and Progression-Free Survival Analysis
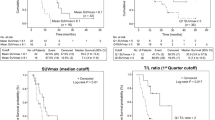
The impact of patient and tumor characteristics, and 18F-FCH PET/CT SUVmax on progression-free survival is presented in Table 3. Only those lesions which were 18F-FCH PET/CT positive were included in this analysis. The only significant predictors of poorer progression-free survival were larger lesion size (HR 1.02, 95% CI 1.01–1.02; p = 0.007), higher baseline 18F-FCH PET/CT SUVmax (HR 1.12, 95% CI 1.03–1.34; p = 0.02), and a trend toward higher baseline AFP (HR 1.001, 95% CI 1.000–1.002; p = 0.064). In the multivariable model, lesion size (p = 0.527) and baseline AFP (p = 0.873) were no longer significant, while there was a trend to significance of baseline 18F-FCH PET/CT SUVmax (HR 1.15 95% CI 0.98–1.36; p = 0.09). Median SUVmax was 9.6 (IQR 8.4–13.6). The impact of three cut points of the SUVmax (lower quartile, median, and upper quartile) on progression-free survival was explored. An SUVmax < 13 (equating to the upper quartile) was a significant predictor of a superior progression-free survival (17.7 months vs. 5.06 months, p = 0.006; Fig. 2) compared to SUVmax > 13. Predictors of SUVmax > 13 were a higher Model for End-Stage Liver Disease (MELD) (p = 0.037), higher AFP (p = 0.02), and a trend to larger lesion size (p = 0.076).
Progression-free survival by baseline 18F-FCH PET/CT SUVmax. A baseline 18F-FCH PET/CT SUVmax of < 13 (blue line) was associated with a superior progression-free survival than a 18F-FCH PET/CT SUVmax > 13 (red line) (17.7 months vs. 5.06 months, p = 0.006). Survival curves were estimated by the Kaplan–Meier method. 18F-FCH PET/CT, 18F-fluorocholine positron emission tomography/computed tomography; SUVmax, maximum standardized uptake values
Change in 18F-FCH PET/CT as a Predictor of Response and Progression-Free Survival
Of the 14 patients who underwent baseline and post-treatment 18F-FCH PET/CT in phase 2 of the study, 11 had a positive baseline 18F-FCH PET/CT. The baseline and post-treatment SUVmax values and percentage decrease in the SUVmax, baseline AFP, lesion size, treatment applied, and mRECIST outcomes are presented in Supplementary Table 1. There was a significant difference in mean progression-free survival (median unable to be calculated due to lack of events in responders) in those with a > 45% reduction in SUVmax (“responders”; representing median percentage decrease in SUVmax) compared to a < 45% reduction (“non-responders”; 36.1 vs. 11.6 months, p = 0.034) (Figs. 3, 4). All patients with a > 45% reduction in SUVmax had a complete response by mRECIST, and all patients with a < 45% reduction had either a partial response or stable disease.
Progression-free survival by percentage change in 18F-FCH PET/CT SUVmax between baseline and post-treatment. A percentage decrease in 18F-FCH PET/CT SUVmax of > 45% (red line) was associated with a superior progression-free survival than percentage decrease in 18F-FCH PET/CT SUVmax of < 45% (red line) (36.1 vs. 11.6 months, p = 0.034). Survival curves were estimated by the Kaplan–Meier method. 18F-FCH PET/CT, 18F-fluorocholine positron emission tomography/computed tomography; SUVmax, maximum standardized uptake values
Two examples of the use of baseline and post-treatment 18F-FCH PET/CT in treatment response prediction. Patient G was a 53-year-old male with a 34 mm HCC (a) treated with ablation followed by TACE the following day. Baseline 18F-FCH PET/CT SUVmax was 9.0 (c, e) which reduced by 80.2% to 1.8 post-treatment (d, f). By mRECIST, the patient was considered to have had a complete response (b) with eventual progression at the site 17.6 months later. Patient I was a 59-year-old male with a 50 mm HCC (g) treated with SIRT. Baseline 18F-FCH PET/CT SUVmax was 13.6 (i, k) which reduced by 44.4% to 7.6 post-treatment (j, l). Post-SIRT MRI was difficult to interpret due to typical post-SIRT changes, and it was thought the patient had a partial response by mRECIST (h) and the patient was placed into 3 monthly surveillances. Progression at the site was demonstrated on the following surveillance scan (5 months post-SIRT). This represents on example in which the use of a baseline and post-treatment 18F-FCH PET/CT may have changed treatment strategy (such as further locoregional therapy), despite the patient having an objective response by mRECIST. Red arrows indicated regions of interest. 18F-FCH PET/CT, 18F-fluorocholine positron emission tomography/computed tomography; SUVmax, maximum standardized uptake values; SIRT, selective internal radiotherapy; mRECIST, modified Response Evaluation Criteria in Solid Tumors. HCC, hepatocellular carcinoma
Discussion
We performed a pilot study exploring the utility of baseline and post-treatment 18F-FCH PET/CT to predict prognosis and provide treatment response information in early- and intermediate-stage HCC. 18F-FCH PET/CT has the potential to provide biological information on the status of an HCC lesion, information which cannot currently be provided by standard of care imaging modalities (CT and MRI), and which is currently limited to only one blood-based biomarker (AFP) or histopathological assessment, which requires a lesion biopsy with its own inherent risks. Our findings are novel and provide the impetus for further studies which may establish 18F-FCH PET/CT as a valuable tool in both prognostication and treatment response prediction.
We demonstrated an overall per-patient 18F-FCH PET/CT sensitivity of 72.4% which is slightly lower than recent studies with sensitivities up to 88% demonstrated [22,23,24]. However, we elected to label tumors with lower than background activity on 18F-FCH PET/CT as negative, whereas in recent studies, these were labeled positive. If we were to have included these lesions, the sensitivity would have been 82.8%; however, a more conservative approach was deemed to be more appropriate. For the full worth of the 18F-FCH PET/CT to be realized, an SUVmax must be able to be calculated which requires the lesion to exhibit higher than background liver activity, and thus, the per-patient sensitivity in our study was lower. A major and novel finding of our study was the correlation of baseline 18F-FCH PET/CT SUVmax with progression-free survival. We explored various cutoff values and identified an SUVmax of > 13 as highly predictive of a shorter progression-free survival compared with an SUVmax of < 13. Critically, in a multivariable model including traditional prognostic markers (AFP and lesion size), there was a trend to SUVmax being independently associated with prognosis (HR 1.15, 95% CI 0.98–1.36; p = 0.09), while AFP (p = 0.873) and lesion size (0.527) were both non-predictive. This finding implies that 18F-FCH PET/CT can provide additional prognostic information to traditional prognostic markers. It should be acknowledged that this pre-treatment variable is only able to be used in those with a positive pre-treatment 18F-FCH PET/CT which therefore reduces the overall power of the test. Being able to accurately and confidently predict outcomes is critical for choosing the appropriate treatments for the most appropriate candidates [8]. This is particularly important in selecting patients for liver transplantation where there is a move away from tumor size and number systems (such as the Milan [27] and UCSF criteria [28]), to those which incorporate other prognostic markers such as AFP and histopathological tumor features [9, 10]. A positive 18F-FCH PET/CT has previously been demonstrated to be associated with well to moderately well-differentiated tumors [21, 29], and thus, the incorporation of a 18F-FCH PET/CT into a liver transplant workup may obviate the need for a liver biopsy and help select the best candidates and will be an important area for future research.
A second novel and important finding was that a decrease in SUVmax between baseline and post-treatment 18F-FCH PET/CT predicted treatment response and correlated with progression-free survival. Responders, with a > 45% decrease in SUVmax post-treatment, had a superior progression-free survival (36.1 months) compared with non-responders, those with a < 45% decrease in SUVmax from baseline (11.6 months, p = 0.034). A preliminary study in six patients who underwent baseline and post-treatment 18F-FCH PET/CT found that treatment response using 18F-FCH PET/CT correlated with standard imaging in four cases, and demonstrated progressive disease which was not identified on standard imaging in one case and was discordant with standard imaging in the final case [23]. Our data built on these findings by correlating 18F-FCH PET/CT findings with mRECIST and progression-free survival, and suggest that this functional imaging technique may play a role in HCC treatment response prediction. The responder group consisted entirely of those with a complete response by mRECIST, while the non-responder group consisted of those with partial response and stable disease. Objective response in HCC is defined as those with a complete or partial response by mRECIST, correlates well with overall survival, and has been proposed as a surrogate endpoint in HCC trials [8, 30]. In two of the four patients who had a partial response post-treatment (technically an objective response by standard imaging, but demonstrating ongoing biological activity on 18F-FCH PET/CT), further locoregional therapy was not instituted until there was evidence of disease progression. Our data suggest that a subgroup of patients with an objective response may benefit from further treatment (either more locoregional therapy or systemic treatment) before waiting for disease progression if there is evidence of residual biological activity on 18F-FCH PET/CT. This may be particularly important in those treated with SIRT, as predicting tumor response by mRECIST is made difficult in post-treatment scans due to the effects of SIRT on surrounding tissue. In our cohort, of the 3 patients who were treated with SIRT and had a positive pre-treatment 18F-FCH PET/CT, 2 were labeled as a partial response and surveillance, as opposed to further imaging was commenced. In both cases, the change in 18F-FCH PET/CT was less than 45% and progression occurred within 6 months. If further treatment (either with locoregional or systemic therapy) was instituted, the patient outcomes may have been positively affected.
Altered choline metabolism has been demonstrated in almost all cancers studied; however, the exact mechanisms which lead to these alterations and whether these pathways are able to be altered, and affect outcomes, have yet to be determined [20]. Interestingly, a choline-deficient diet is a well-described model of murine liver injury and cancer development [31]. Despite this knowledge, further work is required to establish the exact link between HCC development and choline metabolism. Several other potential applications and areas for further investigation for functional imaging with 18F-FCH PET/CT in HCC merit discussion and include: (1) early treatment response assessment instead of the standard 6–12 weeks imaging after locoregional therapy; (2) identifying patients for adjuvant immunotherapy in the setting of a sub-optimal biological response to locoregional therapy (clinicaltrials.gov: NCT03383458); and (3) refining current response prediction, stopping and futility rules in patients treated with TACE [32, 33].
The study had several notable strengths, in particular the prospective enrollment of patients, a rigorously maintained patient database allowing accurate outcome assessment, and reading of all MRIs and PET/CT by two abdominal interventional radiologists (who were blinded to the PET/CT results) and two nuclear medicine physicians. Limitations of our study included its low number of patients, and thus, our findings must be replicated in a larger cohort. Additionally, only patients primarily with early-stage disease were included and further studies including more patients with intermediate and advanced disease are required. Our patient enrollment, while prospective, was non-consecutive as the availability of 18F-FCH was limited due to production requirements of other clinical PET tracers. The vast majority of tumors which had tissue available for histopathological assessment were either well or moderately well-differentiated (94.1%) due to the early-stage disease in the majority of our patients. The sensitivity of 18F-FCH PET/CT in these tumors was 68.8%. The lack of poorly differentiated tumors in the study cohort negated the inclusion of tumor differentiation in survival models. This lack of available histology is a common weakness of studies of PET/CT in HCC [24]. Finally, due to the lack of data in this area, the cut points of 18F-FCH PET/CT SUVmax were only identified by exploration of the data and not set before the study began and thus must be validated externally in further studies.
In conclusion, baseline and post-treatment 18F-FCH PET/CT provides important prognostic and treatment response prediction information in early-stage HCC patients treated with locoregional therapy. Potential applications of this functional imaging strategy are broad and should be examined in a multicenter, prospective fashion to confirm the usefulness of adding 18F-FCH PET/CT to the standard of care in HCC management.
Abbreviations
- 18F-FCH PET/CT:
-
18F-fluorocholine positron emission tomography/computed tomography
- HCC:
-
Hepatocellular carcinoma
- SUVmax:
-
Maximum standardized uptake values
- EASL:
-
European Association for the Study of the Liver
- AFP:
-
Alpha fetoprotein
- mRECIST:
-
Modified Response Evaluation Criteria in Solid Tumors
- SIRT:
-
Selective internal radiotherapy
- 18F-FDG:
-
18F-fluorodeoxyglucose
- AASLD:
-
American Association for the Study of Liver Diseases
- BCLC:
-
Barcelona Clinic Liver Cancer
- TACE:
-
Transarterial chemoembolization
- SBRT:
-
Stereotactic body radiotherapy
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- VOI:
-
Volume of interest
- 95% CI:
-
95% confidence interval
- NAFLD:
-
Nonalcoholic liver disease
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386.
Global Burden of Disease Liver Cancer. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol. 2017;3:1683–1691.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–1314.
Goutte N, Sogni P, Bendersky N, et al. Geographical variations in incidence, management and survival of hepatocellular carcinoma in a Western country. J Hepatol. 2017;66:537–544.
Njei B, Rotman Y, Ditah I, Lim JK. Emerging trends in hepatocellular carcinoma incidence and mortality. Hepatology. 2015;61:191–199.
Wallace MC, Preen DB, Short MW, Adams LA, Jeffrey GP. Hepatocellular carcinoma in Australia 1982 to 2014: increasing incidence and improving survival. Liver Int. 2018;39:522–530.
Wallace MC, Preen D, Jeffrey GP, Adams LA. The evolving epidemiology of hepatocellular carcinoma: a global perspective. Expert Rev Gastroenterol Hepatol. 2015;9:765–779.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Mehta N, Heimbach J, Harnois DM, et al. Validation of a risk estimation of tumor recurrence after transplant (RETREAT) score for hepatocellular carcinoma recurrence after liver transplant. JAMA Oncol. 2017;3:493–500.
Sapisochin G, Goldaracena N, Laurence JM, et al. The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: a prospective validation study. Hepatology. 2016;64:2077–2088.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30:52–60.
Vincenzi B, Di Maio M, Silletta M, et al. Prognostic relevance of objective response according to EASL criteria and mRECIST criteria in hepatocellular carcinoma patients treated with loco-regional therapies: a literature-based meta-analysis. PLoS One. 2015;10:e0133488.
Seyal AR, Gonzalez-Guindalini FD, Arslanoglu A, et al. Reproducibility of mRECIST in assessing response to transarterial radioembolization therapy in hepatocellular carcinoma. Hepatology. 2015;62:1111–1121.
Wang TH, Huang PI, Hu YW, et al. Combined Yttrium-90 microsphere selective internal radiation therapy and external beam radiotherapy in patients with hepatocellular carcinoma: from clinical aspects to dosimetry. PLoS One. 2018;13:e0190098.
Berriolo-Riedinger A, Becker S, Casasnovas O, Vander Borght T, Edeline V. Role of FDG PET-CT in the treatment management of Hodgkin lymphoma. Cancer Radiother. 2018;22:393–400.
Chowdhury FU, Bradley KM, Gleeson FV. The role of 18F-FDG PET/CT in the evaluation of oesophageal carcinoma. Clin Radiol. 2008;63:1297–1309.
Khan MA, Combs CS, Brunt EM, et al. Positron emission tomography scanning in the evaluation of hepatocellular carcinoma. J Hepatol. 2000;32:792–797.
Wu HB, Wang QS, Li BY, et al. F-18 FDG in conjunction with 11C-choline PET/CT in the diagnosis of hepatocellular carcinoma. Clin Nucl Med. 2011;36:1092–1097.
Hong G, Suh KS, Suh SW, et al. Alpha-fetoprotein and (18)F-FDG positron emission tomography predict tumor recurrence better than Milan criteria in living donor liver transplantation. J Hepatol. 2016;64:852–859.
Glunde K, Bhujwalla ZM, Ronen SM. Choline metabolism in malignant transformation. Nat Rev Cancer. 2011;11:835–848.
Bertagna F, Bertoli M, Bosio G, et al. Diagnostic role of radiolabelled choline PET or PET/CT in hepatocellular carcinoma: a systematic review and meta-analysis. Hepatol Int. 2014;8:493–500.
Talbot JN, Fartoux L, Balogova S, et al. Detection of hepatocellular carcinoma with PET/CT: a prospective comparison of 18F-fluorocholine and 18F-FDG in patients with cirrhosis or chronic liver disease. J Nucl Med. 2010;51:1699–1706.
Bieze M, Klumpen HJ, Verheij J, et al. Diagnostic accuracy of (18) F-methylcholine positron emission tomography/computed tomography for intra- and extrahepatic hepatocellular carcinoma. Hepatology. 2014;59:996–1006.
Chalaye J, Costentin CE, Luciani A, et al. Positron emission tomography/computed tomography with 18F-fluorocholine improve tumor staging and treatment allocation in patients with hepatocellular carcinoma. J Hepatol. 2018;69:336–344.
Bruix J, Sherman M. American association for the study of liver D management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022.
Hardy LE, Hessamodini H, Wallace M, Francis R. Is FCH PET able to identify foci of infection superiorly to FDG PET? BMJ Case Rep 2017; 2017.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699.
Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33:1394–1403.
Treglia G, Giovannini E, Di Franco D, et al. The role of positron emission tomography using carbon-11 and fluorine-18 choline in tumors other than prostate cancer: a systematic review. Ann Nucl Med. 2012;26:451–461.
Lencioni R, Montal R, Torres F, et al. Objective response by mRECIST as a predictor and potential surrogate end-point of overall survival in advanced HCC. J Hepatol. 2017;66:1166–1172.
Gogoi-Tiwari J, Kohn-Gaone J, Giles C, et al. The murine choline-deficient, ethionine-supplemented (CDE) diet model of chronic liver injury. J Vis Exp. 2017;128:e56138.
Raoul JL, Gilabert M, Piana G. How to define transarterial chemoembolization failure or refractoriness: a European perspective. Liver Cancer. 2014;3:119–124.
Sieghart W, Hucke F, Pinter M, et al. The ART of decision making: retreatment with transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology. 2013;57:2261–2273.
Acknowledgments
The authors would like to thank Elaine Campbell for her help with study management and data collection.
Funding
This study was funded in part by the Cancer and Palliative Care Research and Evaluation Unit Small Grants Scheme of the University of Western Australia and a research grant from the Australian and New Zealand Society of Nuclear Medicine. The sponsors had no role in the conduct of the research; study design; collection, analysis and interpretation of data; writing of the manuscript; or decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
They authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wallace, M.C., Sek, K., Francis, R.J. et al. Baseline and Post-treatment 18F-Fluorocholine PET/CT Predicts Outcomes in Hepatocellular Carcinoma Following Locoregional Therapy. Dig Dis Sci 65, 647–657 (2020). https://doi.org/10.1007/s10620-019-05781-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05781-6