Abstract
The systematic adoption of the histopathologic criteria provided by the 2016 update of the WHO classification of brain tumors has markedly increased the relative proportion of atypical and anaplastic meningiomas. These tumors exhibit a much greater recurrence rate compared to benign meningiomas, which negatively impacts survival. In recent years, the publication of numerous retrospective case series, yet no randomized controlled trials, on the impact of radiation therapy in non-benign meningioma, has yielded conflicting evidence. At present, maximum safe resection, including the dural attachment, is the preferred primary treatment modality for all types of meningiomas. Adjuvant radiotherapy is currently recommended for subtotally resected grade II and for all grade III meningiomas. However, in grade II meningiomas achieving complete resection, close radiologic and clinical observation is a feasible option. Despite the great amount of non-benign meningiomas available and eligible for trials, there is a striking lack of prospective studies testing adjuvant therapies against observation for this subset of patients. An updated and systematic literature review is provided on the effectiveness and indications of radiotherapy on grade II and III meningiomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningioma accounts for at least one-third of all primary intracranial neoplasms [1]. Overall incidence, about 6–7/100,000 persons [2], increases with age and prevalence estimations reach 2% of the population, acknowledging that many meningiomas are incidentally discovered thanks to neuroimaging [3, 4] or at autopsy [5]. The great majority of meningiomas are benign (grade I), yet with the potential for recurrence, even in the event of complete resection [6].
Atypical (grade II) and anaplastic (grade III or malignant) variants account for a variable percentage of all meningiomas depending on diagnostic criteria [7, 8]. The latest 2016 update of the World Health Organization (WHO) classification of central nervous system tumors maintained this 3-grade stratification of meningiomas (Table 1) based on specific histologic features [9]. Under previous classifications, atypical and anaplastic meningiomas comprised only 5–7% and 3–5% of all meningiomas, respectively [10, 11]. However, the systematic adoption of such newer criteria has increased the proportion of referred atypical meningiomas up to 20–35% [12, 13].
It is widely recognized that atypical and anaplastic meningiomas exhibit at least a 7- to eightfold increased risk of recurrence, and a marked increased risk of mortality, compared to benign meningiomas [13, 14]. As a general principle, maximum safe resection is the recommended primary treatment modality for all meningiomas [15]. However, at least one quarter to one-third of all meningiomas will eventually require adjuvant therapy, either after the first surgery or at the moment of recurrence [12, 13]. Therefore, it is important to confirm whether radiotherapy or other systemic therapies are clinically effective, especially among higher-grade tumors, and to identify what subset of patients benefit most.
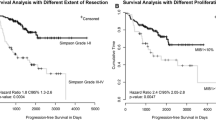
Age, grade, and extent of resection remain the most relevant prognostic factors related to meningioma patient’s survival [16, 17]. Currently, there is relative consensus that all anaplastic and subtotally resected (STR) atypical meningiomas should undergo adjuvant radiotherapy [18,19,20]. However, controversy remains on the optimal treatment of atypical meningiomas undergoing gross total resection (GTR) [12, 13, 19, 21]. At present, GTR is defined by most authors as macroscopically complete tumor removal with or without its dural attachment or underlying bone, that is, Simpson’s grades I, II, and III [22].
Previous systematic reviews have synthesized the evidence regarding the impact of radiotherapy on atypical and malignant meningiomas, showing and discussing some conflicting results among studies. Kaur et al. [21] and Hasan et al. [23] thoroughly reviewed grade II and III meningioma case series published before 2014. More recently, Pereira et al. [24] have summarized the effectiveness of radiotherapy in atypical meningiomas according to studies published up to October 2017. Strikingly, several dozens of additional case series and a few non-randomized trials have been published since then. An updated systematic review on the impact of adjuvant radiotherapy in atypical and anaplastic meningioma patients according to published studies from 2017 to date is presented.
Methods
Search strategy
A systematic review according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) guidelines was performed [25]. Studies were searched and retrieved from PubMed, SCOPUS, Cochrane Controlled of Register Trials, EMBASE, and clinicaltrials.gov databases. The search terms were as follows: meningioma, atypical, anaplastic, malignant, grade II, grade III, radiotherapy, radiation therapy, adjuvant, high grade, irradiation, radiation, resection, gross tumor resection, gross total resection, subtotal resection, postoperative, overall survival, progression-free survival, local control, progression, and recurrence. The search strategy included combinations of these key words with appropriate Boolean operators. References lists from relevant papers and related articles were also screened to make the search as comprehensive as possible. Papers published from 2017 and thereafter were gathered, and no language restriction was applied. The search was performed on April 10, 2020, by the two authors (PDL and ECG) independently, and discrepancies were solved by consensus.
Inclusion and exclusion criteria
All types of study (either observational or intervention studies) published within the last 4 years, that included a minimum of ten patients (either atypical and/or anaplastic meningiomas), were included. Studies on exclusively grade II meningiomas and studies on grade II–III and grade III meningiomas were analyzed, separately. Studies not strictly related to adjuvant radiotherapy in atypical or anaplastic meningioma patients were excluded. Review articles on radiotherapy techniques, chemotherapy or other systemic therapies, histologic features of atypical/malignant meningiomas, and studies in which the clinical course and outcome of patients [local control (LC), progression-free survival (PFS) or overall survival (OS)] were not available were also excluded (Fig. 1).
Data extraction
Information extracted from studies included first author, year of publication, study design, number of participants, histologic grade, number of irradiated patients, median follow-up, extent of resection, outcome regarding LC, PFS, or OS, limitations of the study, and main conclusions. Data on adverse effects related to radiotherapy was beyond the scope of this review and was not specifically addressed. Due to the paucity of prospective trials and the great heterogeneity among studies, a quantitative analysis on the effectiveness of adjuvant radiotherapy was not attempted.
Results
Study selection and main characteristics
Out of the initially screened 3726 studies, 90 were full-text reviewed for eligibility. After applying inclusion and exclusion criteria, 43 studies were finally included in the qualitative synthesis, 22 studies on exclusively atypical meningiomas [12, 13, 20, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44], and 21 studies on anaplastic or atypical/anaplastic series [19, 45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. The main characteristics of the studies are summarized in Table 2 for atypical meningiomas, and Table 3 for anaplastic and atypical/anaplastic meningiomas.
Regarding atypical meningiomas, 20 studies were retrospective cohorts (three multi-center studies) and two were prospective trials. The median number of participants per study was 140, and the median percentage of irradiated patients per cohort was 24.8%. The median follow-up period of studies was 52 months. The RTOG 0539, a non-randomized phase II trial [34] testing the efficacy of postoperative radiotherapy (either intensity-modulated radiotherapy (IMRT) or 3D conformal, 54 Gy in 30 fractions) among the so-called Group 2 or intermediate-risk meningiomas (atypical undergoing GTR and recurrent grade I with any extent of resection), provided results in terms of LC and PFS/OS at 3 years, which were compared with historical controls. The EORTC 22,042–26,042 trial [32], a multi-cohort non-randomized phase II trial, tested the efficacy of postoperative high-dose radiotherapy on PFS at 3 years among atypical and anaplastic meningiomas separately. The majority of patients enrolled were grade II meningiomas undergoing GTR. The objective of the study was to demonstrate that 3-year PFS among completely resected and irradiated grade II patients was higher than 70%.
In the group of studies including grade II and III or exclusively grade III meningiomas, 20 studies were retrospective case series (one multi-center study and five retrospective institutional database reviews) and one non-randomized prospective trial. The median number of participants per study was 60, and the median percentage of irradiated patients per cohort was 72.4%. The reported median follow-up period of studies was 48 months. The RTOG 0539 trial [46] conductors, which recently published the initial analysis of its high-risk cohort, recruited new or recurrent grade III meningiomas of any resection extent, recurrent grade II of any resection extent, and new grade II meningiomas after subtotal resection. Patients received IMRT (60 Gy high dose or 54 Gy low dose in 30 fractions) and PFS was assessed at 3 years.
Effectiveness of radiotherapy in grade II and grade III meningiomas
Among studies including exclusively grade II meningiomas, adjuvant postoperative radiotherapy was generally found beneficial for subtotally resected meningiomas in terms of LC, PFS, and OS [12, 13, 28, 30, 43]. In the case of GTR, the effect of radiotherapy was controversial, with few studies suggesting a clear benefit [29, 37, 39], the majority not confirming a clear influence on PFS or OS [13, 26, 27, 30, 33, 35, 36, 41, 43, 44], and even others suggesting a negative impact [40]. According to several studies, close observation of grade II meningiomas was considered a feasible option if they were completely resected [13, 27, 43, 44]. In general, a greater than 70% PFS rate at 3 years was expected following radiotherapy of grade II and completely resected meningiomas [32, 37]. The impact of radiotherapy on OS was not that clear, although some retrospective studies suggested a moderate or marginal beneficial effect [29, 30, 36, 39, 42, 43].
In general, authors do not recommend adjuvant radiotherapy as mandatory for grade II and GTR patients. In fact, close observation is a feasible and reasonable option, although it has been reported that salvage radiotherapy after re-intervention may not be as effective as early adjuvant radiation [34]. Patients considered of higher risk (advanced age, severe co-morbidities, tumors near critical structures, and lesions requiring large irradiation fields) are good candidates for observation. Likewise, lower-risk patients concerned about radiation-related toxicity can also be observed. Nevertheless, there seems to be relative consensus that local control is enhanced by postoperative adjuvant radiation in grade II meningiomas irrespective of resection extent [12, 34].
Regarding studies including grade II and III (15 studies) or exclusively grade III (6 studies) meningiomas, as expected, adjuvant radiotherapy was given to a larger proportion (near threefold) of patients compared to cohorts of solely grade II meningiomas. Among grade III meningioma patients, there was consensus on the beneficial effect of radiation on LC and PFS, and maybe on OS, irrespective of extent of resection [19, 45,46,47,48,49, 52, 54, 58, 59, 62,63,64]. Yet, adjuvant radiotherapy was found to have unclear or no impact on OS in some studies [50, 51, 56, 61]. Rhabdoid histology was reported to achieve better outcome after radiation in a multivariate analysis [58]. Among studies including both grade II and III meningiomas, the majority confirmed the efficacy of adjuvant radiation on LC, PFS, and likely OS, especially among subtotally resected tumors [19, 45,46,47,48, 52,53,54]. Less efficacy was reported regarding recurrent tumors, especially those located in the falx compared to convexity or skull base meningiomas [63]. Special radiation modalities, like proton therapy, brachytherapy, and boron neutron capture therapy, showed promising results, usually performed as re-irradiation or at the time of recurrence. However, these techniques reported non-negligible rates of radionecrosis and wound morbidity [55, 57, 60].
In general, it is widely accepted that grade III meningiomas need upfront postoperative radiotherapy regardless of the extent of resection. The majority of cohorts including both grades also showed benefit from adjuvant radiotherapy in terms of LC and PFS (although not so clear over OS), especially if performed immediately after the first operation. The impact of radiation at the time of recurrence seems to be less favorable and likely conditioned by the possibility of further resection. Figure 2 depicts a scheme of the current recommendations regarding grade II and III meningioma management according to the extent of resection.
Discussion
Since 2017, numerous grade II and III meningioma case series have been published, adding evidence toward the effectiveness of adjuvant radiation therapy in non-benign meningioma. Unfortunately, the great majority of studies were single-center retrospective cohort reviews. The synthesis of this systematic review confirms the usage and efficacy of adjuvant radiotherapy and underscores the need for prospective comparative trials. Atypical meningiomas can be cured by surgery only in 16–18% of the cases [24], and up to 70% recur within the next few months after surgery [65, 66]. Compared to benign meningiomas, atypical lesions carry a poorer overall prognosis, with 5- and 10-year PFS of 38–59% and 19–22%, respectively [12, 67], and a significantly reduced OS [65].
Application of adjuvant radiotherapy exhibits wide variability partly attributable to a lack of comparative prospective trials. Surveys among neurosurgeons indicate that a majority do not recommend routine adjuvant radiotherapy after GTR [18, 68]. The controversy about adjuvant radiotherapy in operated non-benign meningioma emanates from the conflicting evidence provided by many heterogeneous studies. Such studies commonly included a limited number of patients, the definition of atypical/anaplastic tumors evolved over time, many studies analyzed grade II and III lesions together, the definition of GTR also changed over time, and a certain selection bias (tendency to preferentially irradiate patients with poorer expected prognosis) was present in the majority of retrospective series [13, 69]. Likewise, radiation-related issues were not systematically reported in studies, like technique, dosage, scheme, field, target volume, and margins. In the recent review by Bagshaw et al. [12], adjuvant radiotherapy was offered to all atypical tumors irrespective of extent of resection upon recognizing that salvage treatments, either re-intervention or re-irradiation, do not seem to impact on survival significantly. They recommend relatively high doses of fractionated radiotherapy, at 59.4 Gy and 54 Gy, for STR and GTR, respectively, and single-dose 18–20 Gy if stereotactic radiosurgery is used.
In 2016, the European Association of Neuro-Oncology (EANO) issued guidelines for the diagnosis and treatment of meningiomas [70]. These were in concordance with previous recommendations, in which grade II tumors undergoing GTR could be observed, whereas grade II with STR and grade III should receive fractionated radiotherapy (54–60 Gy). For both grade II and III meningiomas, fractionated radiotherapy is generally preferred over stereotactic radiosurgery, which in turn might be better suited for primary treatment of small benign meningiomas or for small and deep-seated postoperative remnants. Surveillance of non-benign meningiomas require shorter control intervals compared to regular grade I lesions, therefore, repeating MRI every 3–6 months instead of annually. EANO guidelines adopted the definition of GTR as Simpson’s grades I, II, and III. Given the quality of studies supporting the use of adjuvant radiotherapy, all recommendations provided in the EANO guidelines statements were based on evidence level B, C, and good practice points.
In this view, the main issue to elucidate when confronting a high-grade meningioma is whether adjuvant therapy (primarily radiotherapy) should be proposed upfront or reserved for recurrence. Given that the extent of resection is a key prognostic factor, efforts should be made to achieve resections as complete as possible in the first surgery. Yet, it is common practice to observe grade I subtotally resected meningiomas, given that many residues remain unchanged over long periods of time, if not for life. In contrast, subtotally resected high-grade variants, generally due to involvement of vital structures or deeply located, tend to grow locally over time at a much higher speed, making further resections more complicated. These cases are commonly offered adjuvant therapy in the belief that local control is improved, and subsequently PFS and OS.
However, studies have yet failed to demonstrate a sound impact of adjuvant radiotherapy on OS likely attributable to the lack of randomized controlled trials on the matter [12, 13, 70]. It is striking that no such trials had been conducted so far given the enormous amount of eligible patients available worldwide and the conflicting evidence regarding its effectiveness among subgroups of meningiomas, stratified by prognostic factors, like age, grade, extent of resection, location, and histopathological subtypes. The latest WHO classification of meningiomas has transformed many previously considered grade I tumors into higher grades, merely upon histopathologic criteria [9]. In addition, historical surgical aggressiveness directed to deep-seated meningiomas, like cavernous sinus or petroclival region, has been revised given the intolerable surgical morbidity (especially cranial neuropathies) reported in some modern series [71,72,73]. These two factors have significantly increased the number of patients eligible for adjuvant radiation.
Only two prospective non-randomized trials have studied the effect of radiotherapy on non-benign meningiomas. The RTOG 0539 phase II trial [37] analyzed cohorts of intermediate risk (new grade II undergoing GTR or recurrent grade I) and high risk (grade III or new grade II undergoing STR or recurrent grade II). All patients received 54 Gy as adjuvant therapy. They reported a remarkable 3-year PFS of 93.8%. Interestingly, both subgroups within the intermediate risk achieved statistically similar PFS rates. Among high-risk patients, 3-year PFS, LC, and OS were 59.2%, 68.9%, and 78.6%, respectively. The EORTC 22,042–26,042 phase II trial included grade II and III meningiomas. Atypical lesions undergoing GTR and adjuvant radiotherapy (60 Gy) achieved a 3-year PFS and OS of 88.7% and 98.2%, respectively. However, none of these studies compared adjuvant radiotherapy against observation nor randomized patients to treatment and control arms.
The currently ongoing ROAM/EORTC 1308 phase III multi-center trial [69] was designed to randomize GTR atypical meningioma patients to either radiation (60 Gy in 30 fractions) or observation. This trial was intended to determine whether early adjuvant radiotherapy reduced the risk of tumor recurrence following GTR of atypical meningiomas. Embedded within this trial and pre-randomization, a qualitative study was performed [74], in which specific researchers examined how information about the trial is exchanged between physicians and patients during recruitment interviews and its influence on consent obtention. In a sub-sample of patients, they compared discussions during recruitment consultations with clinicians’ and patients’ interpretations of such consultations. This has been shown to be effective to improve patient and doctor acceptability and maximize recruitment [75]. In fact, this analysis identified several challenges that practitioners face in conveying equipoise, addressing difficulties with communication, and exploring patient treatment preferences, with potential impact on improving informed consent and recruitment. A second trial is also underway (phase III NRG-BN-003 trial or NCT 03,180,268), comparing radiation (59.4 Gy) versus observation in GTR patients [13]. Table 4 shows the main characteristics of both trials and the estimated completion date. These trials address a simple but important question about meningioma management, and their preliminary results, likely available in a few years from now, have the potential for changing the current neuro-oncologic practice worldwide. Other clinical trials have been recently activated or are currently recruiting patients in order to test the efficacy of carbon ion radiotherapy in atypical meningioma (NCT01166321), proton dose escalation in atypical and anaplastic meningiomas (NCT02978677), and the efficacy of postoperative radiotherapy for atypical meningiomas without venous sinus invasion after GTR (NCT04127760).
Radiation therapy modalities have not been compared between them in well-designed studies as to provide evidence of one treatment modality over the others. In general, higher doses (at least 54 Gy) seem to provide better overall outcomes [70]. According to the review by Hwang et al. [76], PFS was significantly higher when 60 Gy were given compared to lower doses, and when combined proton and photon irradiation was used [77]. Conventional fractionated external beam radiotherapy (typically using 1.8–2.0 Gy/fraction over 5- to 7-week course) benefits from the conformality of radiation dose delivery provided by intensity-modulated RT (IMRT) and volumetric arch therapy [78]. For grade II and III meningiomas, doses ranging between 60 and 66 Gy are typically used [21, 79]. Applied to skull base meningiomas, stereotactic radiotherapy with IMRT provides 3- and 5-year local control rates over 93%, although this technique is generally viewed as a second-tier option once surgery and/or conventional RT have failed [80]. Single fraction stereotactic radiosurgery (SRS) is an effective option for lesions < 10 cc, a maximum diameter less than 3–4 cm, and sufficient distance from critical structures [76]. According to Kano et al. [81], a marginal dose of 16–20 Gy associates a 5-year local control rate of 60–75%. Interestingly, the inclusion of the dural tail in the treatment volume has proven beneficial in benign meningioma but has not been yet studied in high-grade meningioma [76]. Likewise, hypofractionated stereotactic radiotherapy (five fractions or less), indicated for larger lesions, have yielded good results in benign meningioma but has not been studied in aggressive meningiomas [82, 83]. Interstitial brachytherapy has been reported to be an effective adjunct to surgery and external beam radiotherapy, especially for malignant, recurrent, and large meningiomas, yet associating over 25% rate of wound complications and radiation necrosis, many of which needed further surgery [84]. Salvage brachytherapy with I-125 or Cs-131 seeds, occasionally used in recurrent grade II–III meningiomas already re-operated and irradiated, has yielded a 40% need for reoperation due to wound complications [57]. Finally, heavy particle therapy with carbon ion radiotherapy offers the advantages of highly localized deposition of energy as in proton therapy, reduced cell cycle-dependent radiosensitivity, and increased efficacy for cancer stem-like cells [76]. The NCT01166321 phase II open-label trial (expected to be completed by December 2020) is currently recruiting patients with atypical meningiomas undergoing partial resection (Simpson 4 and 5) treated with carbon ion boost in combination photon radiotherapy.
As already standardized for glioma [9] or ependymoma [84], the eventual upcoming genetic- and molecular-based classification of meningiomas will likely introduce a new way of stratifying risk in meningioma, and may provide a surrogate prognostic factor of survival and recurrence.
Advances on the immunogenetic landscape of meningioma have been recently reviewed [85]. Using unsupervised clustering of DNA methylation data, Sahm et al. [86] were able to identify two major epigenetic patterns across the three grades of meningioma: group A, including four methylation classes (three benign and one intermediate), and group B which included two additional classes (one intermediate and one malignant). Interestingly, the majority of NF2 (Neurofibromatosis-2) gene-mutated tumors gathered in group A, and most TERT mutations in group B. This 6-methylation class subdivision predicted PFS better than the current WHO 15-histology variants and 3-grade classification [86]. Additionally, a meningioma recurrence score has been proposed, based on methylation status, extent of resection, and WHO grade which can be used in the clinical setting to inform choices for follow-up and to decide about adjuvant therapy [87]. However, meningioma is characterized by a relatively low mutational burden compared to other brain tumors; therefore, identification of prognostic biomarkers has yet provided modest clinical impact for decision making. In general, TERT promoter and BAP1 mutations are linked to poorer prognosis [85]. This molecular subgrouping may eventually simplify meningioma stratification and will necessarily need to be acknowledged when designing future trials.
Among unresectable meningiomas, in which tumor growth is confirmed, especially if suspicious of being high grade, upfront radiation or systemic therapy is mandatory [70]. A detailed description on the effectiveness of chemotherapy and other systemic therapies in non-benign meningioma is beyond the scope of this review and can be found elsewhere [88,89,90]. At the time of recurrence, if feasible, re-intervention is the first-choice irrespective of grade or previous extent of resection [12, 13, 24, 70]. Irradiation is the preferred modality when re-intervention is deemed not possible and for small deep tumor remnants. Salvage re-irradiation can also be an option. Studies show that PFS and OS are improved the longer the interval between prior radiotherapy and re-irradiation [13]. Although metastasis is rare and can occur throughout the natural course of any type of meningioma, including grade I lesions [91], it is much more common among higher-grade tumors [13, 70]. Anecdotally, the recent paper by Golub et al. [92] reports on a possible abscopal effect after IMRT treatment of an intracranial meningioma, with radiographically significant response of another untreated second intracranial lesion, distant to the radiation field, also suggestive of meningioma.
Conclusions
According to the recently updated WHO classification of central nervous system tumors, grade II and III meningiomas comprise a larger proportion of all meningiomas. Maximum safe resection including the dural attachment is the recommended first treatment option for all types of meningiomas. Atypical and anaplastic meningiomas carry a significantly increased recurrence rate compared to benign meningiomas, which negatively impacts survival. Adjuvant radiation is currently advised for subtotally resected grade II and for all grade III meningiomas. In the case of grade II meningiomas undergoing gross total resection, close radiologic and clinical observation is feasible. The potential benefit of adjuvant radiation in this subset of patients is currently being tested in ongoing clinical trials.
References
Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, Wolinsky Y, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro Oncol. 2013;15(2):1–56. https://doi.org/10.1093/neuonc/not151.
Dolecek TA, Dressler EV, Thakkar JP, Liu M, Al-Qaisi A, Villano JL. Epidemiology of meningiomas post-Public Law. The Benign Brain Tumor Cancer Registries Amendment. Act Cancer. 2015;121(14):2400–10. https://doi.org/10.1002/cncr.29379 (Epub 2015 Apr 14).
Kuratsu J, Kochi M, Ushio Y. Incidence and clinical features of asymptomatic meningiomas. J Neurosurg. 2000;92(5):766–70.
Håberg AK, Hammer TA, Kvistad KA, Rydland J, Müller TB, Eikenes L, et al. Incidental Intracranial Findings and Their Clinical Impact; the HUNT MRI study in a general population of 1006 participants between 50–66 Years. PLoS ONE. 2016;11(3):15–80.
Nakasu S, Hirano A, Shimura T, Llena JF. Incidental meningiomas in autopsy study. Surg Neurol. 1987;27(4):319–22.
Nakasu S, Fukami T, Jito J, Nozaki K. Recurrence and regrowth of benign meningiomas. Brain Tumor Pathol. 2009;26(2):69–72. https://doi.org/10.1007/s10014-009-0251-2.
Willis J, Smith C, Ironside JW, Erridge S, Whittle IR, Everington D. The accuracy of meningioma grading: a 10-year retrospective audit. Neuropathol Appl Neurobiol. 2005;31(2):141–9.
Pearson BE, Markert JM, Fisher WS, Guthrie BL, Fiveash JB, Palmer CA, et al. Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg Focus. 2008;24(5):E3. https://doi.org/10.3171/FOC/2008/24/5/E3.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 world health organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–20. https://doi.org/10.1007/s00401-016-1545-1 (Epub 2016 May 9).
Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM. Epidemiology of intracranial meningioma. Neurosurgery. 2005;57(6):1088–95.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109 .
Bagshaw HP, Burt LM, Jensen RL, Suneja G, Palmer CA, Couldwell WT, et al. Adjuvant radiotherapy for atypical meningiomas. J Neurosurg. 2017;126(6):1822–8. https://doi.org/10.3171/2016.5.JNS152809 (Epub 2016 Sep 9).
Zhi M, Girvigian MR, Miller MJ, Chen JC, Schumacher AJ, Rahimian J, et al. Long-term outcomes of newly diagnosed resected atypical meningiomas and the role of adjuvant radiotherapy. World Neurosurg. 2019;122:e1153–e1161161. https://doi.org/10.1016/j.wneu.2018.11.006 (Epub 2018 Nov 14).
Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J, et al. Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review J Neurosurg. 2015;122(1):4–23. https://doi.org/10.3171/2014.7.JNS131644.
Sun SQ, Hawasli AH, Huang J, Chicoine MR, Kim AH. An evidence-based treatment algorithm for the management of WHO Grade II and III meningiomas. Neurosurg Focus. 2015;38(3):E3. https://doi.org/10.3171/2015.1.FOCUS14757.
Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20(1):22–39.
Winther TL, Torp SH. Significance of the extent of resection in modern neurosurgical practice of world health organization grade I meningiomas. World Neurosurg. 2017;99:104–10. https://doi.org/10.1016/j.wneu.2016.11.034 (Epub 2016 Nov 17).
Marcus HJ, Price SJ, Wilby M, Santarius T, Kirollos RW. Radiotherapy as an adjuvant in the management of intracranial meningiomas: are we practising evidence-based medicine? Br J Neurosurg. 2008;22(4):520–8. https://doi.org/10.1080/02688690802308687.
Zhu H, Bi WL, Aizer A, Hua L, Tian M, Den J, et al. Efficacy of adjuvant radiotherapy for atypical and anaplastic meningioma. Cancer Med. 2019;8(1):13–20. https://doi.org/10.1002/cam4.1531.
Hemmati SM, Ghadjar P, Grün A, Badakhshi H, Zschaeck S, Senger C, et al. Adjuvant radiotherapy improves progression-free survival in intracranial atypical meningioma. Radiat Oncol. 2019;14(1):160. https://doi.org/10.1186/s13014-019-1368-z.
Kaur G, Sayegh ET, Larson A, Bloch O, Madden M, Sun MZ, et al. Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Neuro Oncol. 2014;16(5):628–36. https://doi.org/10.1093/neuonc/nou025 (Epub 2014 Apr 2).
Jenkinson MD, Waqar M, Farah JO, Farrell M, Barbagallo GM, McManus R, et al. Early adjuvant radiotherapy in the treatment of atypical meningioma. J Clin Neurosci. 2016;28:87–92. https://doi.org/10.1016/j.jocn.2015.09.021 (Epub 2016 Jan 8).
Hasan S, Young M, Albert T, Shah AH, Okoye C, Bregy A, et al. The role of adjuvant radiotherapy after gross total resection of atypical meningiomas. World Neurosurg. 2015;83(5):808–15. https://doi.org/10.1016/j.wneu.2014.12.037 (Epub 2014 Dec 19).
Pereira BJA, de Almeida AN, Paiva WS, Teixeira MJ, Marie SKN. Impact of radiotherapy in atypical meningioma recurrence: literature review. Neurosurg Rev. 2019;42(3):631–7. https://doi.org/10.1007/s10143-018-0959-8 (Epub 2018 Mar 19).
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;2(350):7647. https://doi.org/10.1136/bmj.g7647.
Keric N, Kalasauskas D, Freyschlag CF, Gempt J, Misch M, Poplawski A, et al. Impact of postoperative radiotherapy on recurrence of primary intracranial atypical meningiomas. J Neurooncol. 2020;146(2):347–55. https://doi.org/10.1007/s11060-019-03382-x (Epub 2020 Jan 3).
Poulen G, Vignes JR, Le Corre M, Loiseau H, Bauchet L. WHO grade II meningioma Epidemiology, survival and contribution of postoperative radiotherapy in a multicenter cohort of 88 patients. Neurochirurgie. 2020;4:28–37. https://doi.org/10.1016/j.neuchi.2019.12.008.
Wang F, Xu D, Liu Y, Lin Y, Wei Q, Gao Q, et al. Risk factors associated with postoperative recurrence in atypical intracranial meningioma: analysis of 263 cases at a single neurosurgical centre. Acta Neurochir (Wien). 2019;161(12):2563–70. https://doi.org/10.1007/s00701-019-04073-2 (Epub 2019 Oct 22).
Li H, Zhang YS, Zhang GB, Zhang GJ, Wang B, Li D, et al. Treatment protocol, long-term follow-up, and predictors of mortality in 302 cases of atypical meningioma. World Neurosurg. 2019;122:e1275–e12841284. https://doi.org/10.1016/j.wneu.2018.11.032 (Epub 2018 Nov 14).
Zeng Q, Shi F, Guo Z. Effectiveness of postoperative radiotherapy on atypical meningioma patients: a population-based study. Front Oncol. 2019;20:19–311. .
Zhang G, Zhang Y, Zhang G, Li D, Wu Z, Wang Y, et al. Outcome and prognostic factors for atypical meningiomas after first recurrence. J Clin Neurosci. 2019;63:100–5. https://doi.org/10.1016/j.jocn.2019.01.032 (Epub 2019 Feb 5).
Weber DC, Ares C, Villa S, Peerdeman SM, Renard L, Baumert BG, et al. Adjuvant postoperative high-dose radiotherapy for atypical and malignant meningioma: a phase-II parallel non-randomized and observation study (EORTC 22042–26042). Radiother Oncol. 2018;128(2):260–5. https://doi.org/10.1016/j.radonc.2018.06.018 (Epub 2018 Jun 28).
Liu X, Shan B, Wang M, Xu J. World Health Organization Grade II Meningiomas: the role of adjuvant/salvage gamma knife surgery after initial surgery and prognostic factor assessment. World Neurosurg. 2018;109:e352–e362362. https://doi.org/10.1016/j.wneu.2017.09.178 (Epub 2017 Oct 5).
Pant S, Tonse R, Kannan S, Moiyadi A, Shetty P, Epari S, et al. Impact of timing of radiation therapy on outcomes in atypical meningioma: a clinical audit. Pract Radiat Oncol. 2018;8(5):e275–e284284. https://doi.org/10.1016/j.prro.2018.01.010 (Epub 2018 Feb 4).
Masalha W, Heiland DH, Franco P, Delev D, Haaker JG, Schnell O, et al. Atypical meningioma: progression-free survival in 161 cases treated at our institution with surgery versus surgery and radiotherapy. J Neurooncol. 2018;136(1):147–54. https://doi.org/10.1007/s11060-017-2634-2 (Epub 2017 Oct 28).
Barthélemy E, Loewenstern J, Konuthula N, Pain M, Hall J, Govindaraj S, et al. Primary management of atypical meningioma: treatment patterns and survival outcomes by patient age. J Cancer Res Clin Oncol. 2018;144(5):969–78. https://doi.org/10.1007/s00432-018-2618-4 (Epub 2018 Mar 2).
Rogers L, Zhang P, Vogelbaum MA, Perry A, Ashby LS, Modi JM, et al. Intermediate-risk meningioma: initial outcomes from NRG Oncology RTOG 0539. J Neurosurg. 2018;129(1):35–47. https://doi.org/10.3171/2016.11.JNS161170 (Epub 2017 Oct 6).
Chen WC, Magill ST, Wu A, Vasudevan HN, Morin O, Aghi MK, et al. Histopathological features predictive of local control of atypical meningioma after surgery and adjuvant radiotherapy. J Neurosurg. 2018;130(2):443–50. https://doi.org/10.3171/2017.9.JNS171609.
Rydzewski NR, Lesniak MS, Chandler JP, Kalapurakal JA, Pollom E, Tate MC, et al. Gross total resection and adjuvant radiotherapy most significant predictors of improved survival in patients with atypical meningioma. Cancer. 2018;124(4):734–42. https://doi.org/10.1002/cncr.31088 (Epub 2017 Nov 13).
Budohoski KP, Clerkin J, Millward CP, O'Halloran PJ, Waqar M, Looby S, et al. Predictors of early progression of surgically treated atypical meningiomas. Acta Neurochir (Wien). 2018;160(9):1813–22. https://doi.org/10.1007/s00701-018-3593-x (Epub 2018 Jun 30).
Champeaux C, Houston D, Dunn L. Atypical meningioma A study on recurrence and disease-specific survival. Neurochirurgie. 2017;63(4):273–81. https://doi.org/10.1016/j.neuchi.2017.03.004 (Epub 2017 Sep 4).
Dohm A, McTyre ER, Chan MD, Fan C, Isom S, Bourland JD, et al. Early or late radiotherapy following gross or subtotal resection for atypical meningiomas: clinical outcomes and local control. J Clin Neurosci. 2017;46:90–8. https://doi.org/10.1016/j.jocn.2017.08.023 (Epub 2017 Sep 13).
Wang C, Kaprealian TB, Suh JH, Kubicky CD, Ciporen JN, Chen Y, et al. Overall survival benefit associated with adjuvant radiotherapy in WHO grade II meningioma. Neuro Oncol. 2017;19(9):1263–70. https://doi.org/10.1093/neuonc/nox007.
Graffeo CS, Leeper HE, Perry A, Uhm JH, Lachance DJ, Brown PD, et al. Revisiting adjuvant radiotherapy after gross total resection of World Health Organization Grade II meningioma. World Neurosurg. 2017;103:655–63. https://doi.org/10.1016/j.wneu.2017.04.095 (Epub 2017 Apr 24).
Kim M, Cho YH, Kim JH, Kim CJ, Roh SW, Kwon DH. Role of gamma knife radiosurgery for recurrent or residual World Health Organization grade II and III intracranial meningiomas. Br J Neurosurg. 2020;13:1–7. https://doi.org/10.1080/02688697.2020.1726285.
Rogers CL, Won M, Vogelbaum MA, Perry A, Ashby LS, Modi JM, et al. High-risk Meningioma: Initial Outcomes From NRG Oncology/RTOG 0539. Int J Radiat Oncol Biol Phys. 2020;106(4):790–9. https://doi.org/10.1016/j.ijrobp.2019.11.028 (Epub 2019 Nov 29).
Acker G, Meinert F, Conti A, Kufeld M, Jelgersma C, Nguyen P, et al. Image-guided robotic radiosurgery for treatment of recurrent grade II and III meningiomas. A Single Center Study World Neurosurg. 2019;131:e96–e107. https://doi.org/10.1016/j.wneu.2019.07.058 (Epub 2019 Jul 12).
Champeaux C, Jecko V, Houston D, Thorne L, Dunn L, Fersht N, et al. Malignant meningioma: an international multicentre retrospective study. Neurosurgery. 2019;85(3):E461–E469469. https://doi.org/10.1093/neuros/nyy610.
Masalha W, Heiland DH, Delev D, Fennell JT, Franco P, Scheiwe C, et al. Survival and prognostic predictors of anaplastic meningiomas. World Neurosurg. 2019;131:e321–e328328. https://doi.org/10.1016/j.wneu.2019.07.148 (Epub 2019 Jul 26).
Zhou H, Bai HX, Chan L, Zhang PJ, Karakousis G, Huang R, et al. Survival benefit of adjuvant radiotherapy in elderly patients with WHO grade III meningioma. World Neurosurg. 2019;131:e303–e311311. https://doi.org/10.1016/j.wneu.2019.07.140 (Epub 2019 Jul 26).
Alhourani A, Aljuboori Z, Yusuf M, Woo SY, Hattab EM, Andaluz N, et al. Management trends for anaplastic meningioma with adjuvant radiotherapy and predictors of long-term survival. Neurosurg Focus. 2019;46(6):E4. https://doi.org/10.3171/2019.3.FOCUS1960.
Lee JJB, Lee J, Yoon HI, Kim SH, Cho J, Lee KS, et al. Analysis of patterns of failure and appraisal of postoperative radiation field for grade II-III meningioma. J Neurooncol. 2019;144(2):333–41. https://doi.org/10.1007/s11060-019-03232-w (Epub 2019 Jul 5).
Boulle G, Bracci S, Hitchcock K, Jacob J, Clausse E, Halley A, et al. Treatment of grade II-III intracranial meningioma with helical tomotherapy. J Clin Neurosci. 2019;59:190–6. https://doi.org/10.1016/j.jocn.2018.10.073 (Epub 2018 Oct 24).
Li D, Jiang P, Xu S, Li C, Xi S, Zhang J, et al. Survival impacts of extent of resection and adjuvant radiotherapy for the modern management of high-grade meningiomas. J Neurooncol. 2019;145(1):125–34. https://doi.org/10.1007/s11060-019-03278-w (Epub 2019 Sep 6).
Imber BS, Neal B, Casey DL, Darwish H, Lin AL, Cahlon O, et al. Clinical outcomes of recurrent intracranial meningiomas treated with proton beam reirradiation. Int J Part Ther. 2019;5(4):11–22. https://doi.org/10.14338/IJPT-18-00045.1 (Epub 2019 May 1).
Jiang Y, Lv L, Li J, Ma W, Chen C, Zhou P, et al. Clinical features, radiological findings, and treatment outcomes of high-grade lateral ventricular meningiomas: a report of 26 cases. Neurosurg Rev. 2019;16:4. https://doi.org/10.1007/s10143-019-01078-4.
Koch MJ, Agarwalla P, Royce TJ, Shih HA, Oh K, Niemierko A, et al. Brachytherapy as an adjuvant for recurrent atypical and malignant meningiomas. Neurosurgery. 2019;85(5):E910–E916916. https://doi.org/10.1093/neuros/nyz115.
Zhang GJ, Zhang GB, Zhang YS, Li H, Li CB, Zhang LW, et al. World Health Organization Grade III (Nonanaplastic) Meningioma: experience in a series of 23 cases. World Neurosurg. 2018;112:e754–e762762. https://doi.org/10.1016/j.wneu.2018.01.149 (Epub 2018 Jan 31).
Chohan MO, Ryan CT, Singh R, Lanning RM, Reiner AS, Rosenblum MK, et al. Predictors of treatment response and survival outcomes in meningioma recurrence with atypical or anaplastic histology. Neurosurgery. 2018;82(6):824–32. https://doi.org/10.1093/neuros/nyx312.
Takeuchi K, Kawabata S, Hiramatsu R, Matsushita Y, Tanaka H, Sakurai Y, et al. Boron neutron capture therapy for high-grade skull-base meningioma. J Neurol Surg B Skull Base. 2018;79(Suppl 4):S322–S327327. https://doi.org/10.1055/s-0038-1666837 (Epub 2018 Jul 3).
Pereira BJA, de Almeida AN, de Aguiar PHP, Paiva WS, Cabrera HN, da Silva CC, et al. Atypical and malignant meningiomas: neurooncologic management in a brazilian cohort. World Neurosurg. 2018;110:e20–e2323. https://doi.org/10.1016/j.wneu.2017.09.172 (Epub 2017 Nov 28).
Garzon-Muvdi T, Yang W, Lim M, Brem H, Huang J. Atypical and anaplastic meningioma: outcomes in a population based study. J Neurooncol. 2017;133(2):321–30. https://doi.org/10.1007/s11060-017-2436-6 (Epub 2017 Apr 20).
Lubgan D, Rutzner S, Lambrecht U, Rössler K, Buchfelder M, Eyüpoglu I, et al. Stereotactic radiotherapy as primary definitive or postoperative treatment of intracranial meningioma of WHO grade II and III leads to better disease control than stereotactic radiotherapy of recurrent meningioma. J Neurooncol. 2017;134(2):407–16. https://doi.org/10.1007/s11060-017-2540-7 (Epub 2017 Jun 30).
Sumner WA, Amini A, Hankinson TC, Foreman NK, Gaspar LE, Kavanagh BD, et al. Survival benefit of postoperative radiation in papillary meningioma: analysis of the National Cancer Data Base. Rep Pract Oncol Radiother. 2017;22(6):495–501. https://doi.org/10.1016/j.rpor.2017.10.001 (Epub 2017 Oct 28).
Pisćević I, Villa A, Milićević M, Ilić R, Nikitović M, Cavallo LM, et al. The influence of adjuvant radiotherapy in atypical and anaplastic meningiomas: a series of 88 patients in a single institution. World Neurosurg. 2015;83(6):987–95. https://doi.org/10.1016/j.wneu.2015.02.021 (Epub 2015 Mar 11).
Cao X, Hao S, Wu Z, Wang L, Jia G, Zhang L, et al. Treatment response and prognosis after recurrence of atypical meningiomas. World Neurosurg. 2015;84(4):1014–9. https://doi.org/10.1016/j.wneu.2015.05.032 (Epub 2015 May 30).
Durand A, Labrousse F, Jouvet A, Bauchet L, Kalamaridès M, Menei P, et al. WHO grade II and III meningiomas: a study of prognostic factors. J Neurooncol. 2009;95(3):367–75. https://doi.org/10.1007/s11060-009-9934-0 (Epub 2009 Jun 27).
Simon M, Boström J, Koch P, Schramm J. Interinstitutional variance of postoperative radiotherapy and follow up for meningiomas in Germany: impact of changes of the WHO classification. J Neurol Neurosurg Psychiatry. 2006;77(6):767–73 .
Jenkinson MD, Javadpour M, Haylock BJ, Young B, Gillard H, Vinten J, et al. The ROAM/EORTC-1308 trial: radiation versus observation following surgical resection of atypical meningioma: study protocol for a randomised controlled trial. Trials. 2015;14(16):519. https://doi.org/10.1186/s13063-015-1040-3.
Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 2016;17(9):e383–e391391. https://doi.org/10.1016/S1470-2045(16)30321-7 (Epub 2016 Aug 30).
Gozal YM, Alzhrani G, Abou-Al-Shaar H, Azab MA, Walsh MT, Couldwell WT. Outcomes of decompressive surgery for cavernous sinus meningiomas: long-term follow-up in 50 patients. J Neurosurg. 2019;132(2):380–7. https://doi.org/10.3171/2018.10.JNS181480.
Nanda A, Thakur JD, Sonig A, Missios S. Microsurgical resectability, outcomes, and tumor control in meningiomas occupying the cavernous sinus. J Neurosurg. 2016;125(2):378–92. https://doi.org/10.3171/2015.3.JNS142494 (Epub 2016 Jan 8).
Dufour H, Muracciole X, Métellus P, Régis J, Chinot O, Grisoli F. Long-term tumor control and functional outcome in patients with cavernous sinus meningiomas treated by radiotherapy with or without previous surgery: is there an alternative to aggressive tumor removal? Neurosurgery. 2001;48(2):285–94.
Sherratt FC, Brown SL, Haylock BJ, Francis P, Hickey H, Gamble C, et al. Challenges conveying clinical equipoise and exploring patient treatment preferences in an oncology trial comparing active monitoring with radiotherapy (ROAM/EORTC 1308). Oncologist. 2020;25(4):e691–e700. https://doi.org/10.1634/theoncologist.2019-0571 (Epub 2020 Feb 11).
Fletcher B, Gheorghe A, Moore D, Wilson S, Damery S. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open. 2012;2(1):e496. https://doi.org/10.1136/bmjopen-2011-000496.
Hwang KL, Hwang WL, Bussière MR, Shih HA. The role of radiotherapy in the management of high-grade meningiomas. Chin Clin Oncol. 2017;6(1):S5. https://doi.org/10.21037/cco.2017.06.09.
Boskos C, Feuvret L, Noel G, Habrand JL, Pommier P, Alapetite C, et al. Combined proton and photon conformal radiotherapy for intracranial atypical and malignant meningioma. Int J Radiat Oncol Biol Phys. 2009;75(2):399–406. https://doi.org/10.1016/j.ijrobp.2008.10.053 (Epub 2009 Feb 7 PMID: 19203844).
Moraes FY, Chung C. Radiation for skull base meningiomas: review of the literature on the approach to radiotherapy. Chin Clin Oncol. 2017;6(1):S3. https://doi.org/10.21037/cco.2017.06.08.
Aizer AA, Arvold ND, Catalano P, Claus EB, Golby AJ, Johnson MD, et al. Adjuvant radiation therapy, local recurrence, and the need for salvage therapy in atypical meningioma. Neuro Oncol. 2014;16(11):15–53. https://doi.org/10.1093/neuonc/nou098.
Cohen-Inbar O, Lee CC, Sheehan JP. The contemporary role of stereotactic radiosurgery in the treatment of meningiomas. Neurosurg Clin N Am. 2016;27(2):215–28. https://doi.org/10.1016/j.nec.2015.11.006.
Kano H, Takahashi JA, Katsuki T, Araki N, Oya N, Hiraoka M, et al. Stereotactic radiosurgery for atypical and anaplastic meningiomas. J Neurooncol. 2007;84(1):41–7. https://doi.org/10.1007/s11060-007-9338-y (Epub 2007 Mar 15 PMID: 17361335).
Oermann EK, Bhandari R, Chen VJ, Lebec G, Gurka M, Lei S, et al. Five fraction image-guided radiosurgery for primary and recurrent meningiomas. Front Oncol. 2013;20(3):213.
Ware ML, Larson DA, Sneed PK, Wara WW, McDermott MW. Surgical resection and permanent brachytherapy for recurrent atypical and malignant meningioma. Neurosurgery. 2004;54(1):55–64. https://doi.org/10.1227/01.neu.0000097199.26412.2a.
Pajtler KW, Witt H, Sill M, Jones DT, Hovestadt V, Kratochwil F, et al. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell. 2015;27(5):728–43.
Al-Rashed M, Foshay K, Abedalthagafi M. Recent Advances in Meningioma Immunogenetics. Front Oncol. 2020;8(9):1472.
Sahm F, Schrimpf D, Stichel D, Jones DTW, Hielscher T, Schefzyk S, et al. DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol. 2017;18(5):682–94. https://doi.org/10.1016/S1470-2045(17)30155-9 (Epub 2017 Mar 15).
Nassiri F, Mamatjan Y, Suppiah S, Badhiwala JH, Mansouri S, Karimi S, et al. DNA methylation profiling to predict recurrence risk in meningioma: development and validation of a nomogram to optimize clinical management. Neuro Oncol. 2019;21(7):901–10. https://doi.org/10.1093/neuonc/noz061..
Chamberlain MC. The role of chemotherapy and targeted therapy in the treatment of intracranial meningioma. Curr Opin Oncol. 2012;24(6):666–71. https://doi.org/10.1097/CCO.0b013e328356364d.
Scerrati A, Mongardi L, Visani J, Lofrese G, Cavallo MA, Fiorentino A, et al. The controversial role of Bevacizumab in the treatment of patients with intracranial meningioma: a comprehensive literature review. Expert Rev Anticancer Ther. 2020;20(3):197–203. https://doi.org/10.1080/14737140.2020.1736567 (Epub 2020 Mar 6).
Dasanu CA, Samara Y, Codreanu I, Limonadi FM, Hamid O, Alvarez-Argote J. Systemic therapy for relapsed/refractory meningioma: Is there potential for antiangiogenic agents? J Oncol Pharm Pract. 2019;25(3):638–47. https://doi.org/10.1177/1078155218799850 (Epub 2018 Sep 26).
Delgado-López PD, Martín-Velasco V, Castilla-Díez JM, Fernández-Arconada O, Corrales-García EM, Galacho-Harnero A, et al. Metastatic meningioma to the eleventh dorsal vertebral body: total en bloc spondylectomy. Case report and review of the literature. Neurocirugia. 2006;17(3):240–9.
Golub D, Kwan K, Knisely JPS. Possible abscopal effect observed in frontal meningioma after localized imrt on posterior meningioma resection cavity without adjuvant immunotherapy. Front Oncol. 2019;9:1109.
Funding
This paper received no specific funding from private or public institution.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to the design, literature review, composition of the manuscript, and approval of the final version.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no conflicts of interest regarding the composition of this manuscript.
Consent to participate
Not needed for a literature review article.
Consent for publication
Not applicable.
Ethics approval
Not needed for a literature review article.
Informed consent
Informed consent is not needed for this review article.
Human participants and animals
No patients or animals were used for the composition of this paper.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Delgado-López, P.D., Corrales-García, E.M. Role of adjuvant radiotherapy in atypical (WHO grade II) and anaplastic (WHO grade III) meningiomas: a systematic review. Clin Transl Oncol 23, 205–221 (2021). https://doi.org/10.1007/s12094-020-02434-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02434-3