Abstract
We study metastatic cancer progression through an extremely general individual-patient mathematical model that is rooted in the contemporary understanding of the underlying biomedical processes yet is essentially free of specific biological assumptions of mechanistic nature. The model accounts for primary tumor growth and resection, shedding of metastases off the primary tumor and their selection, dormancy and growth in a given secondary site. However, functional parameters descriptive of these processes are assumed to be essentially arbitrary. In spite of such generality, the model allows for computing the distribution of site-specific sizes of detectable metastases in closed form. Under the assumption of exponential growth of metastases before and after primary tumor resection, we showed that, regardless of other model parameters and for every set of site-specific volumes of detected metastases, the model-based likelihood-maximizing scenario is always the same: complete suppression of metastatic growth before primary tumor resection followed by an abrupt growth acceleration after surgery. This scenario is commonly observed in clinical practice and is supported by a wealth of experimental and clinical studies conducted over the last 110 years. Furthermore, several biological mechanisms have been identified that could bring about suppression of metastasis by the primary tumor and accelerated vascularization and growth of metastases after primary tumor resection. To the best of our knowledge, the methodology for uncovering general biomedical principles developed in this work is new.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
As every oncologist and veterinarian knows, cancer patients and tumor-bearing animals seldom present with clinically manifest metastases. Yet in a large fraction of subjects metastases surface within a few weeks, months or years after removal of the primary tumor. Is this just a coincidence or is there a causal relationship between (a) the presence of the primary tumor and metastatic dormancy; and (b) primary tumor resection and surfacing of metastases? Although a wealth of clinical cases and experiments on animal models accumulated over the last 110 years provide ample biomedical evidence supporting the suppressing effect of the primary tumor and accelerating effect of its ablation on metastasis, see Sect. 3, more definitive general conclusions have been so far elusive, for two reasons. First, dormant micrometastases and critical microevents that trigger their origination, escape from dormancy and progression to detectable secondary tumors in an individual subject are largely unobservable. Second, such randomly occurring microevents are separated by months, years or even decades from their clinical manifestations. These two factors make mathematical modeling an indispensable tool for establishing qualitative and quantitative relationships between various aspects of cancer natural history and assessing the effects of treatment.
Over a few recent decades our understanding of carcinogenesis and cancer progression has seen many dramatic shifts. For example, discoveries of (1) mutational origins of cancer; (2) metabolic plasticity of cancer cells; (3) aberrant regulation of cell cycle, proliferation and apoptosis in cancer cells; (4) the role of angiogenesis in cancer progression; (5) significance of primary and secondary tumor dormancy; (6) complex interactions of cancer cells with the immune and endocrine systems; (7) a critical role of tumor microenvironment as well as local and systemic interactions among various cell types; (8) an important role of inflammation in cancer origination and progression; and (9) identification of cancer stem cells have all considerably changed the landscape of cancer research. Undoubtedly, many other aspects of cancer still remain unknown. That is why answering systemic questions like those posed in this work cannot rely on mathematical models based on specific biological mechanisms. This and other limitations of traditional mathematical modeling call for a different approach.
In this work, we develop an alternative methodology that, to the best of our knowledge, has never been employed in the past. Its main driving force is an extremely general mathematical model of cancer origination and progression in an individual patient that is rooted in basic cancer biology and yet is essentially free of any specific assumptions of mechanistic nature, see Sect. 4. The model combines deterministic description of the pre-surgery primary tumor dynamics and growth of metastases in a given secondary site with stochastic description of the processes that clearly depend on chance (Kendal 2006) such as shedding of metastases off the primary tumor, their selection, and dormancy in a given site. However, the “trick” is that the laws governing primary tumor dynamics, the rate of metastasis shedding, the site-specific distribution of metastasis dormancy times, and metastatic growth are very general in that they are essentially assumed to have only qualitative properties (such as monotonicity, continuity or differentiability) rather than specific functional form. Thus, the model largely avoids the step of initial parameterization that would make it rigid at the outset. Such highly flexible models were discussed and advocated by Hanin (2013). The model described in this work is an extension of a somewhat less general model introduced and studied by Hanin et al. (2006) and Hanin (2008). In spite of its generality, the model still allows for explicit formulas for the distribution of various clinically significant variables observable in a particular patient.
A set of observations most suitable for our purposes is the collection of volumes of metastases detected in a given secondary site (typically lungs, liver, bones, brain or soft tissue). Such volumetric data can be obtained through laborious reading of CT/PET images. Examples of such data sets, their mathematical and statistical analyses based on various parametric versions of our model, and of relevant biomedical findings can be found in Hanin et al. (2006, 2016), Hanin and Korosteleva (2010), Hanin and Zaider (2011), Hanin and Bunimovich-Mendrazitsky (2014), and Hanin and Rose (2016). A general question regarding clinical conclusions that can, or cannot, be made on the basis of such models from a sample of site-specific volumes of metastases was discussed from mathematical and biomedical standpoints by Hanin et al. (2016).
To answer our main question about the effects of primary tumor in situ and its removal on the rate of growth of metastases, we do have to parameterize one part of our model: the laws of growth of metastases before and after primary tumor removal. Quite often, clinical metastases are detected early when they are likely to be still in the exponential phase of their growth. Therefore, in order to compare the growth of metastases pre- and post-surgery, we assumed that vascular metastases lodged in a given site grow exponentially with two rates, not necessarily distinct—one before and one after primary tumor resection, and estimated these two parameters from a given sample of site-specific volumes of metastases. To retain model generality, all other functional parameters were assumed arbitrary. Furthermore, the model of metastatic growth is presented in Sect. 4 in a general form that goes far beyond the exponential law. This makes the model more flexible, allows one to accommodate observations with large metastatic volumes that cannot be assumed to result from exponential growth, and enables an extension of our analysis to parametric families of metastasis growth functions other than exponential in the future.
One of the most appealing ways to estimate the two rates of exponential metastatic growth from data is to select their values that maximize the model-based probability of observations. This fundamental idea, called the Principle of Maximum Likelihood, goes back to Lagrange, Daniel Bernoulli, Euler, Laplace and Gauss, see, e.g., Stigler (2007).
Application of the Principle of Maximum Likelihood has led us to a surprising discovery: for any sample of site-specific volumes of detectable metastases, the likelihood-maximizing scenario is invariably the same—complete suppression of metastatic growth while primary tumor is in place followed by a sudden growth acceleration after primary tumor resection. This conclusion is based, apart from standard assumptions about independent and (distributionally) identical behavior of metastases in a given site, likelihood maximization, and the assumption of exponential growth of metastases pre- and post-surgery, on the premise that metastasis shedding off the primary tumor is governed by a Poisson process (with essentially arbitrary time-dependent rate), see Sect. 4 for more details. Our finding does not mean, of course, that the above scenario should necessarily occur for all solid cancers and all patients. However, due to the generality of our model and conclusions, it provides a compelling explanation for the fact that this scenario is very common in clinical practice.
The outline of the article and the basic flow of ideas are as follows. A brief conceptual overview of the dynamics of solid cancer including metastasis is presented in Sect. 2. Extensive biomedical evidence for the suppression of metastasis by the primary tumor and escape from dormancy following primary tumor resection as well as several possible explanations of this phenomenon are reviewed in Sect. 3. A mathematical model of individual cancer natural history is introduced in Sect. 4 while in Sect. 5 we present the model-based distribution of site-specific volumes of metastases. In Sect. 6 we describe the outcome of likelihood maximization and the resulting limiting model. Finally, in Sect. 7 we formulate and discuss our conclusions.
2 Dynamics of Primary and Secondary Tumors: A Brief Summary
Solid primary tumors originate from a single malignant clonogenic cell or a group of such initiator cells. Unlike normal cells of the same tissue origin, cancer cells have an abnormal control of cell cycle and apoptosis and can evade regulatory signals from the microenvironment. Tumor growth is enabled by the supply of nutrients, oxygen and growth factors which are initially delivered through diffusion. However, according to a fundamental discovery made by Folkman (1974), under such conditions a tumor can only reach a microscopic diameter of about 1–2 mm. To enable its further growth, the tumor has to induce angiogenesis, i.e., develop a capillary network that will provide a more efficient supply of essential chemicals. If the effects of angiogenesis inhibitors are stronger than those of angiogenesis promoters then the tumor may indefinitely reside in a state of dormancy characterized by a dynamic equilibrium between cell proliferation, death and quiescence (Hadfield 1954; Sugarbaker et al. 1971; Holmgren et al. 1995). In the opposite case [or if external microenvironmental or systemic factors such as inflammation, infection, trauma and irradiation shift the balance in favor of pro-angiogenic factors, an event referred to as angiogenic switch (Folkman 2002)], the tumor will vascularize and start an irreversible aggressive growth. This event will be called primary tumor inception.
The most clinically significant aspect of the progression of solid cancers is metastasis, which accounts for about 90% of all cancer-related deaths, see, e.g., Spano et al. (2012). A primary tumor may start shedding bloodborne metastases as soon as it becomes vascularized, i.e., following inception. Because the minimum diameter for clinical detection of tumors is about 5 mm, the aforementioned Folkman’s limit for avascular tumors suggests that at the time of inception primary and secondary tumors may still be undetectable.
Metastasis is a complex multi-stage process (Fidler 1990). A metastasis-generating cell has to separate itself from the primary tumor, migrate to a blood vessel, intravasate, survive through the period of free circulation, extravasate and invade a host site. A solitary metastatic cell lodged in a secondary site may remain dormant (i.e., in the \({G}_{0}\) phase of the cell cycle) for months, years or even decades (Marches et al. 2006). Under favorable conditions it may start to grow, induce angiogenesis and eventually enter the clinical stage. Thus, metastasis is a highly inefficient and selective process in that only a tiny fraction of cancer cells shed off the primary tumor give rise to clinically detectable secondary tumors. Just as for primary tumor, the start of irreversible aggressive growth of a vascular metastasis will be termed inception.
3 Inhibition of Metastasis by the Primary Tumor and the Effects of Its Resection: Biomedical Evidence
Investigation of the interaction between various tumors was initiated by a pioneering work of Ehrlich (1906), see also Bashford et al. (1907). The main conclusion of this and many other experimental studies on animals was that large tumors suppress the growth of smaller ones, see a comprehensive review by Gorelik (1983). In particular, primary tumor in situ impedes the growth of metastases (DeWys 1972; Sugarbaker et al. 1977). This effect is one of the many reasons behind metastatic dormancy whose fundamental role for understanding cancer natural history has been acknowledged and well-documented long ago by Alexander (1983), Holmgren et al. (1995) and Demicheli et al. (1997). It comes, then, as no surprise that resection of a large primary tumor could lead to accelerated growth of metastases. The first experimental study of this phenomenon goes back to the 1910s (Tyzzer 1913). Since then it was observed directly in numerous animal experiments and countless clinical cases where surgical removal of the primary tumor was followed by a sudden rapid outgrowth of multiple metastases, see reviews by Demicheli et al. (2008), Retsky et al. (2010) and Hanin (2013). A vast body of experimental, clinical and epidemiological evidence amassed over the last 110 years has proven that surgical removal of the primary tumor may trigger escape from metastatic dormancy, promote angiogenesis and accelerate the growth of vascular secondary tumors. Mathematical models applied to real data have led to the same conclusion (Hanin and Korosteleva 2010; Hanin and Zaider 2011; Hanin and Bunimovich-Mendrazitsky 2014; Hanin and Pavlova 2016).
A number of non-mutually exclusive mechanisms explaining the suppressive effects of primary tumor in situ and stimulating effects of primary tumor resection on metastases have been proposed:
(1) An explanation due to Prehn (1993) is based on the observation that tumors produce growth and angiogenesis factors as well as inhibitors of these processes. While growth and angiogenesis factors are easily degradable and spread mostly locally by diffusion, their inhibitors are more stable and when shed into the blood stream may reach distant sites and suppress metastatic progression. When the primary tumor is removed, the supply of the inhibitors is cut off, which causes vascularization of metastases and boosts their growth.
(2) Resection of the primary tumor (and any surgery for that matter, see Maida et al. 2009) leads to an increase in local and systemic production of growth and angiogenesis factors required for wound healing. As these factors are captured by dormant or slowly growing metastases, their vascularization and growth are accelerated.
(3) Surgery brings about transient inflammation that may boost cancer progression. The idea that cancer is closely associated with inflammation was advanced by Rudolf Virchow in 1863 and is supported by numerous clinical and experimental studies (Balkwill and Mantovani 2001). A related hypothesis is that inflammation stimulates and fuels metastasis. One of many ways in which this may occur is due to the increase in blood vessel permeability caused by inflammation, which facilitates both intravasation of cancer cells shed off the primary tumor and extravasation of circulating tumor cells. Finally, a striking, if only indirect, evidence of a strong association between inflammation and cancer progression was discovered by a group of Belgian anesthesiologists who found that perioperative use of non-steroidal anti-inflammatory analgesic ketorolac has led to a fivefold reduction in short-term (i.e., within 9–18 months post-surgery) relapses of breast cancer (Forget et al. 2010). This remarkable phenomenon was explained by Retsky et al. (2013) and extensively discussed by Retsky and Demicheli (2017).
(4) Immunogenic primary tumor serves as a source of antigens that activate dendritic cells (DCs) of the immune system (Vatner et al. 2014). When activated DCs reach lymph nodes they in turn activate naïve T cells converting them into cytotoxic lymphocytes (CTLs). The latter flow with the blood circulation and may extravasate at distant metastatic sites thus inhibiting the growth of metastases. After excision of the primary tumor, this massive CTL trafficking is abrogated causing metastases to escape the immune surveillance and start aggressive proliferation.
(5) The adrenergic and inflammatory effects of surgery lead to temporary, yet significant, immunosuppression caused by the perturbed functioning of T-lymphocytes, macrophages, natural killer cells, monocytes and other cells of the immune system (Hiller et al. 2017). This strong perioperative signal may cause “awakening” of dormant micrometastases and their active propagation.
4 A Mathematical Model of Individual Cancer Natural History
A mathematical model introduced by Hanin et al. (2006), Hanin (2008), Hanin and Korosteleva (2010) and presented in its most general form below accounts for the basic aspects of cancer dynamics described in Sect. 2. Its only very mild assumptions are dictated by mathematical convenience and serve the purpose of facilitating mathematical and statistical analysis without unduly restricting the scope of biological possibilities allowed by the model.
Primary tumor growth The model of primary tumor growth describes the dynamics of clonogenic cancer cells after primary tumor inception. These cells are of greatest clinical importance because (a) each of them can regenerate the whole tumor; and (b) some of them may give rise to metastases. The total number of clonogenic cells within the primary tumor at any time t counted from the age, T, of primary tumor inception will be denoted by \(\Phi ({t})\). The significance of primary tumor inception is twofold: First, this is the earliest time when the primary tumor may start shedding bloodborne metastases; and, second, before inception an avascular tumor may grow according to a law different from \(\Phi \) or even remain dormant. It is assumed that up until the time, V, of primary tumor resection \(\Phi \) is a continuous positive function, not necessarily increasing. Allowing a deviation from monotonic increase can account for primary tumor dynamics in patients receiving neo-adjuvant local or systemic treatments, i.e., given radio-, chemo-, immuno- and/or hormonal therapy before surgery.
Metastasis formation We assume that metastasis shedding is governed by a Poisson process whose rate, \(\mu ({t})\), is proportional to the number, L(t), of metastases-producing cells at time \({t}: \mu ({t}) = \alpha {L(t)}\) with constant \(\alpha > 0\), where time t is counted from primary tumor inception. The unobservable number L(t) depends on the current number of clonogenic cells: \({L(t)} = {r}[\Phi ({t})]\), where r is a continuous function with \({r(0)} = 0\) and \({r(x)}> 0\) for \({x}> 0\). Thus, \(\mu ({t}) = \alpha {r}[\Phi ({t})]\). Perhaps the most important examples of function r, explored in Hanin et al. (2006, 2016), Hanin (2008), Hanin and Korosteleva (2010), Hanin and Zaider (2011), Hanin and Bunimovich-Mendrazitsky (2014), Hanin and Rose (2016), are of the form \({r(x)} = \beta {x}^{\theta }\), where \(\beta > 0\) and \(\theta \ge 0\). The case \(\theta = 1\) implies that a fixed fraction of clonogenic cells in the primary tumor have metastatic potential. The case \(\theta = 2/3\) arises under the assumption that metastatic cells originate from the blood vessel-rich surface of the primary tumor, assumed spherical. Finally, if \(\theta = 0\) then the population of metastases-producing cells has constant size, which suggests that it has self-renewal capacity, e.g., through asymmetric division.
It is further assumed that metastases shed by the primary tumor survive and give rise to clinically detectable secondary tumors in a given site independently of each other with the same probability \({q}> 0\). Therefore, see, e.g., Ross (1997, pp. 257–259), inception of metastases in the site of interest is governed by a Poisson process with the rate \(\nu ({t}) = {q}\mu ({t})\).
Next, each viable metastasis is assumed to spend some random time between detachment from the primary tumor and inception in the secondary site, termed metastasis latency time. Latency times of viable metastases bound for a given site are independent and identically distributed (iid) with some continuous probability density function (pdf) f and the corresponding cumulative distribution function (cdf) F. Then, see, e.g., Hanin and Yakovlev (1996), the resulting delayed Poisson process is again a Poisson process with the rate
We assume for simplicity that the growth of all vascular metastases in the site in question starts from the same initial size, \({N}_{0}\), at inception. This implies that the duration of metastatic latency is bounded below by a certain minimal time \(\tau > 0\) during which a metastasis can reach the microscopic size \({N}_{0}\) if it starts to grow at the maximum possible rate immediately after seeding. Accordingly, we assume that \({f(t)} = 0\) for \(0 \le {t} \le \tau \) and \({f(t)}> 0\) tor \(\tau < {t} \le {W}-{T}\), where W is the age at metastasis detection. We think of \(\tau \) as a sufficiently small number so that \(T + \tau < {V}\), see Fig. 1.
Metastasis measurement The size of a metastasis becomes measurable when it exceeds some threshold value m. This value and the accuracy of size measurement depend on the secondary site and the sensitivity of imaging technology. A typical threshold m corresponds to metastatic diameter of about 5 mm while the diameter of metastasis at inception is close to the avascular limit of about 1–2 mm. Therefore, we assume that \({m} > {N}_{0}\).
Schematic timeline of the natural history of metastatic cancer and its treatment in an individual patient. All times are represented as ages counted from the birth of the patient. \({T} + {U}\) is the age at inception of a particular metastasis. Note that the inception may occur either before or after surgery. Numbers with arrows above the timeline represent sizes of the metastasis at the indicated time points
Timeline of metastatic cancer progression and observables Suppose that at age V the primary tumor was resected, and that at age \({W} > {V}\) the patient developed \({n} \ge 1\) detectable metastases in a given secondary site with the observed sizes \({X}_{1}, {X}_{2},\ldots , {X}_{{n}}\), where \({m} < {X}_{1} \le {X}_{2} \le \cdots \le {X}_{{n}}\). Thus, \(0< {T}< {V} <{W}\), see Fig. 1. Initially, the sizes of metastases are represented in volumetric form. Some of these volumes may be identical due to image discretization and rounding. To convert the volume of a metastasis into its size (the number of cells), one has to divide the volume by the volume of a single cell, assumed the same for all metastatic cells in a given site. The corresponding distinct sizes of metastases will be denoted \({Y}_{1}, {Y}_{2},\ldots ,{Y}_{{k}}\), where \({k} \le {n}\), with the understanding that \({Y}_{1}< {Y}_{2}< \cdots < {Y}_{{k}}\). Let also \({Y}_{0}: = {m}\) and \({Z} = {X}_{{n}} = {Y}_{{k}}\) be the largest size of detected metastases.
Metastatic growth Denote by U the inception time of a particular metastasis relative to the age, T, of primary tumor inception, so that \({T} + {U}\) is the patient’s age at metastasis inception, see Fig. 1. Let \(\Psi _{{U}}{(t)}\) be the size of the metastasis at time t counted from time U. Recall that \(\Psi _{{U}}(0) = {N}_{0}\). Observe that, in contrast to the primary tumor, \(\Psi _{{U}}\) accounts for the total number of cancer cells, both clonogenic and non-clonogenic; the reason is that measured at age W are the total volumes of metastases.
In our likelihood maximization argument in Sect. 6, we will assume that every viable metastasis in a given site grows exponentially before and after primary tumor excision with respective rates \(\gamma _{0 }\) and \(\gamma _{1}\), not necessarily distinct. Then in the case \({T} + {U} < {V}\) we have \(\Psi _{{U}}{(t)} = {N}_{0}\exp \{\gamma _{0}{t}\}\) if \(0 \le {t} \le {V}- {T}-{U}\) and \(\Psi _{{U}}{(t)} = {N}_{0}\exp \{\gamma _{0}({V}-{T} -{U})\}\exp \{\gamma _{1 }[{t} - ({V}-{T}-{U})]\}\) if \({t} > {V} -{T} -{U}\), see Fig. 1. Similarly, if \({T} + {U} \ge {V}\) then \(\Psi _{{U}}{(t)} = {N}_{0}{\exp }\{\gamma _{1}{t}\}\), \({t} \ge 0\). In a simpler setting where \(\gamma _{1} = \gamma _{0}\) studied by Hanin et al. (2006), \(\Psi _{{U}}{(t)}\) is a function of t alone, independent of the inception time U. However, if the rate of metastatic growth is affected by resection of the primary tumor (\(\gamma _{1} \ne \gamma _{0})\), this is not true anymore.
The exponential law \(\Psi {(t)} = {N}\hbox { exp}\{\gamma {t}\}\) with \(\gamma > 0\) describes propagation of identical clones generated by N initial cells and growing at constant net per-cell rate \(\gamma \) under the assumption of no interaction between cells. To obtain a more general model of metastatic growth, we relax this assumption by prohibiting interaction only between the clones generated by the cells in a given metastasis present at the time, V, of primary tumor resection if \({T} + {U} < {V}\) or at the post-surgery metastasis inception time \({T} + {U}\) if \({T} + {U} \ge {V}\) while allowing cell interactions within the clones. Such interactions may be due to spatial proximity between cells resulting in contact inhibition and competition for space, nutrients, oxygen and growth factors, and other reasons. As discussed in Sects. 2 and 3, at these two time moments the dynamics of a metastasis may undergo major transformation. It follows from our assumptions that after such a transformation, the size of a metastasis post-surgery can be represented as the product of the number of cells present at the time of transformation and the clone growth function, which will be denoted \(\Psi _{1}\). Although a similar multiplication rule may be also adopted for the pre-surgery metastasis inception, it is technically unnecessary. In the context of clones occupying separate biological niches, a similar approach was proposed by Fakir et al. (2013).
Our model of metastatic growth is based on the following assumptions:
(1) Prior to primary tumor resection, the growth of each viable metastases in a given site is governed by the same function \(\Psi _{0}{(t)}\), where time t is counted from the age \({T} + {U}\) of metastasis inception (individual for each metastasis), with \(\Psi _{0}(0) = {N}_{0}\);
(2) Clones generated by metastatic cells present at time V (or at the metastasis inception time if \({T} + {U} > {V}\)) in a given site grow independently according to the same function \(\Psi _{1 }\) with \(\Psi _{1}(0) = 1\);
(3) Functions \(\Psi _{0}\) and \(\Psi _{1}\) are increasing and differentiable.
Clearly, in the case of exponential metastatic growth discussed above all these assumptions are met. Similar to the exponential case we have:
Observe that function \(\Psi _{{U}}{(t)}\) is increasing, continuous and piecewise differentiable.
Secondary metastasis and the effects/outcomes of treatment Secondary metastasizing (that is, formation of “metastasis of metastasis”) to a given site, both from other sites and from within, is assumed negligible. The resected primary tumor is supposed to be non-recurrent. Thus, formation of new metastases stops at the time of primary tumor resection. Other treatments, including chemo-, immuno-, radiation or hormonal therapies, are assumed to affect metastases only through the rate of their growth (and not through a change in the distribution of their latency times).
5 Distribution of the Sizes of Detectable Metastases
Let X be the size of a particular metastasis with inception time U detected in a given site and surveyed at age W. According to (1)
where \(W-T-U\) is the total metastasis progression time from inception to detection. An important observation is that the function that relates the size X of a metastasis at age W to its progression time actually does not depend on U:
where
Note that function \(\Psi \) is increasing, continuous, piecewise differentiable, and satisfies the condition \(\Psi (0) = {N}_{0}\). The inverse function, \(\delta : = \Psi ^{ -1}\), is given by
It follows from (2) and (3) that the theoretical upper limit for the size of a metastasis at patient’s age W under the model assumptions is
It represents the size of a hypothetical metastasis whose inception with size \({N}_{0}\) occurred over the shortest latency period possible, i.e., at time \({T} + \tau \), see Fig. 1. Clearly, \({M} > {Z}\) (recall that Z is the largest among the sizes of metastases observed at age W).
According to formula (2) the sizes of metastases are a fixed non-random transformation \(\Psi \) of their inception times which, under our model, follow a Poisson process. Then, using a well-known theorem about the conditional joint distribution of the event occurrence times in a Poisson process conditional on their number, see, e.g., Ross (1997, pp. 264–265), we obtain the following result.
Theorem 1
The sizes \({X}_{1} \le {X} _{2} \le \cdots \le {X}_{{n}}\) of metastases in a given site that are detectable at age W are equidistributed, given their number n, with the vector of order statistics for a random sample of size n drawn from the distribution with pdf
and \(p(x) = 0\) for \(x \notin (m, M).\)
For a proof of Theorem 1 in the case \({r(x)} = \beta {x}^{\theta },\) see Hanin et al. (2006); the proof in the general case is obtained by a minor modification. Distribution (6) depends on functional parameters \(\Phi , {r}, \Psi _{0}, \Psi _{1}\) and f. Notice, however, that it is free of parameters \(\alpha \) and q involved in the rate of shedding of viable metastases and independent of the sample size n. The patient- and/or site-specific biological parameters \({T}, {N}_{0}, \tau \), m as well as observables V and W are assumed fixed.
Denote by \({A}: = {N}_{0 }\Psi _{1}({W}-{V})\) the size at age W of a hypothetical metastasis whose inception with initial size \({N}_{0 }\) occurred at the age V of primary tumor resection, then \({N}_{0}< {A} < {M}\). Observe that in view of (3) \({W} -{T} -\delta {(x)} \le {V} -{T}\) if and only if \({x} \ge \Psi ({W}-{V}) = {N}_{0 }\Psi _{1}({W} -{V}) = {A}\). Therefore, in the case \({A} \le {m}\) we have
while if \({A} > {m}\) then
The first and second formulas in (8) account for metastases whose inception occurred after and before primary tumor resection, respectively. From (4) and (5) we find that \(\delta {(M)} = {W} -{T} -\tau \). Therefore, in view of our assumption about the support of pdf f, we have \({p(M-)} = 0\). Thus, pdf p is continuous at point M. By contrast, pdf p(x) has typically a jump discontinuity at points m and \({A}> {m}\). Finally, because \({W} -{T} - \delta {(m)} > {W} -{T} - \delta {(M)} = \tau \), the denominator in formulas (7) and (8) is positive.
Due to the non-stationarity of the Poisson process of metastasis inception, the sizes of metastases detectable in a given secondary site at age W do not form a random sample from a probability distribution. However, it follows from Theorem 1 that the distribution of any symmetric (i.e., rearrangement-invariant) statistic based on the observations \({X}_{1}, {X}_{2},\ldots , {X}_{{n}}\) is identical to the distribution of the same statistic based on a random sample of size n drawn from the pdf p given by formula (6). One of such statistics is the joint likelihood of observations
Therefore, identifiable parameters of a suitably parameterized model of the natural history of metastatic cancer described above can be estimated using the Principle of Maximum Likelihood. If one of the observed volumes of metastases coincides with A then, in order to maximize the likelihood, the larger of the two one-sided limits of the pdf p(x) at \({x} = {A}\) should be employed.
6 Model Parameterization and Optimization
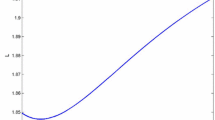
To quantify the effects of the presence of the primary tumor and its resection on the growth of metastases, we assume that before and after resection of the primary tumor metastases grow exponentially with respective rates \(\gamma _{0}, \gamma _{1} > 0: \Psi _{0}{(t)} = {N}_{0 }\exp \{\gamma _{0}{t}\}\) and \(\Psi _{1}{(t)} = \exp \{\gamma _{1}{t}\}\). Then
and according to (4)
Note that in the case \({A} \le {m}\) function \(\delta \) is given by the second formula in (11). It follows from (11) that \(\delta \) is a continuous function on the interval (m, M) and
Because cell cycle duration has a lower limit, d, the growth rate of any cell population is bounded above by \((\mathrm{ln}2)/d\). Another growth rate-limiting factor is cell death due to apoptosis and necrosis. Therefore, parameters \(\gamma _{0}\) and \(\gamma _{1 }\) are bounded above by some constant K. However, quiescence and the possibility of equilibrium between cell proliferation and death suggest that these parameters may approach zero. Observe that due to the constraint \({M}> {Z} > {m}\) and in view of (10) the rates \(\gamma _{0}\) and \(\gamma _{1}\) cannot tend to zero simultaneously. Let \({G} = {(0, K)} \times {(0, K)}\) be the set of admissible pairs \((\gamma _{0}, \gamma _{1})\). Finally, denote
This quantity represents the rate of growth of a metastasis whose inception occurred at age V and that reached size u at age W. Our main goal in this section is to prove the following result.
Theorem 2
For any fixed functional parameters \(\Phi , {r}, {f}\) and for every data set \({X}_{1}, {X}_{2},\ldots , {X}_{{n}},\) the supremum of the likelihood function \({L}(\gamma _{0}, \gamma _{1})\) given by (9) over the set G is infinite. Furthermore, if \({L}(\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\,\, \rightarrow \,\, \infty \) for some sequence \((\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\) in G then \(\gamma _{0}^{({n})}\rightarrow 0\) and \(\gamma _{1}^{(\mathrm{n})}\rightarrow g(Z)\)-.
Proof
The conclusion of the theorem will follow from exploring the behavior of all the factors in the likelihood function \({L}(\gamma _{0}, \gamma _{1})\) defined by (9) for a given set of observations under three conditions: (a) for \(\gamma _0 \rightarrow 0\) and appropriately chosen \(\gamma _{1}\); (b) for \(\gamma _1 \rightarrow 0\) and fixed \(\gamma _{0}\); and (c) when \(\gamma _{0}\) and \(\gamma _{1}\) are bounded away from zero.
(a) Suppose that \(\gamma _0 \rightarrow 0\). Fix \(\rho \) such that \(0< \rho < {V} -{T} -\tau \) and set
which implies that \({A} < {Z}\). In view of (10) this defines parameter \(\gamma _{1}\) as follows:
Clearly, for sufficiently small \(\gamma _{0}\), we have \(\gamma _{1} > 0\) and \({A} > {Y}_{{k}-1}\). Notice that \(\gamma _1 \rightarrow g(Z)-\) as \(\gamma _0 \rightarrow 0\). Thus, \({m} = {Y}_{0}< {Y}_{1}< {\cdots }<{Y}_{{k}-1}< {A}< {Y}_{{k}} = {Z} < {M}\) and \({A}, {M} \rightarrow Z\) as \(\gamma _0 \rightarrow 0\).
We first compute the limit of p(Z) as \(\gamma _0 \rightarrow 0\). Note that \({p}^{{s}}{(Z)}\), where s is the multiplicity of the observation \({Y}_{{k}} = {Z}\), is the factor in (9) corresponding to the largest observed volume of metastases. Invoking the second formula in (11), (13) and (14) we have
so that \({W} -{T} -\delta {(Z)} = {V} -{T} -\rho \). It follows from the first formula in (11) and (14) that
The second equation in (8) and (12) imply that
where in view of (15), (16) and due to the inequality \({V} -{T} -\rho > \tau \) we have
Thus, \(p{(Z)}\rightarrow \infty \) as \(\gamma _0 \rightarrow 0\).
We now compute the limits as \(\gamma _0 \rightarrow 0\) of the other factors in (9) that correspond to (single or multiple) observations \({Y}_{{j}} < {A}, 1 \le {j} \le {k}-1\). Along the lines of (16) we obtain
Using the first formula in (8) and (12) we find that
where by (17) we have for \(1 \le {j} \le {k}-1\):
Setting \({B}_{{k}}: = {W}-{V}\) we extend formula (17) to \({j} = 0\), see (16), and \({j} = {k}\). Then
This implies that the limit of \({Q}_{{j}}(\gamma _{0}), 1 \le {j} \le {k} -1\), as \(\gamma _0 \rightarrow 0\) is finite and positive. Then the same is also true for the limit of \(p{(Y}_{j} )\). In summary, we showed that if \(\gamma _0 \rightarrow 0\) and \(\gamma _{1 }\) is given by (14) then \({L(}\gamma _0 ,\gamma _1 )\rightarrow \infty \). Thus, supremum of the likelihood function over the set G is infinite.
(b) We now turn to the case \(\gamma _1 \rightarrow 0\) with fixed \(\gamma _{0} > 0\). Here we have \(A\rightarrow N_0 <m\), \(M\rightarrow N_0 \exp \{\gamma _0 (V-T-\tau )\}\) and \(\delta (x)\rightarrow B(x)+W-V\) for \({m}< {x} < {M}\), where
Using (7) we find that
where
From the inequalities \({m}<{Z}<{M}\) it follows by taking limit as \(\gamma _1 \rightarrow 0\) that \(m<N_0 \exp \{\gamma _0 (V-T-\tau )\}\) or equivalently \({V}-{T}-{B}{(m)} > \tau \). This implies that
Thus, in the case \(\gamma _1 \rightarrow 0\) with fixed \(\gamma _{0} > 0\) the likelihood function has finite limit.
(c) Suppose now that \(\gamma _{0}\) and \(\gamma _{1}\) are bounded away from zero. Consider a fixed observation Y with \({m}< {Y} < {M}\). We first look at the case \({A} \le {m}\), or equivalently \(0 < \gamma _{1} \le {g(m)}\), where pdf p is given by (7). In accordance with our model assumptions and in view of (11) and (12), p(Y) is a continuous function of \((\gamma _{0}, \gamma _{1})\). Similarly, the same conclusion is true in the (overlapping) cases \({m} < {Y} \le {A}\) (that is, for \(\gamma _{1} \ge {g(Y)}\)) and \({Y} \ge {A} > {m}\) (i.e., for \({g(m)} < \gamma _{1} \le {g(Y)}\)), where pdf p is given by the first and second formulas in (8), respectively. Therefore, the likelihood function \({L}(\gamma _{0}, \gamma _{1})\) is bounded above on any subset of G where \(\gamma _{0}\) and \(\gamma _{1}\) are bounded away from 0.
Let us now assume that \({L}(\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\rightarrow \infty \) for some sequence \((\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\) in G. We first show that \(\gamma _{0}^{({n}) }\rightarrow 0\). Suppose not, then by passing to a subsequence we may assume without loss of generality that \(\gamma _{0}^{({n}) }\rightarrow \gamma _{0} > 0\). If \(\gamma _{1}^{({n}) }\rightarrow 0\) then a slight modification of our argument in part (b) accounting for variable \(\gamma _{0 }\)would show that the sequence \({L}(\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\) has finite limit, which is a contradiction. In the opposite case where \(\gamma _{1}^{({n}) }\) does not converge to zero we may assume without restricting generality that \(\gamma _{1}^{({n}) }\rightarrow \gamma _{1} > 0\). Then by part (c) the sequence \({L}(\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\) is bounded, again a contradiction. Thus, \(\gamma _{0}^{({n}) }\rightarrow 0\).
Next, denote by \({A}^{({n})}\) and \({M}^{({n})}\) the values of parameters A and M, see (10), for the sequence \((\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\). To finish the proof, we need the following result.
Claim
\({A}^{({n})} \le {Z}\) for all sufficiently large n.
To show this, suppose this is false, then \({A}^{({n})} >{Z}\), or equivalently \(\gamma _{1}^{({n})} >{g(Z)}\), for an infinite subsequence of indices n. Again, without loss of generality we may assume that \(\gamma _{1}^{({n}) }\rightarrow \gamma _{1}{}^{*} \ge {g(Z)}\). Using the first formula in (11) we find that
Also, from the first formula in (8) and (12) we obtain
where in view of (19)
Observe that according to (16) and because \(\gamma _{1}{}^{*} \ge {g(Z)}\) we have \({C}_{0} \le {B}_{0}\), which implies in view of (18) with \({j} = 0\) that the denominator in the limits in (20) is positive. Therefore, all the limits in (20) are finite. Thus, we constructed a subsequence of indices n for which \({L}(\gamma _{0}^{({n})}, \gamma _{1}^{({n})})\) has finite limit. This contradiction proves our Claim.
Finally, in view of (10) inequalities \({A}^{({n})} \le {Z} < {M}^{({n})}\) are equivalent to
Since \(\gamma _{0}^{({n}) }\rightarrow 0\) and the inequalities in (21) hold for all sufficiently large n, we conclude that \(\gamma _{1}^{({n}) }\rightarrow {g(Z)}\)-. This completes the proof of Theorem 2.
Remark
A minor modification of the proof of part (a) would show that \({L(}\gamma _0 ,\gamma _1 )\rightarrow \infty \) if \((\gamma _0 ,\gamma _1 )\rightarrow (0,g(Z)-)\) non-tangentially in the sense that \({g(Z)} - \gamma _{1} \le {C} \gamma _{0}\) for some fixed constant C such that
Theorem 2 reveals that, according to the model, the most likely scenario for the n detected metastases is as follows. All those (say, \(\nu \)) metastases whose inception occurred before resection of the primary tumor remained essentially dormant (\(\gamma _{0} \rightarrow 0\)) before surgery while after it they were growing at a rate \(\gamma _{1 }\) close to g(Z) and by age W reached volumes close to the maximum observed volume Z. Additionally, the remaining \(n - \nu \) metastases whose inception occurred after surgery were growing at about the same rate \(\gamma _{1}\) and by age W reached more widely spread volumes \({X}_{1}, {X}_{2}, \dots , {X}_{{n}-\nu }\). As we showed in Sect. 3, the pre-surgery suppression of metastatic growth and its post-surgery acceleration predicted by the model are widely observed in the real world and may be explained by a number of biological mechanisms.
Finally, we describe the limiting model where \(\gamma _{0} = 0\) and \(\gamma _{1} = {g(Z)}\). We start with the following important observation related to the general model (8). Integrating the first formula in (8) we find that in the case \({A} > {m}\)
is independent of \(\Psi _{0}\), see (4). In particular, in the case of exponentially growing metastases, \(\mu \) is independent of \(\gamma _{0}\). According to our model and Theorem 1, \(\mu \) represents the conditional probability, given the number of site-specific detectable metastases at age W, of the event that the inception of a randomly chosen detected metastasis occurred before resection of the primary tumor. Note also that in the case \({A} \le {m}\) we have \(\mu = 1\).
In the limiting case at hand in view of (10) and \(\gamma _{1} = {g(Z)}\) we have \({A} = {Z} = {M} = {N}_{0}\exp \{\gamma _{1}({W-V})\}\). Therefore, \(\nu \ge 1\). The limiting distribution for (8), then, is a mixture of an absolutely continuous distribution with (improper) pdf
where
and a point mass \(\eta \) at M, where
The limiting model depends on parameters \(\Phi , {r}, {f}, {M}\) or alternatively \(\Phi , {r}, {f}, \eta \). Parameter \(\eta \) can be optimized from a sample of observations \({X}_{1}, {X}_{2},\ldots , {X}_{{n}}\), where \({m}< {X}_{1} \le {X}_{2} \le \cdots \le {X}_{{n}- \nu } < {X}_{{n}-\nu +1} = {\cdots } = {X}_{{n}} = {Z}\) with \(\nu \ge 1\), using the Method of Maximum Likelihood. Then \({M} = {Z}\), and the likelihood, viewed as a function of independent parameter \(\eta \), has the form
where \(\Lambda _{0}\) is independent of \(\eta \). The likelihood function is maximized for \(\eta = \nu /{n}\), where \(\nu \) is the multiplicity of the maximum observed volume Z. This imposes a constraint
on the remaining model parameters \(\Phi \), r and f.
7 Conclusions and Discussion
The main question addressed in this work concerns the effects of primary tumor and its resection on the rate of growth of metastases. We found that, according to our model, the most likely scenario is complete suppression of metastatic growth in the presence of the primary tumor followed by active growth after primary tumor resection. Because this is true regardless of the sizes of metastases detected in a given secondary site, this conclusion is essentially a property of our model. However, extreme generality and flexibility of the model allows us to hypothesize that what we have found is “something real” that stems from the very basic temporal and kinetic aspects of metastasis rather than from specific biological mechanisms. In fact, our results are supported by more than a century of clinical observations and experimental studies on animals that produced plentiful evidence, both direct and circumstantial, for two inter-related principles: (1) the metastasis-suppressing effect of the primary tumor; and (2) accelerated growth of metastases after surgical removal of the primary tumor, see Sects. 2 and 3 for more details. We do not claim that our conclusions hold true for all types of solid cancer and all categories of patients nor that metastases cannot eventually escape the inhibiting effect of the primary tumor or remain dormant after its removal. However, what we have discovered by means of mathematical modeling and statistical analysis represents a very common cancer progression scenario.
The model described in Sect. 4 is based on several mathematical assumptions. Central among them is that the process of metastasis shedding off the primary tumor is Poisson. However, the rate of the Poisson process was assumed to be essentially arbitrary. Other mathematical assumptions posit independence and homogeneity properties of the progression of individual metastases. Specifically, we assumed that metastases bound for a given secondary site evolve independently of each other, survive with the same probability, have the same initial size at inception and identically distributed latency times, and grow according to the same laws before and after primary tumor resection. Finally, we postulated some qualitative properties of the model’s functional parameters such as monotonicity, continuity and differentiability. Without all these or similar assumptions, mathematical modeling of metastasis would barely be possible.
Specific biological assumptions of the model were minor. The first of them, that secondary metastasis is negligible, was made out of necessity, for in practice primary and secondary metastases are indistinguishable thus making generation number of a metastasis unobservable. Also, existing biomedical evidence suggests that secondary metastasis is relatively uncommon (Hölzel et al. 2010). The second assumption is the supposition that various treatments of the primary tumor affect metastases through the rate of their growth rather than through a change in their latency times. For chemo-, radiation-, immuno- and hormone therapies, it is to a large degree a statement of fact: It is well-known that dormant micro-tumors and quiescent cancer cells are refractory to these types of treatment, see, e.g., Kleffel and Schatton (2013). For surgery, however, the situation is very different. Although our generic model assumed that surgery does not affect the distribution of latency times, see Sect. 4, application of the Principle of Maximum Likelihood showed, paradoxically, that this is not true for the likelihood maximizing limiting model characterized by zero metastatic growth prior to primary tumor excision. In this case, the phases of metastatic latency and pre-surgery growth become indistinguishable. Biologically, this amounts to extending the latency of metastases after inception until surgery. This observation suggests that the most important way of model refinement would be to incorporate two latency phases: one before and one after surgery. In this case, however, the total metastasis latency times cannot be assumed identically distributed.
From a statistical point of view, our main result, Theorem 2, may seem counterintuitive. Imagine that a large sample of metastatic sizes is generated by model (6) with fixed parameters \(\Phi , {r}, {f}\) and \(\gamma _{0}, \gamma _{1} > 0\). One would expect, contrary to Theorem 2, the maximum likelihood estimates of parameters \(\gamma _{0}, \gamma _{1}\) to be close with high probability to their “true” values. The explanation of this “paradox” is that pdf (6) is discontinuous at point \({A} > {m}\) and, therefore, does not satisfy the regularity conditions that guarantee consistency of the maximum likelihood estimator, see, e.g., Karr (1993, p. 202).
The workings of Nature, of course, are not constrained by the above mathematical and biological assumptions nor do they have to maximize the likelihood. The question, then, is how metastasis suppression by the primary tumor came into being. It is well-known that cancer was common in human ancestors. Also, in most cases primary tumor is not lethal per se; metastases are. Therefore, any natural mechanism of metastasis suppression by the primary tumor including those described in Sect. 3 would confer on its bearers a survival and reproductive advantage over those who do not have this mechanism in place. This would also allow the bearers of this trait to pass it on to the offspring. This hypothetical, and perhaps highly speculative, explanation represents one scenario by which metastasis suppression by the primary tumor could have emerged over the long course of evolution through natural selection.
The limiting likelihood-maximizing model described in Sect. 6 predicts that the observed sets of volumes of metastases may contain, along with widely spread volumes corresponding to metastases whose inception occurred after surgery, some number \(\nu \ge 1\) of tightly clustered metastatic volumes that are much larger than other volumes and come from metastases whose inception occurred prior to surgery. This unexpected pattern was actually observed in several previously analyzed patients. In particular, it occurred in two breast cancer patients with \({n} = 20\) and \({n} = 31\) bone metastases (\(\nu = 1\)) (Hanin and Korosteleva 2010); a renal cancer patient with \({n} = 55\) lung metastases (\(\nu = 1\)) (Hanin et al. 2016); and a prostate cancer patient with \({n} = 36\) bone metastases (\(\nu = 3\)) (Hanin and Zaider 2011; Hanin and Bunimovich-Mendrazitsky 2014).
It is also interesting to mention that in those cases where parametric versions of the model described in Sect. 4 were identifiable, optimization of model parameters in the interior of the parameter space has also led to the conclusion that resection of the primary tumor accelerates the growth of metastases. In fact, when the model with exponentially growing primary tumor and metastases, exponentially distributed latency times and \({r(x)} = \beta {x}^{\theta }\) with \(\beta > 0\) and \(\theta \ge 0\) was applied to the data for the aforementioned breast and prostate cancer patients with \({n} = 31\) and \({n} = 36\) bone metastases, the resulting ratio \(\gamma _{1 }/\gamma _{0}\) was found to be 32 and 4, respectively, notwithstanding the fact that after surgery, in order to prevent local recurrence and metastatic relapse, the breast cancer patient was put on hormonal therapy with tamoxifen while the prostate cancer patient was given radiation, chemotherapy and hormonal therapy (Hanin and Korosteleva 2010; Hanin and Zaider 2011). A similar conclusion also followed when the growth of the primary tumor in these patients was assumed to be governed by the Gompertz law (Hanin and Bunimovich-Mendrazitsky 2014).
Results of this work may potentially have far-reaching clinical implications for cancer diagnosis, staging, treatment and discovery of biomarkers for subclinical metastatic disease. In particular, our results suggest that for some types of cancer and categories of patients keeping primary tumor intact while controlling its growth rather than surgical removal may perhaps be a better metastasis prevention strategy than primary tumor excision. For a detailed biomedical discussion of this hypothesis in the case of breast cancer, see Hanin (2017). Many cancer biologists and oncologists have arrived at a similar conclusion. For example, Bernard Fisher, one of the greatest American breast cancer oncologists of the twentieth century, wrote about the treatment of breast cancer in a review article that summarized his work spanning half a century: “...it is likely that surgery for the disease will continue to diminish in importance...” (Fisher 1999).
References
Alexander P (1983) Dormant metastases: studies in experimental animals. J Pathol 141:379–383
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Bashford E, Murray J, Cramer W (1907) The natural and induced resistance of mice to the growth of cancer. Proc R Soc Lond 79:164–187
Demicheli R, Retsky MW, Swartzendruber DE, Bonadonna G (1997) Proposal for a new model of breast cancer metastatic development. Ann Oncol 8:1075–1080
Demicheli R, Retsky M, Hrushesky WJM, Baum M, Gukas ID (2008) The effects of surgery on tumor growth: a century of investigations. Ann Oncol 19:1821–1828
DeWys WD (1972) Studies correlating the growth rate of a tumor and its metastases and providing evidence for tumor-related systemic growth-retarding factors. Cancer Res 32:374–379
Ehrlich P (1906) Experimentelle Karzinomstudien an Mäusen. Arch Koiglichen Inst Exp Ther Frankfurt am Main 1:65–103 (in German)
Fakir H, Hlatky L, Li H, Sachs R (2013) Repopulation of interacting tumor cells during fractionated radiotherapy: stochastic modeling of the tumor control probability. Med Phys 40(12):121716
Fidler IA (1990) Critical factors in the biology of human cancer metastasis: twenty-eighth G. H. A. Clowes memorial award lecture. Cancer Res 50:6130–6138
Fisher B (1999) From Halsted to prevention and beyond: advances in the management of breast cancer during the twentieth century. Eur J Cancer 35:1963–1973
Folkman J (1974) Tumor angiogenesis factor. Cancer Res 34:2109–2113
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29(6), Suppl 16:15–18
Forget P, Vandenhende J, Berliere M, Machiels JP, Nussbaum B, Legrand C, DeKock M (2010) Do intraoperative analgesics influence breast cancer recurrence after mastectomy? A retrospective analysis. Anesth Analg 110(6):1630–1635
Gorelik E (1983) Concomitant tumor immunity and resistance to a second tumor challenge. Adv Cancer Res 39:71–120
Hadfield G (1954) The dormant cancer cell. Br Med J 2:607–610
Hanin LG (2008) Distribution of the sizes of metastases: mathematical and biomedical considerations. In: Tan WY, Hanin LG (eds) Handbook of cancer models with applications. World Scientific, Singapore, pp 141–169
Hanin LG (2013) Seeing the invisible: how mathematical models uncover tumor dormancy, reconstruct the natural history of cancer and assess the effects of treatment. In: Almog N, Enderling H, Hlatky L (eds) Systems biology of tumor dormancy. Advances in experimental medicine and biology, vol 734. Springer, New York, pp 261–282
Hanin L (2017) Do breast cancer patients benefit from surgery? Hypotheses, mathematical models and false beliefs. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 161–182
Hanin LG, Yakovlev AY (1996) A nonidentifiability aspect of the two-stage model of carcinogenesis. Risk Anal 16:711–715
Hanin LG, Korosteleva O (2010) Does extirpation of the primary breast tumor give boost to growth of metastases? Evidence revealed by mathematical modeling. Math Biosci 223:133–141
Hanin L, Zaider M (2011) Effects of surgery and chemotherapy on metastatic progression of prostate cancer: evidence from the natural history of the disease reconstructed through mathematical modeling. Cancers 3:3632–3660
Hanin LG, Bunimovich-Mendrazitsky S (2014) Reconstruction of the natural history of metastatic cancer and assessment of the effects of surgery: gompertzian growth of the primary tumor. Math Biosci 247:47–58
Hanin L, Pavlova L (2016) A quantitative insight into metastatic relapse of breast cancer. J Theor Biol 394:172–181
Hanin L, Rose J (2016) Uncovering the natural history of cancer from post mortem cross-sectional diameters of hepatic metastases. Math Med Biol 33(4):397–416
Hanin LG, Rose J, Zaider M (2006) A stochastic model for the sizes of detectable metastases. J Theor Biol 243:407–417
Hanin L, Seidel K, Stoevesandt D (2016) A “universal” model of metastatic cancer, its parametric forms and their identification: what can be learned from site-specific volumes of metastases. J Math Biol 72(6):1633–1662
Hiller J, Schier R, Riedel B (2017) Perioperative biologic perturbation and cancer surgery: targeting the adrenergic-inflammatory response and microcirculatory dysregulation. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 83–107
Holmgren K, O’Reilly MS, Folkman J (1995) Dormancy of micrometastases: balanced proliferation and apoptosis in the presence of angiogenesis suppression. Nat Med 1:149–153
Hölzel D, Eckel R, Emeny RT, Engel J (2010) Distant metastases do not metastasize. Cancer Metastasis Rev 29:737–750
Karr AF (1993) Probability. Springer, New York
Kendal WS (2006) Chance mechanisms affecting the burden of metastases. BMC Cancer 5:138
Kleffel S, Schatton T (2013) Tumor dormancy and cancer stem cells: two sides of the same coin? In: Almog N, Enderling H, Hlatky L (eds) Systems biology of tumor dormancy. Advances in experimental medicine and biology, vol 734. Springer, New York, pp 145–179
Maida V, Ennis M, Kuziemsky C, Corban J (2009) Wounds and survival in cancer patients. Eur J Cancer 45:3237–3244
Marches R, Scheuermann R, Uhr J (2006) Cancer dormancy-from mice to man. Cell Cycle 5(16):1772–1778
Prehn RT (1993) Two competing influences that may explain concomitant tumor resistance. Cancer Res 53:3266–3269
Retsky M, Demicheli R (2017) Perioperative inflammation as a triggering origin of metastasis development. In: Retsky M, Demicheli R (eds) Perioperative inflammation as a triggering origin of metastasis development. Springer, New York, pp 19–54
Retsky M, Demicheli R, Hrushesky W, Baum M, Gukas I (2010) Surgery triggers outgrowth of latent distant disease in breast cancer: an inconvenient truth? Cancers 2:305–337
Retsky M, Demicheli R, Hrushesky WJM, Forget P, DeKock M, Gukas I, Rogers RA, Baum M, Sukhatme V, Vaidya JS (2013) Reduction of breast cancer relapses with perioperative non-steroidal anti-inflammatory drugs: new findings and a review. Curr Med Chem 20(33):4163–4176
Ross SM (1997) Introduction to probability models, 6th edn. Academic Press, San Diego
Spano D, Heck C, De Antonelli P, Christofori G, Zollo M (2012) Molecular networks that regulate cancer metastasis. Semin Cancer Biol 22(3):234–49
Stigler SM (2007) The epic story of maximum likelihood. Stat Sci 22(4):598–620
Sugarbaker EV, Ketcham AS, Cohen AM (1971) Studies of dormant tumor cells. Cancer 28:545–552
Sugarbaker E, Thornswaite J, Ketcham A (1977) Inhibitory effect of a primary tumor on metastasis. In: Day S, Myers W, Stansly P, Garattini S, Lewis M (eds) Progress in cancer research and therapy, vol 5. Raven Press, New York, pp 227–240
Tyzzer EE (1913) Factors in the production and growth of tumor metastases. J Med Res 28:309–332
Vatner RE, Cooper BT, Vanpouille-Box C, Demaria S, Formenti SC (2014) Combinations of immunotherapy and radiation in cancer therapy. Front Oncol 4:325
Acknowledgements
Incisive and constructive comments by the two anonymous reviewers have helped the authors to considerably improve the manuscript. The reviewers’ suggestions are greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hanin, L., Rose, J. Suppression of Metastasis by Primary Tumor and Acceleration of Metastasis Following Primary Tumor Resection: A Natural Law?. Bull Math Biol 80, 519–539 (2018). https://doi.org/10.1007/s11538-017-0388-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-017-0388-9