Abstract
Evaluate whether radiotherapy (RT) after the neurosurgical treatment of atypical meningiomas (AM) has an impact on the reduction rate of recurrence. A Medline search through October 2017 using “atypical meningioma” returned 1277 papers for initial review. Inclusion criteria were as follows. We analyzed the database and included articles in which the anatomic pathological classification of atypical meningiomas was in accordance with WHO 2007 or WHO 2016 criteria, patients > 18 years of age, and there was postoperative external beam radiation to the tumor bed. Exclusion criteria were WHO grade I or III meningioma, patients who underwent whole-brain radiation, RT used as salvage therapy for recurrence, palliative dose of RT (< 45 Gy), recurrent AMs, and multiple AMs. Papers reporting outcomes in which atypical and anaplastic meningiomas were analyzed together were rejected, as were papers with small samples that may compromise evaluation. After filtering our initial selection, only 17 papers were selected. After reviewing the seventeen articles including a total of 1761 patients (972 female and 799 male; 1.21 female/1.0 male), the difference in proportion of tumor recurrence between patients with and without radiotherapy after neurosurgical procedure was 1.0448, 95% CI [0.8318 to 1.3125], p value = 0.7062. On the basis of this review, there is no evidence to suggest that RT decreases the rate of recurrence in patients with atypical meningiomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atypical meningiomas (AM) represent up to 8% of all meningiomas [1], and their incidence is increasing (> 5–10% among all types of meningiomas); however, this number should increase given the new World Health Organization (WHO) 2016 criteria for the classification of this subtype of meningioma [2]. In fact, AM account for 20–25% of recurrent meningiomas [3, 4].
The rationale for advocating gross total resection (GTR) as the primary treatment for meningiomas is attributed to effective local control post-GTR and avoiding the toxicity associated with postoperative radiation therapy, including the increased risk of radiation-induced malignancies [5]. In neuro-oncological management, complete resection must be pursued in this subtype of tumor [6], and a definitive cure after surgical resection is achieved in 16–18% of patients. Nevertheless, the disease will recur within a few months in up to 62–69% of cases [7, 8].
Adjuvant radiotherapy after the surgical resection of AM continues to be controversial. Compared to surgery alone, surgery followed by postoperative radiation lowers the incidence of local recurrence of AM, as reported in previous reviews [9]. However, opposite results have also been reported [10, 11]. In a recent retrospective case study of 45 patients with atypical meningioma, Endo et al. [11] showed no additional benefit of adjuvant radiotherapy concerning the long-term tumor control; results similar to those of Champeaux et al. [10], who showed that patients who received radiotherapy did not have a different overall survival nor difference in recurrence rate.
Among the forms of radiotherapy treatment, we also did not observe consensus on the techniques. During the last two decades, stereotactic radiosurgery (SRS) has proved to be an effective treatment for WHO grade I benign meningioma [12, 13]. However, the efficacy of SRS in the treatment of grade II atypical meningiomas is still unclear [14]. Gamma knife radiosurgery (GKRS) for higher-grade meningiomas has been less well studied [15]. In the setting of recurrent atypical or malignant meningiomas, GKRS may provide durable palliation and local control for some but with poor long-term control overall [16].
Given the conflicting reports in the literature, we performed a systematic review to assess the impact of radiotherapy (RT) combined with surgical resection on the recurrence rate in patients with AM.
Methods
A Medline search from 2010 to October 2017 using “atypical meningioma” returned 1277 papers; we based our revision on this initial corpus. As a first selection step, we adopted the following inclusion criteria: (1) reports in which the anatomic pathological classification of AM was in accordance with WHO 2007 [17] or 2016 [2] criteria, (2) patients older than 18 years of age, and (3) postoperative external beam radiation to the tumor bed. Exclusion criteria were WHO grade I or III meningioma, patients who underwent whole-brain RT, RT used as salvage therapy for recurrence, definitive RT, palliative dose of RT (< 45 Gy), recurrent AMs, and multiple AMs.
All papers reporting outcomes in which atypical and anaplastic meningiomas were analyzed together were excluded, as were reports in the format of case reports with small series. Seventeen papers fulfilled the above criteria, and these papers gathered data from 1761 patients, on whom the present analysis of the neuro-oncological management of AM was based.
Data evaluation
The patients’ clinical data and tumor-evolution (recurrence or not) data were tabulated, mainly, the data concerning tumor recurrence after neurosurgical procedure and the impact of RT in terms of preventing tumor recurrence in AM [see Fig. 1 for the PRISMA study flow diagram].
We calculated the weighted mean differences and the 95% confidence interval (CI). Dichotomous variables were presented as odds ratios (ORs) with a 95% CI. Matched analysis was performed as appropriate. Significance was set at p < 0.05.
Results
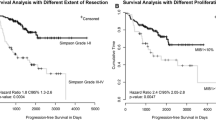
A total of 1761 patients (972 female and 899 male; 1.21 female/1.0 male ratio) reported in 17 manuscripts from worldwide centers during the period from 2010 to October 2017 were selected for the present analysis. Although the majority of the selected studies were from centers in the USA, we managed to analyze studies from each continent (see Table 1). Among them are 573 patients who underwent RT (32.5%) with a recurrence rate of 26% (149 patients). Comparatively, of the 1188 patients who were initially treated only with surgery, 299 patients presented tumor recurrence (25.16%). Thus, the difference in tumor recurrence between the two groups treated and not treated with RT after neurosurgical procedure was not significant (1.0448, 95% CI [0.8318 to 1.3125], p value = 0.7062) (see Table 1 and Fig. 2).
Discussion
Regarding the issue of the recurrence of meningiomas, some factors are already well established, such as the degree of surgical resection [32]. Since the initial work of Simpson [33] has proved that greater tumor resections lead to lower rates of tumor recurrence, other factors are still controversial, such as location. In our review, four of the articles selected [19,20,21,22] have an analysis of the subject, such as greater recurrence in tumors of convexity, but this result should reflect only the fact that this location is the most frequent. Despite technical and technological advances, the perioperative morbidity and mortality are high, because of their intimate anatomical relationship to the brain, cranial nerves, and essential blood vessels [34]. Another factor influencing the evolution of meningiomas is genetic alterations. Past studies have shown that the risk of meningioma recurrence is strongly correlated with the molecular profile of the tumor [35]. Genomic instability is one of the key differentiators between grade I and grade II–III meningiomas [36].
The clinical impact of AM recurrence is high, and the management of these patients poses specific challenges [37]. A robust analysis of large series of AM providing definitive guidelines for the neuro-oncological management of this type of meningioma is still missing; proof of this is that the management of these patients is still controversial and varies according to the group or center evaluated. In Germany, 74.1% of centers offer some form of RT following incomplete resection of AM, with 17.9% of centers offering postoperative RT even when tumor removal is complete [37]. In the UK, 59% of neurosurgeons would advise adjuvant radiotherapy in subtotal resection (STR), with only 20% doing so after gross total resection (GTR) [38]. Multicentricity varies from 19% at the first recurrence to 89% at the last follow-up, and marginal recurrence is progressively higher than the local type at the second and third recurrence, rendering management increasingly difficult [39, 40]. As the disease may be local, marginal, or distant with respect to the previous localization, a preferable indicator of treatment efficacy is disease-free interval [41, 42].
Radiotherapy was applied initially in the management of residual tumors after microsurgery. Its appropriate application proved to be successful when using all the available techniques, including linear accelerator (LINAC) [43,44,45], gamma knife [46, 47], proton beam [48], and conventional fractionated external beam radiation therapy (EBRT) [49]. As demonstrated in the literature, success rates of greater than 90% and with few associated complications can be achieved when stereotactic irradiation is performed in the management of intracranial meningiomas [16, 47, 50, 51]. The use of SRS alone has limitations that preclude its application in every case. These limitations are related to tumor size and proximity to eloquent structures especially the optic apparatus. Single-dose SRS is indicated for meningiomas smaller than 3 cm or 20 ml in volume and with a minimal distance from the optic apparatus of between 2 and 4 cm [52]. Although there are no long-term follow-up data for patients who underwent SRT for intracranial meningiomas, the expected success rate should be similar to that achieved using conventional EBRT, with fewer complications. A 5- and 10-year PFS rates of 92 and 83%, respectively, have been reported after EBRT [53]. The selection of the best treatment option for these lesions, however, should include consideration of tumor location, severity of presenting symptoms, and the long-term follow-up data of the available modalities.
There are several studies with conflicting results [9, 18, 19, 54, 55], and there are no randomized controlled trials, leading to a lack of class I evidence [56]. Our present systematic review failed to demonstrate a significant overall difference with respect to postoperative RT reducing tumor recurrence. However, there should be bias in the choice of patients who underwent radiotherapy, perhaps a point to be debated for future strategies to identify subgroups within the AM that present molecular characteristics at the level of biomarkers, so the patient is optimized and presents better results.
Conclusions
On the basis of this review, there is no evidence to suggest that RT decreases the rate of recurrence in patients with AM. Prospective studies on the effect of adjuvant RT for avoiding recurrence of AMs should be conducted to better address this question.
Limitations
Although this study had a large sample size, its limitations should be mentioned. Information on the extent of tumor resections, type of radiotherapy, and meningioma location is a limitation of our study; most of the articles do not present detail of these.
References
Huffmann BC, Reinacher PC, Gilsbach JM (2005) Gamma knife surgery for atypical meningiomas. J Neurosurg 102(Suppl):283–286
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820
Andric M, Dixit S, Dubey A, Jessup P, Hunn A (2012) Atypical meningiomas—a case series. Clin Neurol Neurosurg 114:699–702
Rogers L, Gilbert M, Vogelbaum MA (2010) Intracranial meningiomas of atypical (WHO grade II) histology. J Neuro-Oncol 99:393–405
Umansky F, Shoshan Y, Rosenthal G, Fraifeld S, Spektor S (2008) Radiation-induced meningioma. Neurosurg Focus 24:E7
de Almeida AN, Pereira BJA, Pires Aguiar PH, Paiva WS, Cabrera HN, da Silva CC, Teixeira MJ, Marie SKN (2017) Clinical outcome, tumor recurrence, and causes of death: a long-term follow-up of surgically treated meningiomas. World neurosurgery 102:139–143
Cao X, Hao S, Wu Z, Wang L, Jia G, Zhang L, Zhang J (2015) Treatment response and prognosis after recurrence of atypical meningiomas. World neurosurgery 84:1014–1019
Piscevic I, Villa A, Milicevic M, Ilic R, Nikitovic M, Cavallo LM et al (2015) The influence of adjuvant radiotherapy in atypical and anaplastic meningiomas: a series of 88 patients in a single institution. World Neurosurg 83:987–995
Park HJ, Kang HC, Kim IH, Park SH, Kim DG, Park CK, Paek SH, Jung HW (2013) The role of adjuvant radiotherapy in atypical meningioma. J Neuro-Oncol 115:241–247
Champeaux C, Dunn L (2016) World Health Organization grade II meningiomas. Acta Neurochirurgica 158:921–929; discussion 929
Endo T, Narisawa A, Ali HS, Murakami K, Watanabe T, Watanabe M et al (2016) A study of prognostic factors in 45 cases of atypical meningioma. Acta Neurochir 158:1661–1667
Kondziolka D, Mathieu D, Lunsford LD, Martin JJ, Madhok R, Niranjan A, Flickinger JC (2008) Radiosurgery as definitive management of intracranial meningiomas. Neurosurgery 62:53–58; discussion 58-60
Pan DH, Guo WY, Chang YC, Chung WY, Shiau CY, Wang LW et al (1998) The effectiveness and factors related to treatment results of gamma knife radiosurgery for meningiomas. Stereotact Funct Neurosurg 70(Suppl 1):19–32
Wang WH, Lee CC, Yang HC, Liu KD, Wu HM, Shiau CY, Guo WY, Pan DHC, Chung WY, Chen MT (2016) Gamma knife radiosurgery for atypical and anaplastic meningiomas. World neurosurgery 87:557–564
Sethi RA, Rush SC, Liu S, Sethi SA, Parker E, Donahue B, Narayana A, Silverman J, Kondziolka D, Golfinos JG (2015) Dose-response relationships for meningioma radiosurgery. Am J Clin Oncol 38:600–604
Stafford SL, Pollock BE, Foote RL, Link MJ, Gorman DA, Schomberg PJ et al (2001) Meningioma radiosurgery: tumor control, outcomes, and complications among 190 consecutive patients. Neurosurgery 49:1029–1037; discussion 1037–1028
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Jo K, Park HJ, Nam DH, Lee JI, Kong DS, Park K, Kim JH (2010) Treatment of atypical meningioma. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 17:1362–1366
Komotar RJ, Iorgulescu JB, Raper DM, Holland EC, Beal K, Bilsky MH et al (2012) The role of radiotherapy following gross-total resection of atypical meningiomas. J Neurosurg 117:679–686
Lee KD, DePowell JJ, Air EL, Dwivedi AK, Kendler A, McPherson CM (2013) Atypical meningiomas: is postoperative radiotherapy indicated? Neurosurg Focus 35:E15
Zaher A, Abdelbari Mattar M, Zayed DH, Ellatif RA, Ashamallah SA (2013) Atypical meningioma: a study of prognostic factors. World neurosurgery 80:549–553
Hardesty DA, Wolf AB, Brachman DG, McBride HL, Youssef E, Nakaji P et al (2013) The impact of adjuvant stereotactic radiosurgery on atypical meningioma recurrence following aggressive microsurgical resection. J Neurosurg 119:475–481
Sun SQ, Kim AH, Cai C, Murphy RK, DeWees T, Sylvester P et al (2014) Management of atypical cranial meningiomas, part 1: predictors of recurrence and the role of adjuvant radiation after gross total resection. Neurosurgery 75:347–354; discussion 354-345; quiz 355
Aizer AA, Arvold ND, Catalano P, Claus EB, Golby AJ, Johnson MD et al (2014) Adjuvant radiation therapy, local recurrence, and the need for salvage therapy in atypical meningioma. Neuro-Oncology 16:1547–1553
Hammouche S, Clark S, Wong AH, Eldridge P, Farah JO (2014) Long-term survival analysis of atypical meningiomas: survival rates, prognostic factors, operative and radiotherapy treatment. Acta Neurochirurgica 156:1475–1481
Yoon H, Mehta MP, Perumal K, Helenowski IB, Chappell RJ, Akture E et al (2015) Atypical meningioma: randomized trials are required to resolve contradictory retrospective results regarding the role of adjuvant radiotherapy. J Cancer Res Therap 11:59–66
Bagshaw HP, Burt LM, Jensen RL, Suneja G, Palmer CA, Couldwell WT et al (2017) Adjuvant radiotherapy for atypical meningiomas. J Neurosurg 126:1822–1828
Jenkinson MD, Waqar M, Farah JO, Farrell M, Barbagallo GM, McManus R et al (2016) Early adjuvant radiotherapy in the treatment of atypical meningioma. J Clin Neurosci 28:87–92
Dohm A, McTyre ER, Chan MD, Fan C, Isom S, Bourland JD et al (2017) Early or late radiotherapy following gross or subtotal resection for atypical meningiomas: Clinical outcomes and local control. J Clin Neurosci 46:90–98
Pereira BJA, de Almeida AN, de Aguiar PHP, Paiva WS, Cabrera HN, da Silva CC, et al (2017) Atypical and Malignant Meningiomas: Neuro-oncological Management in a Brazilian cohort. World Neurosurg
Masalha W, Heiland DH, Franco P, Delev D, Haaker JG, Schnell O et al (2018) Atypical meningioma: progression-free survival in 161 cases treated at our institution with surgery versus surgery and radiotherapy. J Neuro-Oncol 136:147–154
Hasan S, Young M, Albert T, Shah AH, Okoye C, Bregy A, Lo SS, Ishkanian F, Komotar RJ (2015) The role of adjuvant radiotherapy after gross total resection of atypical meningiomas. World neurosurgery 83:808–815
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Zentner J, Meyer B, Vieweg U, Herberhold C, Schramm J (1997) Petroclival meningiomas: is radical resection always the best option? J Neurol Neurosurg Psychiatry 62:341–345
Bi WL, Mei Y, Agarwalla PK, Beroukhim R, Dunn IF (2016) Genomic and epigenomic landscape in meningioma. Neurosurg Clin N Am 27:167–179
Lee WH (1990) Characterization of a newly established malignant meningioma cell line of the human brain: IOMM-Lee. Neurosurgery 27:389–395; discussion 396
Simon M, Bostrom J, Koch P, Schramm J (2006) Interinstitutional variance of postoperative radiotherapy and follow up for meningiomas in Germany: impact of changes of the WHO classification. J Neurol Neurosurg Psychiatry 77:767–773
Marcus HJ, Price SJ, Wilby M, Santarius T, Kirollos RW (2008) Radiotherapy as an adjuvant in the management of intracranial meningiomas: are we practising evidence-based medicine? Br J Neurosurg 22:520–528
Nascimento C, Di Lorenzo Alho AT, Bazan Conceicao Amaral C, Leite REP, Nitrini R, Jacob-Filho W, et al: Prevalence of transactive response DNA-binding protein 43 (TDP-43) proteinopathy in cognitively normal older adults: systematic review and meta-analysis. Neuropathol Appl Neurobiol, 2017
Sun SQ, Cai C, Murphy RK, DeWees T, Dacey RG, Grubb RL et al (2014) Management of atypical cranial meningiomas, part 2: predictors of progression and the role of adjuvant radiation after subtotal resection. Neurosurgery 75:356–363; discussion 363
Attia A, Chan MD, Mott RT, Russell GB, Seif D, Daniel Bourland J, Deguzman AF, Ellis TL, McMullen KP, Munley MT, Tatter SB, Shaw EG (2012) Patterns of failure after treatment of atypical meningioma with gamma knife radiosurgery. J Neuro-Oncol 108:179–185
Hanakita S, Koga T, Igaki H, Murakami N, Oya S, Shin M, Saito N (2013) Role of gamma knife surgery for intracranial atypical (WHO grade II) meningiomas. J Neurosurg 119:1410–1414
De Salles AA, Frighetto L, Grande CV, Solberg TD, Cabatan-Awang C, Selch MT et al (2001) Radiosurgery and stereotactic radiation therapy of skull base meningiomas: proposal of a grading system. Stereotact Funct Neurosurg 76:218–229
Hakim R, Alexander E 3rd, Loeffler JS, Shrieve DC, Wen P, Fallon MP et al (1998) Results of linear accelerator-based radiosurgery for intracranial meningiomas. Neurosurgery 42:446–453; discussion 453–444
Spiegelmann R, Nissim O, Menhel J, Alezra D, Pfeffer MR (2002) Linear accelerator radiosurgery for meningiomas in and around the cavernous sinus. Neurosurgery 51:1373–1379; discussion 1379-1380
Iwai Y, Yamanaka K, Ishiguro T (2003) Gamma knife radiosurgery for the treatment of cavernous sinus meningiomas. Neurosurgery 52:517–524; discussion 523–514
Kobayashi T, Kida Y, Mori Y (2001) Long-term results of stereotactic gamma radiosurgery of meningiomas. Surg Neurol 55:325–331
Vernimmen FJ, Harris JK, Wilson JA, Melvill R, Smit BJ, Slabbert JP (2001) Stereotactic proton beam therapy of skull base meningiomas. Int J Radiat Oncol Biol Phys 49:99–105
Barbaro NM, Gutin PH, Wilson CB, Sheline GE, Boldrey EB, Wara WM (1987) Radiation therapy in the treatment of partially resected meningiomas. Neurosurgery 20:525–528
Duma CM, Lunsford LD, Kondziolka D, GRt H, Flickinger JC (1993) Stereotactic radiosurgery of cavernous sinus meningiomas as an addition or alternative to microsurgery. Neurosurgery 32:699–704; discussion 704-695
Kondziolka D, Levy EI, Niranjan A, Flickinger JC, Lunsford LD (1999) Long-term outcomes after meningioma radiosurgery: physician and patient perspectives. J Neurosurg 91:44–50
Torres RC, Frighetto L, De Salles AA, Goss B, Medin P, Solberg T et al (2003) Radiosurgery and stereotactic radiotherapy for intracranial meningiomas. Neurosurg Focus 14:e5
Nutting C, Brada M, Brazil L, Sibtain A, Saran F, Westbury C, Moore A, Thomas DGT, Traish D, Ashley S (1999) Radiotherapy in the treatment of benign meningioma of the skull base. J Neurosurg 90:823–827
Aghi MK, Carter BS, Cosgrove GR, Ojemann RG, Amin-Hanjani S, Martuza RL et al (2009) Long-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiation. Neurosurgery 64:56–60; discussion 60
Mair R, Morris K, Scott I, Carroll TA (2011) Radiotherapy for atypical meningiomas. J Neurosurg 115:811–819
Pollock BE (2014) Defining the best management for patients with intracranial World Health Organization grade II meningiomas. World Neurosurg 81:712–713
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by our Institutional Review Board under registration CAPPESq no. 200/05.
Informed consent
All authors agree to the publication guidelines of the Neurosurgical Review.
Rights and permissions
About this article
Cite this article
Pereira, B.J.A., de Almeida, A.N., Paiva, W.S. et al. Impact of radiotherapy in atypical meningioma recurrence: literature review. Neurosurg Rev 42, 631–637 (2019). https://doi.org/10.1007/s10143-018-0959-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0959-8