Abstract
The study was designed to determine the fluoride distribution after its oral exposure in drinking water and its associated impact on biochemical, antioxidant markers and histology in the liver, kidney, and heart of male Wistar rats. On 100 ppm exposure, the highest accretion of fluoride occurred in the liver followed by the kidney and heart. Fluoride exposure significantly (p˂0.05) increased the plasma levels of dehydrogenase, aminotransferases, kidney injury molecule-1 (KIM-1), and other plasma renal biomarkers but decreased the levels of total plasma proteins and albumin in a dose-dependent manner. Reduction (p˂0.05) in the activities of antioxidant enzymes viz. acetylcholinesterase, arylesterase, superoxide dismutase, catalase, glutathione peroxidase, and reductase with increased levels of protein and lipid peroxidation was recorded in the liver, kidney, and heart of fluoride-administered rats. Fluoride exposure (100 ppm) induced lipid peroxidation was highest in kidney (4.4 times) followed by liver (2.6 times) and heart (2.5 times) and as compared to their respective control. The percent rise in protein oxidation at 30% was almost equal in the kidney and liver but was 21.5% in the heart as compared to control. The histopathological alterations observed included congestion and hemorrhage along with degeneration and necrosis of parenchymal cells in hepato-renal tissues and myocardium, severity of which varied in a dose-dependent manner. Taken together, fluoride distribution in the liver, heart, and kidney after chronic fluoride intake correlated well with fluoride-induced hepatic and cardio-renal toxicity in a concentration-dependent manner. These results draw attention that chronic fluoride intake pose a significant health risk for human and animal residents of fluoride endemic areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysfunctions of liver, kidney, and heart are becoming exceedingly common in humans as well as animals causing substantial deterioration in the quality of life as well as shortened life expectancy in them and have become huge burdens on health infrastructure of nations worldwide. Intentional fluoridation of community water supply has been carried out since long as an anti-cariogenic measure in most developing as well as developed nations. Drinking water containing fluoride is also advocated by world’s foremost health organizations including WHO and International Association of Dental Research [1, 2]. Moreover, inhalation of air contaminated with fluoride emanating from manufacturing units, wide spread use of fluoride containing products such as cosmetics or dental implants, and consumption of food raised or prepared using fluoridated water also cumulatively enhance fluoride ingress into body. Ground water naturally contaminated with minerals such as fluoride in many parts of the world serves as the primary source of drinking water for its inhabitants [3, 4]. Apart from this, fluoride frequently spills over from geological sources such as rocks to reach ground water to further raise the fluoride water levels. In many parts around the world, its concentration in such waters ranges between 0.5 and 25 ppm [5]. This inherently polluted ground water alone serves as a formidable source of fluoride exposure affecting around 200 million people across 25 countries including India [6]. In addition, bioaccumulation of fluoride tends to occur in crops, fruits, and vegetables owing to the usage of water with high fluoride content for irrigation purposes; therefore, daily intake of fluoride in local population of such area far exceeds that prescribed by international agencies such as the WHO [7,8,9].
A recent study from India found a large number of ground water samples to be polluted with fluoride, and an unsafe hazard index of fluoride was reported in participants of the study [9]. Furthermore, high prevalence of dental fluorosis and dental caries among people from endemic fluorosis areas where ground water has higher than the WHO recommended level (1.5 mg/l) of fluoride has been recorded [10]. A recent report from Mexico also revealed a high prevalence (72.4%) of caries in permanent teeth in children belonging to marginalized rural communities leveling in areas where water fluoridation levels varied between 2.0 and 2.5 ppm while the prevalence of fluorosis was found to be 98% in those areas [11]. Following the oral exposure, rapid absorption of fluoride occurs via the gastrointestinal tract; subsequently, it gets distributed in different tissues [12, 13]. Liver and kidney being the primary organs responsible for xenobiotic detoxification and removal from the body thus get exposed to relatively higher fluoride concentrations. Approximately 50% of the absorbed fluoride is excreted by the kidney. Therefore, fluoride intake in high concentrations impairs renal enzymatic machinery, incurs tubular damage affecting tubular re-absorption as well as urinary ion exchange, and has been directly linked to the development of chronic renal disease which potentially can exert damaging effects on other organ systems as well [14]. Fluoride intoxication raised plasma hepatic and renal health biomarker levels besides causing portal inflammation and hepatic necrosis [15]. Experimental supplementation of fluoride that mimicked natural exposure caused impaired renal tubular absorption and disrupted renal excretion of calcium and phosphate ions [16]. A cross-sectional study conducted among adolescents in the USA revealed that fluoride exposure altered indices associated with kidney and liver functions [17].
Chronic fluoride exposure mediated renal and hepatic functional and structural alterations, also inflicting oxidative injury to myocardium [18]. Fluoride-induced oxidative stress can cause myocardial necrosis and inflammation, aortic stiffness, and diminished ventricular filling; therefore, cardiovascular health may be compromised in people affected with endemic fluorosis [19]. Excessive fluoride ions inhibit cellular metabolic enzymes and alter stress response leading to excessive production of reactive oxygen and nitrogen species (ROS/RNS) and depletion of the thiols (-SH group). Additionally, fluoride is thought to inhibit the activities of antioxidant enzymes viz. catalase (CAT), superoxide dismutase (SOD), glutathione peroxidase (GPx), and glutathione reductase (GR) responsible for scavenging excess ROS/RNS. Excess production of ROS/RNS and declined antioxidant enzymes during fluoride intoxication leading to fluoride-induced oxidative stress suffer extensive peroxidation of membrane lipids as well as cellular proteins and often develop discernible micromorphological alterations [20, 21].
Furthermore, recent reports suggest that cardiac dysfunctions are intertwined with renal disorders and hepatic ailments in many cases [22]. Additionally, the heart facilitates renal excretion of extraneous substances and enables to maintain homeostasis in the body. Since disruption in antioxidant machinery in vital organs can predispose towards their dysfunction impacting the overall health of an individual, hence, a comprehensively study needed to be carried out to assess the impact of chronic fluoride exposure on antioxidant parameters in the liver, kidney, and heart. The present study was therefore conceptualized to determine the correlation between the concentration of fluoride in hepatic, renal, and cardiac tissues and the extent of oxidative damage, antioxidant, and biochemical alterations along with histopathological changes in these organs following chronic exposure to fluoride via drinking water in Wistar rats.
Material and Methods
The study was conducted on adult male Wistar rats procured from the Indian Institute of Integrative Medicine, Jammu. The animals were allowed to acclimatize for a week, fed pelleted food, and were given access to tap water ad-lib and 12 h/12 h light/darkness cycle. The pelleted food (Table 1) provided to Wistar rats was supplied by the Animal Feed Unit, Department of Animal Nutrition, CSKHPKV, Palampur, Himachal Pradesh, India. All the experimental animals were kept under observation during the entire period of study. The experimental protocol was duly approved by the Institutional Animal Ethics Committee (IAEC) vide letter no. 09/IAEC/2020 dated 22/10/2020 (Registration Number of IAEC—862/ac/04/CPCSEA) using the standard guidelines of handling and care of experimental animals. The threshold dose of fluoride in drinking water for renal toxicity in animals is approximately 50 ppm [23,24,25]. Therefore, two dose levels viz. 50 ppm (threshold level) and twice of the threshold dose (100 ppm) were used in the study. Sodium fluoride was used as a source of fluoride (0.2210 g sodium fluoride/l in tap water (providing 100 ppm fluoride) and 0.1105 g/l (providing 50 ppm fluoride) in the medium for induction of chronic fluoride intoxication in Wistar rats. All the chemicals viz. hydrogen peroxide, pyrogallol, acetylcholine iodide, trichloro-acetic acid, and phenyl acetate used in the study were of analytical grade and purchased from different standard firms.
Experimental Protocol
Eighteen adult male Wistar rats (180–200 g, 12–14 weeks of age) were randomly allocated into three groups with six animals in each. Group I served as control and was provided tap water, whereas groups II and III were given drinking water containing 50 and 100 ppm fluoride, respectively, continuously for 180 days. At the end of the experiment, animals were anesthetized with diethyl ether; blood samples were collected directly from the heart in an aliquot containing heparin as an anticoagulant. After that, the animals were sacrificed by cervical dislocation, and the liver, kidney, and heart tissues (1 g, each) were collected in 10 ml ice-cold 0.5 M phosphate buffer (pH 7.4) for tissue antioxidant biomarker analysis. Tissue homogenate (1%) was prepared by homogenizing the tissue using Teflon-coated homogenizer at 1000 rpm for 5–7 min at 4 °C for the determination of antioxidant biomarkers. Tissues were also collected in 10% formaldehyde solution for histopathological studies.
Fluoride Estimation
The fluoride level in the liver, heart, and kidney tissues was estimated (w/v wet basis) according to the standard extraction method [26, 27]. In brief, 1.0 g of fresh tissue was homogenized in solution containing 6.25 ml of 5.0% solution of sodium versenate and 6.25 ml of total ionic strength adjuster buffer III (TISAB III). Following homogenization, the sample container was kept in shaking water bath at 95 °C for 15 min. The cooled samples were filtered on suction funnel, and filtrate was reconstituted to 25 ml with distilled water for estimation of fluoride using ion selective electrochemistry (ISE) analyzer (Versa Star Pro Benchtop Electrochemistry meter, Thermo Scientific Orion). The ISE was first calibrated with working standard fluoride ion concentrations in spiked plasma and tissue samples. The recovery of standard fluoride ranges between 89 and 95% during the standardization. Lower detection limit of equipment is 0.025 ppm, and calibration curve was prepared using different concentrations (0.05 ppm, 0.5 ppm, and 5.0 ppm) for the determination of fluoride in different tissues of Wistar rats [27]. The average slope of the standard curve used for the estimation is − 58.3 mV/dec.
Plasma Biomarkers
The level of kidney injury molecule-1 (KIM-1) was estimated using ELISA kit supplied by the SunRed Biotechnology Company, Shanghai. The plasma biomarkers for renal and hepatic functions, alanine aminotransferase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), blood urea nitrogen (BUN), creatinine (CR), total plasma proteins (TPP), and albumin (ALB), in different groups were determined by standard kits (Transasia Bio-Medicals Ltd, HP, India) using chemistry analyzer (CHEM-7, ERBA, Mannheim).
Antioxidant Biomarkers in Tissues
The activities of antioxidant biomarkers and cellular damage indicators were estimated in hepatic, renal, and cardiac tissues of different groups of rats. Total thiol (TTH) level was determined in different tissues as per the standard protocol, and the concentration of total thiols was expressed in mM using reduced glutathione as a standard [28]. Antioxidant enzyme activities viz. CAT [29], SOD [30], GPx [31], GR [32], acetylcholinesterase (AChE) [33], and arylesterase (AE) [34] were determined in hepatic, renal, and cardiac tissues of different groups of rats and were determined (UV-1601, Shimadzu) to assess the alterations in antioxidant system following exposure to toxicant alone or in combination. To determine the extent of cellular protein and lipid peroxidation, levels of malondialdehyde (MDA) [35] and advanced oxidized protein product (AOPP) [36] in different tissues were determined.
Histopathological Study
The histopathological alterations in the liver, renal, and cardiac tissues were carried out according to the standard protocol [37]. Formalin-fixed tissues of groups were embedded in paraffin, sectioned, stained with hematoxylin and eosin, and examined under a light microscope.
Statistical Analysis
Standard statistical procedures were followed and the data collected during the experiment was subjected to analysis of variance (ANOVA) using statistical software SPSS and the significance was tested using Duncan multiple range test. The significance was assayed at 5% (p < 0.05) levels.
Results
Fluoride Levels in Food, Water, and Tissues
The fluoride levels recorded in the liver, heart, and kidney of Wistar rats following their chronic exposure to sodium fluoride are shown in Table 2. A dose-dependent increase (p˂0.05) in the tissue levels of fluoride was observed in the liver, heart, and kidney of exposed rats as compared to the corresponding control tissues of rats. The highest accumulation of fluoride occurred in liver followed by kidney and heart on 100 ppm fluoride exposure. The fluoride levels in food and tap water provided to the experimental rats were analyzed and level in food was 1.93 ± 0.65 ppm (% dry matter basis) whereas tap water provided to animals contained 1.43 ± 0.17 ppm fluoride.
Plasma Biomarkers
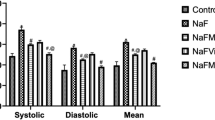
Alterations in hepatic, cardiac, and renal biomarkers in the plasma of Wistar rats following chronic exposure of fluoride at different dose levels are presented in Table 3. The levels of the KIM-1 in different treated groups were determined using double-antibody sandwich ELISA. Total six concentrations between 250 and 8000 pg/ml were used for the preparation of standard curve. The values of KIM-1 (pg/ml) were determined using the straight line equation (y = 1E-04x + 0.153) R2 = 0.997) drawn from the standard curve. The chronic exposure of fluoride significantly (p˂0.05) increased KIM-1 values in a dose-dependent manner, i.e., 50 ppm (26.73%) and 100 ppm (40.55%). The levels of BUN, UA and CR were also significantly raised (p˂0.05) following oral exposure of fluoride in a dose-dependent manner. Likewise, a chronic oral administration of fluoride significantly (p˂0.05) increased the plasma levels of AST, ALT, LDH, and ALP in a concentration-dependent manner. As far as TPP values was concerned although a significant decrease occurred in values after 50 ppm dosage as compared to the control levels, no further change in TPP concentrations was noted after 100 ppm exposure. Similarly, significant reduction in ALB level was observed in rats exposed with 100 ppm fluoride in drinking water.
Antioxidant and Histopathological Alterations in Tissues
Kidney
Alterations in the antioxidant biomarkers in the kidney of Wistar rats following chronic fluoride exposure at different dose levels in drinking water are shown in Table 4. Significantly decreased activities of AE (55.03–82.5%), CAT (38.6–50.5%), SOD (42.4–49.7%), GPx (08.2–14.2%), GR (32.7–42.0%), and TTH (17.9–44.4%) were recorded in the renal tissue of rats exposed to 50 and 100 ppm of fluoride in drinking water as compared to control rats. Reductions were also observed in values of AChE (13.05–35.4%), but these declines were significant only after higher dose toxicity. 100 ppm dose however did not further significantly lower the contents of CAT, SOD, GPx, and GR. In contrast, dose-dependent significant drop in the levels of AE and TTH was noticed. The values of AOPP in the renal tissue of different groups of animals progressively showed an increase compared to the control after treatment with 50 ppm (7.5%) as well as 100 ppm (31.3%) fluoride administration (Fig. 1a). Also, a dose-dependent significant increase in the MDA levels was seen in the renal tissue (Fig. 1b) in fluoride-intoxicated rats. The MDA levels rose more pronouncedly in renal tissue 63.1% (50 ppm) and 438% (100 ppm) as compared to other studied tissues of Wistar rats. Microscopic examination of the kidney of the control rats revealed no visible alterations in renal parenchyma. Glomerulus as well as tubules had normal histological morphology (Fig. 2a). But group II kidneys showed atrophied glomerular tufts with mild degree of degeneration in tubular epithelium besides congestion and lymphoid aggregation in the interstitium (Fig. 2b). Tubular epithelium often desquamated in the lumen of the tubules. Kidney sections from group III rats revealed severe histomorphological changes which included severe degeneration and congestion of glomerular tufts and interstitial blood vessels. Also, severe degrees of inter-tubular hemorrhages were seen (Fig. 2c). Large aggregates of lymphocytic population were seen in inter-tubular areas along with tubular degeneration and necrosis (Fig. 2d). Glomerular tuft was severely atrophied and at many places, Bowman’s capsule was disrupted.
Alterations in (a) advanced oxidative protein products (AOPP) and (b) malondialdehyde (MDA) levels in the liver, kidney, and heart of Wistar rats following chronic exposure of fluoride (50 and 100 ppm) in drinking water. Mean values having different superscript (a, b, c) differ significantly at 5% (p < 0.05) level of significance
Photomicrographs (H&E 400 ×) of stained kidney sections in the control and fluoride-treated rats: (a) normal renal parenchyma room of group I rats (control group) showing healthy glomerulus (arrows) with a tuft of capillaries within Bowman’s capsule and tubules lined by simple cuboidal epithelium. (b) Atrophied glomerulus tuft (blue arrow) severe degeneration of tubules (thin arrow) and mild lymphoid aggregation (black arrow) in group fed 50 ppm fluoride whereas in group fed 100 ppm fluoride (c and d), kidney sections showed severe inter-tubular hemorrhages (blue arrow), severe degenerative changes, necrosis (black arrow), degeneration, and atrophy of glomerulus (yellow arrows) and aggregates of lymphoid infiltrates (star) in renal parenchyma in Wistar rats
Liver
Changes in the antioxidant biomarkers in the liver after chronic fluoride exposure at different dose levels in drinking water in various experimental groups are presented in Table 4. The activities of hepatic AChE in rats declined (p˂0.05) in a dose-dependent manner, and reductions of 36.5% and 53.3% were recorded at 50 and 100 ppm, respectively, when compared to the control; however, the decline at higher dose was insignificant from that caused by lower dose administration. A dose-dependent significant decline (p˂0.05) of 62.6% and 73.8% in the AE activity was also noticed after 50 ppm and 100 ppm fluoride intoxication, respectively. A significant decrease in the CAT values (50.0–75.5%) occurred at both doses as compared to the control but no further significant reduction was witnessed with 100 ppm when compared to the lower dose toxicity. Reduction in the levels of SOD, GPx, and TTH was significant at both doses with respect to the control although decline was not dose dependent. The GR content also registered a fall ranging from 23.5 to 31% although significant variations in respect to the control values were only recorded after 100 ppm dosing. The cellular damage indicators viz. protein and lipid peroxidation levels increased significantly in the liver following the exposure of fluoride in Wistar rats (Fig. 1a and 1b). However, AOPP values were significantly elevated only after 100 ppm exposure in contrast to the dose-dependent significant rise seen in the MDA levels in liver. The increment in the oxidation of proteins ranged between 4.0 and 23.2% which was markedly lower in comparison to lipid peroxidation at 50 ppm (35.7%) and 100 ppm (260%) as compared to their respective control values. On histopathological examination, liver sections from the control rats showed no microscopic alterations. Cords of healthy hexagonal hepatocytes with centrally placed nuclei radiated around the central veins with portal triads revealing no any pathological change (Fig. 3a).In group II rat livers, pathological changes of mild degree were noticed which included congestion, hepatocellular degeneration mainly fatty degeneration with fat vacuoles in the cytoplasm of hepatocytes, and signet ring appearance (Fig. 3b) along with mild congestion, edema, and bile duct hyperplasia. In group III livers, severe changes were appreciated. Multifocal edema alongside necrosis of hepatocytes and hemorrhage was observed in the liver parenchyma (Fig. 3c). The central veins were found engorged and often their basement membranes were disrupted leading to blood spillover in the liver parenchyma to encompass the adjacent hepatocytes which appeared dissociated and necrotic (Fig. 3d). Hemosiderin pigment was also found scattered in the hepatic parenchyma. Moreover, portal triads also had severe bile duct hyperplasia and hemorrhage.
Photomicrographs of H&E (400 ×) stained liver sections in the control and fluoride-treated rats: (a) liver parenchyma of control rats with central vein and hepatocytes arranged radially around it. (b) Liver from 50 ppm fluoride exposure showing mild fatty degeneration (arrows). Liver in figure (c) showing an area of necrosis with edema (arrow) and hemorrhage and (d) congestion (blue arrow) with hemorrhage (black arrow) and disassociation and necrosis of perivascular hepatocytes (arrow heads) of Wistar rats with 100 ppm fluoride exposure
Heart
Variations in the antioxidant profile in cardiac tissue after chronic fluoride administration at different dose levels in different groups of rats are shown in Table 4. Declines in the activities of AChE, AE, CAT, SOD, GPx, GR, and TTH were observed in the cardiac tissue of Wistar rat on chronic fluoride exposure but significant differences were perceived only in the case of AChE, AE, and GR values with respect to control levels. The fall was dose dependent in AE concentration and ranged from 60 to 72.5%, respectively. The variation in GR values varied between 5 and 33.3% but reduction became significant only after high dose treatment. The AChE levels registered a significant decrease after 50 ppm treatment (35.1%) and 100 ppm did not cause any further significant drop. Alterations in the AOPP and MDA levels in various tissues after fluoride treatment are depicted in Fig. 1. Fluoride treatment spurred a significant rise in AOPP values in cardiac tissue only at 100 ppm level (Fig. 1a) whereas a dose-dependent rise in cardiac MDA contents was observed after fluoride administration (Fig. 1b). The AOPP increment ranged from 5.7 to 36.4% and the MDA increment ranges from 76.9 to 249% in the cardiac tissue of Wistar rats following fluoride exposure at different dose levels. Histomorphologically, myocardium in group I rats had normal appearance with myofibers showing cross striations, centrally located nucleus, and normal branching pattern (Fig. 4a). Group II hearts showed mild degeneration of myocardial fibers and congestion (Fig. 4b). However, significant alterations were encountered in the cardiac sections of group III rats which included hemorrhages along with severe myofiber degeneration with loss of cross striations (Fig. 4c). Additionally, diffuse areas of myofiber disorganization, fragmentation, and myonecrosis were also present. Areas with necrotic and fragmented cardiac fibers were infiltrated with mononuclear population of inflammatory cells mainly lymphocytes (Fig. 4d).
Photomicrographs of H&E (400 ×) stained heart in the control and fluoride-treated rats: (a) group I (control) animals had normal cardiac histological architecture, (b) group II rats (50 ppm fluoride exposure) had mild degeneration (arrow) and congestion (arrow head) in cardiac tissue. Severe degeneration of myocardial fibers (thick arrow) along with congestion and hemorrhage (thin arrows) of group III rats (100 ppm fluoride exposure) and (c) severe degeneration and necrosis (arrowheads) of myofibers with infiltration of mononuclear cells (arrows) in group III rats (100 ppm fluoride)
Discussion
Fluoride at lower concentrations functions as a micronutrient since it prevents tooth decay and promotes bone health. But chronic fluoride intake causes it to accumulate in various tissues which in turn lead to cascading effects causing wide ranging pathological alterations involving multiple organ systems in the mammalian body. Fluoride accrual triggers oxidative stress which sabotages the intracellular antioxidant defense system. Increased production of ROS and reduced activity of antioxidant enzymes in blood and tissues were observed in human and animals in endemic fluorosis areas [38, 39]. Fluoride even at low levels causes increased production of ROS viz. superoxide anion, peroxide, hydroperoxides, and hydrogen peroxide, which plays an important role in pathogenesis of ailments recorded in individuals in endemic fluorotic areas [40]. Fluoride induces ROS production, alters mitochondrial membrane potential, and inducts apoptotic cell death by mechanisms which may involve the release of mitochondrial outer membrane cytochrome c and upregulation of p53 among others [41, 42]. Our previous study showed that chronic fluoride toxicosis raised the levels of fluoride in the blood, bones, and brain, induced oxidative damage, and distorted erythrocytic as well as neurological antioxidant functioning and histomorphology besides causing improper mineralization and ossification of bones of rats in a dose-dependent manner [43]. In the present paper, we are discussing the fluoride-induced oxidative damage and biochemical and histological alterations in the kidney, liver, and heart of rats chronically exposed with sodium fluoride at different dose levels.
Alterations in plasma biomarkers of the liver, heart (AST, ALT, and LDH), and kidney (KIM-1, BUN, CR, UA, protein profile) verified the dysregulation in physiological functions of these organs following the chronic fluoride exposure in Wistar rats. Similar observations in laboratory and small ruminants have also been made previously [44,45,46]. Disorders of the cardiovascular system are the foremost causes of global morbidity and mortality in humans [47]. Environmental pollutants including extraneous chemicals are significant contributors in increased incidence and severity of cardiovascular maladies reported all over the world [48]. Excessive fluoride level in the heart alters cardiac biomechanical and electrical functioning in addition to injuring myocardial architecture thus promoting development of a wide array of cardiac abnormalities [6, 47, 49].
In the present study, a concentration-dependent increase in lipid as well as protein peroxidation was noted in cardiac tissues after the induced fluoride intoxication. These oxidative stress-induced alterations in the cardiac tissue probably lead to histopathological changes like myocardial degeneration, loss of cross striations, necrosis, fragmentation, and inflammation observed in our study. Likewise, others have also reported myocardiocyte damage after fluoride intoxication in vivo as well as in vitro studies [42, 50]. Reduced activities of antioxidant system as evidenced by low levels of CAT, SOD, GPx, TTH, and GR indicate that it was probably overwhelmed with fluoride-induced oxidative injury and therefore, a reduced scavenging of free radicals generated following fluoride administration occurred. Earlier observations also recorded that oxidative stress secondary to fluoride toxicity was responsible for myocardial degeneration and necrosis alongside inflammation, edema, hemorrhages, and fibrosis [18, 19, 42, 51]. The fluoride-induced damages in cardiac antioxidant system and architecture as encountered in our study were more severe in animals having higher amassing of fluoride in their cardiac tissues.
A multitude of previous studies found that toxic fluoride exposure may exacerbate the risk of coronary heart disease. Excessive fluoride was shown to induce increased expression of inflammatory cytokines such as IL-8 and IL-6 in rabbit aortas [52] and fluoride accumulation in cardiac vascular channels promoted in situ micro-calcification and hardening [19, 53]. Furthermore, studies have reported that fluoride-induced oxidative stress activates Bcl-2/Bax signaling pathway promoting apoptosis [42]. Necrosis and inflammation were also detected in the heart sections in our study in fluoride-treated rats. Furthermore, increased MDA with reduced AST and TTH in cardiac tissues alongside severe myocardial histological lesions after chronic fluoride intoxication in albino rats as reported in a previous research work [54] is in strong agreement with our work and supports the fact that high-dose long-term fluoride is toxic to the heart and damages cardiac antioxidant machinery, causing large-scale lipid peroxidation and myocardial damage. Overall increased lipid and protein peroxidation, reduced potency of the resident cardiac antioxidant system as a result of fluoride exposure can predispose population residing in fluoride endemic areas to develop cardiac ailments or exacerbate their preexistent heart diseases.
Liver, plays a vital role in synthesis of macromolecules, homeostasis and conversion of exogenous and endogenous compounds to harmless and excretable compounds [46, 55, 56]. Long-term fluoride exposure via drinking water containing fluoride concentration beyond 2.0 mg/l hampers renal and hepatic functioning in children [57]. This was corroborated by the observations of the present study which indicated that severe damage occurred in hepatic tissues of rats exposed chronically with fluoride as reflected by dose-dependent increased peroxidation and depression in action of hepatic antioxidants. Also, significant reductions in the levels of albumin and significant elevations of in ALT and AST supported chronic fluoride-induced hepatocellular damage. Reduced levels of hepatic antioxidant enzymes viz. CAT, SOD, GPx, and GR in our study indicated that scavenging of the ROS generated during the chronic fluorosis was compromised which correlated well with the observed histopathological alterations viz. hepatocellular degeneration and necrosis in the liver tissues of our experimental rats. Fluoride reportedly stalled cell cycle progression and S-phase arrest in mouse hepatocytes and caused increased granularity and vacuolar degeneration alongside necrosis in them [58]. Our results are also in line with the previous works describing mechanisms of fluoride-induced hepatotoxicity in a dose-dependent manner [1, 57]. Fluoride toxicity resulted in high fluoride levels in the liver along with significant elevations in hepatic MDA levels resulting in apoptotic body formation, nuclear and cellular shrinkage, and swelling of organelles viz. mitochondria and endoplasmic reticulum [59]. Similar to our results, chronic fluoride exposure not only decreased SOD, CAT, GSH, GPx, and GST in the liver of mice but also raised serum ALT, AST, and MDA levels along with inflicting histopathological alterations like hepatic vacuolar degeneration and necrosis [51, 60].
Kidney is a multifunctional organ that plays an important role in maintaining homeostasis and excretion of waste products from the body. Being the main site of fluoride accumulation and excretion, it is highly vulnerable to fluoride-induced toxicity [21].The renal dysfunctions have become more prevalent now than ever due to increase in incidence of diseases like diabetes and hypertension coupled with greater exposure to environmental contaminants [61, 62]. Increased plasma KIM-1, BUN, CRE, and UA levels in rats provided with fluoride indicated impairment of renal functions in a dose-dependent manner. The increased BUN, CRE, and UA signaled breakdown of glomerular filtration while raised KIM-1, a type-1 transmembrane protein which is a specific marker expressed on apical surfaces of proximal tubules only in the instances of injury including those mediated by toxicants, suggested significantly diminished proximal renal tubular functioning [63]. These results were further supported by tubular vacuolar degeneration and glomerular damage seen in kidneys of intoxicated rats of our study.
Studies have also shown that sodium fluoride exposure reduces the expression of mitochondrial sirtulin-3 protein, a regulator of the expression of antioxidant enzymes in the kidney which can ultimately induce nephrotoxicity [64]. In the present study, also high fluoride levels reduced the activity of antioxidants in rat kidneys in a dose-dependent manner. The above findings together with significantly higher MDA and AOPP levels in kidneys of our experimental rats indicated fluoride-induced significant renal oxidative damage. Earlier observations have also highlighted that reduction in renal antioxidant system is directly proportional to the levels of fluoride in renal tissue [65]. Histopathologically, the fluoride-mediated oxidative stress brought about extensive glomerular and tubular damage alongside hemorrhage and inflammation in the interstitial tissue which was also manifest through altered biochemical indices. Thus, it can be concluded that upon increased intake, fluoride tends to accumulate in kidneys and can trigger renal failure [17, 66].
In contrast to the high doses of fluoride used in the present study, other researchers noticed renal tubular damage in recently weaned rats at a much lower fluoride concentration (15 ppm), and these changes were not accompanied by any obvious impairment in renal function [67]. The effects of organ damage at lower fluoride administration were not studied in the present work and the higher doses severely impacted renal functioning as reflected by raised plasma renal (KIM-1, BUN, and CR levels) and hepatic biomarkers. The respective levels of fluoride in the liver and kidney in our study were 4.8 and 5 times higher than the corresponding values of the control rats after 100 ppm fluoride administration. The concentration of fluoride in liver was indeed lower than those reported values of fluoride (25 mg F−/L) exposed rats [27].
Nonetheless using a rat model, this work showed that accumulation of fluoride occurred in various organs after chronic exposure to sodium fluoride via drinking water. The distribution of fluoride in these organs correlated well with alterations observed in antioxidant profile and plasma biomarkers indicating organ damage in renal, hepatic, and cardiac tissues was induced. This paper provides a thorough insight into the spectrum of histomorphological changes that could occur in organs such as liver, kidneys, and heart after chronic fluoride exposure. Furthermore, this data can be useful in future toxicant interaction studies and also help find means to counter toxic effects induced by fluoride exposure.
Conclusions
Our results demonstrate that chronic fluoride exposure reduced antioxidant capabilities in the liver, heart, and kidneys. In addition, significant biochemical and histopathological alterations were induced in the liver, kidney, and heart of Wistar rats following chronic fluoride exposure. So, it can be inferred that chronic fluoride toxicity generates oxidative stress which further drives cardiac and hepato-renal dysfunctioning. Therefore, continual fluoride exposure in population residing in endemic fluorosis areas in different parts of the world should be a matter of great concern. Public awareness needs to be created on this aspect and policies should be formulated by the concerned authorities to minimize fluoride exposure among residents of endemic fluorosis localities.
Data Availability
All data generated or analyzed during this study are included in this published article.
Code Availability
Not applicable.
References
Ludlow M, Luxton G, Mathew T (2007) Effects of fluoridation of community water supplies for people with chronic kidney disease. Nephrol Dial Transplant 22:2763–2767. https://doi.org/10.1093/ndt/gfm477
Council NR (2006) Fluoride in drinking water. National Academies Press, Washington, D.C.
Ahmed KM, Bhattacharya P, Hasan MA et al (2004) Arsenic enrichment in groundwater of the alluvial aquifers in Bangladesh: an overview. Appl Geochemistry 19:181–200. https://doi.org/10.1016/j.apgeochem.2003.09.006
Brahman KD, Kazi TG, Afridi HI et al (2013) Evaluation of high levels of fluoride, arsenic species and other physicochemical parameters in underground water of two sub districts of Tharparkar, Pakistan: a multivariate study. Water Res 47:1005–1020. https://doi.org/10.1016/j.watres.2012.10.042
ATSDR (2003) Public health statement: toxicological profile for fluorides, hydrogen fluoride, and fluorine Atlanta. U.S. Department of Health and Human Services, Public Health Service, GA
Srivastava S, Flora SJS (2020) Fluoride in drinking water and skeletal fluorosis: a review of the global impact. Curr Environ Heal reports 7:140–146. https://doi.org/10.1007/s40572-020-00270-9
Samal AC, Bhattacharya P, Mallick A et al (2015) A study to investigate fluoride contamination and fluoride exposure dose assessment in lateritic zones of West Bengal, India. Environ Sci Pollut Res 22:6220–6229. https://doi.org/10.1007/s11356-014-3817-4
Bhattacharya P, Samal AC, Banerjee S et al (2017) Assessment of potential health risk of fluoride consumption through rice, pulses, and vegetables in addition to consumption of fluoride-contaminated drinking water of West Bengal, India. Environ Sci Pollut Res 24:20300–20314. https://doi.org/10.1007/s11356-017-9649-2
Bhattacharya P, Adhikari S, Samal AC et al (2020) Health risk assessment of co-occurrence of toxic fluoride and arsenic in groundwater of Dharmanagar region, North Tripura (India). Groundw Sustain Dev 11:100430. https://doi.org/10.1016/j.gsd.2020.100430
Demelash H, Beyene A, Abebe Z, Melese A (2019) Fluoride concentration in ground water and prevalence of dental fluorosis in Ethiopian Rift Valley: systematic review and meta-analysis. BMC Public Health 19:1298. https://doi.org/10.1186/s12889-019-7646-8
García-Pérez A, Pérez-Pérez NG, Flores-Rojas AI et al (2020) Marginalization and fluorosis its relationship with dental caries in rural children in Mexico: a cross-sectional study. Community Dent Health 37:216–222. https://doi.org/10.1922/CDH_00017Perez07
Nopakun J, Messer HH, Voller V (1989) Fluoride absorption from the gastrointestinal tract of rats. J Nutr 119:1411–1417. https://doi.org/10.1093/jn/119.10.1411
Buzalaf MAR, Whitford GM (2011) Fluoride metabolism. In: Monographs in Oral Science. Karger Publishers, pp 20–36
Dharmaratne RW (2019) Exploring the role of excess fluoride in chronic kidney disease: a review. Hum Exp Toxicol 38:269–279. https://doi.org/10.1177/0960327118814161
Perera T, Ranasinghe S, Alles N, Waduge R (2018) Effect of fluoride on major organs with the different time of exposure in rats. Environ Health Prev Med 23:17. https://doi.org/10.1186/s12199-018-0707-2
Santoyo-Sanchez MP, Del Carmen S-L, Arreola-Mendoza L, Barbier OC (2013) Effects of acute sodium fluoride exposure on kidney function, water homeostasis, and renal handling of calcium and inorganic phosphate. Biol Trace Elem Res 152:367–372. https://doi.org/10.1007/s12011-013-9622-y
Malin AJ, Lesseur C, Busgang SA, et al (2019) Fluoride exposure and kidney and liver function among adolescents in the United States: NHANES, 2013–2016. Environ Int 132: https://doi.org/10.1016/j.envint.2019.105012
Basha M, Sujitha N (2011) Chronic fluoride toxicity and myocardial damage: antioxidant offered protection in second generation rats. Toxicol Int 18:99. https://doi.org/10.4103/0971-6580.84260
Varol E, Varol S (2012) Effect of fluoride toxicity on cardiovascular systems: role of oxidative stress. Arch Toxicol 86:1627–1627. https://doi.org/10.1007/s00204-012-0862-y
Lopes GO, Ferreira MKM, Davis L et al (2020) Effects of fluoride long-term exposure over the cerebellum: global proteomic profile, oxidative biochemistry, cell density, and motor behavior evaluation. Int J Mol Sci 21:1–20. https://doi.org/10.3390/ijms21197297
Chattopadhyay A, Podder S, Agarwal S, Bhattacharya S (2011) Fluoride-induced histopathology and synthesis of stress protein in liver and kidney of mice. Arch Toxicol 85:327–335. https://doi.org/10.1007/s00204-010-0588-7
Kazory A, Ronco C (2019) Hepatorenal syndrome or hepatocardiorenal syndrome: revisiting basic concepts in view of emerging data. Cardiorenal Med 9:1–7. https://doi.org/10.1159/000492791
Karaoz E, Oncu M, Gulle K et al (2004) Effect of chronic fluorosis on lipid peroxidation and histology of kidney tissues in first- and second-generation rats. Biol Trace Elem Res 102:199–208. https://doi.org/10.1385/BTER:102:1-3:199
Council NR (1993) Health effects of ingested fluoride. National Academies Press, Washington, D.C.
Ahmad KR, Noor S, Jabeen S et al (2017) Amelioration by jambul fruit extract of fluoride-induced hepato-nephronal histopathologies and impaired neuromotor capacity in mice. Fluoride 50:2–14
Inkielewicz I, Krechniak J (2003) Fluoride content in soft tissues and urine of rats exposed to sodium fluoride in drinking water. Fluoride 36:263–266
Inkielewicz I, Czarnowski W, Krechniak J (2003) Determination of fluoride in soft tissues. Fluoride 36:16–20
Mochnik PA, Frei B, Ames BN (1994) [23] Measurement of antioxidants in human blood plasma. In: Methods in Enzymology. Methods Enzymol, pp 269–279
Aebi H (1974) Catalase. In: Methods of Enzymatic Analysis. Elsevier, pp 673–684
Marklund S, Marklund G (1974) Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase. Eur J Biochem 47:469–474. https://doi.org/10.1111/j.1432-1033.1974.tb03714.x
Hafeman DG, Sunde RA, Hoekstra WG (1974) Effect of dietary selenium on erythrocyte and liver glutathione peroxidase in the rat. J Nutr 104:580–587. https://doi.org/10.1093/jn/104.5.580
Carlberg I, Mannervik B (1985) [59] Glutathione reductase. Methods Enzymol 113:484–490. https://doi.org/10.1016/S0076-6879(85)13062-4
Voss G, Sachsse K (1970) Red cell and plasma cholinesterase activities in microsamples of human and animal blood determined simultaneously by a modified acetylthiocholine/DTNB procedure. Toxicol Appl Pharmacol 16:764–772. https://doi.org/10.1016/0041-008X(70)90082-7
Burlina A, Michielin E, Galzigna L (1977) Characteristics and behaviour of arylesterase in human serum and liver. Eur J Clin Invest 7:17–20. https://doi.org/10.1111/j.1365-2362.1977.tb01564.x
Shafiq-Ur-Rehman (1984) Lead-induced regional lipid peroxidation in brain. Toxicol Lett 21:333–7
Witko-Sarsat V, Friedlander M, Capeillère-Blandin C et al (1996) Advanced oxidation protein products as a novel marker of oxidative stress in uremia. Kidney Int 49:1304–1313. https://doi.org/10.1038/ki.1996.186
Drury, R.A.B WEA (1980) Carleton’s histological technique. (1980 edition) | Open Library
Strunecka A, Strunecky O (2020) Mechanisms of fluoride toxicity: from enzymes to underlying integrative networks. Appl Sci 10:1–24
Bharti VK, Srivastava RS (2009) Fluoride-induced oxidative stress in rat’s brain and its amelioration by buffalo (bubalus bubalis) pineal proteins and melatonin. Biol Trace Elem Res 130:131–140. https://doi.org/10.1007/s12011-009-8320-2
Jothiramajayam M, Sinha S, Ghosh M et al (2014) Sodium fluoride promotes apoptosis by generation of reactive oxygen species in human lymphocytes. J Toxicol Environ Heal - Part A Curr Issues 77:1269–1280. https://doi.org/10.1080/15287394.2014.928658
Agalakova NI, Gusev GP (2012) Molecular mechanisms of cytotoxicity and apoptosis induced by inorganic fluoride. ISRN Cell Biol 2012:1–16. https://doi.org/10.5402/2012/403835
Yan X, Yang X, Hao X et al (2015) Sodium fluoride induces apoptosis in H9c2 cardiomyocytes by altering mitochondrial membrane potential and intracellular ROS level. Biol Trace Elem Res 166:210–215. https://doi.org/10.1007/s12011-015-0273-z
Sharma P, Verma PK, Sood S, et al (2021) Distribution of fluoride in plasma, brain, and bones and associated oxidative damage after induced chronic fluorosis in Wistar rats. Biol Trace Elem Res 1–12. https://doi.org/10.1007/s12011-021-02782-3
Arulkumar M, Vijayan R, Penislusshiyan S et al (2017) Alteration of paraoxonase, arylesterase and lactonase activities in people around fluoride endemic area of Tamil Nadu, India. Clin Chim Acta 471:206–215. https://doi.org/10.1016/j.cca.2017.05.036
Kant V, Srivastava AK, Verma PK, Raina R (2009) Alterations in biochemical parameters during subacute toxicity of fluoride alone and in conjunction with aluminum sulfate in goats. Biol Trace Elem Res 130:20–30. https://doi.org/10.1007/s12011-008-8311-8
Raina R, Baba NA, Verma PK et al (2015) Hepatotoxicity induced by subchronic exposure of fluoride and chlorpyrifos in Wistar rats: mitigating effect of ascorbic acid. Biol Trace Elem Res 166:157–162. https://doi.org/10.1007/s12011-015-0263-1
Adali MK, Varol E, Aksoy F et al (2013) Impaired heart rate recovery in patients with endemic fluorosis. Biol Trace Elem Res 152:310–315. https://doi.org/10.1007/s12011-013-9627-6
O’Toole TE, Conklin DJ, Bhatnagar A (2008) Environmental risk factors for heart disease. Rev Environ Health 23:167–202. https://doi.org/10.1515/REVEH.2008.23.3.167
Parveen A, Babbar R, Agarwal S et al (2011) Mechanistic clues in the cardioprotective effect of terminalia arjuna bark extract in isoproterenol-induced chronic heart failure in rats. Cardiovasc Toxicol 11:48–57. https://doi.org/10.1007/s12012-010-9099-2
Wang J, Yang J, Cheng X et al (2019) Calcium alleviates fluoride-induced bone damage by inhibiting endoplasmic reticulum stress and mitochondrial dysfunction. J Agric Food Chem 67:10832–10843. https://doi.org/10.1021/acs.jafc.9b04295
Zhou B Hua, Zhao J, Liu J, et al (2015) Fluoride-induced oxidative stress is involved in the morphological damage and dysfunction of liver in female mice. Chemosphere 139:504–511. https://doi.org/10.1016/j.chemosphere.2015.08.030
Ma Y, Niu R, Sun Z et al (2012) Inflammatory responses induced by fluoride and arsenic at toxic concentration in rabbit aorta. Arch Toxicol 86:849–856. https://doi.org/10.1007/s00204-012-0803-9
Li Y, Berenji GR, Shaba WF et al (2012) Association of vascular fluoride uptake with vascular calcification and coronary artery disease. Nucl Med Commun 33:14–20. https://doi.org/10.1097/MNM.0b013e32834c187e
Mujahid M, Ramaswamy C, Shanthi Naidu K, Shobha M (2015) Effect of fluoride induced toxicity on cardiac tissue: possible role of oxidative stress in degenerative changes of cardiac tissue. Res J Pharm Biol Chem Sci 6:333–338
Akinrinde AS, Tijani M, Awodele OA, Oyagbemi AA (2021) Fluoride-induced hepatotoxicity is prevented by L-arginine supplementation via suppression of oxidative stress and stimulation of nitric oxide production in rats. Toxicol Environ Health Sci 13:57–64. https://doi.org/10.1007/s13530-020-00070-6
Verma PK, Raina R, Sultana M et al (2016) Acetaminophen induced oxidative and histopathological alterations in hepatic tissue: protective effects of Alstonia scholaris leaf extracts. Pharmacogn J 8:385–391. https://doi.org/10.5530/pj.2016.4.12
Xiong X, Liu J, He W et al (2007) Dose–effect relationship between drinking water fluoride levels and damage to liver and kidney functions in children. Environ Res 103:112–116. https://doi.org/10.1016/j.envres.2006.05.008
Liu Y, O′flaherty C (2017) In vivo oxidative stress alters thiol redox status of peroxiredoxin 1 and 6 and impairs rat sperm quality. Asian J Androl 19:73–79. https://doi.org/10.4103/1008-682X.170863
Zhang Z, Zhou B, Wang H et al (2014) Maize purple plant pigment protects against fluoride-induced oxidative damage of liver and kidney in rats. Int J Environ Res Public Health 11:1020–1033. https://doi.org/10.3390/ijerph110101020
Lu Y, Luo Q, Cui H, et al (2017) Sodium fluoride causes oxidative stress and apoptosis in the mouse liver. Aging (Albany NY) 9:1623–1639. https://doi.org/10.18632/aging.101257
Guo X, ying, Sun G fan, Sun Y chun, (2003) Erratum: Oxidative stress from fluoride-induced hepatotoxicity in rats (Flouride (2003) 36:1 (25–29)). Fluoride 36:83
Khan AM, Raina R, Dubey N, Verma PK (2018) Effect of deltamethrin and fluoride co-exposure on the brain antioxidant status and cholinesterase activity in Wistar rats. Drug Chem Toxicol 41:123–127. https://doi.org/10.1080/01480545.2017.1321009
Bonventre JV (2008) Kidney injury molecule-1 (KIM-1): a specific and sensitive biomarker of kidney injury. Scand J Clin Lab Invest 68:78–83. https://doi.org/10.1080/00365510802145059
Song C, Fu B, Zhang J et al (2017) Sodium fluoride induces nephrotoxicity via oxidative stress-regulated mitochondrial SIRT3 signaling pathway. Sci Rep 7:672. https://doi.org/10.1038/s41598-017-00796-3
Zhan XA, Li JX, Wang M, Xu ZR (2006) Effects of fluoride on growth and thyroid function in young pigs. Fluoride 39:95–100
Waikar SS, Sabbisetti V, Ärnlöv J et al (2016) Relationship of proximal tubular injury to chronic kidney disease as assessed by urinary kidney injury molecule-1 in five cohort studies. Nephrol Dial Transplant 31:1460–1470. https://doi.org/10.1093/ndt/gfw203
Cárdenas-González MC, Del Razo LM, Barrera-Chimal J et al (2013) Proximal renal tubular injury in rats sub-chronically exposed to low fluoride concentrations. Toxicol Appl Pharmacol 272:888–894. https://doi.org/10.1016/j.taap.2013.07.026
Acknowledgements
The authors thank the Dean, Faculty of Veterinary Science and Animal Husbandry, R S Pura, Jammu, for providing necessary facilities for conducting the research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Dr Priyanka Sharma and Dr Pawan Kumar Verma contributed to the conception, design, and execution of the research work to generate the basic data. Dr Shilpa Sood carried out histopathological work and final editing of the manuscript. Dr Maninder Singh and Ms Deepika contributed to the statistical analysis of data.
Corresponding author
Ethics declarations
Ethics Approval
The experimental protocol was duly approved by Institutional Animal Ethics Committee (IAEC) vide letter no. 09/IAEC/2020 dated 22/10/2020.
Consent to Participate
Not applicable.
Consent for Publication
All authors are agreed to publication of article.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, P., Verma, P.K., Sood, S. et al. Impact of Chronic Sodium Fluoride Toxicity on Antioxidant Capacity, Biochemical Parameters, and Histomorphology in Cardiac, Hepatic, and Renal Tissues of Wistar Rats. Biol Trace Elem Res 201, 229–241 (2023). https://doi.org/10.1007/s12011-022-03113-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03113-w