Abstract
Purpose
The incidence of adenocarcinoma of the esophagogastric junction (AEG) and proximal gastric cancer (PGC) is rising worldwide. Recently, the use of indocyanine green (ICG) tracer-guided surgery has been reported; however, its efficacy for total/proximal gastrectomy has not been clarified. We evaluated the feasibility and safety of ICG fluorescent marking for tumor localization in AEG/PGC treatment by laparoscopic surgery.
Methods
We enrolled patients with AEG/PGC from October 2016 to March 2019 from a prospectively registered database. On the day before surgery, ICG markings were made at four locations just at the edge of the tumor by gastrointestinal fiberscope examination. Surgery was performed while viewing the fluorescence image of ICG, and the proximal portions of the esophagus and the distal portion of the stomach were resected at the edge of the area where ICG had spread.
Results
We enrolled 130 patients with AEG/PGC. Overall, 107 patients were eventually included in the study: AEG n = 64 (60%) and PGC n = 43 (40%). ICG markings were detected intraoperatively in all cases, and cancer invasion into the resection lines of the esophagus and stomach, performed based on ICG fluorescence images, was negative in all cases. The median visible range of ICG fluorescence was 22.5 mm. ICG diffusion expanded 20 mm proximal for AEG. There were no adverse events associated with endoscopic ICG injection.
Conclusion
ICG fluorescence imaging is feasible and safe and can potentially be used as a tumor-marking agent for determining the surgical resection line for total/proximal gastrectomy in AEG and PGC treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the incidences of adenocarcinoma of the esophagogastric junction (AEG) and proximal gastric cancer (PGC) have been rapidly increasing in Asian and Western countries, despite the decline in the incidence of lower gastric cancer [1,2,3,4,5]. The Siewert classification categorizes AEG into three subtypes according to the anatomical location of the tumor epicenter relative to the esophagogastric junction, as this reflects the differences in tumor behavior by location [6]. Lymph node metastasis is a well-known prognostic factor in malignant tumors [7]. The length of esophageal invasion has been reported to determine the frequency of mediastinal lymph node metastasis [7, 8]. Kurokawa et al. [8] performed lymph node mapping for esophagogastric junction tumors, including adenocarcinoma and squamous cell carcinoma, according to the Japanese Classification of Esophageal Cancer (11th edition) [9]. They recommended resection of lymph nodes with a metastatic rate of at least 5% and showed that the extent of lymph node resection should be determined according to the preoperative diagnosis of esophageal invasion.
Several studies have demonstrated that the length of the surgical margin from the resection line of the esophagus and esophageal infiltration was related to the prognosis of AEG [10,11,12]. Thus, securing the correct surgical margin with adequate lymphadenectomy is the fundamental goal of curative surgery. However, some previous studies have found discrepancies between preoperative Siewert classification and pathologic classification, especially in patients with large tumors or hiatal hernias [13, 14]. Furthermore, in minimally invasive surgeries, such as laparoscopic and robotic surgeries, determining the tumor location during surgery is difficult due to the lack of tactile sensation.
Recently, indocyanine green (ICG) fluorescence imaging has become popular in laparoscopic surgery. ICG binds to plasma proteins and fluoresces when stimulated by laser light [15, 16] or near-infrared (NIR) light [17, 18] with a wavelength of approximately 820 nm. The maximum absorption and emission wavelengths of ICG are about 807 nm and 822 nm, respectively [19]. A dedicated scope and camera then detect the fluorescence of the emitted ICG. Currently, ICG fluorescence imaging is used for navigational laparoscopic gastrectomy, lymphatic flow detection, blood flow visualization in gastric cancers [20,21,22,23,24,25,26], and tumor location during tumor resection in laparoscopic distal gastrectomy [27]. However, there are few reports of ICG fluorescence-guided gastrectomy in minimally invasive surgery for AEG and PGC.
Therefore, we evaluated the usefulness and safety of a preoperative ICG marking method by activating NIR fluorescence and a laparoscopic imaging system in treating AEG/PCG.
Materials and methods
Study design
This cohort study used prospectively registered data to evaluate the safety and efficacy of ICG fluorescence-guided gastrectomy for AEG and PGC. We enrolled patients with AEG according to the Japanese Classification of Esophageal Cancer (11th edition) [9]/PGC with a location of the tumor epicenter within 5 cm of the esophagogastric junction who were scheduled to undergo laparoscopic total or proximal gastrectomy from October 2016 to March 2019. Eligible participants included those ≥ 20 years old with histologically confirmed AEG and gastric cancer. The following exclusion criteria were applied: history of laparotomy; super-obese patients with body mass index ≥ 35, macroscopic type 4 (diffuse infiltrative) or 5 (unclassifiable) gastric cancer according to the Japanese Classification of Gastric Carcinoma, 3rd English Edition [28]; previous or other concomitant cancer; a renal, hepatic, or metabolic disorder (e.g., severe diabetes); cardiac disease; and a history of gastrectomy. Patients with R1 resection for positive peritoneal lavage cytology with no gross peritoneal dissemination were included, as gastrectomy for P0CY1 gastric cancer is a routine procedure. Patients with bulky lymph nodes or distant metastasis, such as para-aortic lymph node metastases, liver metastases, or peritoneal dissemination, were treated with chemotherapy followed by surgery. We also included patients who received neoadjuvant chemotherapy and those who had undergone conversion surgery after chemotherapy for unresectable gastric cancer.
This study was approved by the Institutional Review Board of Osaka International Cancer Institute (No. 18033–5). The data were collected and analyzed in accordance with the Declaration of Helsinki (1975). All patients provided written informed consent. Patients were withdrawn from the study if they withdrew consent or experienced a serious adverse event.
Study endpoints
The primary endpoints were the detection rate of ICG marking and the rate of negative infiltration to the esophageal and gastric resection lines. The secondary endpoints were the adverse events related to ICG injection, the length of the proximal margin, and the perioperative outcomes, including operative time, estimated blood loss, postoperative mortality, morbidity, and hospital stay. Morbidity was stratified as recommended by Dindo et al. [29]. The Japanese Classification of Gastric Carcinoma, 3rd English Edition, was used for TNM staging [28].
Preoperative ICG marking
The procedure for ICG marking has been described previously [27]. In our previous study, 0.05 mg/mL of Diagnogreen solution was submucosally injected into gastric mucosa at four sites (0.5 mL each; proximal, distal, and bilateral) around the tumor under preoperative endoscopic guidance. The visible range of ICG fluorescence was a median of 25 mm [27]. As in the previous study, the solution for ICG (Diagnogreen® Daiichi Sankyo Company, Limited (Tokyo, Japan)) marking was prepared by dissolving 1 V (25 mg) of Diagnogreen in 10 mL of distilled water, and 0.2 mL of this solution was mixed with 9.8 mL of distilled water to obtain a 10-mL solution (0.05 mg/mL of Diagnogreen). The prepared solution was submucosally injected into four sites (0.5 mL each; proximal, distal, and bilateral) just at the edge of the tumor under endoscopic guidance 1 day before surgery (Fig. 1). Postoperatively, clipping was performed at the injection site to evaluate the spread of ICG. After tumor resection, the extent of ICG spread from the clipping point was measured and recorded at four locations.
Laparoscopic equipment
All procedures were performed using a laparoscopic laser-free full HD system. Images were generated using an NIR/ICG telescope and a camera head system (IMAGE1 SPIES ™ System, KARL STORZ, Tuttlingen, Germany) connected to a 30-degree rigid high-definition scope equipped with a specific filter for optimal detection of NIR fluorescence and white light without manual switching. The xenon light source (D-LIGHT P, KARL STORZ) provided both visible and NIR excitation light, enhancing the background display. Using a footswitch, the surgeon controlled the change between white light and NIR fluorescence modes. Visualization of both standard and NIR light was improved by an image enhancement system (IMAGE1 STM System, KARL STORZ), which provided a visualization modality that could be adjusted according to the surgeon’s preference.
Surgical approach
Surgery was performed by three surgeons, including one experienced surgeon certified by the Japanese Society of Endoscopic Surgery (with more than 200 cases of experience in laparoscopic gastrectomy for gastric cancer) and two trainees. Trainees are always supervised by an experienced surgeon when performing this procedure. We have previously reported our surgical procedure for laparoscopic gastrectomy [30,31,32]. Briefly, the patient was placed in the reverse Trendelenburg position with their legs open. The surgeon stood between the patient’s legs, and assistants were present on either side of the patient. Transumbilical laparotomy was performed through a 2.5–3.0-cm vertical umbilical incision, and a wound protector (Lap protector; Hakko, Nagano, Japan) was placed. During the procedure, the abdominal cavity was secured with approximately 8–12 mmHg of carbon dioxide insufflation according to the patient’s body shape. Laparoscopic proximal gastrectomy (including lower esophagectomy if an esophageal invasion was present) was performed using five ports (one 12-mm port in the umbilicus, 5-mm and 12-mm ports in the right and left lateral abdomen, respectively). The esophagus and stomach were first illuminated with white light (Fig. 2). The ICG was then activated by NIR light and was observed using the laparoscopic imaging system to determine the location of the tumor. Laparoscopic ultrasonic coagulation scissors (Harmonic ACE, Ethicon Endosurgery, Cincinnati, OH, USA) were mainly used for esophageal and gastric mobilization and lymph node dissection. After dissection of the perigastric and suprapancreatic lymph nodes, the right and left crura of the diaphragm were cut to secure visualization of the lower mediastinal space. After opening the pericardial region, lymph nodes 110 and 111, bordering the pericardium and inferior vena cava, respectively, were dissected. Next, lymph node dissection was performed at stations 112ao along the aorta and 112pul along the lung. Finally, the esophagus and stomach were incised at the proximal/distal border of ICG staining using a linear stapling device with reference to ICG fluorescence images (ECHELON FLEX Powered ENDOPATH Stapler, Ethicon Endosurgery, Cincinnati, OH or Signia™ with a Tri-staple 60 mm purple cartridge, Medtronic, Ireland, Dublin), after which the resected specimen was extracted via a small incision. ICG staining was defined as a region containing bright or faint fluorescence (Fig. 3). After gross examination and measurement of serous tumor lesions, the esophagus and stomach were opened along the greater curvature to examine the stomach from the mucosal side and measure the size of the tumor and length of the proximal and distal resection margins. If a positive resection margin was suspected, a histological examination of the frozen section was performed intraoperatively, and if the pathological resection margin turned out to be positive, an additional resection of the distal esophagus was performed to make the proximal resection margin negative. After resection of the esophagus or stomach, the gastrointestinal tract was reconstructed using intracorporeal anastomosis [30, 31].
ICG-guided transection of the esophagus. a White light image. b Fluorescence image. ICG staining was defined as a region containing bright or faint fluorescence. The esophagus was transected at the border of ICG staining. Since it was possible to switch between visible and fluorescent images with a footswitch while viewing the positional relationship between the tumor and the gastric wall, it was particularly effective in determining the resection line. This way, real-time laparoscopic surgery under white light was made possible without the need for night vision confirmation. ICG, indocyanine green
Perioperative surgical outcomes
The data were collected prospectively and recorded in a computer database at our hospital. The collected data included patient characteristics, operative time, estimated blood loss, pathological findings (e.g., tumor depth, proximal and distal margins, number of lymph nodes dissected, and lymph node metastasis), postoperative morbidity rate, frequency of additional resection, and duration of postoperative hospital stay. Outcomes specific to ICG marking were the detection rate of ICG during gastrectomy, the size of the visualized ICG, morbidity after a preoperative upper endoscopy, and adverse effects after ICG injection.
Statistical analysis
All statistical calculations were performed using the JMP v14 software (SAS Institute, Inc., Cary, NC, USA). The demographic and clinicopathological characteristics are summarized descriptively. All quantitative values are expressed as mean and standard deviation unless otherwise stated. Student’s t-tests or Mann–Whitney U tests and Pearson’s χ2 tests were used to compare continuous and categorical variables, respectively. All values were two-tailed, and p-values < 0.05 were considered statistically significant.
Results
Baseline demographics and preoperative assessment
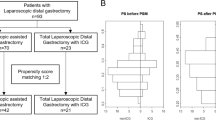
The study flow chart is summarized in Fig. 1. We enrolled 130 patients with AEG/PGC who underwent laparoscopic total or proximal gastrectomy between October 2016 and March 2019. Of these patients, 23 were excluded due to pathological neuroendocrine carcinoma (n = 2), type 4 or 5 gastric cancer (n = 20), and failed ICG infusion (n = 1). A total of 107 patients were eventually included in the study (median age, 70 years; 86 males and 21 females). The baseline characteristics of patients are summarized in Table 1. The median tumor size was 40 mm, and the median length of the esophageal invasion was 20 mm. Of the 107 patients, 64 (60%) had AEG (Siewert type I, n = 5; Siewert type II, n = 59), and 43 (40%) had PGC. Proximal gastrectomy was performed in 86 patients (80%), and total gastrectomy was performed in 21 patients (20%).
Perioperative outcomes
Surgical outcomes are summarized in Table 2. All surgeries were performed laparoscopically, and none of the cases required conversion to laparotomy. The median operative time was 292 min, and the estimated blood loss was 12.5 mL. Except for cases of gastric cancer with positive peritoneal leverage cytology (n = 3), peritoneal metastasis (n = 1), and lung metastasis (n = 1), R0 resection was achieved in all patients. Overall, postoperative complications were observed in 13 patients (13%). Only one patient (0.9%) had Clavien-Dindo grade III complication of pleural effusion. There were no anastomotic-related complications or pancreatic fistulas. The median postoperative hospital stay was 7 days, and no mortality was recorded in this cohort.
Assessment of surgical margin
The rates of negative infiltration to the resection line of the esophagus/stomach and surgical margin lengths are presented in Tables 2 and 3. All patients had negative proximal or distal infiltration to the resection line (100%). In patients with AEG, the median lengths of the proximal and distal margins were 27 mm (range: 2–60 mm) and 50 mm (range: 5–40), respectively. In patients with PGC, the median proximal margin was 34 mm (range: 5–65 mm), and the median distal margin was 45 mm (range: 7–180 mm). The esophagus was incised according to the ICG markings, and intraoperative gastrointestinal endoscopy was not required.
Intraoperative frozen section analysis deemed necessary by the surgeon was performed in 5 patients (3 examined the proximal margin, and 2 examined the distal margin). No patients had positive frozen sections except one. One patient had advanced cancer invading the diaphragmatic crura with positive peritoneal filtration cytology. The resection line was 3 cm away from the ICG mark location, but the frozen section of the proximal margin was positive. An additional 1-cm resection of the proximal esophagus resulted in a negative proximal resection and a pathologic proximal margin of 7 mm.
Outcomes of ICG injection
All ICG-specific outcome measures are presented in Tables 2 and 4. ICG markings were detected intraoperatively in all cases, and the resection of the esophagus and stomach was performed based on the ICG fluorescence images. There were four patients with BMI ≥ 30 in this study, and ICG marks were detected in all of them. No complications were associated with the upper gastrointestinal endoscopy performed for ICG injection, and no perioperative adverse events related to the use of ICG, such as intra-abdominal peritonitis or adhesion, were observed within the abdominal cavity during surgery.
The visible range of ICG fluorescence was 5–70 mm, with a median of 22.5 mm. ICG diffusion in the tumor was evaluated in four directions (proximal, distal, and bilateral), and no difference in ICG diffusion distance between these directions was observed. The median proximal ICG diffusion of all cases was 20 mm. ICG diffusion expanded 20 mm proximal to the esophagus for AEG and 25 mm for PGC. The median distance between the pathological proximal margin and the edge of proximal ICG diffusion (ΔPM) was 5 mm (interquartile range: 0–16.5 mm), and that of the distal margin (ΔDM) was 20 mm (interquartile range: 5–50 mm) (Fig. 4). ΔPM was 5 mm (interquartile range: 0–11.5 mm), and ΔDM was 20 mm (interquartile range: 5–50 mm) in patients with AEG.
Distance from the proximal/distal margins to the edge of the ICG diffusion region. The median distance from the pathological proximal margin and the edge of proximal ICG diffusion (ΔPM) was 5 mm (range: − 21–50 mm). ΔDM was 20 mm (range: − 10–145 mm). ΔPM, the distance from the pathological proximal margin and the edge of proximal ICG diffusion. ΔDM, the distance from the pathological distal margin and the edge of distal ICG diffusion. ICG, indocyanine green
Discussion
This study evaluated the safety and efficacy of preoperative ICG marking in minimally invasive surgery for AEG and PGC. The intraoperative ICG detection rate and the negative infiltration to the surgical resection line were 100%, and the use of ICG marking allowed us to secure the surgical margin and easily determine the esophageal and gastric resection lines. In addition, no adverse events related to ICG injection were observed in the perioperative period. Thus, ICG marking is useful for detecting tumor localization and resection lines in laparoscopic gastrectomy for AEG and PGC.
In laparoscopic surgery, the abdominal organs cannot be touched; thus, the tumor location can only be determined by the image on the monitor and the “sense of touch” through forceps. In addition, in early-stage and advanced gastric cancers, unless the tumor is exposed to the serosa, the exact tumor location cannot be visually confirmed by laparoscopy. Furthermore, the spread of cancer in the lumen of both early and advanced cancers cannot be detected outside the stomach wall.
Previous reports on surgical treatment of gastric cancer indicate that positive proximal margins have a poor prognosis; thus, the proximal margin should be kept negative [33, 34]. Moreover, the resection margin length from the resection line and esophageal invasion are associated with AEG prognosis [10,11,12]. Thus, ensuring the correct surgical margin is an essential goal of radical surgery. In the present study, we showed that all patients achieved negative surgical margins, and the median proximal margin was 30 mm, with resection of the expansive portion of ICG detected on extraluminal fluorescence imaging. Thus, our method helps obtain sufficient and appropriate surgical margins for AEG/PGC.
In this study, a histological examination of the frozen section was performed intraoperatively when a positive resection margin was suspected in the resection specimen. Although one case with an advanced tumor had a positive proximal margin, additional resection of the proximal esophagus allowed the surgical margin to be negative. In this case, the first resection line was 3 cm away from the ICG injection site, suggesting that tumor invasion was more proximal than endoscopically diagnosed. ICG marking may assist in detecting macroscopic tumor location, but we believe that frozen sections are necessary to confirm the negative pathologic surgical margin. A frozen section examination should be aggressively performed if a positive resection margin is suspected in the resection specimen.
In gastric cancer, preoperative endoscopic tattooing is a common practice; this method involves the injection of a dye, such as black ink, locally near the tumor under endoscopic guidance before surgery [35, 36]. However, depending on the location of the tumor, amount of fat, and thickness of the gastric wall, it may be difficult to identify the tattoo before surgery. Additionally, localization can be obscured due to the extensive spread of ink [37]. Another disadvantage is the splattering of intra-abdominal and intestinal mucosa following an intestinal puncture, leading to peritonitis, intra-abdominal adhesions, and poor visual field; the effect of ink under these conditions is unknown [38, 39]. In contrast, ICG, a bioabsorbable drug with guaranteed safety, is effective in marking tumors because it can be visualized regardless of local factors, such as tumor location, fat content, and stomach wall thickness. Even if ICG is punctured outside the gastrointestinal tract, unlike ink tattoos, no color change is observed after spreading to the abdominal cavity or mesentery. In this study, the intraoperative ICG detection rate was 100%, regardless of the patient’s body shape or tumor stage. When ICG was injected preoperatively at the proximal edge of the tumor, the median ICG spread was 20 mm on the mucosal side, equivalent to intraoperative extraluminal detection. Thus, preoperative intraluminal ICG injection is safe and effective for intraoperative detection of extraluminal ICG fluorescence excitation.
Intraoperative endoscopy helps confirm tumor location [40,41,42], but this method requires additional staff and prolongs operative time. Our method eliminates its need. In addition, verifying the localization of the marking clip by X-ray fluoroscopy is unnecessary. As a result, the operation time might be minimized, and surgical invasion might be reduced accordingly.
Our study has several limitations. First, the additional equipment needed for ICG detection is more expensive than that required for ink tattooing. Second, the time required for endoscopy-guided ICG injection is longer than that required for tattooing. Third, this study was limited to cases in which ICG marking was performed the day before surgery to exclude intraoperative endoscopy; further research is needed to determine the appropriate timing for ICG injection. Fourth, this study included a small number of cases from a single institution. Finally, ICG is not available for patients who are prescribed medications or are allergic to contrast media. Therefore, data from larger, multicenter studies are needed to evaluate the safety and usefulness of ICG fluorescence in determining tumor location.
Conclusion
This study demonstrated the usefulness of ICG fluorescence in laparoscopic surgery, including transhiatal lower esophagectomy for AEG. Determination of the surgical resection line using ICG fluorescence is useful and feasible, as it can be confirmed in real-time during laparoscopic surgery. The use of ICG resulted in negative resection margins in all cases, which did not affect the technique or cause any adverse events. We believe that ICG fluorescence is a valuable marking technique that will facilitate the next generation of AEG/PGC surgery.
References
Wu H, Rusiecki JA, Zhu K, Potter J, Devesa SS (2009) Stomach carcinoma incidence patterns in the United States by histologic type and anatomic site. Cancer Epidemiol Biomark Prev 18:1945–1952. https://doi.org/10.1158/1055-9965.EPI-09-0250
Steevens J, Botterweck AA, Dirx MJ, van den Brandt PA, Schouten LJ (2010) Trends in incidence of oesophageal and stomach cancer subtypes in Europe. Eur J Gastroenterol Hepatol 22:669–678. https://doi.org/10.1097/MEG.0b013e32832ca091
Kusano C, Gotoda T, Khor CJ, Katai H, Kato H, Taniguchi H, Shimoda T (2008) Changing trends in the proportion of adenocarcinoma of the esophagogastric junction in a large tertiary referral center in Japan. J Gastroenterol Hepatol 23:1662–1665. https://doi.org/10.1111/j.1440-1746.2008.05572.x
Blaser MJ, Saito D (2002) Trends in reported adenocarcinomas of the oesophagus and gastric cardia in Japan. Eur J Gastroenterol Hepatol 14:107–113. https://doi.org/10.1097/00042737-200202000-00003
Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, Kim WH, Lee KU, Yang HK (2011) Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg 98:255–260. https://doi.org/10.1002/bjs.7310
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the esophagogastric junction. Br J Surg 85:1457–1459. https://doi.org/10.1046/j.1365-2168.1998.00940.x
Koyanagi K, Kato F, Kanamori J, Daiko H, Ozawa S, Tachimori Y (2018) Clinical significance of esophageal invasion length for the prediction of mediastinal lymph node metastasis in Siewert type II adenocarcinoma: a retrospective single singleor the pred. Ann Gastroenterol Surg 2:187–196. https://doi.org/10.1002/ags3.12069
Kurokawa Y, Takeuchi H, Doki Y, Mine S, Terashima M, Yasuda T, Yoshida K, Daiko H, Sakuramoto S, Yoshikawa T, Kunisaki C, Seto Y, Tamura S, Shimokowa T, Sano T, Kitagwa Y (2021) Mapping of lymph node metastasis from esophagogastric junction tumors: a prospective nationwide multicenter study. Ann Surg 274:120–127. https://doi.org/10.1097/SLA.0000000000003499
Japan Esophageal Society (2017) Japanese Classification of Esophageal Cancer, 11th Edition: part II and III. Japan Esophageal Society Esophagus 14:37–65. https://doi.org/10.1007/s10388-016-0556-2
Mine S, Sano T, Hiki N, Yamada K, Kosuga T, Nunobe S, Yamaguchi T (2013) Proximal margin length with transhiatal gastrectomy for Siewert type II and III adenocarcinomas of the oesophagogastric junction. Br J Surg 100:1050–1054. https://doi.org/10.1002/bjs.9170
Barbour AP, Rizk NP, Gonen M, Tang L, Bains MS, Rusch VW, Coit DG, Brennan MF (2007) Adenocarcinoma of the gastroesophageal junction: influence of esophageal resection margin and operative approach on outcome. Ann Surg 246:1–8. https://doi.org/10.1097/01.sla.0000255563.65157.d2
Niclauss N, Jung MK, Chevallay M, Mönig SP (2019) Minimal length of proximal resection margin in adenocarcinoma of the esophagogastric junction: a systematic review of the literature. Updates Surg 71:401–409. https://doi.org/10.1007/s13304-019-00665-w
Leers JM, DeMeester SR, Chan N, Ayazi S, Oezcelik A, Abate E, Banki F, Lipham JC, Hagen JA, DeMeester TR (2009) Clinical characteristics, biologic behavior, and survival after esophagectomy are similar for adenocarcinoma of the gastroesophageal junction and the distal esophagus. J Thorac Cardiovasc Surg 138:594–602. https://doi.org/10.1016/j.jtcvs.2009.05.039
Grotenhuis BA, Wijnhoven BP, Poley JW, Hermans JJ, Biermann K, Spaander MC, Bruno MJ, Tilanus HW, van Lanschot JJ (2013) Preoperative assessment of tumor location and station-specific lymph node status in patients with adenocarcinoma of the gastroesophageal junction. World J Surg 37:147–155. https://doi.org/10.1007/s00268-012-1804-9
Daskalaki D, Fernandes E, Wang X, Bianco FM, Elli EF, Ayloo S, Masrur M, Milone L, Giulianotti PC (2014) Indocyanine green (ICG) fluorescent cholangiography during robotic cholecystectomy: results of 184 consecutive cases in a single institution. Surg Innov 21:615–621. https://doi.org/10.1177/1553350614524839
Spinoglio G, Priora F, Bianchi PP, Lucido FS, Licciardello A, Maglione V, Grosso F, Quarati R, Ravazzoni F, Lenti LM (2013) Real-time near-infrared (NIR) fluorescent cholangiography in single-site robotic cholecystectomy (SSRC): a single-institutional prospective study. Surg Endosc 27:2156–2162. https://doi.org/10.1007/s00464-012-2733-2
Luo S, Zhang E, Su Y, Cheng T, Shi C (2011) A review of NIR dyes in cancer targeting and imaging. Biomaterials 32:7127–7138. https://doi.org/10.1016/j.biomaterials.2011.06.024
Namikawa T, Sato T, Hanazaki K (2015) Recent advances in near-infrared fluorescence-guided imaging surgery using indocyanine green. Surg Today 45:1467–1474. https://doi.org/10.1007/s00595-015-1158-7
Alander JT, Kaartinen I, Laakso A, Pätilä T, Spillmann T, Tuchin VV, Venermo M, Välisuo P (2012) A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging 2012:940585. https://doi.org/10.1155/2012/940585
Goto O, Takeuchi H, Kawakubo H, Matsuda S, Kato F, Sasaki M, Fujimoto A, Ochiai Y, Horii J, Uraoka T, Kitagawa Y, Yahagi N (2015) Feasibility of non-exposed endoscopic wall-inversion surgery with sentinel node basin dissection as a new surgical method for early gastric cancer: a porcine survival study. Gastric Cancer 18:440–445. https://doi.org/10.1007/s10120-014-0358-y
Kim M, Son SY, Cui LH, Shin HJ, Hur H, Han SU (2017) Real-time vessel navigation using indocyanine green fluorescence during robotic or laparoscopic gastrectomy for gastric cancer. J Gastric Cancer 17:145–153. https://doi.org/10.5230/jgc.2017.17.e17
Tajima Y, Murakami M, Yamazaki K, Masuda Y, Kato M, Sato A, Goto S, Otsuka K, Kato T, Kusano M (2010) Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol 17:1787–1793. https://doi.org/10.1245/s10434-010-0944-0
Takahashi N, Nimura H, Fujita T, Mitsumori N, Shiraishi N, Kitano S, Satodate H, Yanaga K (2017) Laparoscopic sentinel node navigation surgery for early gastric cancer: a prospective multicenter trial. Langenbecks Arch Surg 402:27–32. https://doi.org/10.1007/s00423-016-1540-y
Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K (2012) The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer 15:287–291. https://doi.org/10.1007/s10120-011-0105-6
Kwon IG, Son T, Kim HI, Hyung WJ (2019) Fluorescent lymphography–guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg 154:150–158. https://doi.org/10.1001/jamasurg.2018.4267
Chen QY, Xie JW, Zhong Q, Wang JB, Lin JX, Lu J, Cao LL, Lin M, Tu RH, Huang ZN, Lin JL, Zheng HL, Li P, Zheng CH, Huang CM (2020) Safety and efficacy of indocyanine green tracer-guided lymph node dissection during laparoscopic radical gastrectomy in patients with gastric cancer: a randomized clinical trial. JAMA Surg 155:300–311. https://doi.org/10.1001/jamasurg.2019.6033
Ushimaru Y, Omori T, Fujiwara Y, Yanagimoto Y, Sugimura K, Yamamoto K, Moon JH, Miyata H, Ohue M, Yano M (2019) The feasibility and safety of preoperative fluorescence marking with indocyanine green (ICG) in laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg 23:468–476. https://doi.org/10.1007/s11605-018-3900-0
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma 3rd English Edition. Gastric Cancer 14:101–112. https://doi.org/10.1007/s10120-011-0041-5
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Omori T, Fujiwara Y, Moon J, Sugimura K, Miyata H, Masuzawa T, Kishi K, Miyoshi N, Tomokuni A, Akita H, Takahashi H, Kobayashi S, Yasui M, Ohue M, Yano M, Sakon M (2016) Comparison of single-incision and conventional multi-port laparoscopic distal gastrectomy with D2 lymph node dissection for gastric cancer: a propensity score-matched analysis. Ann Surg Oncol 23:817–824. https://doi.org/10.1245/s10434-016-5485-8
Omori T, Yamamoto K, Yanagimoto Y, Shinno N, Sugimura K, Takahashi H, Yasui M, Wada H, Miyata H, Ohue M, Yano M, Sakon M (2021) A novel valvuloplastic esophagogastrostomy technique for laparoscopic transhiatal lower esophagectomy and proximal gastrectomy for Siewert type II esophagogastric junction carcinoma-the tri double-flap hybrid method. J Gastrointest Surg 25:16–27. https://doi.org/10.1007/s11605-020-04547-0
Hamabe A, Omori T, Tanaka K, Nishida T (2012) Comparison of long-term results between laparoscopy-assisted gastrectomy and open gastrectomy with D2 lymph node dissection for advanced gastric cancer. Surg Endosc 26:1702–1709. https://doi.org/10.1007/s00464-011-2096-0
Squires MH 3rd, Kooby DA, Pawlik TM, Weber SM, Poultsides G, Schmidt C, Votanopoulos K, Fields RC, Ejaz A, Acher AW, Worhunsky DJ (2014) Utility of the proximal margin frozen section for resection of gastric adenocarcinoma: a 7-Institution Study of the US Gastric Cancer Collaborative. Ann Surg Oncol 21:4202–4210. https://doi.org/10.1245/s10434-014-3834-z
Kim MG, Lee JH, Ha TK, Kwon SJ (2014) The distance of proximal resection margin dose not significantly influence on the prognosis of gastric cancer patients after curative resection. Ann Surg Treat Res 87:223–231. https://doi.org/10.4174/astr.2014.87.5.223
Qi XD (1989) Gastroscopic mucosal biopsy and carbon ink injection marking for determination of resection line on the gastric wall in stomach cancer. Zhonghua Zhong Liu Za Zhi [Chinese Journal of Oncology] 11:136–138
Tokuhara T, Nakata E, Tenjo T, Kawai I, Satoi S, Inoue K, Araki M, Ueda H, Higashi C (2017) A novel option for preoperative endoscopic marking with India ink in totally laparoscopic distal gastrectomy for gastric cancer: a useful technique considering the morphological characteristics of the stomach. Mol Clin Oncol 6:483–486. https://doi.org/10.3892/mco.2017.1191
Matsuda T, Iwasaki T, Hirata K, Tsugawa D, Sugita Y, Ishida S, Kanaji S, Kakeji Y (2017) Simple and reliable method for tumor localization during totally laparoscopic gastrectomy: intraoperative laparoscopic ultrasonography combined with tattooing. Gastric Cancer 20:548–552. https://doi.org/10.1007/s10120-016-0635-z
Park SI, Genta RS, Romeo DP, Weesner RE (1991) Colonic abscess and focal peritonitis secondary to india ink tattooing of the colon. Gastrointest Endosc 37:68–71. https://doi.org/10.1016/S0016-5107(91)70627-5
Singh S, Arif A, Fox C, Basnyat P (2006) Complication after preoperative India ink tattooing in a colonic lesion. Dig Surg 23:303. https://doi.org/10.1159/000096245
Kawakatsu S, Ohashi M, Hiki N, Nunobe S, Nagino M, Sano T (2017) Use of endoscopy to determine the resection margin during laparoscopic gastrectomy for cancer. Br J Surg 104:1829–1836. https://doi.org/10.1002/bjs.10618
Hur H, Son SY, Cho YK, Han SU (2016) Intraoperative gastroscopy for tumor localization in laparoscopic surgery for gastric adenocarcinoma. J Vis Exp 53170. https://doi.org/10.3791/53170
Xuan Y, Hur H, Byun CS, Han SU, Cho YK (2013) Efficacy of intraoperative gastroscopy for tumor localization in totally laparoscopic distal gastrectomy for cancer in the middle third of the stomach. Surg Endosc 27:4364–4370. https://doi.org/10.1007/s00464-013-3042-0
Author information
Authors and Affiliations
Contributions
Study conception and design: TO, HH, and NS. Acquisition of data: TO and NS. Analysis and interpretation of data: TO and NS. Drafting of the manuscript: TO, HH, NS, and MY. Critical revision of the manuscript: TO, HH, NS, MY, TK, TT, HA, HW, MY, CM, JN, MO, MS, and HM.
Corresponding author
Ethics declarations
I confirm that I understand journal Langenbeck’s Archives of Surgery is a transformative journal. When research is accepted for publication, there is a choice to publish using either immediate gold open access or the traditional publishing route. No, I declare that the authors have no competing interests as defined by Springer or other interests that might be perceived to influence the results and/or discussion reported in this paper. The results/data/figures in this manuscript have not been published elsewhere, nor are they under consideration (from you or one of your contributing authors) by another publisher. I have read the Springer journal policies on author responsibilities and submit this manuscript in accordance with those policies. All of the material is owned by the authors, and/or no permissions are required.
Ethics approval
This study was approved by the Institutional Review Board of the Osaka International Cancer Institute (No. 18033–5). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments.
Consent to participate
Informed consent to be included in the study was obtained from all patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Omori, T., Hara, H., Shinno, N. et al. Safety and efficacy of preoperative indocyanine green fluorescence marking in laparoscopic gastrectomy for proximal gastric and esophagogastric junction adenocarcinoma (ICG MAP study). Langenbecks Arch Surg 407, 3387–3396 (2022). https://doi.org/10.1007/s00423-022-02680-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02680-9