Abstract
Background
Over recent decades, laparoscopic adjustable gastric banding (LAGB) has been among the most common bariatric surgeries. Nowadays, many patients require revision surgery due to insufficient weight loss and band-related complications. Sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are the two most common revision surgeries for failed LAGB, but the conclusions about their efficacy and safety have been inconsistent. This meta-analysis aimed to review the clinical outcomes of SG and RYGB after failed LAGB.
Methods
In accordance with the PRISMA guidelines, the PubMed, Embase, Scopus, and Cochrane Central Register of Controlled Trials (CENTRAL) databases were systematically searched for articles that had studied the efficacy and safety of SG and RYGB. The most appropriate effects model was chosen based on the heterogeneity of the articles included in this meta-analysis. Statistical analysis was conducted using Stata 14.0.
Results
Of 586 articles that were retrieved, 16 articles which examined 2141 SG and 2990 RYGB patients met the inclusion criteria. The patients in RYGB groups showed increased percent excess weight loss (%EWL) at 12 and 24 months after revision surgery but no statistically significant change was found about %EWL after 3, 6, or 36 months. In addition, RYGB was associated with a higher rate of complications, interventions, and readmission in addition to being of more operative time.
Conclusions
This review suggested that RYGB was more effective at demonstrating weight loss after 12 and 24 months, but comparisons of the long-term efficacy of RYGB with that of SG remain inconclusive. In addition, RYGB was accompanied by a greater number of post-operative complications, interventions, and readmissions. Thus, surgeons should consider the overall status of the patients and their comorbidities as crucial factors when selecting a form of revision surgery. Additional high-quality randomized controlled studies are required to further compare the efficacy and safety of these treatments with longer follow-up times.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Global obesity rates have increased significantly in recent decades, with adverse health impacts such as diabetes mellitus (DM), obstructive sleep apnea, stroke, coronary heart disease (CHD), hypertension (HTN), gastroesophageal reflux disease (GERD), and cancer highlighting this obesity epidemic as a central public health concern [1, 2]. Bariatric surgery is the most effective and lasting treatment for obesity and its associated comorbidities [3]. Over the past few decades, laparoscopic adjustable gastric banding (LAGB) has become one of the most common surgical procedures for morbid obesity because it is less invasive than other options and not a permanent operation [4, 5]. However, LAGB is no longer so commonly performed because enthusiasm for LAGB has been tempered by the frequent occurrence of late-onset complications and poor long-term weight loss. However, a considerable number of patients have gastric bands which may require revision surgery [6]. In addition, the percentage of people requiring reoperation due to failed weight loss and complications has been reported to be in the range of 30–60% [6,7,8,9,10]. Current strategies for failed LAGB consist of removal of the gastric band with or without revision. However, a number of published studies have reported that the removal of gastric bands is not effective since weight is later regained [11,12,13]. Therefore, many surgeons have chosen to convert a failed LAGB to an alternative revision surgery such as Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) [14, 15]. Recently, SG has instead gained acceptance worldwide as it promotes effective weight loss with a sustained resolution of comorbidities when performed as either primary or revision surgery [16, 17].
The safety and efficacy of SG and RYGB as revision surgery have been reported by a number of studies, but the most suitable revision surgery for patients with LAGB failure remains controversial. This meta-analysis was conducted to compare the efficacy and safety of SG with RYGB for failed LAGB.
Materials and Methods
The principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 Guidelines [18] were used as the standard in this review.
Literature Search
Two reviewers searched the following keywords for relevant articles: “failed adjustable gastric banding,” “revision surgery,” “sleeve gastrectomy,” “Roux-En-Y gastric bypass,” “operative time,” “hospital stay,” and “complications” using the PubMed, Scopus, the Cochrane Central Register of Controlled Trails (CENTRAL), and Embase databases. The literature search publication date ranged from the inception of each database until January 11, 2019. In addition, the references of all relevant articles were searched to identify other eligible studies. This search was performed from January 5, 2019, to January 12, 2019. Two reviewers conducted the complete search process independently. For any disagreement, a third reviewer would examine the study until consensus was reached.
Inclusion Criteria
Two reviewers selected relevant articles independently in accordance with the following criteria: (i) articles were published in English; (ii) articles included patients who required conversion of failed LAGB to SG or RYGB; (iii) more than 10 patients were included in the two groups; (iv) the reported results comprised one or more of the following parameters: percent excess weight loss (%EWL), BMI, complications, remission (effectiveness of revision surgery on medical comorbidities), reintervention, readmission, hospital stay, and operative time; (v) the articles included available data; and (vi) the full text was available. Disagreements were resolved by discussion with a third reviewer until a consensus was reached.
Data Extraction
Two reviewers extracted the following information independently from each eligible article: the last name of the author, publication year, country or region, revision procedure, patient demographics, complications, remission, reintervention and readmission, hospital stay, operative time, and %EWL.
Statistical Analysis
Dichotomous variables were analyzed and presented as odds ratio (OR) with a 95% confidence interval (95% CI). In addition, weighted mean difference (WMD) was calculated with a 95% CI to assess the difference in continuous variables. If OR > 1 or WMD > 0, it means that values in the RYGB group were higher than those of SG patients. For dichotomous variables, a value of 0.5 was added to each cell if any of the cells were 0 in a fourfold table. Heterogeneity was assessed using Q test and I2 test value. A value of I2 < 50% or the p (heterogeneity) > 0.05 indicated that little statistical heterogeneity was presented in the results and thus the data were analyzed using a fixed-effects model (Mantel-Haenszel method) [19]. Conversely, heterogeneous data were analyzed using the random-effects model (DerSimonian and Laird method) [20]. Results were considered statistically significant when the p value was less than 0.05. All statistical analyses were conducted in Stata 14.0 (StataCorp, College Station, TX, USA).
Quality and Publication Bias Assessment
The methodological quality of the articles included in the review was appraised in accordance with the Newcastle-Ottawa Quality scale (NOS) [21]. In accordance with the NOS guidelines, two reviewers independently evaluated the quality of each article according to the following parameters: selection, comparability, and exposure. The results are shown in Table 1. In addition, studies which achieved 5–9 stars were defined as high-quality articles [22]. Publication bias was assessed using Egger’s and Begg’s tests and presented using a funnel plot [23]. The “leave one-out” approach was used to perform a sensitivity analysis, if required.
Results
Literature Search and Characteristics
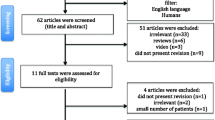
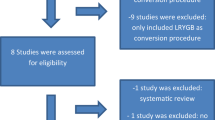
A total of 584 articles were retrieved from the 4 databases of which 155 duplicate articles were excluded using the document manager. Finally, 37 full-text articles were selected for further evaluation. Based on the established inclusion criteria, 16 articles were included in this meta-analysis. The search process described above and the PRISMA checklist are shown separately in Fig. 1 and Table S1. This meta-analysis included 5131 patients, 2141 of whom underwent revision surgery using SG and 2990 with RYGB, extracted from the 16 articles for the assessment of safety and efficacy of SG versus RYGB after failed LAGB (Table 1). The selected articles described patients from the USA [24,25,26,27,28], UK [29, 30], Spain [31], Turkey [32], Greece [33], Taiwan [34, 35], Poland [36], Italy [37], Singapore [38], and France [39]. The sample sizes for the RYGB and SG procedures ranged from 9 to 1354 patients, with SG performed in 41.7% of cases. The proportion of female patients was 83.2% and 83.0% in the SG and RYGB groups, respectively. The mean age of SG patients ranged from 35.6 to 49.8 years and from 33.9 to 50.7 years for RYGB patients. Mean BMI at the time of conversion surgery in the two groups was 41.10 ± 6.24 (SG) and 41.22 ± 35.34 kg/m2 (RYGB).
Quantitative Synthesis
Complications
Comparisons of complications between the SG and RYGB groups were presented in 8 articles, with 7 that analyzed early complications (within 30 days) and 5 articles that included late complications (over 30 days). However, no statistical difference was found regarding early complications (OR = 1.53 [95% CI 0.54–4.30] p = 0.421), late complications (OR = 2.17 [95% CI 0.94–5.02] p = 0.070), and total complications (OR = 2.01 [95% CI 0.99–4.12] p = 0.055) between the RYGB and SG groups (Table 2, Fig. 2). In addition, 5 studies reported stenosis data, showing no significant difference between the RYGB and SG groups (OR = 0.50 [95% CI 0.15–1.64] p = 0.249). Eight studies included data on leaks, also finding no significant difference between the RYGB and SG groups when analyzed together (OR = 1.60 [95% CI 0.95–2.69] p = 0.076). Furthermore, no significant difference between the two groups was reported regarding bleeding (OR = 3.64 [95% CI 1.89–7.00] p = 0.000), ulcer (OR = 1.94 [95% CI 0.20–19.07] p = 0.570), or incisional hernia (OR = 1.16 [95% CI 0.29–4.62] p = 0.831). However, 5 studies that reported obstruction indicating that RYGB as a revision surgery for failed LAGB increased the incidence of obstruction (OR = 4.16 [95% CI 1.001–17.28] p = 0.050) (Table 2, Fig. 3).
Reintervention and Readmission Within 30 Days
Reintervention was analyzed in 5 articles, demonstrating that the number of patients who underwent reintervention in the RYGB and SG groups was 74 and 23, respectively. Readmission was analyzed in 4 articles, with the number of readmissions in the RYGB and SG groups being 63 and 124 patients, respectively. The incidence of reintervention (OR = 3.13 [95% CI 1.95–5.02] p = 0.000) and readmission (OR = 2.02 [95% CI 1.47–2.76] p = 0.000) was significantly higher in RYGB group (Table 2, Fig. 4).
Complication Remission Rate Following Revision Surgery
Only 2 studies presented data concerning the effectiveness of revision surgery on medical comorbidities [28, 29]. There were 68 GERD patients before revision surgery, of which 13 (19.12%) received SG and 55 (80.88%) RYGB. The remission rates in the SG and RYGB groups were 23.08% and 45.45%, respectively. The two studies reported that 41.18% (OR = 1.47 [95% CI 0.14–14.98] I2 = 58.3%, p = 0.375) of the patients experienced remission from GERD. In addition, 33 patients that had DM preoperatively underwent revision, of which 6 (18.18%) received SG and 27 (81.82%) received RYGB. The remission rates in the SG and RYGB groups were 33.33% and 40.7%, respectively. It was reported that 39.39% (OR = 1.18 [95%CI 0.24–5.88] I2 = 0.0%, p = 0.844) of the patients experienced remission from DM. Furthermore, 69 patients exhibited HTN before revision surgery of which 8 (11.59%) underwent SG and 61 received (88.41%) RYGB. The remission rates in the SG and RYGB patients were 25% and 59.02%, respectively. The two studies reported that 55.07% (OR = 2.09 [95% CI 0.48–9.09] p = 0.324) of the patients achieved remission from HTN. Overall, RYG B had a better trend than SG in terms of remission in preoperative GERD, DM, and HTN, although no significant statistical difference was found regarding effectiveness of revision surgery on GERD (OR = 1.47 [95%CI 0.14–14.98] p = 0.375), HTN (OR = 2.09 [95%CI 0.48–9.09] p = 0.324), or DM (OR = 1.18 [95%CI 0.24–5.88] p = 0.844). The results of the remission rate following revision surgery are shown in Table 2 and Fig. 5.
%EWL
The %EWL at 3, 6, 12, 24, and 36 months was reported in 13 of the articles included in the review. There was no significant difference after 3 months (WMD = − 0.89 [95% CI − 11.56–9.79] p = 0.871) and 6 months (WMD = − 1.80 [95% CI − 12.31–8.71] p = 0.737). However, %EWL after 12 months was significantly higher in the RYGB group (WMD = 7.00 [95% CI 2.48–11.52] p = 0.002). In addition, %EWL was also significantly higher after 24 months (WMD = 12.37 [95% CI 6.20–18.54] p = 0.000) in the RYGB group compared with SG patients (Table 2, Fig. 6). There was no statistical difference in %EWL after 36 months (WMD = 3.67 [95% CI = − 4.35–11.69] p = 0.370) (Fig. 6).
Mean Length of Hospital Stay and Operative Time
The mean length of hospital stay in the RYGB group ranged from 1.2 to 5 days and from 1.5 to 5.7 days in the SG group. There was no significant difference in length of hospital stay (WMD = 0.25 [95% CI − 0.32–0.82] p = 0.387) (Table 2, Figure S1). The mean operative time ranged from 140 to 218.9 min in the RYGB group and from 108.4 to 172.7 min in the SG group. This difference was statistically significant, indicating that RYGB requires more operative time than SG (WMD = 38.81 [95% CI 30.46–47.16] p = 0.000) (Table 2, Figure S1).
Assessment of Publication Bias and Quality
Publication bias was assessed using an Egger’s formal statistical test and a Begg’s correlation test then presented using a funnel plot when the number of articles analyzed was not less than 10. Therefore, we conducted an assessment of publication bias for %EWL after 12 months. The results (Egger P > |t| = 0.721 Begg, Pr > |z| = 0.837) showed that there was no publication bias (Figures S2, S3, and S4). In addition, the quality assessment of the articles ranged from 6 to 7 stars (Table 1), thus classifying them as high-quality articles.
Discussion
LAGB has gained worldwide acceptance for the treatment of obesity, thanks to the simplicity, good short-term results, and low early complication rate of the procedure [40]. However, several studies have reported that many patients eventually require revision surgery due to high failure rates, weight regain, and band-related complications in long-term follow-up [41,42,43]. In addition, RYGB and SG have both been proven effective in treating patients with failed LAGB [44, 45]. Moreover, different surgeons have varying opinions about which revision is preferable. Those in favor of SG were of the opinion that LSG had gained worldwide recognition as a result of sustained resolution of comorbidities and the significant reduction in weight as either primary or revision surgery [46, 47]. Conversely, those in favor of RYGB have argued that RYGB for failed vertical banded gastroplasty (VBG) has demonstrated to be the operation of choice for satisfactory weight loss in revisions, thus indicating that RYGB may have greater efficacy than SG as a revision surgery for failed LAGB [26].
Several similar reviews were published to discuss the clinical outcomes of revision surgery after failed LAGB, but their conclusions have not been consistent [45, 48, 49]. In this meta-analysis, the results demonstrated that the efficacy of RYGB for failed LAGB was better than of SG after12 months (WMD = 7.00 [95% CI 2.48–11.52] p = 0.002) and 24 months (WMD = 12.37 [95% CI 6.20–18.54] p = 0.000). However, there was no difference in their effect on weight loss after 36 months (WMD = 3.67 [95% CI = − 4.35–11.69] p = 0.370). This suggests that SG may have the additional benefit of regulation of hormones as revision procedure during the longer-term follow-up, an effect which has been previously reported in a clinical article by Cohen et al. [50]. In addition, the clinical results about %EWL after 24 months by Magouliotis et al. supported our final conclusion. In contrast to our results, Magouliotis, Sharples, and Zhou et al. conducted meta-analyses which reported no statistical difference in %EWL after 12 months. Sharples et al. suggested that there was no statistical difference in %EWL at 24 months [45, 48, 49]. The insufficient number of articles and short follow-up time may have caused their results to be unreliable. Moreover, a published review by Elnahas et al. suggested that RYGB was better than SG at promoting weight loss. However, no standardized outcome measurement and significant heterogeneity between studies made its results uncertain [51]. The remission rate of complications following revision surgery was slightly better in RYGB about preoperative GERD, DM, and HTN than in SG group, although the differences were not significantly different. When choosing revision surgery for patients with medical comorbidities, the actual situation of patients should be taken into consideration.
Based on our results, the incidence of complications, reintervention, and readmission was significantly higher in RYGB patients. Similarly, a study conducted by Spaniolas also suggested that RYGB was associated with a higher rate of uneventful recovery compared with SG [52]. There was no statistically significant difference in the mean length of hospital stay, but the mean operative time in the RYGB group was significantly higher. However, there are many factors affecting the length of hospital stay and operative time. Hospital stay is a poor metric of surgical outcomes. In addition, operative time may be increased if gastric band explantation and conversion to another procedure take place synchronously compared with two-step revision surgery, so surgeons should treat such results in the light of the actual situation. RYGB as revision surgery alters the structure of the intestine and its gastrointestinal anastomosis, possibly accounting for a higher complication rate. In addition, SG is essentially the first step of the BPD-DS procedure, the reason that SG requires less operative time.
Our meta-analysis included a higher number of patients than previous clinical studies and reviews. Nevertheless, the principal limitations of this meta-analysis were the small number of patients that contributes to the outcomes in each category and the methodological issues associated with research design, as all articles included in the review were observational studies. Therefore, limitations arising from the lack of randomized controlled studies are inevitable.
Conclusions
This meta-analysis indicated that RYGB was associated with better weight loss at 12 and 24 months; however, this appeared to be at the expense of increased post-operative complications and readmissions. There was a lack of detail regarding the type and severity of complications and the need for readmissions as well as a paucity of data on long-term outcomes. Thus, there is a pressing need for prospective controlled studies comparing surgical techniques to treat failed gastric banding.
References
Collins J, Meng C, Eng A. Psychological impact of severe obesity. Curr Obes Rep. 2016;5(4):1–6.
Welsh LK, Murayama KM. History of bariatric Surgery. 2018.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery and Endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27(9):2279–89.
Franck Z, Jean-Marc C, Richard D, et al. Laparoscopic gastric banding: a minimally invasive surgical treatment for morbid obesity: prospective study of 500 consecutive patients. Ann Surg. 2003;237(1):1–9.
Peterli R, Donadini A, Peters T, et al. Re-operations following laparoscopic adjustable gastric banding. Obes Surg. 2002;12(6):851–6.
Brown JJS, Boyle M, Mahawar K, et al. Laparoscopic adjustable gastric band survival in a high-volume bariatric unit. Br J Surg. 2013;100(12):1614–8.
Spivak H, Beltran OR, Ng AW, et al. Long-term outcomes of laparoscopic adjustable gastric banding and laparoscopic roux-en-Y gastric bypass in the United States. Surg Endosc. 2012;26(7):1909–19.
Zuegel NP, Lang RA, Hüttl TP, et al. Complications and outcome after laparoscopic bariatric surgery: LAGB versus LRYGB. Langenbecks Archives of Surgery. 2012;397(8):1235–41.
Nieuwenhove YV, Ceelen W, Stockman A, et al. Long-term results of a prospective study on laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011;21(5):582–7.
Buchwald H, Oien DM. Metabolic/bariatric Surgery worldwide 2011. Obes Surg. 2013.
Aarts EO, Dogan K, Koehestanie P, et al. What happens after gastric band removal without additional bariatric surgery? Surgery for Obesity & Related Diseases Official Journal of the American Society for Bariatric Surgery. 2014;10(6):1092–6.
Victorzon M, Tolonen P. Mean fourteen-year, 100% follow-up of laparoscopic adjustable gastric banding for morbid obesity. Surgery for Obesity & Related Diseases. 2013;9(5):753–7.
Kirshtein B, Kirshtein A, Perry Z, et al. Laparoscopic adjustable gastric band removal and outcome of subsequent revisional bariatric procedures: a retrospective review of 214 consecutive patients. Int J Surg. 2016;27:133–7.
Boza C, Gamboa C, Perez G, et al. Laparoscopic adjustable gastric banding (LAGB): surgical results and 5-year follow-up. Surg Endosc. 2011;25(1):292–7.
Abu-Gazala S, Keidar A. Conversion of failed gastric banding into four different bariatric procedures. Surgery for Obesity & Related Diseases. 2012;8(4):400–7.
Magouliotis DE, Tasiopoulou VS, Sioka E, et al. Robotic versus laparoscopic sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis. Obes Surg. 2017;27(1):245–53.
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of Reoperative bariatric Surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21(8):1209–19.
Alessandro L, Altman DG, Jennifer T, Cynthia M, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Epidemiology Biostatistics & Public Health. 2009.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Nat Cancer Inst. 1959;22:719–48.
Dersimonian R, Nan L. Meta-analysis in clinical trials. Control Clin Trials. 1986.
Andreas S. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Aziz O, Constantinides V, Tekkis PP, et al. Laparoscopic versus open Surgery for rectal Cancer: a meta-analysis. Ann Surg Oncol. 2006;13(3):413–24.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Creange C, Jenkins M, Pergamo M, Fielding G, Ren-Fielding C, Schwack B. Gastric band conversion to roux-en-Y gastric bypass shows greater weight loss than conversion to sleeve gastrectomy: 5-year outcomes. Surgery for Obesity & Related Diseases. 2018;S1550728918302995-.
Yeung L, Durkan B, Barrett A, et al. Single-stage revision from gastric band to gastric bypass or sleeve gastrectomy: 6- and 12-month outcomes. Surg Endosc. 2016;30(6):2244–50.
Marin-Perez P, Betancourt A, Lamota M, et al. Outcomes after laparoscopic conversion of failed adjustable gastric banding to sleeve gastrectomy or roux-en-Y gastric bypass. Br J Surg. 2014;101(3):254–60.
Gonzalez-Heredia R, Masrur M, Patton K, et al. Revisions after failed gastric band: sleeve gastrectomy and roux-en-Y gastric bypass. Surg Endosc. 2015;29(9):2533–7.
Moon RC, Teixeira AF, Jawad MA. Conversion of failed laparoscopic adjustable gastric banding: sleeve gastrectomy or roux-en-Y gastric bypass? - Surgery for obesity and related diseases. Surgery for Obesity & Related Diseases. 2013;9(6):901–7.
Khan OA, Mcglone ER, Maynard W, Hopkins J, Dexter S, Finlay I, et al. Single-stage conversions from failed gastric band to sleeve gastrectomy versus roux-en-Y gastric bypass: results from the United Kingdom National Bariatric Surgical Registry. Surg Obes Relat Dis 2018;S1550728918303423-.
Carr WRJ, Jennings NA, Boyle M, et al. A retrospective comparison of early results of conversion of failed gastric banding to sleeve gastrectomy or gastric bypass. Surgery for Obesity & Related Diseases. 2015;11(2):379–84.
Rafols JP, Abbas AIA, Devriendt S, Guerra A, Herrera MF, Himpens J, et al. Roux-En-Y gastric bypass, sleeve gastrectomy, or one anastomosis gastric bypass as rescue therapy after failed adjustable gastric banding: a multicenter comparative study. Surg Obes Relat Dis 2018;S1550728918304945-.
Avsar FM, Sapmaz A, Uluer A, et al. Conversion Surgery for failed adjustable gastric banding: outcomes with sleeve gastrectomy vs roux-en-Y gastric bypass. Obes Surg. 2018:1–7.
Mousa K, Ibtisam AB, Ali M, et al. Sleeve gastrectomy or gastric bypass as revisional bariatric procedures: retrospective evaluation of outcomes. Surg Endosc. 2013;27(11):4277–83.
Chansaenroj P, Aung L, Lee WJ, et al. Revision procedures after failed adjustable gastric banding: comparison of efficacy and safety. Obes Surg. 2017;27(11):2861–7.
Keng-Hao L, Michele D, Michel V, et al. Revisional surgery after failed adjustable gastric banding: institutional experience with 90 consecutive cases. Surg Endosc. 2013;27(11):4044–8.
Janik MR, Rogula TG, Mustafa RR, Saleh AA, Khaitan L. Safety of revision sleeve gastrectomy compared to roux-Y gastric bypass after failed gastric banding: analysis of the MBSAQIP. Ann Surg. 2017;1.
Angrisani L, Vitiello A, Santonicola A, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy as Revisional procedures after adjustable gastric band: 5-year outcomes. Obes Surg. 2017;27(6):1430–7.
Ngiam KY, Khoo VYH, Kong L, et al. Laparoscopic adjustable gastric banding revisions in Singapore: a 10-year experience. Obes Surg. 2016;26(5):1069–74.
Carandina S, Maldonado PS, Tabbara M, et al. Two-step conversion surgery after failed laparoscopic adjustable gastric banding. Comparison between laparoscopic roux-en-Y gastric bypass and laparoscopic gastric sleeve. Surgery for Obesity & Related Diseases. 2014;10(6):1085–91.
Chapman AE, Kiroff G, Game P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery. 2004;135(3):326–51.
Snow JM, Severson PA. Complications of adjustable gastric banding. Surg Clin N Am. 2011;91(6):1249–64.
Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16(7):829.
Dogan K, Gadiot RPM, Aarts EO, et al. Effectiveness and safety of sleeve gastrectomy, gastric bypass, and adjustable gastric banding in morbidly obese patients: a multicenter, retrospective, matched cohort study. Obes Surg. 2015;25(7):1110–8.
Mahawar KK, Graham Y, Carr WRJ, et al. Revisional roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg. 2015;25(7):1–10.
Sharples AJ, Charalampakis V, Daskalakis M, et al. Systematic review and meta-analysis of outcomes after Revisional bariatric Surgery following a failed adjustable gastric band. Obes Surg. 2017;27(12):1–15.
CICotASf M, Surgery B. Updated position statement on sleeve gastrectomy as a bariatric procedure. Surgery for Obesity & Related Diseases Official Journal of the American Society for Bariatric Surgery. 2012;8(3):e21–e6.
Bransen J, Gilissen LPL, Rutte PWJV, et al. Costs of leaks and bleeding after sleeve Gastrectomies. Obes Surg. 2015;25(10):1767.
Zhou R, Poirier J, Torquati A, Omotosho P. Short-term outcomes of conversion of failed gastric banding to laparoscopic sleeve gastrectomy or roux-En-Y gastric bypass: a meta-analysis. Obes Surg. 2018.
Magouliotis DE, Tasiopoulou VS, Svokos AA, et al. Roux-En-Y gastric bypass versus sleeve gastrectomy as Revisional procedure after adjustable gastric band: a systematic review and meta-analysis. Obes Surg. 2017;27(5):1365–73.
Cohen R, Uzzan B, Bihan H, et al. Ghrelin levels and sleeve gastrectomy in super-super-obesity. Obes Surg. 2005;15(10):1501–2.
Elnahas A, Graybiel K, Farrokhyar F, et al. Revisional surgery after failed laparoscopic adjustable gastric banding: a systematic review. Surg Endosc. 2013;27(3):740.
Spaniolas K, Bates AT, Jr DS, et al. Single stage conversion from adjustable gastric banding to sleeve gastrectomy or roux-en-Y gastric bypass: an analysis of 4875 patients. Surgery for Obesity & Related Diseases Official Journal of the American Society for Bariatric Surgery. 2017;13(11):1880.
Acknowledgments
Our team thanks Shi-cheng, Rixing-bai, Meng-zhao, and Hongyi-zhang of Tiantan Hospital for their insightful comments and suggestions. Capital Medical University is also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Figure S1
The forest plot showed the WMD (95% CI) of hospital stay and operative time for RYGB and SG groups as revision surgery after failed LAGB with random-effects model (PNG 372 kb)
Figure S2
Egger’s test for identifying publication bias for %EWL at 12 months (PNG 67 kb)
Figure S3
Begg’s test for identifying publication bias for %EWL at 12 months. (PNG 89 kb)
Figure S4
Funnel plots for identifying publication bias for %EWL at 12 months (PNG 112 kb)
Table S1
PRISMA checklist (DOC 59 kb)
Rights and permissions
About this article
Cite this article
Wu, C., Wang, Fg., Yan, WM. et al. Clinical Outcomes of Sleeve Gastrectomy Versus Roux-En-Y Gastric Bypass After Failed Adjustable Gastric Banding. OBES SURG 29, 3252–3263 (2019). https://doi.org/10.1007/s11695-019-03988-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03988-0