Abstract
Background/Objective
The effect of bariatric surgery in renal function varies and the postoperative benefit time point remains unclear. We aim to assess the changes of renal function after bariatric surgery (BS) in different postoperative periods and subgroups.
Methods
We searched the databases of PubMed and Cochrane from inception to December 14, 2020. Articles included in the study were drawn from all recipients of BS that provided assessments of renal function pre and post-surgery. Meta-analysis was performed to compare glomerular filtration rate (GFR), serum creatinine, albumin-to-creatinine ratio (ACR), and albuminuria before and after BS.
Results
The study included 49 articles involving 8515 patients. Compared with pre-operative renal function, the overall analysis showed that bariatric surgery significantly reduced serum creatinine levels, ACR, and albuminuria. There was significant increase of GFR in the CKD subgroup, yet a noticeable decrease in the hyperfiltration subgroup. The most significant improvement in GFR was seen 6–12 months after BS, while ACR dropped most dramatically 12–24 months after BS.
Conclusions
Bariatric surgery can improve renal function in obese patients with kidney dysfunction, especially 1 year after surgery.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a serious risk factor for the occurrence and development of chronic kidney disease (CKD). Obesity not only indirectly increases the risk of CKD through diabetes and hypertension, but also directly affects renal function and structure [1]. The high filtration rate caused by obesity gradually decreased, along with the development of obesity-related renal damaged, and eventually developed into end-stage renal disease [2]. In the setting of obesity, the main clinical manifestations of kidney disease were proteinuria, albuminuria, hyperfiltration, or decreased glomerular filtration rate [3].
Bariatric surgery is one of the most effective treatments to maintain long-term weight loss. The obesity-related complications are significantly improved after BS such as hypertension, dyslipidemia, and diabetic complications and and [4,5,6]. The improvement of these complications will have a positive effect on the kidney theoretically. Several previous studies have also showed that BS can improve renal function [7,8,9]. However, in other studies, BS is regarded as a risk factor to acute kidney damage and is associated with hyperoxaluria which can lead to kidney stone formation and renal insufficiency [10, 11]. Therefore, the effect of bariatric surgery on renal function remains controversial.
There are some previous meta-analysis of the effect of BS on renal function. However, these studies were limited to the analysis of single renal function indicators or specific patients such as patients with T2D or CKD [12,13,14]. Moreover, these meta-reviews did not compare the impact of bariatric surgery on renal function between different BS methods or different follow-up stages. Several important studies with larger sample size were reported recently regarding the changes in pre- and post-operative renal function, which may provide further evidence for the influence of BS on renal function [9, 15,16,17,18]. Therefore, we included the latest relevant literature and more evaluation index of renal function to conduct a more comprehensive meta-analysis of the influence of BS on renal function.
Materials and Methods
Search Strategy
Two authors independently searched published studies indexed in the databases of PubMed and Cochrane from inception to December 14, 2020. The search keywords are as follows: bariatric surgery, metabolic surgery, gastric bypass, gastric banding, Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), renal function, renal outcomes, glomerular filtration rate, serum creatinine, creatinine clearance, albuminuria, 24-h urine albumin excretion rate, and urine albumin-to-creatinine ratio.
Study Selection
We screened all the articles that participants received bariatric surgery and reported renal function indexes before and after surgery. The renal function indexes included GFR, serum creatinine, albuminuria, and ACR. The bariatric surgery mainly included RYGB and SG, but not limited to these two types of surgery. The patients did not have specific limits if the participants met the bariatric surgical indications. Reviews, case reports, or meta-analysis was excluded. Articles that had no follow-up rate, no available data, or based on the same study population were excluded.
Data Extraction and Synthesis
This review included all published randomized controlled trials or observational studies that assessed the change of GFR, serum creatinine, albuminuria, and ACR after BS. The pre- and post-surgery mean values with standard deviation (or standard error) of those renal function indexes were collected and included in the analysis. The continuous data provided in some studies were median and interquartile ranges, which were inconsistent with other articles, so they were not included in the analysis. For articles that reported renal function indexes at multiple follow-up time, we selected the data of the longest follow-up to analysis; only in subgroup analysis based on different follow-up periods after bariatric surgery, we included the date of all follow-up time reported in the article. The information of study design, baseline clinical characteristics of the study population, type of surgery, and duration of follow-up were extracted in all included articles.
Quality Assessment
Two authors assessed the study quality for all included observational studies using the Newcastle–Ottawa scale (NOS). A total score of 3 or less was considered poor quality. We excluded studies from our meta-analysis if they had poor quality. Discrepant opinions were resolved by consultation between all authors.
Statistical Analysis
All statistical analyses were performed using ReviewManager version 5.3. We used a random-effects model for meta-analysis and expressed treatment effects as a risk ratio with 95% confidence intervals (CI) for dichotomous outcomes and mean difference with 95% CI for continuous outcomes. An I2 > 50% indicated a large heterogeneity not explained by chance.
Results
Description of Included Studies
1585 studies were cited as relevant articles after database searching. Repeated, unreported renal function, case reports, reviews, or meta-analysis was excluded after reading the title and abstract. Sixty-one articles were screened for intensive reading. Twelve articles were excluded because of no follow-up rate, no available data, or based on the same study population. Finally, 49 studies were incorporated into the meta-analysis [7,8,9, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. A flow diagram displaying the process of selecting the included studies is illustrated in Fig. 1. And the baseline study and patients’ characteristics are outlined in Table 1.
Quality Assessment of Included Studies
Newcastle–Ottawa scale was used to evaluate the quality of the included studies. Total score of each document ranges from 4 to 9. And the total score of all studies was not less than 3 (3 represents low quality). Totally 49 studies were all incorporated into the meta-analysis.
Meta-analysis Results
GFR
GFR was assessed in 33 out of 49 studies pre- and post-operative; 6 articles were excluded because their results were inconsistent with other studies. GFR increased after BS in 22 out of 27 studies, while decreased in the remaining 5 studies. Twenty-seven studies involving 3157 patients were integrated into meta-analysis of GFR. There was no significant difference in GFR changes after BS in the analysis between the overall group (MD, 3.08 ml/min/1.73 m2; 95% CI, − 1.35 to + 7.52 ml/min/1.73 m2) and the normal GFR subgroup (90 ≤ GFR ≤ 120) (MD, 0.44 ml/min/1.73 m2; 95% CI, − 3.46 to + 4.35 ml/min/1.73 m2) (Fig. 2). However, with GFR < 90 subgroup (CDK subgroup), the post-operative GFR increased by 13.81 ml/min/1.73 m2 (95% CI, 10.31 to 17.32 ml/min/1.73 m2). For the GFR > 120 subgroup (hyperfiltration subgroup), the post-operative GFR decreased by 9.61 (95% CI, − 16.31 to − 2.91 ml/min/1.73 m2) (Fig. 2). Also, there was no statistically significant of the pre- and post-operative changes in GFR, with or without diabetes, no matter how the surgical technique (RYGB, SG, or LAGB) had been taken (Supplemental Fig. 1). There was a biggest increase of GFR (MD 14.27 ml/min/1.73 m2) in 6–12 months after BS. Post-operative GFR of 6 months, 2 years, and 5–10 years increased 9.53, 7.37, and 6.02 ml/min/1.73 m2, respectively (Fig. 7A and Supplemental Fig. 2).
Serum Creatinine
A total of 33 studies reported before-and-after changes on serum creatinine; 5 articles were excluded due to their data were not compatible with other studies. The concentration of serum creatinine decreased in the overall group after BS (MD, − 0.07 mg/dl; 95% CI, − 0.09 to − 0.05 mg/dl). Only GFR > 90 subgroup (no CKD subgroup), serum creatinine increased by 0.02 mg/dl (95% CI, 0.00 to + 0.04 mg/dl) (Fig. 3). Compared with RYGB (MD, − 0.08 mg/dl; 95% CI, − 0.15 to 0.00 mg/dl), SG (MD, − 0.13 mg/dl; 95% CI, − 0.18 to − 0.08 mg/dl) has better effect in reducing serum creatinine (Supplemental Fig. 3). There was no significant difference in pre- and post-operative changes of serum creatinine between the two groups of patients with and without diabetes (Supplemental Fig. 3). Although creatinine dropped the most in 3–5 years after BS (MD, − 0.11 mg/dl; 95% CI, − 0.16 to − 0.07 mg/dl), it was no significantly decrease (p = 0.27) in the following period: 6 months (MD, − 0.08 mg/dl; 95% CI, − 0.12 to − 0.04 mg/dl), 1 year (MD, − 0.06 mg/dl; 95% CI, − 0.09 to − 0.03 mg/dl), or 2 years follow-up (MD, − 0.06 mg/dl; 95% CI, − 0.14 to − 0.03 mg/dl) (Fig. 7B and Supplemental Fig. 4).
ACR
Only 8 studies with available data were for ACR out of 49 included studies. ACR be slightly increased in 2 out of 8 studies, while reduced in the remaining 6 studies. It had been decreased in the overall group (MD, − 12.46 mg/g; 95% CI, − 20.11 to − 4.82 mg/g) (Fig. 4) and all subgroups after BS. Reductions in ACR were seen after RYGB or SG and in patients with or without diabetes (Supplemental Fig. 5). There was no significant difference in pre- and post-operative changes of ACR for all subgroups. It also declined most significantly at 1 year (MD, − 18.03 mg/g; 95% CI, − 27.35 to − 8.71 mg/g) and 2 years (MD, − 18.20 mg/g; 95% CI, − 29.20 to − 7.19 mg/g) after BS (Fig. 7C and Supplemental Fig. 6).
Albuminuria
Twenty-three out of 49 studies had albuminuria inspection pre- and post-operative. It had significantly improved in all other studies except for one that did not change. There was a statistically significant reduction in the incidence of albuminuria after bariatric surgery (RR: 0.40, 95% CI: 0.31–0.51, p < 0.0001; I2 = 71%) (Fig. 5). A decrease in albuminuria was noted after BS (MD, − 14.17 mg/day; 95% CI, − 22.59 to − 5.76 mg/day) (Fig. 6).
Discussion
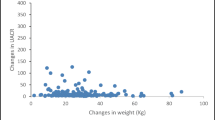
Evidence from this meta-analysis shows an improvement in renal function after bariatric surgery. First, although the change of GFR was inconsistent in all included studies, it decreased in patients with hyperfiltration while increased in patients with reduced eGFR (CKD). Second, serum creatinine level decreased significantly after BS in the overall group, while it increased slightly in the subgroup with GFR > 90. But it still keeps in the normal range. Third, data on changes pre- and post-operative indicated that ACR and albuminuria decreased significantly after bariatric surgery. Fourth, renal function improved the most in 1–2 years after bariatric surgery (Fig. 7).
The changes of renal function after bariatric surgery in different postoperative periods. A The GFR difference of preoperative and postoperative in different periods. B The creatinine difference of preoperative and postoperative in different periods. C The ACR difference of preoperative and postoperative in different periods
GFR is the product of functional nephrons’ quantity which remains constant after birth and the filtration rate of single nephron [62]. Healthy kidney has functional renal reserve, i.e., not all nephrons are activated in normal physiological states. And some nephrons are in idle state [63]. Early obesity leads to the decrease of functional renal reserve which activated the motionless nephrons. It makes the body show hyperfiltration [64]. Nevertheless, long-term hyperfiltration will reduce the filtration of single nephron declining the total GFR, and eventually leads to kidney damage [65]. Therefore, hyperfiltration may be reversible because of the renal functional reserve. Whether the decrease or increase in post-operative GFR results from an improvement in hyperfiltration or a real renal function is uncertain. It is illogical to judge the effect of bariatric surgery on renal function only based on the rising and falling of GFR. For obese patients with normal renal reserve function, bariatric surgery was initially to redress the hyperfiltration caused by obesity and maintain the normal number of activated nephrons. So, GFR showed a downward tendency. For patients who activated all nephrons with renal insufficiency and reserve function dysfunction, in this condition, the effect of bariatric surgery on renal function can be truly reflected from the change of total GFR. And the increase in total GFR is necessarily the result of the growing of filtration rate of single nephron. Our meta-analysis demonstrates that bariatric surgery can reduce the GFR of patients with hyperfiltration and increase the GFR of patients with renal insufficiency, which is the favorable evidence for bariatric surgery to enhance renal function.
Serum creatinine levels are usually relatively normal due to renal reserve function until about 50% of nephrons be invalidated or GFR drops to nearly 60 ml/min/1.73 m2 [66]. Therefore, when GFR > 60 ml/min/1.73 m2, serum creatinine is not an accurate indicator of renal function. But the level of serum creatinine to some extent reflects the capability of the kidney to clean up metabolic waste. Serum creatinine is maintained at a normal level, indicating that the renal clearance function can meet the metabolic needs. Moreover, creatinine-based eGFR is not validated in obese individuals because of high muscle quality, which may underestimate renal function in obese individuals [67]. Hence, it is more convincing that the decrease of creatinine level reflects the improvement in renal clearance after BS.
Albuminuria closely relating to all levels of renal function is an important manifestation of renal function damage. There is no question that microalbuminuria is improved after bariatric surgery, whether post-operative remission of pre-operative albuminuria or new onset albuminuria. Compared with non-surgical control group, the post-operative microalbuminuria in the operation group reduced significantly after BS. Our results are consistent with previous studies that the incidence of albuminuria, microalbuminuria level, and uACR decreased after BS.
The weight loss caused by BS is the most significant 1 year after operation. Then, the weight regained in different degrees. The optimal benefit time of bariatric surgery on renal function, however, has not been studied. This study first conducts subgroup analysis based on different follow-up periods after bariatric surgery. Considering the early decline of GFR due to improvement of hyperfiltration in patients with preserved renal reserve function, we only included patients with renal insufficiency (GFR < 90) at baseline in the follow-up subgroup analysis of GFR. The maximum increase of GFR is noted during 6–12 months after BS. And serum creatinine achieved the most noticeable decrease in 3–5 years after BS (although no significant difference). These are inconsistent with the trajectory of weight loss after BS. So, it has yet to be further proved that bariatric surgery can not only benefit from weight loss, but also enhance renal function through other mechanisms.
Our research has some limitations. First, the study is disunity in various literature on the measurement of GFR and whether the GFR is adjusted according to the surface area. Secondly, it is the innovation of this study to explore the optimal benefit time point of renal function after bariatric surgery based on subgroup analysis of follow-up time, but more intuitive research is needed to verify the trajectory of renal function after bariatric surgery. Finally, the conclusion of our article has limited effect, because the included articles are mostly observational single-arm studies and have significant heterogeneity.
Conclusion
Bariatric surgery can improve renal function in obese patients with kidney dysfunction, it reduces the GFR of patients with hyperfiltration and increase the GFR of patients with renal insufficiency, and the incidence of albuminuria, microalbuminuria level, and uACR decrease after BS. In the future, more intuitive research is needed to investigate the trajectory of renal function after bariatric surgery to verify the optimal postoperative benefit time.
Change history
07 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11695-021-05699-x
References
Yun HR, et al. Obesity, metabolic abnormality, and progression of CKD. Am J Kidney Dis. 2018;72(3):400–10.
Silva Junior GB, et al. Obesity and kidney disease. J Bras Nefrol. 2017;39(1):65–9.
Xu T, Sheng Z, Yao L. Obesity-related glomerulopathy: pathogenesis, pathologic, clinical characteristics and treatment. Front Med. 2017;11(3):340–8.
Owen JG, Yazdi F, Reisin E. Bariatric surgery and hypertension. Am J Hypertens. 2017;31(1):11–7.
Climent E, et al. Atherogenic dyslipidemia remission 1 year after bariatric surgery. Obes Surg. 2017;27(6):1548–53.
Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–55.
Holcomb CN, et al. Bariatric surgery is associated with renal function improvement. Surg Endosc. 2018;32(1):276–81.
Kim EY, Kim YJ. Does bariatric surgery really prevent deterioration of renal function? Surg Obes Relat Dis. 2016;12(4):856–61.
Saeed K, et al. Bariatric surgery improves renal function: a large inner-city population outcome study. Obes Surg. 2021;31(1):260–6.
Carbone A, et al. Obesity and kidney stone disease: a systematic review. Minerva Urol Nefrol. 2018;70(4):393–400.
Monda S, et al. The risks of stone diagnosis and stone removal procedure after different bariatric surgeries. J Endourol. 2021;35(5):674–81.
Zhou X, et al. Impact of bariatric surgery on renal functions in patients with type 2 diabetes: systematic review of randomized trials and observational studies. Surg Obes Relat Dis. 2016;12(10):1873–82.
Li K, et al. Effects of bariatric surgery on renal function in obese patients: a systematic review and meta analysis. PLoS One. 2016;11(10):e0163907.
Upala S, et al. Bariatric surgery reduces urinary albumin excretion in diabetic nephropathy: a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12(5):1037–44.
Shulman A, et al. Remission and progression of pre-existing micro- and macroalbuminuria over 15 years after bariatric surgery in Swedish obese subjects study. Int J Obes (Lond). 2021;45(3):535–46.
Bjornstad P, et al. Five-year kidney outcomes of bariatric surgery differ in severely obese adolescents and adults with and without type 2 diabetes. Kidney Int. 2020;97(5):995–1005.
McIsaac M, et al. Long-term impact of bariatric surgery on renal outcomes at a community-based publicly funded bariatric program: the Regina bariatric study. Can J Kidney Health Dis. 2019;6:2054358119884903.
Friedman AN, et al. The association between kidney disease and diabetes remission in bariatric surgery patients with type 2 diabetes. Am J Kidney Dis. 2019;74(6):761–70.
Khalil R, et al. Kidney injury molecule-1: a potential marker of renal recovery after laparoscopic sleeve gastrectomy. Kidney Res Clin Pract. 2020;39(2):162–71.
Brix JM, et al. Albuminuria in patients with morbid obesity and the effect of weight loss following bariatric surgery. Obes Surg. 2019;29(11):3581–8.
Young L, et al. Long-term impact of bariatric surgery in diabetic nephropathy. Surg Endosc. 2019;33(5):1654–60.
Park S, et al. Bariatric surgery can reduce albuminuria in patients with severe obesity and normal kidney function by reducing systemic inflammation. Obes Surg. 2018;28(3):831–7.
Billeter AT, et al. Renal function in type 2 diabetes following gastric bypass. Dtsch Arztebl Int. 2016;113(49):827–33.
Nehus EJ, et al. Kidney outcomes three years after bariatric surgery in severely obese adolescents. Kidney Int. 2017;91(2):451–8.
Neff KJ, et al. Renal function and remission of hypertension after bariatric surgery: a 5-year prospective cohort study. Obes Surg. 2017;27(3):613–9.
Garcia MS, et al. Renal function 1 year after bariatric surgery: influence of Roux-en-Y gastric bypass and identification of pre-operative predictors of improvement. Obes Surg. 2020;30(3):860–6.
Solini A, et al. Renal resistive index predicts post-bariatric surgery renal outcome in nondiabetic individuals with severe obesity. Obesity (Silver Spring). 2019;27(1):68–74.
Hung KC, et al. Impact of serum uric acid on renal function after bariatric surgery: a retrospective study. Surg Obes Relat Dis. 2020;16(2):288–95.
Hou CC, et al. Improved renal function 12 months after bariatric surgery. Surg Obes Relat Dis. 2013;9(2):202–6.
Mirajkar N, et al. The impact of bariatric surgery on estimated glomerular filtration rate in patients with type 2 diabetes: a retrospective cohort study. Surg Obes Relat Dis. 2016;12(10):1883–9.
Reid TJ, et al. The effect of bariatric surgery on renal function. Surg Obes Relat Dis. 2014;10(5):808–13.
Fenske WK, et al. Effect of bariatric surgery-induced weight loss on renal and systemic inflammation and blood pressure: a 12-month prospective study. Surg Obes Relat Dis. 2013;9(4):559–68.
Navaneethan SD, Yehnert H. Bariatric surgery and progression of chronic kidney disease. Surg Obes Relat Dis. 2009;5(6):662–5.
De Paula AL, et al. Prospective randomized controlled trial comparing 2 versions of laparoscopic ileal interposition associated with sleeve gastrectomy for patients with type 2 diabetes with BMI 21–34 kg/m(2). Surg Obes Relat Dis. 2010;6(3):296–304.
Zakaria AS, et al. Effects of gastric banding on glucose tolerance, cardiovascular and renal function, and diabetic complications: a 13-year study of the morbidly obese. Surg Obes Relat Dis. 2016;12(3):587–95.
Ngoh CLY, et al. Effect of weight loss after bariatric surgery on kidney function in a multiethnic Asian population. Surg Obes Relat Dis. 2016;12(3):600–5.
Miras AD, et al. Type 2 diabetes mellitus and microvascular complications 1 year after Roux-en-Y gastric bypass: a case-control study. Diabetologia. 2015;58(7):1443–7.
Chagnac A, et al. The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol. 2003;14(6):1480–6.
Zhang H, et al. The short-term remission of diabetic nephropathy after Roux-en-Y gastric bypass in Chinese patients of T2DM with obesity. Obes Surg. 2015;25(7):1263–70.
Stephenson DT, et al. Improvement in albuminuria in patients with type 2 diabetes after laparoscopic adjustable gastric banding. Diab Vasc Dis Res. 2013;10(6):514–9.
Abouchacra S, et al. GFR estimation in the morbidly obese pre- and postbariatric surgery: one size does not fit all. Int Urol Nephrol. 2013;45(1):157–62.
Amor A, et al. Weight loss independently predicts urinary albumin excretion normalization in morbidly obese type 2 diabetic patients undergoing bariatric surgery. Surg Endosc. 2013;27(6):2046–51.
DePaula AL, et al. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg Endosc. 2009;23(6):1313–20.
Getty JL, et al. Changes in renal function following Roux-en-Y gastric bypass: a prospective study. Obes Surg. 2012;22(7):1055–9.
Saliba J, et al. Roux-en-Y gastric bypass reverses renal glomerular but not tubular abnormalities in excessively obese diabetics. Surgery. 2010;147(2):282–7.
Zeve JL, et al. Obese patients with diabetes mellitus type 2 undergoing gastric bypass in Roux-en-Y: analysis of results and its influence in complications. Arq Bras Cir Dig. 2013;26(Suppl 1):47–52.
Luaces M, et al. The impact of bariatric surgery on renal and cardiac functions in morbidly obese patients. Nephrol Dial Transplant. 2012;27(Suppl 4): iv53–7.
Jose B, et al. The effect of biliopancreatic diversion surgery on renal function—a retrospective study. Obes Surg. 2013;23(5):634–7.
Mohan S, et al. Early improvement in albuminuria in non-diabetic patients after Roux-en-Y bariatric surgery. Obes Surg. 2012;22(3):375–80.
Navaneethan SD, et al. Urinary albumin excretion, HMW adiponectin, and insulin sensitivity in type 2 diabetic patients undergoing bariatric surgery. Obes Surg. 2010;20(3):308–15.
Friedman AN, et al. Predicting the glomerular filtration rate in bariatric surgery patients. Am J Nephrol. 2014;39(1):8–15.
Lieske JC, et al. Gastric bypass surgery and measured and estimated GFR in women. Am J Kidney Dis. 2014;64(4):663–5.
Ruiz-Tovar J, et al. Laparoscopic sleeve gastrectomy prevents the deterioration of renal function in morbidly obese patients over 40 years. Obes Surg. 2015;25(5):796–9.
Navarro-Diaz M, et al. Effect of drastic weight loss after bariatric surgery on renal parameters in extremely obese patients: long-term follow-up. J Am Soc Nephrol. 2006;17(12 Suppl 3):S213–7.
Palomar R, et al. Effects of weight loss after biliopancreatic diversion on metabolism and cardiovascular profile. Obes Surg. 2005;15(6):794–8.
Iaconelli A, et al. Effects of bilio-pancreatic diversion on diabetic complications: a 10-year follow-up. Diabetes Care. 2011;34(3):561–7.
Heneghan HM, et al. Effects of bariatric surgery on diabetic nephropathy after 5 years of follow-up. Surg Obes Relat Dis. 2013;9(1):7–14.
Celik F, et al. The longer-term effects of Roux-en-Y gastric bypass surgery on sodium excretion. Obes Surg. 2013;23(3):358–64.
Schuster DP, et al. Effect of bariatric surgery on normal and abnormal renal function. Surg Obes Relat Dis. 2011;7(4):459–64.
Agrawal V, et al. The effect of weight loss after bariatric surgery on albuminuria. Clin Nephrol. 2008;70(3):194–202.
Serpa Neto A, et al. Effect of weight loss after Roux-en-Y gastric bypass, on renal function and blood pressure in morbidly obese patients. J Nephrol. 2009;22(5):637–46.
Favre G, et al. Longitudinal assessment of renal function in native kidney after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1411–8.
Thomas DM, Coles GA, Williams JD. What does the renal reserve mean? Kidney Int. 1994;45(2):411–6.
D’Agati VD, et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12(8):453–71.
Kindgen-Milles D, Slowinski T, Dimski T. New kidney function tests: renal functional reserve and furosemide stress test. Med Klin Intensivmed Notfmed. 2020;115(1):37–42.
Sharma A, Mucino MJ, Ronco C. Renal functional reserve and renal recovery after acute kidney injury. Nephron Clin Pract. 2014;127(1–4):94–100.
Kittiskulnam P, et al. The failure of glomerular filtration rate estimating equations among obese population. PLoS One. 2020;15(11):e0242447.
Funding
This work was supported by the Science and Technology Program of Guangzhou, China (Grant No. 202002020069).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
For systematic review and meta-analysis studies, formal consent is not required.
Consent to Participate
Does not apply.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Bariatric surgery can improve renal function only in obese patients with kidney dysfunction.
• Renal function improved most after 1 year of bariatric surgery.
• Compared with RYGB (Roux-en-Y gastric bypass), patients received SG (sleeve gastrectomy) benefited more in the reduction of serum creatinine.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, H., Lu, J., Dai, X. et al. Improvement of Renal Function After Bariatric Surgery: a Systematic Review and Meta-analysis. OBES SURG 31, 4470–4484 (2021). https://doi.org/10.1007/s11695-021-05630-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05630-4