Abstract
Background
Securing the surgical margin is the most essential and important task in curative surgery. However, it is difficult to accurately identify the tumor location during laparoscopic surgery for gastric cancer, and existing methods, such as preoperative endoscopic marking with tattooing and clipping, have multiple disadvantages.
Aims
We investigated the feasibility and safety of indocyanine green (ICG) fluorescence marking for determining the tumor location during laparoscopic gastrectomy.
Methods
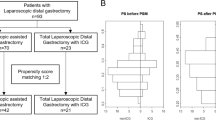
We retrospectively analyzed preoperative and perioperative data from consecutive patients with gastric cancer undergoing planned laparoscopic distal gastrectomy. Data was maintained in a prospectively compiled surgical database, and patients were categorized into ICG (n = 84) or non-ICG (n = 174) groups based on whether they underwent preoperative endoscopic mucosal ICG injection. One-to-one propensity score matching (PSM) was performed to compare outcomes between the two groups.
Results
We included 84 patient pairs after PSM, and there were no significant differences in preoperative patient characteristics. The ICG group had shorter procedure time (p < 0.001), lower estimated blood loss (p = 0.005), and significantly shorter postoperative hospital stay (p < 0.001). Positive resection margins were confirmed in five cases (6.0%) in the non-ICG group, whereas there were none in the ICG group (p = 0.008). Real-time confirmation was possible during laparoscopy, and the injected ICG did not affect the surgical procedure or result in adverse events.
Conclusion
ICG fluorescence imaging is feasible and safe and can potentially be used as a tumor-marking agent for determining the surgical resection line.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Securing the correct surgical margin is the most essential and important task in curative surgery. However, in laparoscopic surgery, determining the tumor location is difficult, and there is no standard protocol for the same. In Japan and other Asian countries with a high proportion of early gastric cancer patients, a preoperative endoscopic marking method, such as India ink tattooing and/or a clipping method, is usually performed to precisely identify the tumor location during surgery.1,2,3,4,5,6,7 However, the use of India ink tattooing has resulted in reports of adverse events, such as peritonitis due to intraperitoneal spraying of the black ink and ileus obstruction due to adhesion, and the safety of this procedure remains unclear.8,9 In addition, intraperitoneal spraying of India ink leads to poor recognition of the release layer and affects the procedure by making it impossible to recognize an appropriate resection line. On the other hand, the clipping method requires confirmation by palpation, which is not useful during laparoscopic surgery. Further, clipping may not be recognizable during a laparotomy because of excessive intestinal wall or fat thickness, making this an unreliable method. The reported confirmation method involving marking clips with intraoperative endoscopy7 is cumbersome as the process is increased, and the preparation of the intraoperative endoscopy is necessary. Thus, these approaches require extraneous efforts, with increased operation time, the need for additional manpower, the possibility of additional frozen sections in suspicious cases of the gross margin.10
In recent years, indocyanine green (ICG) fluorescence imaging has received much attention in laparoscopic surgery. ICG binds to plasma proteins and emits fluorescence after stimulation using a laser beam11,12 or near-infrared (NIR) light at a wavelength of approximately ≥ 820 nm.13,14 The absorption maximum of ICG is approximately 807 nm while the emission maximum is approximately 822 nm.15 The emitted ICG fluorescence is detected using specifically designated scopes and camera. Currently, ICG fluorescence imaging is being used for navigational laparoscopic gastrectomy, to detect the sentinel lymph nodes during gastric cancer and visualize blood flow,16,17,18,19,20 and for determining the tumor location during laparoscopic colon tumor resection.21,22 However, there are no reports on ICG fluorescence tumor marking for laparoscopic gastrectomy. Therefore, we assessed the usefulness and safety of a preoperative ICG marking method that used NIR fluorescence for activation and a laparoscopic imaging system during total laparoscopic gastrectomy.
Methods
Patients
This retrospective analysis used prospectively compiled surgical data from July 2015 to August 2017 at Department of Surgery, Osaka International Cancer Institute, Osaka, Japan. Data on consecutive patients who underwent scheduled laparoscopic distal gastrectomy (LDG) for gastric cancer were extracted from the database that included patient characteristics (age, sex, body mass index (BMI; kg/m2)), preoperative data (clinical T and N stages and preoperative histology), surgical outcomes including intraoperative events (surgical approach, procedure time, and estimated blood loss), and postoperative course and outcome. We only used data from patients who fulfilled the inclusion criteria of gastric cancer without distant metastasis as determined by preoperative physical examination and imaging studies and who were physiologically normal, defined as the American Society of Anesthesiology physical status score of ≤ 2. Patients with concurrent malignancies, those who had undergone preoperative neoadjuvant chemotherapy (NAC), and those participating in other clinical trials were excluded from the study. We identified 258 patient records, and these were divided into two groups based on ICG use as patients with ICG marking (ICG group, n = 84) and those without ICG marking (non-ICG group, n = 174).
Gastric resection and anastomosis construction were performed intracorporeally in all cases and were a delta-shaped anastomosis or Roux-en-Y reconstruction, depending on the size of the remnant stomach after LDG. In addition, a D1+ or D2 lymphadenectomy was performed in all cases to comply with the treatment guidelines of the Japanese Gastric Cancer Association.23
Localization Procedure
ICG (Diagnogreen®) was purchased from Daiichi-Sankyo Co., Ltd. (Tokyo, Japan). All cases in the ICG group underwent GIF 1 day preoperatively, and ICG marking was performed around the tumor. The solution for ICG marking was prepared by dissolving Diagnogreen 1 V in 10 ml of distilled water; 0.2 ml of this solution was mixed with 9.8 ml of distilled water to obtain 10 ml of solution (0.05 mg/ml of Diagnogreen). The prepared solution (0.5 ml at a time) was submucosally injected under endoscopic guidance at four sites around the tumor (proximal side, distal side, and bilateral sides) (Fig. 1). To evaluate the spread of ICG from the injection site after the operation, clipping was performed at the injection point. In the non-ICG group, clipping was performed on the oral side of the tumor. ICG diffusion range from the clipping points was measured after tumor excision and recorded at four places.
Preoperative endoscopic fluorescence tattooing and clipping. Endoscopic view. a Indocyanine green (ICG) was injected after locating the tumor lesion, b 0.5 mL was injected at four points, namely, proximal, distal, and bilateral, in the gastric cancer region (white arrow describes the ICG marking). c Marking clips were placed on the scar after injecting ICG (white arrows indicate marking clip positions at ICG injection points). d After ICG tattooing and clipping, we evaluated their position using X-rays (white arrow indicates the marking clip positions at the ICG injection points)
Laparoscopic Equipment
A laparoscopic laser-free FULL HD system was used for all procedures. Images were generated using a NIR/ICG telescope and camera head system (IMAGE1 S™ System, KARL STORZ, Tuttlingen, Germany) connected to a laparoscope (30″ field of direction and 10 mm diameter) equipped with a specific filter for optimal detection of NIR fluorescence and white light without manual switching. The xenon light source (D-LIGHT P, KARL STORZ) provided both visible and NIR excitation light with enhanced background display. Switching between white light and NIR fluorescence mode was controlled by the surgeon using a footswitch. Visualization, both in standard and NIR light, was improved by an image enhancement system (IMAGE1 S™ System, KARL STORZ) that offered adjustable visualization modalities that could be selected according to the surgeon’s preferences.
Surgical Approach
The surgical procedure used for LDG has been described previously.24 Briefly, the initial port was placed through a 2.5-cm infraumbilical incision made using the open method and a commercially available access port (EZ Access; Hakko, Nagano, Japan). During the procedure, a pneumoperitoneum was established using carbon dioxide insufflation at a pressure of approximately 10–12 mmHg according to body type of the patient. LDG was performed using five ports (one 12-mm port in the umbilicus and 5- and 12-mm ports in the right and left lateral abdomen). We mainly used conventional straight graspers and an ultrasonic coagulation-cutting device (Harmonic scalpel; Ethicon Endo-Surgery, Cincinnati, OH, USA) to perform gastric mobilization and lymph node dissection. During laparoscopic gastrectomy, the stomach was first illuminated with white light (Fig. 2), and ICG was subsequently activated with NIR light and viewed via a laparoscopic imaging system in patients injected with ICG to determine the tumor location. Afterward, the stomach was resected. After gross inspection and measurement of any serosal tumor involvement, the stomach was, in principle, opened along its greater curvature for examination from the mucosal side and measurement of the tumor size and length of the proximal and distal resection margins. If a positive resection margin was suspected, intraoperative histological examination of frozen sections was performed, and if indeed the resection margin was positive, the procedure was changed to laparoscopic total gastrectomy (LTG). Postoperatively, if the stump was also found to have positive margins, another LTG was planned as soon as possible, and the intracorporeal anastomosis technique was used for reconstruction.25,26
Tumor localization using the intraoperative laparoscopic fluorescence imaging system. Laparoscopic view. Tumor location was visualized using near-infrared light-activated ICG fluorescence. a, c Under white light. b, d under near-infrared light-activated ICG. a White arrow indicates fluorescent outer wall of the stomach. d White arrow indicates fluorescent inner wall of the stomach
Perioperative Surgical Outcomes
Data obtained from patient records included patient characteristics, procedure duration, intraoperative estimated blood loss, pathological findings (e.g., tumor depth, proximal and distal margins, number of lymph node dissected, and lymph node metastasis), postoperative morbidity rate, frequency of additional resection, and duration of postoperative hospital stay. Complications during surgery were assessed based on the Clavien–Dindo classification,27 and TNM staging was based on the Japanese Classification of Gastric Carcinoma.28 Outcomes specific to ICG usage were detection rate of ICG during gastrectomy, size of the visualized ICG, morbidity after preoperative upper endoscopy, and adverse effects after ICG injection.
Statistical Analysis
All statistical analyses were performed using the JMP® PRO software (JMP version 13.1.0, SAS Institute, Cary, NC). PSM analysis was conducted using a logistic regression model with the following covariates: age, sex, American Society of Anesthesiologists physical status classification (ASA-PS), BMI, histology, tumor location, clinical stage, and presence of preoperative ESD. We used a caliper width of 0.2 for the pooled standard deviation of the logit for calculating the propensity score for PSM. Demographic and clinicopathological characteristics were summarized and descriptively analyzed, and all qualitative values are presented as means and standard deviations, unless otherwise specified. The Student’s t test or the Mann–Whitney U test and Pearson’s χ2 test were used to compare continuous and categorical variables, respectively. Categorical variables were also compared using the Fisher’s exact test. All values were two tailed, and p values < 0.05 were considered to be significant.
Results
Baseline Demographics and Preoperative Assessment
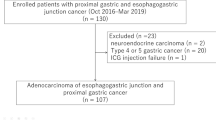
The study flow chart is summarized in Fig. 3. We identified 274 consecutive cases that underwent LDG from July 2015 to August 2017. One hundred eighty-one cases in the previous term in continuous cases were in the non-ICG group and 93 cases in the later period were in the ICG group. We excluded 16 cases due to preoperative NAC (n = 8), ASA-PS score of ≥3 (n = 7), and preoperative NAC with concurrent malignancy (n = 1). Eighty-four cases in the ICG group and 174 cases in the non-ICG group were adjusted by PSM and 84 pairs of cases were analyzed. The baseline characteristics of the ICG and non-ICG groups are summarized in Table 1. No significant differences were observed between the two groups with respect to preoperative characteristics.
Study flow chart. The inclusion criteria are as follows: a normal physiologic condition defined as an ASA-PS score of ≤ 2, the patients without concurrent malignancies, NAC, and those participating in other clinical trials. PSM was performed by logistic analysis using age, sex, ASA-PS, BMI, histology, tumor location, clinical stage, and presence of preoperative ESD as covariates. We used 0.2 times of the pooled standard deviation of the logit of the propensity score as caliper width for PSM
Perioperative Outcomes
All surgical outcomes analyzed are detailed in Table 2. All procedures were laparoscopic, and no case needed conversion to open gastrectomy. A comparison of surgical characteristics showed that the procedure time was significantly shorter, and estimated blood loss was significantly lower (p = 0.005) in the ICG group than in the non-ICG group (p < 0.001). Evaluation after surgical tumor resection used frozen sections of the resection line if the tumor border was unclear. In the non-ICG group, five patients had a R1 resection (positive resection margin), and four of these cases were identified by intraoperative frozen section assessment of the resection line; this resulted in the surgical procedure being converted to LTG. There was no significant difference in the rate of tumor retention after initial gastrectomy between the two groups (p = 0.238). One case was diagnosed as a R1 resection margin on postoperative permanent specimens, and LTG was subsequently performed after 2 weeks postoperatively. Finally, R0 resection was achieved for all cases with gastric cancer.
There was no significant difference between the tumor size, proximal margin, distal margin, and histopathologic classification between the two groups (Table 2). In the TNM classification, there was no difference between the two groups in the final stage or tumor depth, but N scores were higher in the ICG group (p = 0.002). The number of lymph node dissections observed in the permanent specimens was significantly higher in the ICG group than in the non-ICG group (p = 0.046). The rate of postoperative complications did not differ between the two groups, and there were no grade ≥ 3 complications, according to the Clavien–Dindo classification. There were also no cases of postoperative mortality and the postoperative hospital stay was significantly shorter in the ICG group than in the non-ICG group (p < 0.001).
Outcomes of ICG Injection
All ICG-specific outcome measures are described in Tables 2 and 3. ICG injection was confirmed intraoperatively in all cases, there were no complications associated with the upper gastrointestinal endoscopy performed for ICG injection, and no adverse effects were observed after ICG injection. During the surgery, tumor localization was identified and lymph flow was confirmed by injecting ICG. No adverse effects attributable to ICG use, such as intra-abdominal peritonitis or adhesion, were observed within the abdominal cavity during surgery. The visible range of ICG fluorescence was calculated to be 10–70 mm with a median of 25 mm. ICG diffusion in the tumor was assessed in four directions (proximal, distal, and bilateral), and there was no difference in ICG diffusion distance among these directions.
Discussion
During laparoscopic gastrectomy, the tumor location can be determined only based on images on the monitor and the sense of “touch” perceived through the forceps as it is impossible to palpate intra-abdominal organs. Further, in early gastric cancer, the tumor cannot be visually identified, except in cases where the location can be recognized by resistance perceived through the forceps. Even in advanced gastric cancer, the accurate tumor location cannot be confirmed visually in laparoscopy, unless the tumor is exposed to serosa. Also, in both early and advanced cancers, the spread of cancer in the lumen cannot be recognized from outside the stomach wall. Previous reports have stated that every effort must be made to secure a negative proximal margin during the surgical treatment of gastric cancer because of the poor prognostic nature of a positive proximal margin.29,30 Bissolati et al. have demonstrated that survival after gastrectomy is negatively affected by a positive resection margin.31
We have used ICG fluorescence to confirm tumor location by locally injecting it under endoscopic guidance into the stomach wall from the mucosal side prior to the gastrectomy. Switching between visible light and fluorescent images was possible using a footswitch, and as this could be performed while looking at the positional relationship between the tumor and the stomach wall, it was particularly useful for determining the resection line. Under these conditions, real-time laparoscopic surgery was possible under white light without the need for confirmation under night vision. This technology was also useful because there is no need to withdraw the stomach from the abdominal cavity during operation.
We performed clipping with ICG injection 1 day prior to the surgery; however, we did not perform intraoperative endoscopy. ICG was injected to surround the cancer, which enabled the determination of the exact localization of the gastric cancer. ICG injection was confirmed to have no complications and adverse events in all cases, including in those where ICG was injected a day prior to the surgery. Excision enabled easy R0 resection; as a result, no fluorescence from ICG was observed in the residual stomach. In addition, intraoperative endoscopy has been reported to be useful in localizing the tumor7,32,33; however, our method does not require confirmation of the tumor location by intraoperative endoscopy. In addition, confirmation of the marking clip localization by X-ray fluoroscopy is unnecessary. As a result, it is possible to reduce the operation time more efficiently and accordingly reduce the surgical invasion.
ICG also flows through the lymph duct, and occasionally, the regional lymph nodes may also be labeled by ICG, which may be useful for determining the lymphadenectomy range. This could account for the observation that the number of dissected lymph nodes in the ICG group was significantly larger than that in the non-ICG group. Nimura et al. have reported that infrared ray-based ICG fluorescence imaging make it easy to distinguish between lymphatic vessels and lymph nodes containing ICG and the surrounding tissues compared with naked eye observation.34 Similarly, many studies have suggested that ICG fluorescence imaging during laparoscopic sentinel node biopsy for gastric cancer is feasible, useful, and safe.34,35,36,37,38 We have previously reported on the usefulness of detecting sentinel lymph nodes in gastric cancer36,39,40,41; however, the results of a multicenter collaborative research showed an unacceptably high number of false negatives.42 Therefore, the concept of sentinel lymph nodes in gastric cancer is still not popular, and it is premature to choose reduction surgery according to the results of sentinel lymph nodes. According to our research, LDG using ICG fluorescence enabled the dissection of more number of lymph nodes, and lymph flows such as lymph duct were clearly marked by ICG fluorescence. Thus, this procedure may be useful for intraoperative lymph flow mapping.
In gastric cancer, it is difficult to locate the tumor from outside the wall; therefore, it is currently common to locally inject India ink in the vicinity of the tumor under endoscopic guidance preoperatively.5,6 However, it is often difficult to confirm the preoperative tattooing with dye injection depending on the tumor location, the fat volume, and the thickness of stomach wall. In addition, it has been reported that the ink spreads widely, resulting in uncertain localization.4 Matsuda et al. have described a method that combines intraoperative laparoscopic ultrasonography with preoperative clipping and tattooing, but a disadvantage of this method is that clips may be applied erroneously in the anterior wall when the tumor is located at the posterior wall.4
In addition, peritonitis due to intraperitoneal/intestinal mucosal scattering through the intestinal puncture, intra-abdominal adhesion, and poor visual field are also disadvantages, and the effects of India ink under such conditions remain unknown.8,9,43 In contrast, our method with ICG, a bio-absorbable drug whose safety is guaranteed, is very useful for marking tumors because its visibility is independent on local factors, such as the tumor location, fat volume, and thickness of the stomach wall. Even if puncture occurs outside the alimentary tract, unlike the India ink tattooing, there is no color change after its spread to the peritoneal cavity/mesentery, and it does not hamper the surgical procedure.
However, this study has several limitations. First, the additional equipment required for ICG detection is more expensive than that required for India ink Tattooing. Second, the amount of time required for gastrointestinal endoscopy to inject ICG is much higher than that required for tattooing. Third, in this study, we selected the cases who received ICG marking on the day before surgery to investigate the efficacy of preoperative endoscopy. Therefore, further investigation is needed for evaluating the appropriate timing of ICG injection (e.g., immediately before surgery, during intraoperative endoscopy, etc.). Finally, the number of cases in this series was small, and data was obtained from a single institute. Further, ICG cannot be used in patients prescribed drugs or those allergic to the contrast agent. Therefore, it is necessary to acquire data from larger multi-centric studies to evaluate the safety and usefulness of using ICG fluorescence for determining the tumor location.
Conclusion
This is the first report that statistically proved that ICG fluorescence is useful in laparoscopic gastric cancer surgery. Determining the surgical resection line using ICG fluorescence is both useful and feasible as real-time confirmation is possible during the laparoscopic procedure itself. ICG use resulted in negative resection margins in all cases, shorter procedure time, lower estimated blood loss, and significantly shorter postoperative hospital stay and did not affect the procedure or result in adverse events. We think that ICG fluorescence is an invaluable marking method that can greatly facilitate next-generation surgery for gastric cancer.
References
Hachisu T, Miyazaki S, Hamaguchi K. Endoscopic clip-marking of lesions using the newly developed HX-3L clip. Surg Endosc. 1989;3(3):142–7.
Kojima F, Sato T, Tsunoda S, Takahata H, Hamaji M, Komatsu T et al. Development of a novel marking system for laparoscopic gastrectomy using endoclips with radio frequency identification tags: feasibility study in a canine model. Surg Endosc. 2014;28(9):2752–9. https://doi.org/10.1007/s00464-014-3501-2.
Ohdaira T, Nagai H, Shibusawa H. Intraoperative localization of early-stage gastrointestinal tumors using a marking clip detector system. Surgical Technology International. 2005;14:79–83.
Matsuda T, Iwasaki T, Hirata K, Tsugawa D, Sugita Y, Ishida S et al. Simple and reliable method for tumor localization during totally laparoscopic gastrectomy: intraoperative laparoscopic ultrasonography combined with tattooing. Gastric Cancer. 2017;20(3):548–52. https://doi.org/10.1007/s10120-016-0635-z.
Qi XD. [Gastroscopic mucosal biopsy and carbon ink injection marking for determination of resection line on the gastric wall in stomach cancer]. Zhonghua zhong liu za zhi [Chinese Journal of Oncology]. 1989;11(2):136–8.
Tokuhara T, Nakata E, Tenjo T, Kawai I, Satoi S, Inoue K et al. A novel option for preoperative endoscopic marking with India ink in totally laparoscopic distal gastrectomy for gastric cancer: a useful technique considering the morphological characteristics of the stomach. Molecular and clinical oncology. 2017;6(4):483–6. https://doi.org/10.3892/mco.2017.1191.
Kawakatsu S, Ohashi M, Hiki N, Nunobe S, Nagino M, Sano T. Use of endoscopy to determine the resection margin during laparoscopic gastrectomy for cancer. Br J Surg. 2017;104(13):1829–36. https://doi.org/10.1002/bjs.10618.
Park SI, Genta RS, Romeo DP, Weesner RE. Colonic abscess and focal peritonitis secondary to india ink tattooing of the colon. Gastrointestinal endoscopy. 1991;37(1):68–71.
Singh S, Arif A, Fox C, Basnyat P. Complication after pre-operative India ink tattooing in a colonic lesion. Digestive Surgery. 2006;23(5–6):303. https://doi.org/10.1159/000096245.
Chung JW, Seo KW, Jung K, Park MI, Kim SE, Park SJ et al. A promising method for tumor localization during total laparoscopic distal gastrectomy: preoperative endoscopic clipping based on negative biopsy and selective intraoperative radiography findings. Journal of Gastric Cancer. 2017;17(3):220–7. https://doi.org/10.5230/jgc.2017.17.e25.
Daskalaki D, Fernandes E, Wang X, Bianco FM, Elli EF, Ayloo S et al. Indocyanine green (ICG) fluorescent cholangiography during robotic cholecystectomy: results of 184 consecutive cases in a single institution. Surgical Innovation. 2014;21(6):615–21. https://doi.org/10.1177/1553350614524839.
Spinoglio G, Priora F, Bianchi PP, Lucido FS, Licciardello A, Maglione V et al. Real-time near-infrared (NIR) fluorescent cholangiography in single-site robotic cholecystectomy (SSRC): a single-institutional prospective study. Surg Endosc. 2013;27(6):2156–62. https://doi.org/10.1007/s00464-012-2733-2.
Luo S, Zhang E, Su Y, Cheng T, Shi C. A review of NIR dyes in cancer targeting and imaging. Biomaterials. 2011;32(29):7127–38. https://doi.org/10.1016/j.biomaterials.2011.06.024.
Namikawa T, Sato T, Hanazaki K. Recent advances in near-infrared fluorescence-guided imaging surgery using indocyanine green. Surg Today. 2015;45(12):1467–74. https://doi.org/10.1007/s00595-015-1158-7.
Alander JT, Kaartinen I, Laakso A, Patila T, Spillmann T, Tuchin VV et al. A review of indocyanine green fluorescent imaging in surgery. International Journal of Biomedical Imaging. 2012;2012:940585. https://doi.org/10.1155/2012/940585.
Goto O, Takeuchi H, Kawakubo H, Matsuda S, Kato F, Sasaki M et al. Feasibility of non-exposed endoscopic wall-inversion surgery with sentinel node basin dissection as a new surgical method for early gastric cancer: a porcine survival study. Gastric Cancer. 2015;18(2):440–5. https://doi.org/10.1007/s10120-014-0358-y.
Kim M, Son SY, Cui LH, Shin HJ, Hur H, Han SU. Real-time Vessel Navigation Using Indocyanine Green Fluorescence during Robotic or Laparoscopic Gastrectomy for Gastric Cancer. Journal of Gastric Cancer. 2017;17(2):145–53. https://doi.org/10.5230/jgc.2017.17.e17.
Tajima Y, Murakami M, Yamazaki K, Masuda Y, Kato M, Sato A et al. Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol. 2010;17(7):1787–93. https://doi.org/10.1245/s10434-010-0944-0.
Takahashi N, Nimura H, Fujita T, Mitsumori N, Shiraishi N, Kitano S et al. Laparoscopic sentinel node navigation surgery for early gastric cancer: a prospective multicenter trial. Langenbecks Arch Surg. 2017;402(1):27–32. https://doi.org/10.1007/s00423-016-1540-y.
Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer. 2012;15(3):287–91. https://doi.org/10.1007/s10120-011-0105-6.
Ozawa Y, Murakami M, Watanabe M, Yoshizawa S, Goto S, Otsuka K et al. Preoperative colonic cancer tattooing using the near-infrared fluorescence laparoscopic imaging system. Asian J Endosc Surg. 2016;9(4):340–3. https://doi.org/10.1111/ases.12306.
Watanabe M, Murakami M, Ozawa Y, Yoshizawa S, Matsui N, Aoki T. Intraoperative identification of colonic tumor sites using a near-infrared fluorescence endoscopic imaging system and indocyanine green. Digestive Surgery. 2017;34(6):495–501. https://doi.org/10.1159/000458450.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1–19. https://doi.org/10.1007/s10120-016-0622-4.
Hamabe A, Omori T, Tanaka K, Nishida T. Comparison of long-term results between laparoscopy-assisted gastrectomy and open gastrectomy with D2 lymph node dissection for advanced gastric cancer. Surg Endosc. 2012;26(6):1702–9. https://doi.org/10.1007/s00464-011-2096-0.
Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011;14(4):365–71. https://doi.org/10.1007/s10120-011-0054-0.
Kitagami H, Morimoto M, Nozawa M, Nakamura K, Tanimura S, Murakawa K et al. Evaluation of the delta-shaped anastomosis in laparoscopic distal gastrectomy: midterm results of a comparison with Roux-en-Y anastomosis. Surg Endosc. 2014;28(7):2137–44. https://doi.org/10.1007/s00464-014-3445-6.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Japanese Gastric Cancer A. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14(2):101–12. https://doi.org/10.1007/s10120-011-0041-5.
Squires MH, 3rd, Kooby DA, Pawlik TM, Weber SM, Poultsides G, Schmidt C et al. Utility of the proximal margin frozen section for resection of gastric adenocarcinoma: a 7-Institution Study of the US Gastric Cancer Collaborative. Ann Surg Oncol. 2014;21(13):4202–10. https://doi.org/10.1245/s10434-014-3834-z.
Kim MG, Lee JH, Ha TK, Kwon SJ. The distance of proximal resection margin dose not significantly influence on the prognosis of gastric cancer patients after curative resection. Annals of Surgical Treatment and Research. 2014;87(5):223–31. https://doi.org/10.4174/astr.2014.87.5.223.
Bissolati M, Desio M, Rosa F, Rausei S, Marrelli D, Baiocchi GL et al. Risk factor analysis for involvement of resection margins in gastric and esophagogastric junction cancer: an Italian multicenter study. Gastric Cancer. 2017;20(1):70–82. https://doi.org/10.1007/s10120-015-0589-6.
Hur H, Son SY, Cho YK, Han SU. Intraoperative gastroscopy for tumor localization in laparoscopic surgery for gastric adenocarcinoma. Journal of Visualized Experiments: JoVE. 2016(114). https://doi.org/10.3791/53170.
Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Efficacy of intraoperative gastroscopy for tumor localization in totally laparoscopic distal gastrectomy for cancer in the middle third of the stomach. Surg Endosc. 2013;27(11):4364–70. https://doi.org/10.1007/s00464-013-3042-0.
Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg. 2004;91(5):575–9. https://doi.org/10.1002/bjs.4470.
Kinami S, Oonishi T, Fujita J, Tomita Y, Funaki H, Fujita H et al. Optimal settings and accuracy of indocyanine green fluorescence imaging for sentinel node biopsy in early gastric cancer. Oncology Letters. 2016;11(6):4055–62. https://doi.org/10.3892/ol.2016.4492.
Miyashiro I, Kishi K, Yano M, Tanaka K, Motoori M, Ohue M et al. Laparoscopic detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging. Surg Endosc. 2011;25(5):1672–6. https://doi.org/10.1007/s00464-010-1405-3.
Tummers Q, Boogerd LSF, de Steur WO, Verbeek FPR, Boonstra MC, Handgraaf HJM et al. Near-infrared fluorescence sentinel lymph node detection in gastric cancer: a pilot study. World Journal of Gastroenterology. 2016;22(13):3644–51. https://doi.org/10.3748/wjg.v22.i13.3644.
Yoshida M, Kubota K, Kuroda J, Ohta K, Nakamura T, Saito J et al. Indocyanine green injection for detecting sentinel nodes using color fluorescence camera in the laparoscopy-assisted gastrectomy. Journal of Gastroenterology and Hepatology. 2012;27 Suppl 3:29–33. https://doi.org/10.1111/j.1440-1746.2012.07067.x.
Hiratsuka M, Miyashiro I, Ishikawa O, Furukawa H, Motomura K, Ohigashi H et al. Application of sentinel node biopsy to gastric cancer surgery. Surgery. 2001;129(3):335–40. https://doi.org/10.1067/msy.2001.111699.
Miyashiro I. What is the problem in clinical application of sentinel node concept to gastric cancer surgery? Journal of Gastric Cancer. 2012;12(1):7–12. https://doi.org/10.5230/jgc.2012.12.1.7.
Miyashiro I, Hiratsuka M, Kishi K, Takachi K, Yano M, Takenaka A et al. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: an institutional trial by experienced surgeons. Ann Surg Oncol. 2013;20(2):542–6. https://doi.org/10.1245/s10434-012-2608-8.
Miyashiro I, Hiratsuka M, Sasako M, Sano T, Mizusawa J, Nakamura K et al. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer. 2014;17(2):316–23. https://doi.org/10.1007/s10120-013-0285-3.
McArthur CS, Roayaie S, Waye JD. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg Endosc. 1999;13(4):397–400.
Author information
Authors and Affiliations
Contributions
Ushimaru designed the study and wrote the initial draft of the manuscript. Omori contributed to the interpretation of the data and to the critical revision of the manuscript for important intellectual content. All the other authors (Fujiwara, Yanagimoto, Sugimura, Yamamoto, Moon, Miyata, Ohue, and Yano) contributed to data collection and interpretation and critical review of the manuscript. All the authors have read and approved the final version of the manuscript and have agreed to the accountability of all aspects of the study, ensuring that any queries related to the accuracy or integrity of any part of the work are answerable.
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of the Osaka International Cancer Institute. All patients signed a written informed consent. Data collection and analysis were performed in compliance with the Helsinki Declaration of 1975.
Disclosures
Drs. Yuki Ushimaru, Takeshi Omori, Yoshiyuki Fujiwara, Yoshitomo Yanagimoto, Keijiro Sugimura, Kazuyoshi Yamamoto, Jeong-Ho Moon, Hiroshi Miyata, Masayuki Ohue, and Masahiko Yano have no conflicts of interest or financial ties to declare.
Conflict of Interest
There are no funding sources for this study or any associated financial conflicts.
Rights and permissions
About this article
Cite this article
Ushimaru, Y., Omori, T., Fujiwara, Y. et al. The Feasibility and Safety of Preoperative Fluorescence Marking with Indocyanine Green (ICG) in Laparoscopic Gastrectomy for Gastric Cancer. J Gastrointest Surg 23, 468–476 (2019). https://doi.org/10.1007/s11605-018-3900-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3900-0