Abstract
Microcystis aeruginosa produces an abundant cyanotoxin (microcystins (MCs) in freshwater supplies. MCs have adverse health hazards to animals and humans. Microcystin-leucine-arginine (microcystin-LR or MC-LR) is the most studied among these MCs due to their high toxicity. So, this study was designed to evaluate the possible therapeutic role of the natural algal food supplement, Spirulina platensis (SP), against MC-LR-induced toxic effects in male Wistar rats. Forty rats were randomly divided into five groups. Control and SP groups orally administered distilled water and SP (1000 mg/kg/daily), respectively, for 21 days. MC-LR group was intraperitoneally injected with MC-LR (10 μg/kg/day) for 14 days. MC-LR-SP500 and MC-LR-SP1000 groups were orally treated with SP (500 and 1000 mg/kg, respectively) for 7 days and concomitantly with MC-LR for 14 days. MC-LR induced oxidative hepatorenal damage, cardiotoxicity, and neurotoxicity greatly, which was represented by reduction of reduced glutathione content and the activities of glutathione peroxidase, catalase, and superoxide dismutase and elevation of concentrations of nitric oxide and malondialdehyde in renal, hepatic, brain, and heart tissues. In addition, it increased serum levels of urea, creatinine, tumor necrosis factor-alfa, interleukin-1beta and interleukin-6 and serum activities of alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, creatine kinase, and creatine kinase-MB. However, S. platensis restored normal levels of measured serum parameters, ameliorated MC-LR-induced oxidative damage, and normalized tissue antioxidant biomarkers. In conclusion, SP alleviated MC-induced organ toxicities by mitigating oxidative and nitrosative stress and lipid peroxidation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The blue-green algae (cyanobacteria) inhabit freshwater, brackish, marine, and terrestrial environments (Hitzfeld et al. 2000; Ward et al. 1998). Their toxins have deleterious effects on humans, animals, and plants (Carmichael 2001; Corbel et al. 2014; Wang et al. 2021). Microcystis aeruginosa (cyanobacteria) produce the most abundant cyanotoxin, microcystin (MC), into freshwater due to extensive anthropogenic eutrophication (Ahmad et al. 2014). MC tolerates high temperatures (up to 300°C), which increases its stability in the aquatic environment (Wannemacher 1989). The exposure of humans and animals to MC occurs through drinking water and eating contaminated vegetables and seafood (Hu et al. 2016; WHO 1998). MC-induced toxic effects have been reported in many countries including Saudi Arabia (Mohamed 2008), Egypt (Mohamed et al. 2003), Poland (Romanowska-Duda et al. 2002), China (Chen and Xie 2005), Japan (Yokoyama and Park 2002), and Brazil (Azevedo et al. 2002). They are considered a potent neuro- and hepatotoxin (Hu et al. 2016; Jiang et al. 2013) that can cause liver damage by inhibiting protein phosphates 1 and 2A (Humpage and Falconer 1999; Campos and Vasconcelos 2010). MC reaches the hepatocytes through the biliary system because of its high affinity to serine/threonine-containing enzyme phosphatases, which leads to disruption in signaling pathways and cytoskeleton integrity (Xu et al. 2013; Basha et al. 2008). Moreover, the prolonged exposure to MC damages the liver (Chen et al. 2009) and promotes carcinogenesis in humans (Xu et al., 2013). It has been implicated in promoting colon (Humpage et al. 2000) and liver tumors (Ito et al. 1997). MC induces its toxicities by inhibiting cellular antioxidant systems and reactive oxygen species (ROS) overproduction (Jiang et al. 2013; Wang et al. 2017). Biodegradation of MC includes physical, chemical, microbiological, and biotechnological methods. Alternative strategies to detoxify MC have become a global research interest (Massey et al. 2018). It has been indicated that reduced glutathione (GSH) plays indispensable roles in the detoxification of MC as it conjugates with MCS in the liver of mice, rats, and aquatic organisms forming MCLR-GSH conjugate (Pflugmacher et al. 1998; Gehringer et al. 2004; Li et al. 2015). Among various MCs, MC-LR is the most studied one (Li et al. 2021).
Spirulina platensis (SP) is a nutritionally enriched filamentous cyanobacterium with many biomedical applications (Khan et al. 2005; Abdel-Daim et al. 2013; Abdel-Daim et al. 2019a; Abdel-Daim et al. 2015). It contains free radical scavenging agents and naturally occurring antioxidants, including phenolic compounds, tocopherol, β-carotene, γ-linolenic acid, and phycocyanin (Khan et al. 2005). In addition, SP and its main constituent, C-phycocyanin, exhibit hepatoprotective, neuroprotective, anti-inflammatory, immunomodulatory, and anticancer action (Reddy et al. 2000; Romay et al. 2003; Khan et al. 2005). They have been reported to improve organ toxicities caused by heavy metals (El-Desoky et al. 2013; Simsek et al. 2009). SP received growing interest due to its safety, high bioavailability, and significant protection against organ toxicities induced by different chemicals and pollutants (Lu et al. 2010; Avdagic et al. 2008; Abdel-Daim et al. 2013; Abdel-Daim et al. 2019a; El-Desoky et al. 2013; Ibrahim and Abdel-Daim 2015).
Therefore, the current work aimed to evaluate SP protective, anti-inflammatory, and antioxidant effects against MC-induced multi-organ toxicities in rats, mainly by examining liver and kidney functions, proinflammatory cytokines, and oxidant/antioxidants status.
Materials and methods
Chemicals
Pure powder of Spirulina platensis was obtained from HerbaForce (UK) and MC-LR was obtained from Sigma-Aldrich (USA). Kits for oxidant/antioxidant marker determination and biochemical assay kits (urea, creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase (ALP) were obtained from Biodiagnostics Company (Egypt). Kits for LDH (lactate dehydrogenase) were purchased from Randox Lab. Ltd. (UK), while CK-MB (creatine kinase-MB) and CK (creatine kinase) were obtained from StanbioTM (USA). To assess the inflammatory response, kits for TNF-α (tumor necrosis factor-α) was obtained from BioSource Inter. Inc. (USA), while kits for determination of interleukin-6 (IL-6) and interleukin-1β (IL-1β) were purchased from Glory Science Co. Ltd. (USA).
Animals
Forty male Albino Wistar rats with an average weight of 170+20 g were obtained from the Egyptian Organization for Biological Products and Vaccines (VACSERA, Dokki, Giza, Egypt). Rats were accommodated for a week prior to commencement of the experiment under controlled conditions with moderate humidity (60+5%) and light/dark cycle (12:12L/D) and an average temperature of 25 ± 2 °C. Rats were fed ad libitum. The experiment was approved (No:2020089) by The Research Ethical Committee of the Faculty of Veterinary Medicine, Suez Canal University, Ismailia, Egypt. The international regulations were followed to care for laboratory animals to avoid animal suffering.
Experimental protocol
The forty rats were classified randomly into five experimental groups (GI—GV).
-
G-I (control): rats received distilled water for 21 days.
-
G-II (SP): rats received oral SP (1000 mg/kg BW/day) for 21 days (Abdel-Daim et al. 2013).
-
G-III (MC): rats received distilled water orally for 7 days before IP injection with MC-LR (10 μg/kg/day) for 14 days (Arman et al. 2019).
-
G-IV (MC-LR-SP-500) group: rats received SP (500 mg/kg/day), orally for 7 days, and then concurrently administrated with MC (10 μg/kg/day, IP) for the subsequent14 days.
-
G-V (MC-LR-SP1000) group: rats received SP (1000 mg/kg/day), orally for 7 days, and then concurrently administrated with MC (10 μg/kg/day, IP) for the subsequent14 days.
Collection of blood and tissue samples
Twenty-four hours following the last treatment, rats were anesthetized by isoflurane. Blood specimens were collected by cardiac puncture. The coagulated blood was centrifuged at 3000 rpm for 15 min; serum was collected in aliquots and preserved at −20°C for biochemical assays. Then rats were sacrificed by decapitation, and the heart, brain, liver, and kidney were immediately collected, scrubbed by physiological saline to be free from blood, and homogenized in 0.2M Tris-HCl buffer (ice-cold; pH7.4), and then centrifuged for 30min at (4°C) and 5000 rpm. The resultant supernatants were preserved at −80°C to measure tissue oxidative/antioxidant biomarkers in each tissue.
Biochemical analysis
The activities of and ALT were evaluated according to Reitman and Frankel (1957), while the activity of ALP was evaluated as reported by Tietz et al. (1983). Serum creatinine and urea levels were determined as stated in Larsen (1972 ) and Coulombe and Favreau (1963), respectively, while cardiac biomarkers, CK, CK-MB, and LDH, were estimated as reported by Szasz et al. (1979), Wurzburg et al. (1976), and Babson and Babson (1973), respectively.
Estimation of proinflammatory cytokines
The serum levels of pro-inflammatory markers, TNF-α, IL-1β, and IL-6, were estimated by ELISA kits as reported in manufacturer’s instructions. Using an automatic ELISA reader, the absorbance was determined at 420 nm.
Estimation of the liver, kidney, brain, and heart oxidant/antioxidant markers
The oxidant/antioxidant biomarkers’ levels were estimated in the homogenates of the liver, kidney, heart, and brain tissues. For nitrosative stress, nitric oxide (NO) concentrations were evaluated as reported by Green et al. (1982), and for lipid peroxidation, malondialdehyde (MDA) levels were determined as reported by Mihara and Uchiyama (1978). Further, reduced glutathione (GSH) was determined as reported by Beutler et al. (1963), and glutathione peroxidase (GSH-Px) was evaluated as reported by Paglia and Valentine (1967) in the tissue homogenates, while catalase (CAT) was determined as reported by Aebi (1984) and superoxide dismutase (SOD) was determined as stated in Nishikimi et al. (1972).
Data statistical analysis
For each group, data were presented as mean ± standard error (mean ± SE). Using SPSS (SPSS Inc., version 21.0, USA), the data were statistically analyzed. Homogeneity of variance was checked. The statistical significance was evaluated by applying one-way analysis of variance (ANOVA) followed by Tukey’s test under a probability of 0.05.
Results
Impact of SP treatment on serum biochemical parameters in MC-LR-intoxicated rats
MC-intoxicated rats exhibited a significant increase (P<0.05) in liver enzymes (ALT, 263.3%; AST, 232.5%; and ALP, 236.9%), renal biomarkers (urea 208.7% and creatinine 551.4%), and cardiac enzymes (CK 224.4% and CK-MB 310.9%; LDH 225.7%) compared with normal control rats, while MC-intoxicated rats treated with SP at doses of 500 and 1000 mg/kg were associated with significant improvements (P<0.05) in liver (AST, ALT, and ALP), kidney (urea and creatinine), and cardiac (LDH, CK, and CK-MB) level recording (66.1%, 68.4%, 60.6%, 65.0%, 42.2%, 67.5%, 67.3%, and 52.2% for SP500 mg/kg and 46.8%, 39.7%, 44.4%, 51.4%, 26.0%, 47.0%, 50.8%, and 37.1% for SP1000 mg/kg, respectively) when compared with MC-intoxicated rats (Table 1).
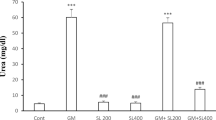
Impact of SP treatment on inflammatory reactions in MC-LR intoxicated rats
There is a significant increase (P<0.05) in serum level of inflammatory markers (TNF-α, IL-1β, and IL-6) in MC-treated rats compared with normal control rats recording (350.8%, 364.9%, and 363.9%, respectively) (Figure 1), while treatment of MC-intoxicated rats using SP at doses of 500 and 1000 mg/kg explained significant decrease (P<0.05) in serum TNF-α, IL-1β, and IL-6 concentration recording (44.5%, 48.0%, and 52.5% for SP 500 mg/kg and 67.5%, 32.7%, and 38.3% for SP1000 mg/kg, respectively) when compared with MC-intoxicated rats (Figure 1).
Protective effect of Spirulina platensis (SP) against microcystin (MC)-LR-induced changes in serum level of proinflammatory markers in intoxicated rats. A Interleukin-1β (IL-1β); B interleukin-6 (IL-6); C tumor necrosis factor-α (TNF-α). Data are presented as mean+SE values. Columns labeled with different letters are significantly different at P<0.05.
Effects of SP on oxidant/antioxidant biomarkers in MC-LR intoxicated rats
Liver
MC intoxication explained dramatic increase (P<0.05) in liver NO and MDA concentration recording (263.0% and 209.7%, respectively), and significantly decreased (P<0.05) in SOD (32.8%), CAT (44.3%), GSH (50.8%), and GSH-PX (41.5%) activities, when compared with normal control rats.
On the contrary, handling with SP at doses of 500 and 1000 mg/kg, liver NO and MDA level significantly reduced (P<0.05) recording (56.0% and 70.7% for SP 500 mg/kg group and 43.2% and 55.0% for SP1000 mg/kg group, respectively, when compared with MC-intoxicated rats), while treatment by SP explained significant increase (P<0.05) in antioxidant markers’ (GSH, GSHPX, SOD, and CAT) concentrations (for SP500 mg/kg group: 164.5%, 178.9%, 209.2%, and 174.5%, respectively; while for SP1000 mg/kg group: 206.5%, 235.7%, 279.9%, and 210.6%, respectively, compared with MC-intoxicated rats) (Figure 2). Therefore, SP protected liver tissue against the toxicity of MC and normalized the liver tissue levels of antioxidant biomarkers and oxidative stress.
Protective effect of Spirulina platensis (SP) against microcystin (MC)-LR-induced oxidative damage in liver of intoxicated rats. A Malondialdehyde (MDA); B nitric oxide concentration (NO); C reduced glutathione concentration (GSH); D glutathione peroxidase activity (GSH-Px); E superoxide dismutase activity (SOD); and F catalase activity (CAT). Data are presented as mean+SE values. Columns labeled with different letters are significantly different at (P<0.05)
Kidney
MC intoxication explained significant increase (P<0.05) in kidney NO and MDA concentrations (254.3% and 239.6%, respectively), and significantly decreased (P<0.05) in antioxidant (GSH, GSHPX, CAT, and SOD) activities (45.9%, 30.7%, 29.6%, and 54.4%, respectively), when compared with normal control rats.
On the contrary, treatment using SP at doses of 500 and 1000 mg/kg was associated with significant decrease in renal NO and MDA level (for SP 500 mg/kg group: 74.1% and 63.2%, respectively; for SP1000 mg/kg group: 43.5% and 44.5%, respectively compared with MC-intoxicated rats), while treatment with SP caused significant increase (P<0.05) in kidney antioxidant markers’ (GSH, GSHPX, CAT, and SOD) concentrations (for SP500 mg/kg group: 164.0%, 220.9%, 211.7%, and 131.2%, respectively; while for SP1000 mg/kg group: 212.0%, 316.0%, 318.3, and 174.3%, respectively compared with MC-intoxicated rats) (Figure 3). Therefore, SP protected the kidney tissue against the toxicity of MC and normalized the kidney tissue concentration of antioxidant biomarkers and oxidative stress.
Protective effect of Spirulina platensis (SP) against microcystin (MC)-LR-induced oxidative damage in kidney of intoxicated rats. A Malondialdehyde (MDA); B nitric oxide concentration (NO); C reduced glutathione concentration (GSH); D glutathione peroxidase activity (GSH-Px); E superoxide dismutase activity (SOD); and F catalase activity (CAT). Data are presented as mean+SE values. Columns labeled with different letters are significantly different at (P<0.05)
Brain
MC intoxication explained dramatic increase (P<0.05) in brain tissue NO and MDA concentrations (188.9% and 197.9%, respectively), but significantly decreased (P<0.05) in GSH (48.8%), GSH-PX (41.3%), CAT (42.7%), and SOD (51.8%) activities, when compared with normal control rats.
On the contrary, treatment by SP at doses of 500 and 1000 mg/kg significantly decreased brain tissue NO and MDA concentrations (P<0.05) (for SP 500 mg/kg group: 75.5% and 79.9%, respectively; for SP1000 mg/kg group: 53.8% and 59.9%, respectively, compared with MC-intoxicated rats), while recorded significant release (P<0.05) in antioxidant markers’ (GSH, GSHPX, CAT, and SOD) activities (for SP 500 mg/kg group: 176.8%, 139.3%, 148.57, and 145.6, respectively; for SP1000 mg/kg group: 203.9%, 210.1%, 228.9%, and 181.4, respectively, when compared with MC-intoxicated rats) (Figure 4). Therefore, SP protected the brain tissue against MC toxicity and normalized the levels of antioxidant biomarkers and oxidative stress.
Protective effect of Spirulina platensis (SP) against microcystin (MC)-LR-induced oxidative damage in brain of intoxicated rats. A Malondialdehyde (MDA); B nitric oxide concentration (NO); C reduced glutathione concentration (GSH); D glutathione peroxidase activity (GSH-Px); E superoxide dismutase activity (SOD); and F catalase activity (CAT). Data are presented as mean+SE values. Columns labeled with different letters are significantly different at (P<0.05)
Heart
MC intoxication explained significant increase (P<0.05) in heart tissue NO and MDA concentration recording (234.2% and 227% respectively), and significantly decreased (P<0.05) in heart tissue antioxidant (GSH, GSHPX, CAT, and SOD) activities (41.9%, 45.0%, 24.9%, and 41.9%, respectively) when compared with normal control rats.
On the contrary, treatment with SP at doses of 500 and 1000 mg/kg significantly decreased (P<0.05) cardiac tissue NO and MDA concentrations (for SP 500 mg/kg group: 59.8% and 63.8%, respectively; for SP1000 mg/kg group: 44.8% and 46.4%, respectively compared with MC-intoxicated rats). Moreover, significant increase (P<0.05) was recorded in cardiac tissue antioxidant markers’ (GSH, GSHPX, CAT, and SOD) activities (for SP500 mg/kg group: 168.9%, 158.4%, 200%, and 162.9%, respectively; for SP1000 mg/kg group: 218.6%, 214.0%, 377.0%, and 221.5%, respectively, compared with MC-intoxicated rats) (Figure 5). Therefore, SP protected the cardiac tissue against MC toxicity and normalized the cardiac tissue levels of antioxidant biomarkers and oxidative stress.
Protective effect of Spirulina platensis (SP) against microcystin (MC)-LR-induced oxidative damage in heart of intoxicated rats. A Malondialdehyde(MDA); B nitric oxide concentration (NO); C reduced glutathione concentration (GSH); D glutathione peroxidase activity (GSH-Px); E superoxide dismutase activity (SOD); and F catalase activity (CAT). Data are presented as mean+SE values. Columns labeled with different letters are significantly different at (P<0.05)
Discussion
Spirulina platensis (SP) is a food supplement microalga with high nutritional importance and a wide range of biomedical applications. It is rich in potent free radical scavenging agents including proteins, lipids, carbohydrates, essential amino acids, essential fatty acids, C-phycocyanin, β carotene, minerals, and vitamins. Besides the antioxidant activity, Spirulina and its active constituents induce neuroprotective, hepatoprotective, nephroprotective, cardioprotective, immunomodulatory, anti-inflammatory, analgesic, antiaging, and anticancer activities (Abdel-Daim et al. 2013; Abdel-Daim et al. 2019a; Abdel-Daim et al. 2015; Abdelkhalek et al. 2015).
This study estimated the preventive role of SP against MC-LR toxic effects on the liver, kidney, heart, and brain. MC-LR induced significant increases in serum values of ALT, AST, ALP, CPK, CK-MB, LDH, urea, creatinine, TNF-α, IL-1β, and IL-6, tissue NO and MDA, and significant reductions in tissue GSH, GSH-PX, CAT, and SOD indicated a dramatic MC-LR toxicity. These data were in consent with the former reports (Abdel-Daim et al. 2019b; Chen and Xie 2005; Jiang et al. 2013; Lone et al. 2017; Robinson et al. 1991). The liver cells represent the essential target of MC-LR intoxication (Campos and Vasconcelos 2010; Robinson et al. 1991). MC-LR affinity with hepatic serine/threonine-specific protein phosphatases induced MC-hepatotoxicity (Greer et al. 2018). This causes cellular dysfunction, leading to leakage of hepatic enzymes into the bloodstream (Robinson et al. 1991). Strong evidence suggests that oxidative stress is implicated in MC-LR-induced hepatotoxicity (Ahmad et al. 2014; Greer et al. 2018). Further, MC-LR acts as a tumor promoter in the liver and colon (Ito et al. 1997; Humpage et al. 2000).
Due to lipid peroxidation, the cell membrane integrity is lost and LDH has released increasing serum levels (Jovanović et al. 2010; Abdel-Daim et al. 2019b). Through the aerobic glycolysis (along the electron transport chain), there is a decrease in ATP production. The reaction shifts to anaerobic glycolysis increasing lactates and LDH (Lone et al. 2017; Jovanović et al. 2010). The MC possibly affects the electron transport chain (Campos and Vasconcelos 2010; Fischer et al. 2005). In addition to hepatotoxicity, nephrotoxicity, and cardiotoxicity, MC-LR can pass the blood-brain barrier inducing neurotoxicity through oxidative damage and phosphatase inhibition (Hu et al. 2016; Fischer et al. 2005).
Oxidative stress in the biological systems occurs through a sequence of events which include the excessive generation of reactive oxygen species (ROS) and NO, which are freed inside the mammalian body due to exposure to endogenous metabolic processes or exogenous drugs in our environment (Sun 1990). Free radicals cause many degenerative diseases like cardiac disease, cataracts, diabetes, cancer, ageing, and stroke (Yeung et al. 2019; Sies et al. 2017). Excessive ROS production overcomes the cellular antioxidant defense mechanisms, which has harmful effects on cellular macromolecules inducing lipid peroxidation, DNA damage, mitochondrial dysfunction, protein oxidation, and ATP reduction (Sies et al. 2017; Salzano et al. 2014). Hydroxyl radicals (•OH) attack the cellular membrane causing MDA production, which binds to other cell molecules increasing the damaging effect. Cellular antioxidants as GSH-PX, GSH, and CAT are required; due to the depletion of these antioxidants, large amount of •OH are formed from H2O2 as it shifts to Fenton’s reaction (Sies et al. 2017). In this study, the significant increase in NO and MDA concentrations with reduction of cellular antioxidants, GSH-Px, GSH, CAT, and SOD, in the liver, kidney, heart, and brain tissues suggested implication of oxidative stress in MC-LR-induced toxicity. MC evoked lipid peroxidation, reducing hepatocyte membrane efficiency and efflux of transaminases into blood stream (Abdel-Daim et al. 2019b; Campos and Vasconcelos 2010). MC accumulation in the liver forms hepatic GSH complex (MC-GSH) as a part of its detoxification process; this leads to GSH exhaustion that is necessary for GSH-PX recycling through hydrolysis of hydrogen peroxide to water (Nordberg and Arnér 2001; Greer et al. 2018).
The oxidative stress and excessive ROS production initiate the intracellular cascade signaling which enhances proinflammatory cytokines expression (Salzano et al. 2014). The current data revealed that MC-LR elevated serum TNF-α, IL-1β, and IL-6 levels because it might induce oxidative stress in the tissues of the liver, kidney, heart, and brain. These data highlighted that the inflammatory reaction might be due to oxidative damage, which was in line with previous findings (Ahmad et al. 2014; Lone et al. 2017). Interestingly, MC could contaminate many SP products, which cannot be ignored as many human beings consume SP on a regular basis as a food supplement (Jiang et al. 2008).
Spirulina platensis supplementation at doses of 500 and 1000 mg/kg significantly decreased the serum injury biomarkers, in addition, lipid peroxidation, as well as it protected liver, kidney, cardiac, and cerebral tissues. SP normalized the elevated activities of serum LDH, CK, and CK-MB and decreased the TIL-induced lipid peroxidation and oxidative stress in a dose-dependent manner (Ibrahim and Abdel-Daim 2015). SP decreases serum concentrations of ALT, AST, ALP, uric acid, urea, and creatinine in deltamethrin-treated animals. In addition, it reduces deltamethrin-induced lipid peroxidation and oxidative stress (Abdel-Daim et al. 2013). This is probably due to the inimical effect of SP that contrary to MC induced oxidative damage through improving SOD and CAT activities or by inhibition of NO and MDA besides scavenging of free radicals (the cellular free radicals’ scavengers and endogenous enzymatic antioxidant). The SP antioxidant and protective effects may be due to its richness with antioxidant active constituents, like β carotene, C-phycocyanin, proteins, lipids, essential fatty acids, essential amino acids, carbohydrates, minerals, and vitamins that are characterized by anti-inflammatory and potent antioxidant activities (Upasani and Balaraman 2003; Abdel-Daim et al. 2015; Abdelkhalek et al. 2015). Numerous studies explained the cardioprotective, hepatoprotective, and nephroprotective role of SP and its active ingredients in contrary to drugs, chemicals, and xenobiotics (Karadeniz et al. 2008; Ibrahim and Abdel-Daim 2015; Kuriakose and Kurup 2011). Moreover, feeding pregnant rats on SP improves the newborns brain damage (Gargouri et al. 2012).
Pre-treatment with SP markedly alleviated the heavy metals’ (cadmium, lead, and mercury) toxicities in rats and mice. SP protective effects is due to its antioxidant roles that are obvious by the decrease in NO and MDA concentration and the increase in GSH levels and SOD action in hepatic tissue (El-Desoky et al. 2013; Karadeniz et al. 2009; Simsek et al. 2009). Moreover, SP has hepatorenal-protective effects by reduction of the contents of NO, MDA, urea, and creatinine, while it increases GSH concentration and GSH-Px, SOD, and CAT activities that indicate the therapeutic effect of SP contrary to cyclosporine, gentamicin, and cisplatin-induced oxidative stress and nephrotoxicity (Lu et al. 2010; Avdagic et al. 2008; Mohan et al. 2006; Khan et al. 2006; Karadeniz et al. 2008; Abdel-Daim et al. 2019a). Antioxidant properties of SP protect against cerebral ischemia injury (Thaakur and Sravanthi 2010). Further, SP reduces lead-induced neurotoxicity in rats (Gargouri et al. 2012). Therefore, our results confirmed SP must play an essential role in avoiding and curing MC-induced cardiac, neurological, hepatic, and renal damage via its powerful antioxidant activities.
Conclusions
MC-LR intoxication caused a significant elevation in serum biomarkers, proinflammatory cytokines, and lipid peroxidation while it suppressed the activity of the antioxidant enzymes. On the other hand, SP could prevent all these changes and normalize all parameters, especially at high concentration doses via its antioxidant and anti-inflammatory activities, which counteract the oxidative stress and inflammatory cascade induced by MC-LR toxicity.
Availability of data and materials
All data are available from the corresponding author when required.
References
Abdel-Daim MM, Abuzead SM, Halawa SM (2013) Protective role of Spirulina platensis against acute deltamethrin-induced toxicity in rats. PloS one 8(9):e72991. https://doi.org/10.1371/journal.pone.0072991
Abdel-Daim MM, Ahmed A, Ijaz H, Abushouk AI, Ahmed H, Negida A, Aleya L, Bungau SG (2019a) Influence of Spirulina platensis and ascorbic acid on amikacin-induced nephrotoxicity in rabbits. Environmental science and pollution research 26(8):8080–8086. https://doi.org/10.1007/s11356-019-04249-4
Abdel-Daim MM, Farouk SM, Madkour FF, Azab SS (2015) Anti-inflammatory and immunomodulatory effects of Spirulina platensis in comparison to Dunaliella salina in acetic acid-induced rat experimental colitis. Immunopharmacol Immunotoxicol 37(2):126–139. https://doi.org/10.3109/08923973.2014.998368
Abdel-Daim MM, Sayed AA, Abdeen A, Aleya L, Ali D, Alkahtane AA, Alarifi S, Alkahtani S (2019b) Piperine enhances the antioxidant and anti-inflammatory activities of thymoquinone against microcystin-lr-induced hepatotoxicity and neurotoxicity in mice. Oxid Med Cell Longev 2019:1309175–1309110. https://doi.org/10.1155/2019/1309175
Abdelkhalek NKM, Ghazy EW, Abdel-Daim MM (2015) Pharmacodynamic interaction of Spirulina platensis and deltamethrin in freshwater fish Nile tilapia, Oreochromis niloticus: impact on lipid peroxidation and oxidative stress. Environmental Science and Pollution Research 22(4):3023–3031. https://doi.org/10.1007/s11356-014-3578-0
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Ahmad W, Emdadul Haque ATM, Jamshed F, Saad A, Al-Jasabi S (2014) Prevention of formation of toxic carbonyl and aldehyde compounds in BALB/C micehepatocytes caused by the toxicity of microcystin-LR using hydroxytyrosol extracted from Zizyphusspina-christi. Toxicological Sciences 6(3):68–73
Arman T, Lynch KD, Montonye ML, Goedken M, Clarke JD (2019) Sub-chronic microcystin-LR liver toxicity in preexisting diet-induced nonalcoholic steatohepatitis in rats. Toxins 11(7). https://doi.org/10.3390/toxins11070398
Avdagic N, Cosovic E, Nakas-Icindic E, Mornjakovic Z, Zaciragic A, Hadzovic-Dzuvo A (2008) Spirulina platensis protects against renal injury in rats with gentamicin-induced acute tubular necrosis. Bosnian journal of basic medical sciences 8(4):331–336. https://doi.org/10.17305/bjbms.2008.2892
Azevedo SM, Carmichael WW, Jochimsen EM, Rinehart KL, Lau S, Shaw GR, Eaglesham GK (2002) Human intoxication by microcystins during renal dialysis treatment in Caruaru-Brazil. Toxicology 181-182:441–446. https://doi.org/10.1016/s0300-483x(02)00491-2
Babson AL, Babson SR (1973) Kinetic colorimetric measurement of serum lactate dehydrogenase activity. Clinical Chemistry 19(7):766–769
Basha OM, Hafez RA, El-Ayouty YM, Mahrous KF, Bareedy MH, Salama AM (2008) C-Phycocyanin inhibits cell proliferation and may induce apoptosis in human HepG2 cells. Egypt J Immunol 15:161–167
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Campos A, Vasconcelos V (2010) Molecular mechanisms of microcystin toxicity in animal cells. International journal of molecular sciences 11(1):268–287. https://doi.org/10.3390/ijms11010268
Carmichael WW (2001) Assessment of Blue-Green Algal Toxins in Raw and Finished Drinking Water. Denver, AWWA Research Foundation and American Water Works Association
Chen J, Xie P (2005) Seasonal dynamics of the hepatotoxic microcystins in various organs of four freshwater bivalves from the large eutrophic lake Taihu of subtropical China and the risk to human consumption. Environmental toxicology 20(6):572–584. https://doi.org/10.1002/tox.20146
Chen J, Xie P, Li L, Xu J (2009) First identification of the hepatotoxic microcystins in the serum of a chronically exposed human population together with indication of hepatocellular damage. Toxicol Sci. 108(1):81–89
Corbel S, Mougin C, Bouaicha N (2014) Cyanobacterial toxins: modes of actions, fate in aquatic and soil ecosystems, phytotoxicity and bioaccumulation in agricultural crops. Chemosphere 96:1–15. https://doi.org/10.1016/j.chemosphere.2013.07.056
Coulombe JJ, Favreau L (1963) A new simple semimicro method for colorimetric determination of urea. Clin Chem 9:102–108
El-Desoky GE, Bashandy SA, Alhazza IM, Al-Othman ZA, Aboul-Soud MA, Yusuf K (2013) Improvement of mercuric chloride-induced testis injuries and sperm quality deteriorations by Spirulina platensis in rats. PloS one 8(3):e59177. https://doi.org/10.1371/journal.pone.0059177
Fischer WJ, Altheimer S, Cattori V, Meier PJ, Dietrich DR, Hagenbuch B (2005) Organic anion transporting polypeptides expressed in liver and brain mediate uptake of microcystin. Toxicology and applied pharmacology 203(3):257–263. https://doi.org/10.1016/j.taap.2004.08.012
Gargouri M, Ghorbel-Koubaa F, Bonenfant-Magne M, Magne C, Dauvergne X, Ksouri R, Krichen Y, Abdelly C, El Feki A (2012) Spirulina or dandelion-enriched diet of mothers alleviates lead-induced damages in brain and cerebellum of newborn rats. Food and chemical toxicology: an international journal published for the British Industrial Biological Research Association 50(7):2303–2310. https://doi.org/10.1016/j.fct.2012.04.003
Gehringer MM, Shephard EG, Downing TG, Wiegand C, NeilanBA (2004) An investigation into the detoxification of microcystin-LR by the glutathione pathway in Balb/c mice. IntJ Biochem Cell Biol 36:931–941
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS (1982) Analysis of nitrate, nitrite, and [15N] nitrate in biological fluids. Anal Biochem 126:131–138
Greer B, Meneely JP, Elliott CT (2018) Uptake and accumulation of microcystin-LR based on exposure through drinking water: an animal model assessing the human health risk. Scientific Reports 8(1):4913
Hitzfeld BC, Hoger SJ, Dietrich DR (2000) Cyanobacterial toxins: removal during drinking water treatment, and human risk assessment. Environmental health perspectives 108(Suppl 1):113–122. https://doi.org/10.1289/ehp.00108s1113
Hu Y, Chen J, Fan H, Xie P, He J (2016) A review of neurotoxicity of microcystins. Environmental science and pollution research 23(8):7211–7219. https://doi.org/10.1007/s11356-016-6073-y
Humpage AR, Falconer IR (1999) MCYST-LR and liver tumor promotion: effects on cytokinesis, ploidy, and apoptosis in cultured hepatocytes. Environ Toxicol 14:61–76
Humpage AR, Hardy SJ, Moore EJ, Froscio SM, Falconer IR (2000) Microcystins (cyanobacterial toxins) in drinking water enhance the growth of aberrant crypt foci in the mouse colon. Journal of toxicology and environmental health Part A 61(3):155–165. https://doi.org/10.1080/00984100050131305
Ibrahim AE, Abdel-Daim MM (2015) Modulating effects of Spirulina platensis against tilmicosin-induced cardiotoxicity in mice. Cell J 17(1):137–144. https://doi.org/10.22074/cellj.2015.520
Ito E, Kondo F, Terao K, Harada K (1997) Neoplastic nodular formation in mouse liver induced by repeated intraperitoneal injections of microcystin-LR. Toxicon: official journal of the International Society on Toxinology 35(9):1453–1457. https://doi.org/10.1016/s0041-0101(97)00026-3
Jiang J, Shan Z, Xu W, Wang X, Zhou J, Kong D, Xu J (2013) Microcystin-LR induced reactive oxygen species mediate cytoskeletal disruption and apoptosis of hepatocytes in Cyprinus carpio L. PloS one 8(12):e84768. https://doi.org/10.1371/journal.pone.0084768
Jiang Y, Xie P, Chen J, Liang G (2008) Detection of the hepatotoxic microcystins in 36 kinds of cyanobacteria Spirulina food products in China. Food additives & contaminants Part A, Chemistry, analysis, control, exposure & risk assessment 25(7):885–894. https://doi.org/10.1080/02652030701822045
Jovanović P, Žorić L, Stefanović I (2010) Lactate dehydrogenase and oxidative stress activity in primary open-angle glaucoma aqueous humour. Bosnian journal of basic medical sciences 10(1):83–88
Karadeniz A, Cemek M, Simsek N (2009) The effects of Panax ginseng and Spirulina platensis on hepatotoxicity induced by cadmium in rats. Ecotoxicology and environmental safety 72(1):231–235. https://doi.org/10.1016/j.ecoenv.2008.02.021
Karadeniz A, Yildirim A, Simsek N, Kalkan Y, Celebi F (2008) Spirulina platensis protects against gentamicin-induced nephrotoxicity in rats. Phytother Res 22(11):1506–1510. https://doi.org/10.1002/ptr.2522
Khan M, Shobha JC, Mohan IK, M.U. RN, Prayag A (2006) Spirulina attenuates cyclosporine-induced nephrotoxicity in rats. J Appl Toxicol 26:444–451
Khan Z, Bhadouria P, Bisen PS (2005) Nutritional and therapeutic potential of Spirulina. Current pharmaceutical biotechnology 6(5):373–379. https://doi.org/10.2174/138920105774370607
Kuriakose GC, Kurup MG (2011) Antioxidant and antihepatotoxic effect of Spirulina laxissima against carbon tetrachloride-induced hepatotoxicity in rats. Food Funct 2(3-4):190–196
Larsen K (1972) Creatinine assay in the presence of protein with LKB 8600 Reaction Rate Analyser. Clin Chim Acta 38:475–476
Lone Y, Bhide M, Koiri RK (2017) Amelioratory effect of coenzyme Q10 on potential human carcinogen Microcystin-LR induced toxicity in mice. Food and chemical toxicology: an international journal published for the British Industrial Biological Research Association 102:176–185. https://doi.org/10.1016/j.fct.2017.02.018
Li B, Liu Y, Zhang H, Liu Y, Liu Y, Xie P (2021) Research progress in the functionalization of microcystin-LR based on interdisciplinary technologies. Coord Chem Rev 443:214041. https://doi.org/10.1016/j.ccr.2021.214041
Li S, Chen J, Xie P, Guo X, Fan H, Yu D, Zeng C, Chen L (2015) The role of glutathione detoxification pathway in MCLR-induced hepatotoxicity in SD rats. Environ Toxicol. 30(12):1470–1480
Lu J, Ren DF, Wang JZ, Sanada H, Egashira Y (2010) Protection by dietary Spirulina platensis against D-galactosamine--and acetaminophen-induced liver injuries. The British journal of nutrition 103(11):1573–1576. https://doi.org/10.1017/S0007114509993758
Massey IY, Zhang X, Yang F (2018) Importance of bacterial biodegradation and detoxification processes of microcystins for environmental health. Journal of toxicology and environmental health Part B, Critical reviews 21(6-8):357–369. https://doi.org/10.1080/10937404.2018.1532701
Mihara M, Uchiyama M (1978) Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Analytical Biochemistry 86(1):271–278
Mohamed ZA (2008) Toxic cyanobacteria and cyanotoxins in public hot springs in Saudi Arabia. Toxicon: official journal of the International Society on Toxinology 51(1):17–27. https://doi.org/10.1016/j.toxicon.2007.07.007
Mohamed ZA, Carmichael WW, Hussein AA (2003) Estimation of microcystins in the freshwater fish Oreochromis niloticus in an Egyptian fish farm containing a Microcystis bloom. Environmental toxicology 18(2):137–141. https://doi.org/10.1002/tox.10111
Mohan IK, Khan M, Shobha JC, Naidu MU, Prayag A (2006) Protection against cisplatin-induced nephrotoxicity by Spirulina in rats. Cancer Chemother Pharmacol 58:802–808
Nishikimi M, Rao NA, Yagi K (1972) The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochemical and biophysical research communications 46(2):849–854
Nordberg J, Arnér ESJ (2001) Reactive oxygen species, antioxidants, and the mammalian thioredoxin system. Free Radical Biology and Medicine 31(11):1287–1312
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. The Journal of Laboratory and Clinical Medicine 70(1):158–169
Pflugmacher S, Wiegand C, Oberemm A, Beattie KA, Krause E, Codd GA, Steinberg CE (1998) Identification of an enzymatically formed glutathione conjugate of the cyanobacterial hepatotoxin microcystin-LR: the first step of detoxication. Biochim Biophys Acta 1425:527–533
Reddy CM, Bhat VB, Kiranmai G, Reddy MN, Reddanna P, Madyastha KM (2000) Selective inhibition of cyclooxygenase-2 by C-phycocyanin, a biliprotein from Spirulina platensis. Biochemical and biophysical research communications 277(3):599–603. https://doi.org/10.1006/bbrc.2000.3725
Reitman S, Frankel S (1957) A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. American Journal of Clinical Pathology 28(1):56–63
Robinson NA, Matson CF, Pace JG (1991) Association of microcystin-LR and its biotransformation product with a hepatic-cytosolic protein. Journal of biochemical toxicology 6(3):171–180. https://doi.org/10.1002/jbt.2570060303
Romanowska-Duda Z, Mankiewicz J, Tarczynska M, Walter Z, Zalewski M (2002) The effect of toxic cyanobacteria (blue-green algae) on water plants and animal cells. Polish Journal of Environmental Studies 11:561–566
Romay C, Gonzalez R, Ledon N, Remirez D, Rimbau V (2003) C-phycocyanin: a bili protein with antioxidant, anti-inflammatory and neuroprotective effects. Curr Protein Pept Sci 4(3):207–216
Salzano S, Checconi P, Hanschmann EM (2014) Linkage of inflammation and oxidative stress via release of glutathionylated peroxiredoxin-2, which acts as a danger signal. Proceedings of the National Academy of Sciences 111(33):12157–12162
Sies H, Berndt C, Jones DP (2017) Oxidative stress. Annual Review of Biochemistry 86(1):715–748
Simsek N, Karadeniz A, Kalkan Y, Keles ON, Unal B (2009) Spirulina platensis feeding inhibited the anemia- and leucopenia-induced lead and cadmium in rats. Journal of hazardous materials 164(2-3):1304–1309. https://doi.org/10.1016/j.jhazmat.2008.09.041
Sun Y (1990) Free radicals, antioxidant enzymes, and carcinogenesis. Free Radic Biol Med 8(6):583–599
Szasz G, Waldenstrom J, Gruber W (1979) Creatine kinase in serum: Inhibition by endogenous polyvalent cations, and effect of chelators on the activity and stability of some assay components. Clin Chem 25(3) (3):446-452.
Thaakur S, Sravanthi R (2010) Neuroprotective effect of Spirulina in cerebral ischemia-reperfusion injury in rats. Journal of neural transmission 117(9):1083–1091. https://doi.org/10.1007/s00702-010-0440-5
Tietz NW, Burtis CA, Duncan P, Ervin K, Petitclerc CJ (1983) A reference method for measurement of alkaline phosphatase activity in human serum. Clin Chem 29:751–761
Upasani CD, Balaraman R (2003) Protective effect of Spirulina on lead-induced deleterious changes in the lipid peroxidation and endogenous antioxidants in rats. Phytother Res 17(4):330–334
Wang K, Garg S, Waite TD (2017) Light-mediated reactive oxygen species generation and iron redox transformations in the presence of exudate from the cyanobacterium Microcystis aeruginosa. Environmental science & technology 51(15):8384–8395. https://doi.org/10.1021/acs.est.7b01441
Wang H, Xu C, Liu Y, Jeppesen E, Svenning J-C, Wu J, Zhang W, Zhou T, Wang P, Nangombe S, Ma J, Duan H, Fang J, Xie P (2021) From unusual suspect to serial killer: Cyanotoxins boosted by climate change may jeopardize megafauna. The Innovation 2(2):100092
Wannemacher RW (1989) Chemical stability and laboratory safety of naturally occurring toxins. Fort Detrick, Frederick, MD, US Army Medical Research Institute of Infectious Disease.
Ward DM, Ferris MJ, Nold SC, Bateson MM (1998) A natural view of microbial biodiversity within hot spring cyanobacterial mat communities. Microbiology and molecular biology reviews: MMBR 62(4):1353–1370
WHO (1998) Cyanobacterial toxins: microcystin-LR in drinking- water Environmental Health 2:1–14
Wurzburg U, Hennrich N, Lang H, Prellwitz W, Neumeier D, Knedel M (1976) Determination of creatine kinase-MB in serum using inhibiting antibodies. Klin Wochenschr 54(8):357–360
Xu P, Zhang XX, Miao C, Fu Z, Li Z, Zhang G, Zheng M, Liu Y, Yang L, Wang T (2013) Promotion of melanoma cell invasion and tumor metastasis by microcystin-LR via phosphatidylinositol 3-kinase/AKT pathway. Environmental science & technology 47(15):8801–8808. https://doi.org/10.1021/es4007228
Yeung AWK, Tzvetkov NT, El-Tawil OS, Bungǎu SG, Abdel-Daim MM, Atanasov AG (2019) Antioxidants: scientific literature landscape analysis. Oxidative Medicine and Cellular Longevity 2019:8278454–8278411. https://doi.org/10.1155/2019/8278454
Yokoyama A, Park HD (2002) Mechanism and prediction for contamination of freshwater bivalves (Unionidae) with the cyanobacterial toxin microcystin in hypereutrophic Lake Suwa, Japan. Environmental toxicology 17(5):424–433. https://doi.org/10.1002/tox.10075
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research at Jouf University for funding this work through research grant number (40/370).
Funding
This work is funded by the Deanship of Scientific Research at Jouf University through research grant number (40/370).
Author information
Authors and Affiliations
Contributions
Idea and design: M. O. G., M. M. A. F., M. M. A-D
Data collection: M. O. G., M. M. A. F., M. K., M. M. A-D
Data analysis: M. O. G., M. M. A. F., M. K., M. M. A-D
Funding: M. O. G., M. M. A. F., M. K., M. M. A-D
Investigation: M. O. G., M. M. A. F., M. K., M. M. A-D
Methodology: M. O. G., M. M. A. F., M. K., M. M. A-D
Project administration: M. O. G., M. M. A. F., M. M. A-D
Software: M. O. G., M. M. A. F., M. K., M. M. A-D
Supervision: M. O. G., M. M. A-D
Validation: M. O. G., M. M. A. F., M. K., M. M. A-D
Visualization: M. O. G., M. M. A. F., M. K., M. M. A-D
Manuscript draft writing: M. O. G., M. M. A. F., M. K., M. M. A-D
Manuscript revision and editing: M. O. G., M. M. A. F., M. K., M. M. A-D
All authors approved and confirmed this submission.
Corresponding author
Ethics declarations
Ethics approval
The Research Ethical Committee of the Faculty of Veterinary Medicine, Suez Canal University, Ismailia, Egypt, permitted the experimental scheme and animal management (the approval no 2020089). We took all the possible procedures to reduce rat sufferance.
Consent for publication
All authors approve this submission.
Consent to participate
Not applicable as the study did not includes human subject.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Germoush, .O., Fouda, M.M.A., Kamel, M. et al. Spirulina platensis protects against microcystin-LR-induced toxicity in rats. Environ Sci Pollut Res 29, 11320–11331 (2022). https://doi.org/10.1007/s11356-021-16481-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16481-y