Abstract
Heterotopic ossification (HO) is a pathological process characterized by the aberrant formation of bone in muscles and soft tissues. It is commonly triggered by traumatic brain injury, spinal cord injury, and burns. Despite a wide range of evidence underscoring the significance of neurogenic signals in proper bone remodeling, a clear understanding of HO induced by nerve injury remains rudimentary. Recent studies suggest that injury to the nervous system can activate various signaling pathways, such as TGF-β, leading to neurogenic HO through the release of neurotrophins. These pathophysiological changes lay a robust groundwork for the prevention and treatment of HO. In this review, we collected evidence to elucidate the mechanisms underlying the pathogenesis of HO related to nerve injury, aiming to enhance our understanding of how neurological repair processes can culminate in HO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
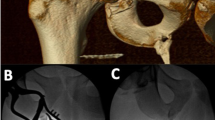
Heterotopic ossification (HO) is characterized by the abnormal formation of bone in soft tissues where bone typically does not form, which can be induced by multiple factors, and nerve injury is commonly considered the predominant factor [1,2,3]. Approximately 10% to 53% of HO patients suffer from postcentral nervous system injury [2]. Injuries to the spinal cord or peripheral nerves can also lead to HO [3, 4]. HO is most commonly observed in the hip joint in patients with spinal cord injury, but within patients with traumatic brain injury, HO may occur throughout the body such as in the shoulder and knee joints [2]. However, the structure and characteristics of HO induced by different forms of trauma exhibit significant similarities. The cellular origins of HO formation are relatively complex [5]. Cells involved in pathological ossification may originate from the osteogenic differentiation of various stem cells under specific stimuli [6]. The formation of cartilage occurs first followed by cartilage ossification in traumatic HO. In addition, some mesenchymal stem cells (MSCs) at the site of traumatic HO injury accompanied by nerve damage can also affect cartilage ossification and the differentiation into osteoblasts.
Both HO and the nervous system have been shown to play significant roles in bone development and growth [7,8,9]. The surface of the periosteal bone is covered by primary sensory and sympathetic nerve axons [5]. The mechanism driving HO is intricate and not entirely elucidated. At the injury site, sensory neurons receive and convey local information to the brain. This results in the brain sending neuroendocrine signals to the hypothalamus, initiating repair [9]. Various neural factors have been identified as key players in bone formation, such as nerve growth factor (NGF) [10] brain-derived neurotrophic factor (BDNF) [11] and neurotrophic factor (NT) [12, 13]. These neurotrophins and their receptors are diffusely expressed within the skeletal tissue promoting bone formation [14]. Localization of neurotransmitter receptors in the skeletal microenvironment plays a crucial role within the bone metabolism. These neurotrophins can signal through tyrosine kinase receptor (TrKs) and neurotrophins receptor (p75NTR) to regulate downstream signaling pathways contributing to the formation of HO [15].
The cerebrospinal fluid of patients with brain injuries exhibits osteogenic induction properties. The site of brain injury can promote the release of osteogenic inducers and neurotrophins [16]. These neurotrophins are extensively involved in neural development. Neurotrophins play a crucial role in promoting the development and survival of sensory and sympathetic neurons, as well as in regulating the differentiation of neural precursors [17]. In addition, neurotrophins can promote the formation of granulocytes and monocytes, reduce cardiomyocyte apoptosis, regulate blood glucose levels, induce the differentiation of bone marrow mesenchymal stromal cells (BMSCs), enhance memory and contribute to the treatment of Parkinson’s disease [18].
While the exact methods by which these nervous factors stimulate HO remain enigmatic, it is evident that some nerve fibers located near skeletal cells release neurotransmitters and neuropeptides. It has demonstrated that abundant neurite-like protrusions are in contact with the trabecular bone and nearby blood vessels through electron microscopy [19]. Neural fibers observed in the callus formed post-fracture can interact with osteoblasts and its precursors [7]. This interaction regulates bone metabolism through the secretion of neuropeptides and neurotrophic factors. These proteins regulate bone metabolism via multiple signaling pathways. The differentiation of MSCs is steered by both the transforming growth factor-beta (TGF-β) and bone morphogenic protein (BMP) pathways, which are integral to skeletal development and bone formation [20]. Notably, the BMP pathway is vital for regular bone formation and is also implicated in HO development [21,22,23]. Specific inflammatory factors such as TNF-α have also been identified as contributors to HO except the TGF-β pathway [1, 20, 24].
Given this complexity, understanding the pathogenesis of HO in relation to the nervous system becomes paramount. This review aims to synthesize current knowledge on how the nervous system fosters bone formation and endochondral ossification. It will further explore the roles of neural factors and TGF-β in HO development.
Nerve Injury and HO
HO arises following nerve injury and represents a complex dysfunction rooted in bone formation and remodeling [25]. In vitro research shows that cerebrospinal fluid from patients can stimulate bone growth after nerve injuries [16]. Serum obtained shortly after traumatic brain injury (TBI) contains humoral factors that encourage osteoblast differentiation within skeletal muscles and enhance the growth of skeletal muscle mesenchymal cells, both pivotal in advancing ossification and HO [26, 27]. In a model of polytrauma involving TBI and fracture, it was observed that TBI can alter the local neuroinflammatory state during the fracture healing process, stimulating endochondral ossification and early fracture healing in the contralateral limb [28]. Interestingly, serum from TBI model mice intensifies the proliferation and differentiation of pericytes, exacerbating endochondral bone formation within this model [29]. Neuroendocrine modulation advances bone formation post TBI, and TBI patients exhibit expedited fracture healing [30].
Patients with combined trauma and nerve injury face a substantially higher HO risk than those without combined trauma [31]. Nerve injuries can compromise the blood–brain barrier, prompting the release of cytokines that promote osteogenic factors in the bloodstream [31, 32]. BMPs, part of the transforming growth factor family, which are crucial in endochondral osteogenesis and fracture healing, are often employed to induce HO in vivo [25, 33]. Utilizing bone morphogenetic protein-2 (BMP-2) in spine fusion surgeries has been linked with possible complications of HO [34]. Postbrain injury, elevated BMP gene and protein expression levels have been reported [27].
Evidence has shown enhanced fracture callus formation in TBI patients [35,36,37,38]. Osteoinductive factors are released in areas where HO is induced by brain damage [16]. Slc33a1wt/mut mice in dorsal root ganglion cultures and sciatic nerve crush injury models have demonstrated injury-induced axonal regeneration through heightened BMP signaling [39]. There is a notable increase in the downstream BMP signaling pathway components pSmad1/5/8 and Bmpr1a, as well as in the number of myelinated axons within cortical neurons of mice. Conversely, injuries from BMP signaling could be mitigated with therapeutic Noggin, a BMP signaling antagonist [39]. Both BMP-2 and neurotrauma induce the growth of nerve-derived adult pluripotent cells (NEDAPS) to facilitate bone formation [40, 41]. Neural injury-induced HO in mouse models has shown effective BMP-2 suppression using pyrophosphate [41]. BMP-2 directly influences sensory neurons, initiating a neurogenic inflammatory response, which promotes nervous system remodeling and osteogenic stem cell release, culminating in bone formation [3, 42].
Chemically modified mRNA encoding BMP-2, when optimally delivered to osteotomies in rat femurs, aids in bone defect healing [43]. Increased BMP expression might enhance HO occurrence in rat tendons [44]. Overexpressing BMP-2 in the Tie2 + lineage produces HO in mice, linking abnormal BMP-2 signaling to skeletal muscle fiber injuries and increased Tie2 + lineage fibro-adipogenic precursor cells [45]. Around bone injury sites, BMPs may extend into surrounding muscle tissue, potentially inducing HO [46, 47]. Tfr2 deletion in osteoblasts attenuates the BMP-MAPK signaling pathway, inhibiting HO formation in mice [48]. Despite the involvement of the central nervous system in BMP signaling, the role of BMP in synapse formation in neurons has been proposed [49]. Additionally, BMP-2 appears to stimulate human peripheral neurogenic pluripotent cell differentiation into fibroblasts [50]. Targeting fibrinogen or the BMP signaling pathway might aid central nervous system repair [51]. Regarding bone repair, neurotrophin-3 (NT-3) might act as an osteogenic factor preceding BMP-2, inducing BMP-2 mRNA expression in injured growth plates [52]. Peripheral nerve progenitors can differentiate into osteoblasts and chondrocytes, leading to HO [4]. Trauma-induced neuroinflammation induces early osteogenic differentiation in endoneurial cells and activates HO-essential factors [53]. Osteoblast-specific transcription factors in endoneurial cells advance HO as blood enters the new bone formation site [8].
Studies suggest that inflammatory factors are released, such as TBI. These factors, combined with neural elements, accumulate within the nervous system. They then traverse the blood–brain barrier, entering peripheral circulation, which subsequently drives HO formation [26, 27, 29]. Moreover, trauma-induced HO predominantly unfolds via endochondral ossification [5, 54, 55]. Recent findings emphasize the critical role of osteogenic progenitors residing within the endoneurium, positing them as the chief osteogenic precursors in HO development [8]. Importantly, the regulation of endochondral ossification is deeply influenced by both the BMP pathway and inflammatory mediators. These agents synergistically activate osteogenic progenitors, bolstering the onset of HO [23, 56]. Tendon and muscle-resident interstitial cells also activate chondrocytes and osteoblasts within HO [56].
Furthermore, osteoporosis is another bone metabolic disorder following central nervous system trauma. Patients with TBI may experience an increased risk of bone loss and osteoporosis [57]. Following injury to the central nervous system, there is an increase in sympathetic outflow which activates bone resorption [58]. TBI significantly reduces the bone density of cortical bone with in the mouse model [59]. TBI can disrupt the function of the hypothalamic–pituitary–adrenal axis leading to a deficiency in pituitary-secreted growth hormone, which in turn induces catabolic effects resulting in decreased bone mass and bone density [60]. Furthermore, TBI has been also associated with vitamin D deficiency which is able to lead to osteoporosis [61]. Osteoprotegerin (OPG) plays a crucial role in the negative regulation of osteoclast-mediated bone resorption. The inhibition of stimulated osteoclast formation by OPG can lead to an increase in the volume of ectopic bone [62]. The insertion of metallic particles targeting osteoclasts to stimulate bone resorption around ectopic bone may represent a novel therapeutic strategy for HO [63].
In the context of HO formation following the neurological injury, a multitude of endocrine hormones and paracrine mechanisms are intricately involved in the regulation of bone metabolism. HO induced by spinal cord injury is more common in patients with hyperparathyroidism [64]. Parathyroid hormone (PTH) can stimulate the formation of trabecular bone and participate in bone remodeling, enhancing osteoblast activity and promoting the production of ALP [65, 66]. Parathyroid hormone-related protein (PTHrP) is essential for the production of trabecular bone mass and cortical bone [67]. PTHrP, originating from osteocytes, is transported through the network of lacunar-canalicular. It influences nearby osteoblasts via the PTHR1/cAMP signaling pathway to stimulate bone formation and regulate the expression of genes related to matrix mineralization [68]. PTHrP enhances the production of ephrinB2 and ephrinB2 signaling regulates osteoblast differentiation and the expression of osteoblast genes through a paracrine mechanism within the osteoblast lineage [69]. A reduction in osteocalcin (OCN) can enhance bone formation in mice model [70]. Lower levels of osteocalcin may play a significant role in the development of HO in patients with nerve injuries [71]. Insulin can inhibit BMP2-induced HO in muscle by suppressing the expression of Osterix [46]. Leptin is involved in functional recovery following the neural injury [72]. Leptin participates in the formation of HO by promoting the mineralization of the extracellular matrix and regulating osteoblast function [73]. The expression of SOX9 is reduced and results in the suppression of trauma-induced HO within the leptin-deficient diabetic mice [74]. Fibroblast growth factor receptor 3 (FGFR3) is closely associated with the signaling pathways formation and cartilage development involved in HO [75, 76]. FGFR3 is highly expressed in chondrocytes and osteoblasts and the FGFR3 signaling pathway influences the formation of trabecular bone through a paracrine mechanism [77].
Neural Factors Regulate Bone Formation
Neurotrophic factors, including NGF, BDNF, and NT, play crucial roles in maintaining the functionality of the neural system and promoting neuronal survival and maturation [78,79,80,81]. In response to inflammatory stimuli, mast cells and macrophages coordinate the production of these neurotrophic factors [82,83,84]. Notably, the majority of bone-forming cells show localization of NGF. Additionally, BDNF is present in osteoblast-like cells, and NT-3 is identified in both osteoblast-like cells and hypertrophic chondrocytes within the fracture callus [15].
These neurotrophins activate the p75NTR and TrKs thereby promoting bone formation [83, 85]. Studies have revealed that p75NTR aids in the differentiation of ectomesenchymal stem cells into osteoblasts [12]. After bone injury, there is a significant upregulation of p75NTR expression. This receptor not only influences bone repair but is also vital for stromal cell migration and subsequent bone regeneration [86]. Activation of p75NTR enhances the proliferation of MSCs, boosts neurological recovery, and activates glial cells [13].
In fracture models, NGF stimulates osteoblast maturation, increases innervation, and speeds up bone repair. Moreover, local administration of NGF accelerates callus maturation [87]. NGF-responsive TrkA-expressing nerves have been linked to enhanced cartilage antigen expression and increased TGF-β signaling at injury sites, leading to HO. NGF and TrkA are expressed within the process of endochondral fracture repair, and local injection of recombinant human β-NGF (β-NGF) within the cartilage promotes the expression of genes associated with endochondral ossification, such as Ihh and Alpl [88]. Consequently, inhibiting NGF signaling could prevent HO [89]. NGF distribution is notably dense at the subchondral bone or articular cartilage interface, with both p75NTR and TrkA being expressed in bone and articular cartilage [44]. Relatedly, MSC treatment has been shown to reduce apoptosis of oligodendrocytes caused by p75NTR [90].
Skeletal neurons release NGF, which promotes bone growth by stimulating the proliferation and differentiation of BMSCs [91]. After rib fractures in male rats, applying NGF to the fracture site significantly increased bone tissue, leading to a higher cartilage proportion [92]. Post bone injury, there is a significant rise in nerve fibers in bone tissue. Dendrites shift within the periosteum, and there is an increase in NGF and TrkA expression [93,94,95].
In mice, the NGF and TrkA signaling pathways in sensory nerves enhance bone formation in response to mechanical stresses [96]. This signaling pathway also stimulates the mineralization process in human chondrocytes [97]. One study found that following skull injury, macrophage-derived NGF levels rose, promoting sensory axon growth and skull regeneration. However, inhibiting TrkA activity delayed nerve growth and skull repair [98]. TrkA improves the survival and regenerative abilities of BMSCs by amplifying the Erk/Bcl-2 pathway [99]. There is also evidence suggesting that NGF inhibition can reduce bone destruction caused by tumors [100]. Interestingly, NGF has been found to activate the NF-κB signaling pathway by binding to p75NTR [101]. The role of NF-κB in bone metabolism and bone formation is well documented [102,103,104] and its activation is a key mechanism in the development of HO [105]. Inhibition of the NF-κB signaling pathway can suppress the function and differentiation of osteoclasts, effectively ameliorating bone loss in OVX mice model [104]. NF-κB signaling pathway is involved in the regulation of growth plate cartilage formation and osteoblasts, there is an increase in osteoblast differentiation and BMP-2 activation when the NF-κB signaling pathway is blocked.
NGF may alleviate neuropathic pain by inhibiting TAK1, subsequently suppressing the downstream MAPK and NF-κB signaling pathways. However, it remains uncertain whether this pathway influences HO [106]. In addition, astrocytes can activate the NF-κB pathway, and both TGF-β1 and β-NGF have been noted to upregulate this pathway [107, 108]. BDNF has been shown to promote osteogenesis and HO in BMSCs via the Erk/Runx2 pathway while also enhancing neurogenesis [8, 37]. BDNF stimulates the proliferation and differentiation of mesenchymal stem cells into osteoblasts [109, 110]. Furthermore, BDNF exhibits a high affinity for TrkB [15] and promotes neuronal cell survival through its interaction with TrkB [111].
BDNF and TrkB are present at different stages of bone formation [112]. The BDNF/TrkB signaling activates Akt stimulating the expression of ALP and BMP-2 [113]. TrkB is abundantly expressed in osteoblasts [94]. BDNF can suppress the differentiation of RAW264.7 cells into osteoclasts, and TrkB inhibition further hampers osteoblast proliferation [114]. K252a, BDNF receptor Trk inhibitor, significantly inhibits the formation of peripheral blood mononuclear cells induced osteoclasts stimulated by BDNF [115]. Through the TrkB-Erk1/2 signaling pathway, BDNF modulates the balance of RANKL/OPG expression in osteoblasts. BDNF depletion markedly reinstates RANKL/OPG homeostasis, curbing osteolytic bone destruction [116]. The molecule 7,8-dihydroxyflavone, a BDNF and TrkB agonist mimic, can inhibit BDNF/TrkB signaling, thereby thwarting RANKL-induced osteoclastogenesis and preventing bone loss [112].
Glial cell line-derived neurotrophic factor (GDNF) elevates Nr4a1 expression in BMSCs and activates the PI3K/Akt signaling pathway, enhancing the proliferation and osteogenic differentiation of BMSCs after promoting the presence of activated astrocytes and GDNF in the hippocampus [117]. This factor also fosters the migration and osteogenic differentiation of MSCs94. The neurological system has an abundance of RET receptors. GDNF synthesis in neurons, in tandem with RET receptors, activates the MAPK, Erk, and Akt pathways—all pivotal in bone formation [118,119,120,121].
NT-3 augments the expression of Sox9 and Runx2 by activating the endothelial‐mesenchymal transition. TrkC-specific inhibitors can alleviate NT-3-induced HO formation [52, 122]. Activated macrophages regulate NT-3 secretion, which, in turn, hastens HO through the Erk signaling pathway [123]. NGF-β, GDNF, and NT-3 can drive the differentiation of BMSCs into neurons [124, 125].
In summary, neurotrophic factors can signal through both the Trks and the p75NTR [15]. In addition to promoting survival and differentiation, neurotrophic factors also function through interactions with other receptors and ion channels. Neurotrophic factors can selectively bind with specific Trks. Trks function by regulating the Erk and PI3K signaling pathways. On the other hand, p75NTR can activate NF-κB and Jun N-terminal kinase (JNK).
Furthermore, BMP-2 has been revealed to enhance the interaction between peripheral nerves and bone, ensuring bone health in synergy with neurotrophin [14]. Engineered sensory nerves releasing NGF significantly stimulate the osteogenic differentiation of BMSCs via the NGF-TrkA pathway. Simultaneously, NGF may also foster bone healing through BMP-2 [126]. BDNF can boost BMP-2 gene synthesis, presenting therapeutic possibilities for treating periodontal defects [127, 128]. BDNF also promotes the expression of ALP, type I collagen as well as OCN, which play a significant role in bone formation [127]. NT-3 has been found to considerably raise BMP-2 and TGF-β levels, thereby hastening bone formation following tibial fractures in rats [128].
Glutamate, the primary neurotransmitter within the central nervous system, experiences an increase in release following neural injury [129]. The glutamate receptor N-methyl-D-aspartate receptor (NMDAR) which is associated with signal transduction in the central nervous system, is highly expressed in osteoblasts and osteoclasts [130]. Intense staining of NMDAR has been observed on osteoblasts and osteoclasts in human osteophyte tissues. Inhibition of NMDAR can suppress bone resorption and the activation of the NF-κB signaling pathway [131]. NMDAR inhibitors have been shown to suppress the expression of bone formation markers such as OCN, type I collagen, as well as ALP [132]. Furthermore, the activation of NMDAR can promote the production of bone remodeling markers mediated by parathyroid hormone [133]. Sympathetic Nervous System modulates bone remodeling through the signaling of beta-2 adrenergic receptor (B2AR) located on osteoblasts [134]. A specific inhibition and deficiency of B2AR in osteoblasts results in a reduction of bone resorption and an increase within the bone density [135, 136].
TGF-β and HO
TGF-β is integral for tissue homeostasis, directing various cellular activities, including proliferation, differentiation, apoptosis, and migration [137,138,139]. It orchestrates a vast range of biological processes, activating both non-Smad and Smad pathways, with the intricate involvement of upstream and downstream signaling molecules [140, 141]. Additionally, TGF-β is crucial in modulating HO and bone organogenesis [142].
Traumatized human tissue samples show pronounced increases in markers associated with bone growth. Notably, TGF-β expression, a marker for tissue fibrosis, escalates in injured tissues, subsequently leading to HO [143]. During bone remodeling, TGF-β regulates the recruitment of MSCs, ensuring bone homeostasis [144]. It also fosters the early differentiation of osteogenic progenitor cells and stimulates chondrocyte proliferation [145]. The resorption activity of osteoclasts can also activate TGF-β thereby inducing the progression of HO in patients with ankylosing spondylitis [146].
Neurologically, TGF-β expression intensifies in areas of nerve injury, helping to mitigate neuroinflammation [147, 148]. The TGF-β family has a seminal role throughout neurodevelopment, with profound clinical relevance to both injured and pathological nervous systems [149, 150]. Elevated expression of TGF-β1 and TGF-β has been noted in humans with posttraumatic spinal cord injuries [151,152,153]. Similarly, TGF-β is markedly expressed at injury sites after peripheral nerve damage [154, 155]. When introduced after chronic nerve injuries, TGF-β bolsters axonal regeneration [156]. Post spinal cord injuries in rats manifest as a significant upsurge in Ephrin type-B receptor 2 expression, accompanied by enhanced TGF-β1 secretion from activated astrocytes [157]. Mouse glial cells also exhibit increased TGF-β expression following trauma [158, 159]. Notably, the circular RNA Plek has been observed to amplify TGF-β1 after spinal cord injuries [160].
On a molecular level, TGF-β activates intracellular Smad signaling, a pathway influenced by a diverse set of factors and routes. Moreover, TGF-β collaborates with various pathways, such as MAPK, Wnt, Notch, and Akt/mTOR, all of which are pivotal for bone metabolism [161, 162]. WNT/β-catenin, acting as a mediator of the TGF-β/BMP signaling pathway, can regulate the differentiation of progenitor cells into osteoblasts and inhibit the apoptosis of osteoblast [161]. Smad serves as a platform for integrating MAPK/RTK signals with the TGF-β/BMP pathway. Ser203, Thr178 and Ser207 residues in the Smad3 linker region serve as phosphorylation sites for Erk1/2. TGF-β activating kinase and TAK binding protein activate MAPK through BMPR [163]. The MAPKs/TAK1 signaling pathway plays a role in the differentiation of MSCs and bone formation [161]. BMP2 can regulate MAPKs and activate the PI3K pathway [164]. The Notch pathway is active in the early stages of osteoblast differentiation, and disruption of Notch signaling genes leads to reduced osteogenesis and bone mass [165]. The subchondral bone microenvironment undergoes changes due to high levels of active TGF-β protein, leading to an accumulation of osteoprogenitor cells and an influx of new blood vessels [166, 167]. Additionally, mutations in the TGF-β1 gene locus in Camurati–Engelmann disease have been associated with long bone diaphysis hyperostosis and sclerosis, while TGF-β signaling anomalies can result in aneurysmal osteoarthritis syndrome [137].
Osteoclasts have been shown to resorb TGF-β in bone marrow, inducing HO [146]. Matrine can inhibit HO by obstructing the migration and osteogenic differentiation of MSCs induced by TGF-β in mice [168]. Additionally, MSCs can secrete TGF-β, modulating synaptic transmission and neuronal excitability in dorsal root ganglia [169]. When activated, TGF-β stimulates the formation of cortical bone [170, 171] emphasizing its pivotal role in managing HO and aberrant formation of subchondral bone [172, 173].
Therapeutic strategies for HO may be based on the suppression of the TGF-β signaling pathway [171, 174] which has been implicated as a crucial stimulator of human cartilage production [175]. TGF-β exerts a divergent effect on MSCs, inhibiting their osteogenic differentiation [176] while mitigating neural damage when administered in mice [177].
NGF significantly enhances the production of TGF-β1 and the expression of P75NTR, known for its pronounced stimulatory effect on the amniotic membrane [178, 179]. Moreover, the mRNA level of NGF in chondrocytes is upregulated by TGF-β via the ALK5-Smad2/3 signaling pathway [180, 181]. The role of TGF-β is highlighted during osteoarthritis progression, recruiting MSCs to stimulate bone formation within the subchondral bone marrow [167]. It also fosters axonal regeneration after nerve injuries, increasing the mRNA concentration of TGF-β1 within the distal nerve stump and enhancing NGF mRNA levels in rats and mice [155, 182,183,184,185].
The TGF-β signaling pathway, modulated by sensory nerves, facilitates cranial suture closure upon NGF binding to TrkA and serves as an autocrine factor on cells via TGF-β receptor (TβR) activation, stimulating the release of NGF [186, 187]. The absence of NGF and the inhibition of its receptor TrkA both suppress chondrocyte differentiation and the progression of HO [10]. Cellular domains rich in NGF promote the development of TrkA + sensory nerve fibers and the interruption of TrkA signal transduction inhibits the fracture healing [188]. Blocking NGF helps to alleviate bone destruction in mice model of bone tumors [100]. Inhibition of TGF-β1-induced Smad2/3 pathway activation decreases NGF expression [189]. Marine compounds have been identified to prevent HO by inhibiting the migration and osteogenic differentiation of MSCs via the TGF-β/Smad2/3 pathway [168]. TGF-β also promotes the expression of NGF in chondrocytes via the Smad2/3 signaling pathway [180]. TGF-β activates two Smad signals leading to an increase in the levels of NGF within the pancreatic stellate cells [190]. TGF-β1 can enhance the survival of Dorsal Root Ganglia (DRGs) mediated by NGF [185].
TGF-β signaling protects damaged neurons during the early stages of TBI through Smad3 activation and is essential for cell motility, enhancing serum expression and secretion levels of TGF-β1 [191, 192]. This cytokine enhances the expression of GDNF via TβR, protecting spinal sympathetic neurons from apoptosis [193,194,195,196]. TGF-β exerts a potent trophic effect on midbrain dopaminergic neurons, and the signal transduction of classical neurotrophic factors may be influenced by TGF-β [196]. The combination of TGF-β with NT-3 and NT-4 promotes the survival of more neurons and the neurotrophic function of GDNF requires the involvement of TGF-β. It is ubiquitously distributed in mature mouse bone marrow and is expressed extensively within cartilage [195].
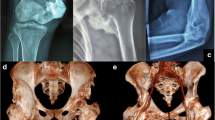
Research shows the prevalent presence of TGF-β signaling pathways within sensory nerves [197] and in astrocytes, it not only enhances protein expression but also modulates its own signaling pathway [198, 199]. Systemic injection of a TGF-β neutralizing antibody attenuates HO in BMP-induced spontaneous HO models in mice [24]. With intact BMP receptors, MSCs serve as BMP target cells in bone, with BMP being an effective inducer of osteoblast differentiation in vitro [22]. The TGF-β signaling pathway in astrocytes can inhibit inflammation and alleviate neuronal injury within the central nervous system [200] (Fig. 1).
Role of neuromodulation in HO after nerve injury. Blood levels of BMPs and TGF-β rise in response to damage to brain or nerve fibers, and these molecules directly influence intracellular signaling pathways to contribute to HO. Mast cells, macrophages and astrocytes are activated and accompanied by the release of neurotrophic factors following nerve injury. These neurotrophic factors in conjunction with BMPs and TGF-β combine with its corresponding receptor respectively and activate the signaling pathways to promote the progression of HO
Other Factors Inducing HO
Inflammation serves as a pivotal inducer of HO. Neuroinflammatory cascade is activated following the neural injury [201]. This process leads to the migration of chondro-osseous progenitor cells. TBI triggers a series of complex inflammatory responses activating the NF-KB, JNK and TAK1 signaling pathway, which is closely related to bone metabolism [202, 203]. Sensory neurons release neuroinflammatory molecules leading to the recruitment of hypertrophic cells [3]. The involvement of inflammatory responses, mediated by macrophages and mast cells, is observed in the development of HO subsequent to nerve injury [204, 205]. Macrophages are integral in promoting HO, facilitating the inflammatory response, and expressing cytokines such as TGF-β1, BMP, and Substance P (SP), which encourage the differentiation of MSCs [206]. There is a recognized association between HO, abnormal chondroprogenitor differentiation, and TGF-β1-producing monocytes or macrophages [207, 208]. However, TNF-α secreted by M1 macrophages has been implicated in the bone erosion associated with rheumatoid arthritis [209]. In the mouse model of HO induced by BMP or injury, the depletion of monocytes can promote the differentiation of endothelial cells into endochondral formation, ultimately leading to HO and an increase in bone density [207]. In addition, BMP-2 also plays a directly role in sensory neurons inducing neurogenic inflammation and resulting in the activation of osteoblasts [3]. TGF-β1 are closely associated with HO and abnormal differentiation of cartilage progenitor cells after musculoskeletal trauma [208].
Oncostatin M, produced by activated macrophages, stimulates osteogenic differentiation and mineralization of myocytes in individuals with spinal cord or brain damage, contributing to HO development [206, 210]. Following nerve injury, an upregulation of SP is observed, which is released by diverse cell types in the nervous system, including macrophages, neurons, and dendritic cells [211]. This molecule interacts with neurokinin receptors, playing a role in the differentiation of chondrocytes and osteoblasts.
The established interplay between inflammation and oxidative stress under various pathological conditions is a critical aspect of disease progression. During the formation of HO, there is a notable dysregulation in the redox process. Macrophages exhibit antioxidant properties through nuclear factor E2–related factor 2 (Nrf2) aiding in the formation of chondrocytes [212]. Inhibition of Nrf2 can significantly alleviate HO. Nrf2 positive chondrocytes can prevent hypoxia, thereby facilitating the development of HO [213]. NGF/TrkA promotes the vitality of BMSCs under hypoxic conditions through the activation of the Nrf2 pathway [214]. A prolonged inflammatory response ensues characterized by the production of reactive oxygen species (ROS) and upregulation of Nrf2 expression following SCI [215]. This heightened inflammatory response induced by the injury can promote HO. CH6-MF NPs loaded with BMP2 siRNA can effectively scavenge ROS and actively deliver siRNA to MSCs and osteoblasts which effectively inhibits osteogenic differentiation under inflammatory conditions in vitro [216]. The Hedgehog signaling pathway regulates the antioxidant pathway affecting the generation of ROS in tendon-derived stem cells, thereby promoting trauma-induced tendinopathy [217]. Photo-crosslinked nanoparticles responds to the acidic and ROS in the inflammatory microenvironment to suppress HO [218].
Furthermore, the posttraumatic hypoxic microenvironment increases the availability of hypoxia-inducible factor-1 (HIF-1α). The subsequent upregulation of HIF-1α regulates the gene expression of BMPs and neuropilin-1, impacting mechanisms of HO, such as bone resorption and osteogenesis [219, 220]. Moreover, neuroinflammation following nerve injury induces the release of calcitonin gene-related protein, influencing bone metabolism by promoting chondrogenic differentiation of fibro/adipogenic progenitors [221].
In this detailed nexus of interactions, each molecule and cell type play a critical and interconnected role in the development of HO post-nerve injury, illustrating the complexity of the physiological responses that are involved.
Conclusion
HO is a complex pathological condition with numerous associated risk factors. While it is rooted in the pathological differentiation of pluripotent stem cells, it also shares similarities with typical physiological processes. However, our grasp of the cellular origin, etiology, and underlying mechanisms of HO is still not comprehensive. After nerve injury, neurotrophic factors have been shown to play a role in the development of HO, acting through various signaling pathways and in conjunction with local inflammation and immune responses. At present, there are no established treatments specifically for HO. Nonetheless, there is potential that future preventive and therapeutic strategies could utilize innate neuromodulatory mechanisms.
References
Wong KR, Mychasiuk R, O’Brien TJ, Shultz SR, McDonald SJ, Brady RD (2020) Neurological heterotopic ossification: novel mechanisms, prognostic biomarkers and prophylactic therapies. Bone Res 8(1):10
Ranganathan K, Loder S, Agarwal S, Wong VW, Forsberg J, Davis TA, Wang S, James AW, Levi B (2015) Heterotopic ossification: basic-science principles and clinical correlates. J Bone Joint Surg 97(13):1101–1111
Salisbury E, Rodenberg E, Sonnet C, Hipp J, Gannon FH, Vadakkan TJ, Dickinson ME, Olmsted-Davis EA, Davis AR (2011) Sensory nerve induced inflammation contributes to heterotopic ossification. J Cell Biochem 112(10):2748–2758
Olmsted-Davis EA, Salisbury EA, Hoang D, Davis EL, Lazard Z, Sonnet C, Davis TA, Forsberg JA, Davis AR (2017) Progenitors in peripheral nerves launch heterotopic ossification. Stem Cells Transl Med 6(4):1109–1119
Dey D, Wheatley BM, Cholok D, Agarwal S, Yu PB, Levi B, Davis TA (2017) The traumatic bone: trauma-induced heterotopic ossification. Transl Res 186:95–111
Xu Y, Huang M, He W, He C, Chen K, Hou J, Huang M, Jiao Y, Liu R, Zou N, Liu L, Li C (2022) Heterotopic ossification: clinical features, basic researches, and mechanical stimulations. Front Cell Develop Biol 10:1
Wan QQ, Qin WP, Ma YX, Shen MJ, Li J, Zhang ZB, Chen JH, Tay FR, Niu LN, Jiao K (2021) Crosstalk between bone and nerves within bone. Adv Sci. https://doi.org/10.1002/advs.202003390
Lazard ZW, Olmsted-Davis EA, Salisbury EA, Gugala Z, Sonnet C, Davis EL, Beal E, Ubogu EE, Davis AR (2015) Osteoblasts have a neural origin in heterotopic ossification. Clin Orthop Relat Res 473(9):2790–2806
Salisbury E, Sonnet C, Heggeness M, Davis AR, Olmsted-Davis E (2010) Heterotopic ossification has some nerve. Crit Rev Eukaryot Gene Expr 20(4):313–324
Lee S, Hwang C, Marini S, Tower RJ, Qin Q, Negri S, Pagani CA, Sun Y, Stepien DM, Sorkin M, Kubiak CA, Visser ND, Meyers CA, Wang Y, Rasheed HA, Xu J, Miller S, Huber AK, Minichiello L, Cederna PS, Kemp SWP, Clemens TL, James AW, Levi B (2021) NGF-TrkA signaling dictates neural ingrowth and aberrant osteochondral differentiation after soft tissue trauma. Nat Commun. https://doi.org/10.1038/s41467-021-25143-z
Liu Q, Lei L, Yu T, Jiang T, Kang Y (2018) Effect of brain-derived neurotrophic factor on the neurogenesis and osteogenesis in bone engineering. Tissue Eng Part A 24(15–16):1283–1292
Wang Y, Yang K, Li G, Liu R, Liu J, Li J, Tang M, Zhao M, Song J, Wen X (2020) p75NTR−/− mice exhibit an alveolar bone loss phenotype and inhibited PI3K/Akt/β-catenin pathway. Cell Prolif. https://doi.org/10.1111/cpr.12800
Wu K, Huang D, Zhu C, Kasanga EA, Zhang Y, Yu E, Zhang H, Ni Z, Ye S, Zhang C, Hu J, Zhuge Q, Yang J (2019) NT3P75–2 gene-modified bone mesenchymal stem cells improve neurological function recovery in mouse TBI model. Stem Cell Res Ther. https://doi.org/10.1186/s13287-019-1428-1
Abeynayake N, Arthur A, Gronthos S (2021) Crosstalk between skeletal and neural tissues is critical for skeletal health. Bone. https://doi.org/10.1016/j.bone.2020.115645
Chao MV (2003) Neurotrophins and their receptors: a convergence point for many signalling pathways. Nat Rev Neurosci 4(4):299–309
Gautschi OP, Toffoli AM, Joesbury KA, Skirving AP, Filgueira L, Zellweger R (2007) Osteoinductive effect of cerebrospinal fluid from brain-injured patients. J Neurotrauma 24(1):154–162
Huang EJ, Reichardt LF (2001) Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci 24:677–736
Xiao N, Le QT (2016) Neurotrophic factors and their potential applications in tissue regeneration. Arch Immunol Ther Exp 64(2):89–99
Serre CM, Farlay D, Delmas PD, Chenu C (1999) Evidence for a dense and intimate innervation of the bone tissue, including glutamate-containing fibers. Bone 25(6):623–629
Wu M, Chen G, Li YP (2016) TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Res. https://doi.org/10.1038/boneres.2016.9
Lowery JW, Rosen V (2018) The BMP pathway and its inhibitors in the skeleton. Physiol Rev 98(4):2431–2452
Rosen V (2006) BMP and BMP inhibitors in bone. Ann N Y Acad Sci 1068(1):19–25
Yu PB, Deng DY, Lai CS, Hong CC, Cuny GD, Bouxsein ML, Hong DW, McManus PM, Katagiri T, Sachidanandan C, Kamiya N, Fukuda T, Mishina Y, Peterson RT, Bloch KD (2008) BMP type I receptor inhibition reduces heterotopic ossification. Nat Med 14(12):1363–1369
Wang X, Li F, Xie L, Crane J, Zhen G, Mishina Y, Deng R, Gao B, Chen H, Liu S, Yang P, Gao M, Tu M, Wang Y, Wan M, Fan C, Cao X (2018) Inhibition of overactive TGF-β attenuates progression of heterotopic ossification in mice. Nat Commun. https://doi.org/10.1038/s41467-018-02988-5
Balboni TA, Gobezie R, Mamon HJ (2006) Heterotopic ossification: pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys 65(5):1289–1299
Cadosch D, Toffoli AM, Gautschi OP, Frey SP, Zellweger R, Skirving AP, Filgueira L (2010) Serum after traumatic brain injury increases proliferation and supports expression of osteoblast markers in muscle cells. J Bone Joint Surg Am 92(3):645–653
Huang H, Cheng WX, Hu YP, Chen JH, Zheng ZT, Zhang P (2018) Relationship between heterotopic ossification and traumatic brain injury. J Orthop Trans 12:16–25
Morioka K, Marmor Y, Sacramento JA, Lin A, Shao T, Miclau KR, Clark DR, Beattie MS, Marcucio RS, Miclau T, Ferguson AR, Bresnahan JC, Bahney CS (2019) Differential fracture response to traumatic brain injury suggests dominance of neuroinflammatory response in polytrauma. Sci Rep 9(1):12199
Kesavan C, Gomez GA, Pourteymoor S, Mohan S (2023) Development of an animal model for traumatic brain injury augmentation of heterotopic ossification in response to local injury. Biomedicines 11(3):943
Haffner-Luntzer M, Weber B, Morioka K, Lackner I, Fischer V, Bahney C, Ignatius A, Kalbitz M, Marcucio R, Miclau T (2023) Altered early immune response after fracture and traumatic brain injury. Front Immunol. https://doi.org/10.3389/fimmu.2023.1074207
Cao G, Zhang S, Wang Y, Quan S, Yue C, Yao J, Alexander PG, Tan H (2023) Pathogenesis of acquired heterotopic ossification: Risk factors, cellular mechanisms, and therapeutic implications. Bone 168:10
Shlosberg D, Benifla M, Kaufer D, Friedman A (2010) Blood–brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol 6(7):393–403
Scarfì S (2016) Use of bone morphogenetic proteins in mesenchymal stem cell stimulation of cartilage and bone repair. World J Stem Cells. https://doi.org/10.4252/wjsc.v8.i1.1
Tannoury CA, An HS (2014) Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J 14(3):552–559
Cadosch D, Gautschi OP, Thyer M, Song S, Skirving AP, Filgueira L, Zellweger R (2009) Humoral factors enhance fracture-healing and callus formation in patients with traumatic brain injury. J Bone Joint Surg Am 91(2):282–288
Gadomski S, Fielding C, García-García A, Korn C, Kapeni C, Ashraf S, Villadiego J, Toro RD, Domingues O, Skepper JN, Michel T, Zimmer J, Sendtner R, Dillon S, Poole KES, Holdsworth G, Sendtner M, Toledo-Aral JJ, De Bari C, McCaskie AW, Robey PG, Méndez-Ferrer S (2022) A cholinergic neuroskeletal interface promotes bone formation during postnatal growth and exercise. Cell Stem Cell 29(4):528-544.e9
Zhang Y, Xu J, Ruan YC, Yu MK, O’Laughlin M, Wise H, Chen D, Tian L, Shi D, Wang J, Chen S, Feng JQ, Chow DHK, Xie X, Zheng L, Huang L, Huang S, Leung K, Lu N, Zhao L, Li H, Zhao D, Guo X, Chan K, Witte F, Chan HC, Zheng Y, Qin L (2016) Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat Med 22(10):1160–1169
Almangour W, Schnitzler A, Salga M, Debaud C, Denormandie P, Genêt F (2016) Recurrence of heterotopic ossification after removal in patients with traumatic brain injury: a systematic review. Ann Phys Rehabil Med 59(4):263–269
Liu P, Jiang B, Ma J, Lin P, Zhang Y, Shao C, Sun W, Gong Y (2016) S113R mutation in Slc33a1 leads to neurodegeneration and augmented BMP signaling in a mouse model. Dis Models Mech. https://doi.org/10.1242/dmm.026880
Molligan J, Mitchell R, Schon L, Achilefu S, Zahoor T, Cho Y, Loube J, Zhang Z (2016) Influence of bone and muscle injuries on the osteogenic potential of muscle progenitors: contribution of tissue environment to heterotopic ossification. Stem Cells Transl Med 5(6):745–753
Tőkési N, Kozák E, Fülöp K, Dedinszki D, Hegedűs N, Király B, Szigeti K, Ajtay K, Jakus Z, Zaworski J, Letavernier E, Pomozi V, Váradi A (2020) Pyrophosphate therapy prevents trauma-induced calcification in the mouse model of neurogenic heterotopic ossification. J Cell Mol Med 24(20):11791–11799
Salazar VS, Gamer LW, Rosen V (2016) BMP signalling in skeletal development, disease and repair. Nat Rev Endocrinol 12(4):203–221
De La Vega RE, van Griensven M, Zhang W, Coenen MJ, Nagelli CV, Panos JA, Peniche Silva CJ, Geiger J, Plank C, Evans CH, Balmayor ER (2022) Efficient healing of large osseous segmental defects using optimized chemically modified messenger RNA encoding BMP-2. Sci Adv. https://doi.org/10.1126/sciadv.abl6242
Dai G, Li Y, Liu J, Zhang C, Chen M, Lu P, Rui Y (2020) Higher BMP expression in tendon stem/progenitor cells contributes to the increased heterotopic ossification in achilles tendon with aging. Front Cell Develop Biol. https://doi.org/10.3389/fcell.2020.570605
Prados B, del Toro R, MacGrogan D, Gómez-Apiñániz P, Papoutsi T, Muñoz-Cánoves P, Méndez-Ferrer S, de la Pompa JL (2021) Heterotopic ossification in mice overexpressing Bmp2 in Tie2+ lineages. Cell Death Dis. https://doi.org/10.1038/s41419-021-04003-0
Zhang J, Zhao Y, Hou X, Chen B, Xiao Z, Han J, Shi C, Liu J, Miao Q, Dai J (2014) The inhibition effects of insulin on BMP2-induced muscle heterotopic ossification. Biomaterials 35(34):9322–9331
Bhakta G, Lim ZXH, Rai B, Lin T, Hui JH, Prestwich GD, van Wijnen AJ, Nurcombe V, Cool SM (2013) The influence of collagen and hyaluronan matrices on the delivery and bioactivity of bone morphogenetic protein-2 and ectopic bone formation. Acta Biomater 9(11):9098–9106
Rauner M, Baschant U, Roetto A, Pellegrino RM, Rother S, Salbach-Hirsch J, Weidner H, Hintze V, Campbell G, Petzold A, Lemaitre R, Henry I, Bellido T, Theurl I, Altamura S, Colucci S, Muckenthaler MU, Schett G, Komla-Ebri DSK, Bassett JHD, Williams GR, Platzbecker U, Hofbauer LC (2019) Transferrin receptor 2 controls bone mass and pathological bone formation via BMP and Wnt signalling. Nat Metab 1(1):111–124
Xiao L, Michalski N, Kronander E, Gjoni E, Genoud C, Knott G, Schneggenburger R (2013) BMP signaling specifies the development of a large and fast CNS synapse. Nat Neurosci 16(7):856–864
Sun R, Jia T, Dart B, Shrestha S, Bretches M, Heggeness MH, Yang S-Y (2021) Human peripheral nerve-derived pluripotent cells can be stimulated by in vitro bone morphogenetic protein-2. Bioengineering 8(10):10
Norris EH, Strickland S (2017) Fibrinogen in the nervous system: glia beware. Neuron 96(5):951–953
Su YW, Chung R, Ruan CS, Chim SM, Kuek V, Dwivedi PP, Hassanshahi M, Chen KM, Xie Y, Chen L, Foster BK, Rosen V, Zhou XF, Xu J, Xian CJ (2016) Neurotrophin-3 induces BMP-2 and VEGF activities and promotes the bony repair of injured growth plate cartilage and bone in rats. J Bone Miner Res 31(6):1258–1274
Davis EL, Davis AR, Gugala Z, Olmsted-Davis EA (2018) Is heterotopic ossification getting nervous?: The role of the peripheral nervous system in heterotopic ossification. Bone 109:22–27
Tannous O, Stall AC, Griffith C, Donaldson CT, Castellani RJ, Pellegrini VD (2013) Heterotopic bone formation about the hip undergoes endochondral ossification: a rabbit model. Clin Orthop Relat Res 471(5):1584–1592
Lin L, Shen Q, Leng H, Duan X, Fu X, Yu C (2011) Synergistic inhibition of endochondral bone formation by silencing Hif1α and Runx2 in trauma-induced heterotopic ossification. Mol Ther 19(8):1426–1432
Xu R, Hu J, Zhou X, Yang Y (2018) Heterotopic ossification: Mechanistic insights and clinical challenges. Bone 109:134–142
Banham-Hall N, Kothwal K, Pipkin J, Bentley J, Dickens GL (2013) Prevalence of low bone mineral density in inpatients with traumatic brain injury receiving neurobehavioural rehabilitation: a postoperative, observational study. Physiotherapy 99(4):328–334
McDonald SJ, Sharkey JM, Sun M, Kaukas LM, Shultz SR, Turner RJ, Leonard AV, Brady RD, Corrigan F (2020) Beyond the brain: peripheral interactions after traumatic brain injury. J Neurotrauma 37(5):770–781
Yu H, Watt H, Mohan S (2014) The negative impact of traumatic brain injury (TBI) on bone in a mouse model. Brain Inj 28(2):244–251
Bajwa NM, Kesavan C, Mohan S (2018) Long-term consequences of traumatic brain injury in bone metabolism. Front Neurol 9:115
Smith É, Comiskey C, Carroll Á (2016) Prevalence of and risk factors for osteoporosis in adults with acquired brain injury. Ir J Med Sci 185(2):473–481
Tabuchi M, Miyazawa K, Kimura M, Maeda H, Kawai T, Kameyama Y, Goto S (2005) Enhancement of crude bone morphogenetic protein-induced new bone formation and normalization of endochondral ossification by bisphosphonate treatment in osteoprotegerin-deficient mice. Calcif Tissue Int 77(4):239–249
Yuan P, Wang WC, Li ZH, Mao XZ (2009) Could insertion of the particles that induce osteolysis be a new treatment option in heterotopic ossification? Med Hypotheses 73(1):27–28
Oleson CV, Seidel BJ, Zhan T (2013) Association of vitamin D deficiency, secondary hyperparathyroidism, and heterotopic ossification in spinal cord injury. J Rehabil Res Dev 50(9):1177–1186
Benayahu D, Fried A, Wientroub S (1995) PTH and 1,25(OH)2 vitamin D priming to growth factors differentially regulates the osteoblastic markers in MBA-15 clonal subpopulations. Biochem Biophys Res Commun 210(1):197–204
Canalis E (2010) Update in new anabolic therapies for osteoporosis. J Clin Endocrinol Metab 95(4):1496–1504
Amizuka N, Warshawsky H, Henderson JE, Goltzman D, Karaplis AC (1994) Parathyroid hormone-related peptide-depleted mice show abnormal epiphyseal cartilage development and altered endochondral bone formation. J Cell Biol 126(6):1611–1623
Ansari N, Ho PWM, Crimeen-Irwin B, Poulton IJ, Brunt AR, Forwood MR, Divieti Pajevic P, Gooi JH, Martin TJ, Sims NA (2017) Autocrine and paracrine regulation of the murine skeleton by osteocyte-derived parathyroid hormone-related protein. J Bone Mineral Res 33(1):137–153
Martin TJ, Allan EH, Ho PWM, Gooi JH, Quinn JMW, Gillespie MT, Krasnoperov V, Sims NA (2009) Communication between EphrinB2 and EphB4 within the osteoblast lineage. In: Choi Y (ed) Osteoimmunology. Springer, Boston, pp 51–60
Ducy P, Desbois C, Boyce B, Pinero G, Story B, Dunstan C, Smith E, Bonadio J, Goldstein S, Gundberg C, Bradley A, Karsenty G (1996) Increased bone formation in osteocalcin-deficient mice. Nature 382(6590):448–452
Trentz OA, Handschin AE, Bestmann L, Hoerstrup SP, Trentz OL, Platz A (2005) Influence of brain injury on early posttraumatic bone metabolism. Crit Care Med 33(2):399–406
Sundaram VK, Schütza V, Schröter NH, Backhaus A, Bilsing A, Joneck L, Seelbach A, Mutschler C, Gomez-Sanchez JA, Schäffner E, Sánchez EE, Akkermann D, Paul C, Schwagarus N, Müller S, Odle A, Childs G, Ewers D, Kungl T, Sitte M, Salinas G, Sereda MW, Nave KA, Schwab MH, Ost M, Arthur-Farraj P, Stassart RM, Fledrich R (2023) Adipo-glial signaling mediates metabolic adaptation in peripheral nerve regeneration. Cell Metab. https://doi.org/10.1016/j.cmet.2023.10.017
Handschin AE, Trentz OA, Hemmi S, Wedler V, Trentz O, Giovanoli P, Wanner GA (2007) Leptin increases extracellular matrix mineralization of human osteoblasts from heterotopic ossification and normal bone. Ann Plast Surg 59(3):329–333
Agarwal S, Loder S, Li J, Brownley C, Peterson JR, Oluwatobi E, Drake J, Cholok D, Ranganathan K, Sung HH, Goulet J, Li S, Levi B (2015) Diminished chondrogenesis and enhanced osteoclastogenesis in leptin-deficient diabetic mice (ob/ob) impair pathologic trauma-induced heterotopic ossification. Stem Cells Develop 24(24):2864–2872
Nishimura R, Hata K, Takahata Y, Murakami T, Nakamura E, Ohkawa M, Ruengsinpinya L (2020) Role of signal transduction pathways and transcription factors in cartilage and joint diseases. Int J Mol Sci 21(4):1340
Di Rocco F, Biosse Duplan M, Heuzé Y, Kaci N, Komla-Ebri D, Munnich A, Mugniery E, Benoist-Lasselin C, Legeai-Mallet L (2014) FGFR3 mutation causes abnormal membranous ossification in achondroplasia. Hum Mol Gene 23(11):2914–2925
Mugniery E, Dacquin R, Marty C, Benoist-Lasselin C, de Vernejoul M-C, Jurdic P, Munnich A, Geoffroy V, Legeai-Mallet L (2012) An activating Fgfr3 mutation affects trabecular bone formation via a paracrine mechanism during growth. Hum Mol Genet 21(11):2503–2513
Huang EJ, Reichardt LF (2001) Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci 24(1):677–736
Xiao N, Le QT (2015) Neurotrophic factors and their potential applications in tissue regeneration. Arch Immunol Ther Exp 64(2):89–99
Emanueli C, Schratzberger P, Kirchmair R, Madeddu P (2009) Paracrine control of vascularization and neurogenesis by neurotrophins. Br J Pharmacol 140(4):614–619
Keefe K, Sheikh I, Smith G (2017) Targeting neurotrophins to specific populations of neurons: NGF, BDNF, and NT-3 and their relevance for treatment of spinal cord injury. Int J Mol Sci 18(3):1
Sun S, Diggins NH, Gunderson ZJ, Fehrenbacher JC, White FA, Kacena MA (2020) No pain, no gain? The effects of pain-promoting neuropeptides and neurotrophins on fracture healing. Bone. https://doi.org/10.1016/j.bone.2019.115109
Lewin GR, Nykjaer A (2014) Pro-neurotrophins, sortilin, and nociception. Eur J Neurosci 39(3):363–374
Kobayashi H, Gleich GJ, Butterfield JH, Kita H (2002) Human eosinophils produce neurotrophins and secrete nerve growth factor on immunologic stimuli. Blood 99(6):2214–2220
Su YW, Zhou XF, Foster BK, Grills BL, Xu J, Xian CJ (2017) Roles of neurotrophins in skeletal tissue formation and healing. J Cell Physiol 233(3):2133–2145
Xu J, Li Z, Tower RJ, Negri S, Wang Y, Meyers CA, Sono T, Qin Q, Lu A, Xing X, McCarthy EF, Clemens TL, James AW (2022) NGF-p75 signaling coordinates skeletal cell migration during bone repair. Sci Adv 8(11):eabl5716
Wang L, Zhou S, Liu B, Lei D, Zhao Y, Lu C, Tan A (2006) Locally applied nerve growth factor enhances bone consolidation in a rabbit model of mandibular distraction osteogenesis. J Orthop Res 24(12):2238–2245
Rivera KO, Russo F, Boileau RM, Tomlinson RE, Miclau T, Marcucio RS, Desai TA, Bahney CS (2020) Local injections of β-NGF accelerates endochondral fracture repair by promoting cartilage to bone conversion. Sci Rep 10(1):22241
Cherief M, Negri S, Qin Q, Pagani CA, Lee S, Yang YP, Clemens TL, Levi B, James AW (2022) TrkA+ neurons induce pathologic regeneration after soft tissue trauma. Stem Cells Transl Med 11(11):1165–1176
Zhang J, Brodie C, Li Y, Zheng X, Roberts C, Lu M, Gao Q, Borneman J, Savant-Bhonsale S, Elias SB, Chopp M (2009) Bone marrow stromal cell therapy reduces proNGF and p75 expression in mice with experimental autoimmune encephalomyelitis. J Neurol Sci 279(1–2):30–38
Wu XH, Dou B, Sun NY, Gao J, Liu XL (2020) Astragalus saponin IV promotes osteogenic differentiation of bone marrow mesenchymal stem cells via miR-21/NGF/BMP2/Runx2 pathway. Acta Histochem. https://doi.org/10.1016/j.acthis.2020.151549
Grills BL, Schuijers JA, Ward AR (1997) Topical application of nerve growth factor improves fracture healing in rats. J Orthop Res 15(2):235–242
Li Z, Meyers CA, Chang L, Lee S, Li Z, Tomlinson R, Hoke A, Clemens TL, James AW (2019) Fracture repair requires TrkA signaling by skeletal sensory nerves. J Clin Investig 129(12):5137–5150
Yasui M, Shiraishi Y, Ozaki N, Hayashi K, Hori K, Ichiyanagi M, Sugiura Y (2011) Nerve growth factor and associated nerve sprouting contribute to local mechanical hyperalgesia in a rat model of bone injury. Eur J Pain 16(7):953–965
Fitzpatrick V, Martín-Moldes Z, Deck A, Torres-Sanchez R, Valat A, Cairns D, Li C, Kaplan DL (2021) Functionalized 3D-printed silk-hydroxyapatite scaffolds for enhanced bone regeneration with innervation and vascularization. Biomaterials. https://doi.org/10.1016/j.biomaterials.2021.120995
Tomlinson RE, Li Z, Li Z, Minichiello L, Riddle RC, Venkatesan A, Clemens TL (2017) NGF-TrkA signaling in sensory nerves is required for skeletal adaptation to mechanical loads in mice. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.1701054114
Jiang Y, Tuan RS (2019) Role of NGF-TrkA signaling in calcification of articular chondrocytes. FASEB J 33(9):10231–10239
Meyers CA, Lee S, Sono T, Xu J, Negri S, Tian Y, Wang Y, Li Z, Miller S, Chang L, Gao Y, Minichiello L, Clemens TL, James AW (2020) A neurotrophic mechanism directs sensory nerve transit in cranial bone. Cell Rep. https://doi.org/10.1016/j.celrep.2020.107696
Wang D, Zhang J, Zheng MG, Sui WY, He ZD, Liu Y, Huang YL, Mu SH, Xu XZ, Zhang JS, Qu JL (2019) TrkA regulates the regenerative capacity of bone marrow stromal stem cells in nerve grafts. Neural Regen Res. https://doi.org/10.4103/1673-5374.257540
McCaffrey G, Thompson ML, Majuta L, Fealk MN, Chartier S, Longo G, Mantyh PW (2014) NGF blockade at early times during bone cancer development attenuates bone destruction and increases limb use. Can Res 74(23):7014–7023
Spoletini M, Taurone S, Tombolini M, Minni A, Altissimi G, Wierzbicki V, Giangaspero F, Parnigotto PP, Artico M, Bardella L, Agostinelli E, Pastore FS (2017) Trophic and neurotrophic factors in human pituitary adenomas (review). Int J Oncol 51(4):1014–1024
Novack DV (2010) Role of NF-κB in the skeleton. Cell Res 21(1):169–182
Tarapore RS, Lim J, Tian C, Pacios S, Xiao W, Reid D, Guan H, Mattos M, Yu B, Wang CY, Graves DT (2015) NF-κB has a direct role in inhibiting Bmp- and Wnt-induced matrix protein expression. J Bone Miner Res 31(1):52–64
Zhu M, Xu W, Jiang J, Wang Y, Guo Y, Yang R, Chang Y, Zhao B, Wang Z, Zhang J, Wang T, Shangguan L, Wang S (2021) Peiminine suppresses RANKL-induced osteoclastogenesis by inhibiting the NFATc1, ERK, and NF-κB signaling pathways. Front Endocrinol. https://doi.org/10.3389/fendo.2021.736863
Barruet E, Morales BM, Cain CJ, Ton AN, Wentworth KL, Chan TV, Moody TA, Haks MC, Ottenhoff THM, Hellman J, Nakamura MC, Hsiao EC (2018) NF-κB/MAPK activation underlies ACVR1-mediated inflammation in human heterotopic ossification. JCI Insight. https://doi.org/10.1172/jci.insight.122958
Dai WL, Yan B, Bao YN, Fan JF, Liu JH (2020) Suppression of peripheral NGF attenuates neuropathic pain induced by chronic constriction injury through the TAK1-MAPK/NF-κB signaling pathways. Cell Commun Signal. https://doi.org/10.1186/s12964-020-00556-3
Ni H, Wang Y, An K, Liu Q, Xu L, Zhu C, Deng H, He Q, Wang T, Xu M, Zheng Y, Huang B, Fang J, Yao M (2019) Crosstalk between NFκB-dependent astrocytic CXCL1 and neuron CXCR2 plays a role in descending pain facilitation. J Neuroinflam. https://doi.org/10.1186/s12974-018-1391-2
Jung EJ, Paramanantham A, Kim HJ, Shin SC, Kim GS, Jung JM, Hong SC, Chung KH, Kim CW, Lee WS (2022) Identification of growth factors, cytokines and mediators regulated by Artemisia annua L. polyphenols (pKAL) in HCT116 colorectal cancer cells: TGF-β1 and NGF-β attenuate pKAL-induced anticancer effects via NF-κB p65 upregulation. Int J Mol Sci. https://doi.org/10.3390/ijms23031598
Loy TL, Vehlow D, Kauschke V, Müller M, Heiss C, Lips KS (2020) Effects of BDNF and PEC nanoparticles on osteocytes. Molecules. https://doi.org/10.3390/molecules25184151
Spejo AB, Chiarotto GB, Ferreira ADF, Gomes DA, Ferreira RS, Barraviera B, Oliveira ALR (2018) Neuroprotection and immunomodulation following intraspinal axotomy of motoneurons by treatment with adult mesenchymal stem cells. J Neuroinflam. https://doi.org/10.1186/s12974-018-1268-4
Fiorina P, Sharma GP, Frei AC, Narayanan J, Gasperetti T, Veley D, Amjad A, Albano K, Fish BL, Himburg HA (2021) Brain-derived neurotrophic factor promotes immune reconstitution following radiation injury via activation of bone marrow mesenchymal stem cells. PLoS ONE. https://doi.org/10.1371/journal.pone.0259042
Xiong J, Liao J, Liu X, Zhang Z, Adams J, Pacifici R, Ye K (2022) A TrkB agonist prodrug prevents bone loss via inhibiting asparagine endopeptidase and increasing osteoprotegerin. Nat Commun. https://doi.org/10.1038/s41467-022-32435-5
Kajiya M, Shiba H, Fujita T, Ouhara K, Takeda K, Mizuno N, Kawaguchi H, Kitagawa M, Takata T, Tsuji K, Kurihara H (2008) Brain-derived neurotrophic factor stimulates bone/cementum-related protein gene expression in cementoblasts. J Biol Chem 283(23):16259–16267
Xue F, Zhao Z, Gu Y, Han J, Ye K, Zhang Y (2021) 7,8-Dihydroxyflavone modulates bone formation and resorption and ameliorates ovariectomy-induced osteoporosis. Elife. https://doi.org/10.7554/eLife.64872
Sun CY, Chu ZB, She XM, Zhang L, Chen L, Ai LS, Hu Y (2012) Brain-derived neurotrophic factor is a potential osteoclast stimulating factor in multiple myeloma. Int J Cancer 130(4):827–836
Ai LS, Sun CY, Wang YD, Zhang L, Chu ZB, Qin Y, Gao F, Yan H, Guo T, Chen L, Yang D, Hu Y (2013) Gene silencing of the BDNF/TrkB axis in multiple myeloma blocks bone destruction and tumor burden in vitro and in vivo. Int J Cancer 133(5):1074–1084
Wang Y, Gao Y, Wang Y, Zhang H, Qin Q, Xu Z, Liu S, Wang X, Qu Y, Liu Y, Jiang X, He H (2023) GDNF promotes the proliferation and osteogenic differentiation of jaw bone marrow mesenchymal stem cells via the Nr4a1/PI3K/Akt pathway. Cell Signal. https://doi.org/10.1016/j.cellsig.2023.110721
Li X, Zheng Y, Zheng Y, Huang Y, Zhang Y, Jia L, Li W (2018) Circular RNA CDR1as regulates osteoblastic differentiation of periodontal ligament stem cells via the miR-7/GDF5/SMAD and p38 MAPK signaling pathway. Stem Cell Res Ther. https://doi.org/10.1186/s13287-018-0976-0
Kim JM, Yang YS, Park KH, Oh H, Greenblatt MB, Shim JH (2019) The ERK MAPK pathway is essential for skeletal development and homeostasis. Int J Mol Sci. https://doi.org/10.3390/ijms20081803
Tang L, Wu M, Lu S, Zhang H, Shen Y, Shen C, Liang H, Ge H, Ding X, Wang Z (2021) Fgf9 negatively regulates bone mass by inhibiting osteogenesis and promoting osteoclastogenesis via MAPK and PI3K/AKT signaling. J Bone Miner Res 36(4):779–791
Cintrón-Colón AF, Almeida-Alves G, Boynton AM, Spitsbergen JM (2020) GDNF synthesis, signaling, and retrograde transport in motor neurons. Cell Tissue Res 382(1):47–56
Zhang J, Wang L, Cao H, Chen N, Yan B, Ao X, Zhao H, Chu J, Huang M, Zhang Z (2019) Neurotrophin-3 acts on the endothelial-mesenchymal transition of heterotopic ossification in rats. J Cell Mol Med 23(4):2595–2609
Zhang J, Wang L, Chu J, Ao X, Jiang T, Yan B, Huang M, Zhang Z (2020) Macrophage-derived neurotrophin-3 promotes heterotopic ossification in rats. Lab Invest 100(5):762–776
Zhu T, Yu D, Feng J, Wu X, Xiang L, Gao H, Zhang X, Wei M (2014) GDNF and NT-3 induce progenitor bone mesenchymal stem cell differentiation into neurons in fetal gut culture medium. Cell Mol Neurobiol 35(2):255–264
Yuan J, Huang G, Xiao Z, Lin L, Han T (2013) Overexpression of β-NGF promotes differentiation of bone marrow mesenchymal stem cells into neurons through regulation of AKT and MAPK pathway. Mol Cell Biochem 383(1–2):201–211
Zhang Z, Wang F, Huang X, Sun H, Xu J, Qu H, Yan X, Shi W, Teng W, Jin X, Shao Z, Zhang Y, Zhao S, Wu Y, Ye Z, Yu X (2023) Engineered sensory nerve guides self-adaptive bone healing via NGF-TrkA signaling pathway. Adv Sci. https://doi.org/10.1002/advs.202206155
Takeda K, Shiba H, Mizuno N, Hasegawa N, Mouri Y, Hirachi A, Yoshino H, Kawaguchi H, Kurihara H (2005) Brain-derived neurotrophic factor enhances periodontal tissue regeneration. Tissue Eng 11(9–10):1618–1629
Li X, Sun DC, Li Y, Wu XY (2018) Neurotrophin-3 improves fracture healing in rats. Eur Rev Med Pharmacol Sci 22(8):2439–2446
Malet M, Brumovsky PR (2015) VGLUTs and glutamate synthesis-focus on DRG neurons and pain. Biomolecules 5(4):3416–3437
Patton AJ, Genever PG, Birch MA, Suva LJ, Skerry TM (1998) Expression of an N-methyl-D-aspartate-type receptor by human and rat osteoblasts and osteoclasts suggests a novel glutamate signaling pathway in bone. Bone 22(6):645–649
Bozic M, Valdivielso JM (2015) The potential of targeting NMDA receptors outside the CNS. Expert Opin Ther Targets 19(3):399–413
Ho ML, Tsai TN, Chang JK, Shao TS, Jeng YR, Hsu C (2005) Down-regulation of N-methyl D-aspartate receptor in rat-modeled disuse osteopenia. Osteoporos Int 16(12):1780–1788
Parisi E, Bozic M, Ibarz M, Panizo S, Valcheva P, Coll B, Fernández E, Valdivielso JM (2010) Sustained activation of renal N-methyl-D-aspartate receptors decreases vitamin D synthesis: a possible role for glutamate on the onset of secondary HPT. Am J Physiol Endocrinol Metab 299(5):E825–E831
Veldhuis-Vlug AG, Oei L, Souverein PC, Tanck MW, Rivadeneira F, Zillikens MC, Kamphuisen PW, Maitland-van der Zee AH, de Groot MC, Hofman A, Uitterlinden AG, Fliers E, de Boer A, Bisschop PH (2015) Association of polymorphisms in the beta-2 adrenergic receptor gene with fracture risk and bone mineral density. Osteoporos Int 26(7):2019–2027
Kajimura D, Hinoi E, Ferron M, Kode A, Riley KJ, Zhou B, Guo XE, Karsenty G (2011) Genetic determination of the cellular basis of the sympathetic regulation of bone mass accrual. J Exp Med 208(4):841–851
Veldhuis-Vlug AG, Tanck MW, Limonard EJ, Endert E, Heijboer AC, Lips P, Fliers E, Bisschop PH (2015) The effects of beta-2 adrenergic agonist and antagonist on human bone metabolism: a randomized controlled trial. Bone 71:196–200
Morikawa M, Derynck R, Miyazono K (2016) TGF-β and the TGF-β family: context-dependent roles in cell and tissue physiology. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a021873
Hata A, Chen YG (2016) TGF-β Signaling from receptors to smads. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a022061
Zhang Y, Alexander PB, Wang XF (2017) TGF-β family signaling in the control of cell proliferation and survival. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a022145
Zhang YE (2018) Mechanistic insight into contextual TGF-β signaling. Curr Opin Cell Biol 51:1–7
Derynck R, Budi EH (2019) Specificity, versatility, and control of TGF-β family signaling. Sci Signal. https://doi.org/10.1126/scisignal.aav5183
Alexander KA, Tseng HW, Salga M, Genêt F, Levesque J-P (2020) When the nervous system turns skeletal muscles into bones: how to solve the conundrum of neurogenic heterotopic ossification. Curr Osteoporos Rep 18(6):666–676
de Vasconcellos JF, Zicari S, Fernicola SD, Griffin DW, Ji Y, Shin EH, Jones P, Christopherson GT, Bharmal H, Cirino C, Nguyen T, Robertson A, Pellegrini VD, Nesti LJ (2019) In vivo model of human post-traumatic heterotopic ossification demonstrates early fibroproliferative signature. J Transl Med. https://doi.org/10.1186/s12967-019-1996-y
Crane JL, Cao X (2014) Bone marrow mesenchymal stem cells and TGF-β signaling in bone remodeling. J Clin Investig 124(2):466–472
Grafe I, Alexander S, Peterson JR, Snider TN, Levi B, Lee B, Mishina Y (2018) TGF-β family signaling in mesenchymal differentiation. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a022202
Yu T, Zhang J, Zhu W, Wang X, Bai Y, Feng B, Zhuang Q, Han C, Wang S, Hu Q, An S, Wan M, Dong S, Xu J, Weng X, Cao X (2021) Chondrogenesis mediates progression of ankylosing spondylitis through heterotopic ossification. Bone Res. https://doi.org/10.1038/s41413-021-00140-6
Chen NF, Huang SY, Chen WF, Chen CH, Lu CH, Chen CL, Yang SN, Wang HM, Wen ZH (2013) TGF-β1 attenuates spinal neuroinflammation and the excitatory amino acid system in rats with neuropathic pain. J Pain 14(12):1671–1685
Sulaiman W, Dreesen T, Nguyen D (2018) Single local application of TGF-β promotes a proregenerative state throughout a chronically injured nerve. Neurosurgery 82(6):894–902
Meyers EA, Kessler JA (2017) TGF-β family signaling in neural and neuronal differentiation, development, and function. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a022244
Hammond TR, Marsh SE, Stevens B (2019) Immune signaling in neurodegeneration. Immunity 50(4):955–974
Bastien D, Lacroix S (2014) Cytokine pathways regulating glial and leukocyte function after spinal cord and peripheral nerve injury. Exp Neurol 258:62–77
Lee JS, Hsu YH, Chiu YS, Jou IM, Chang MS (2020) Anti-IL-20 antibody improved motor function and reduced glial scar formation after traumatic spinal cord injury in rats. J Neuroinflam. https://doi.org/10.1186/s12974-020-01814-4
Patterson ZR, Holahan MR (2012) Understanding the neuroinflammatory response following concussion to develop treatment strategies. Front Cell Neurosci. https://doi.org/10.3389/fncel.2012.00058
Ye Z, Wei J, Zhan C, Hou J (2022) Role of transforming growth factor beta in peripheral nerve regeneration: cellular and molecular mechanisms. Front Neurosci. https://doi.org/10.3389/fnins.2022.917587
Nguyen D, Sulaiman W (2016) Transforming growth factor beta 1, a cytokine with regenerative functions. Neural Regen Res. https://doi.org/10.4103/1673-5374.193223
Sulaiman W, Dreesen TD (2014) Effect of local application of transforming growth factor–β at the nerve repair site following chronic axotomy and denervation on the expression of regeneration-associated genes. J Neurosurg 121(4):859–874
Wu J, Lu B, Yang R, Chen Y, Chen X, Li Y (2021) EphB2 knockdown decreases the formation of astroglial-fibrotic scars to promote nerve regeneration after spinal cord injury in rats. CNS Neurosci Ther 27(6):714–724
Song S, Wang S, Pigott VM, Jiang T, Foley LM, Mishra A, Nayak R, Zhu W, Begum G, Shi Y, Carney KE, Hitchens TK, Shull GE, Sun D (2018) Selective role of Na+/H+ exchanger in Cx3cr1+ microglial activation, white matter demyelination, and post-stroke function recovery. Glia 66(11):2279–2298
Kisucká A, Bimbová K, Bačová M, Gálik J, Lukáčová N (2021) Activation of neuroprotective microglia and astrocytes at the lesion site and in the adjacent segments is crucial for spontaneous locomotor recovery after spinal cord injury. Cells. https://doi.org/10.3390/cells10081943
Wang W, He D, Chen J, Zhang Z, Wang S, Jiang Y, Wei J (2021) Circular RNA plek promotes fibrogenic activation by regulating the miR-135b-5p/TGF-βR1 axis after spinal cord injury. Aging 13(9):13211–13224
Rahman MS, Akhtar N, Jamil HM, Banik RS, Asaduzzaman SM (2015) TGF-β/BMP signaling and other molecular events: regulation of osteoblastogenesis and bone formation. Bone Res. https://doi.org/10.1038/boneres.2015.5
Katsuno Y, Derynck R (2021) Epithelial plasticity, epithelial-mesenchymal transition, and the TGF-β family. Dev Cell 56(6):726–746
Herpin A, Cunningham C (2007) Cross-talk between the bone morphogenetic protein pathway and other major signaling pathways results in tightly regulated cell-specific outcomes. FEBS J 274(12):2977–2985
Moustakas A, Heldin C-H (2005) Non-Smad TGF-beta signals. J Cell Sci 118(Pt 16):3573–3584
Engin F, Lee B (2010) NOTCHing the bone: insights into multi-functionality. Bone 46(2):274–280
Zhen G, Cao X (2014) Targeting TGFβ signaling in subchondral bone and articular cartilage homeostasis. Trends Pharmacol Sci 35(5):227–236
Cui Z, Crane J, Xie H, Jin X, Zhen G, Li C, Xie L, Wang L, Bian Q, Qiu T, Wan M, Xie M, Ding S, Yu B, Cao X (2016) Halofuginone attenuates osteoarthritis by inhibition of TGF-β activity and H-type vessel formation in subchondral bone. Ann Rheum Dis 75(9):1714–1721
Mao D, Pan X, Rui Y, Li F (2020) Matrine attenuates heterotopic ossification by suppressing TGF-β induced mesenchymal stromal cell migration and osteogenic differentiation. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2020.110152
Huh Y, Ji RR, Chen G (2017) Neuroinflammation, bone marrow stem cells, and chronic pain. Front Immunol. https://doi.org/10.3389/fimmu.2017.01014
Deng R, Li C, Wang X, Chang L, Ni S, Zhang W, Xue P, Pan D, Wan M, Deng L, Cao X (2021) Periosteal CD68+F4/80+ macrophages are mechanosensitive for cortical bone formation by secretion and activation of TGF-β1. Adv Sci. https://doi.org/10.1002/advs.202103343
Patel NK, Nunez JH, Sorkin M, Marini S, Pagani CA, Strong AL, Hwang CD, Li S, Padmanabhan KR, Kumar R, Bancroft AC, Greenstein JA, Nelson R, Rasheed HA, Livingston N, Vasquez K, Huber AK, Levi B (2022) Macrophage TGF-β signaling is critical for wound healing with heterotopic ossification after trauma. JCI Insight. https://doi.org/10.1172/jci.insight.144925
Zhen G, Wen C, Jia X, Li Y, Crane JL, Mears SC, Askin FB, Frassica FJ, Chang W, Yao J, Carrino JA, Cosgarea A, Artemov D, Chen Q, Zhao Z, Zhou X, Riley L, Sponseller P, Wan M, Lu WW, Cao X (2013) Inhibition of TGF-β signaling in mesenchymal stem cells of subchondral bone attenuates osteoarthritis. Nat Med 19(6):704–712
Bailey KN, Nguyen J, Yee CS, Dole NS, Dang A, Alliston T (2021) Mechanosensitive control of articular cartilage and subchondral bone homeostasis in mice requires osteocytic transforming growth factor β signaling. Arthr Rheumatol 73(3):414–425
Tu B, Li J, Sun Z, Zhang T, Liu H, Yuan F, Fan C (2022) Macrophage-derived TGF-β and VEGF promote the progression of trauma-induced HO. Inflammation 46(1):202–216
Liu W, Feng M, Jayasuriya CT, Peng H, Zhang L, Guan Y, Froehlich JA, Terek RM, Chen Q (2020) Human osteoarthritis cartilage-derived stromal cells activate joint degeneration through TGF-beta lateral signaling. FASEB J 34(12):16552–16566
Zhang P, Zhang H, Lin J, Xiao T, Xu R, Fu Y, Zhang Y, Du Y, Cheng J, Jiang H (2020) Insulin impedes osteogenesis of BMSCs by inhibiting autophagy and promoting premature senescence via the TGF-β1 pathway. Aging 12(3):2084–2100
Evangelista AF, Vannier-Santos MA, de Assis Silva GS, Silva DN, Juiz PJL, Nonaka CKV, dos Santos RR, Soares MBP, Villarreal CF (2018) Bone marrow-derived mesenchymal stem/stromal cells reverse the sensorial diabetic neuropathy via modulation of spinal neuroinflammatory cascades. J Neuroinflam. https://doi.org/10.1186/s12974-018-1224-3
Coassin M, Lambiase A, Micera A, Tirassa P, Aloe L, Bonini S (2005) Nerve growth factor modulates in vitro the expression and release of TGF-β1 by amniotic membrane. Graefes Arch Clin Exp Ophthalmol 244(4):485–491
Lee HC, Hsu YM, Tsai CC, Ke CJ, Yao CH, Chen YS (2015) Improved peripheral nerve regeneration in streptozotocin-induced diabetic rats by oral lumbrokinase. Am J Chin Med 43(02):215–230
Blaney Davidson EN, van Caam APM, Vitters EL, Bennink MB, Thijssen E, van den Berg WB, Koenders MI, van Lent PLEM, van de Loo FAJ, van der Kraan PM (2015) TGF-β is a potent inducer of nerve growth factor in articular cartilage via the ALK5-Smad2/3 pathway. Potential role in OA related pain? Osteoarthr Cartil 23(3):478–486
Driscoll C, Chanalaris A, Knights C, Ismail H, Sacitharan PK, Gentry C, Bevan S, Vincent TL (2016) Nociceptive sensitizers are regulated in damaged joint tissues including articular cartilage, when osteoarthritic mice display pain behaviour. Arthr Rheumatol 68(4):857–867
Li S, Gu X, Yi S (2017) The regulatory effects of transforming growth factor-β on nerve regeneration. Cell Transplant 26(3):381–394
Yokozeki Y, Uchida K, Kawakubo A, Nakawaki M, Okubo T, Miyagi M, Inoue G, Itakura M, Sekiguchi H, Takaso M (2021) TGF-β regulates nerve growth factor expression in a mouse intervertebral disc injury model. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-021-04509-w
Scherer SS, Kamholz J, Jakowlew SB (1993) Axons modulate the expression of transforming growth factor-betas in Schwann cells. Glia 8(4):265–276
Chalazonitis A, Kalberg J, Twardzik DR, Morrison RS, Kessler JA (1992) Transforming growth factor beta has neurotrophic actions on sensory neurons in vitro and is synergistic with nerve growth factor. Dev Biol 152(1):121–132
Tower RJ, Li Z, Cheng YH, Wang XW, Rajbhandari L, Zhang Q, Negri S, Uytingco CR, Venkatesan A, Zhou FQ, Cahan P, James AW, Clemens TL (2021) Spatial transcriptomics reveals a role for sensory nerves in preserving cranial suture patency through modulation of BMP/TGF-β signaling. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.2103087118
Bouchet C, Cardouat G, Douard M, Coste F, Robillard P, Delcambre F, Ducret T, Quignard JF, Vacher P, Baudrimont I, Marthan R, Berger P, Guibert C, Freund-Michel V (2022) Inflammation and oxidative stress induce NGF secretion by pulmonary arterial cells through a TGF-β1-dependent mechanism. Cells. https://doi.org/10.3390/cells11182795
Li Z, Meyers CA, Chang L, Lee S, Li Z, Tomlinson R, Hoke A, Clemens TL, James AW (2019) Fracture repair requires TrkA signaling by skeletal sensory nerves. J Clin Invest 129(12):5137–5150
Ohta M, Chosa N, Kyakumoto S, Yokota S, Okubo N, Nemoto A, Kamo M, Joh S, Satoh K, Ishisaki A (2018) IL-1β and TNF-α suppress TGF-β-promoted NGF expression in periodontal ligament-derived fibroblasts through inactivation of TGF-β-induced Smad2/3- and p38 MAPK-mediated signals. Int J Mol Med 42(3):1484–1494
Haas SL, Fitzner B, Jaster R, Wiercinska E, Gaitantzi H, Jesnowski R, Lohr JM, Singer MV, Dooley S, Breitkopf K (2009) Transforming growth factor-beta induces nerve growth factor expression in pancreatic stellate cells by activation of the ALK-5 pathway. Growth Factors 27(5):289–299
Villapol S, Wang Y, Adams M, Symes AJ (2013) Smad3 deficiency increases cortical and hippocampal neuronal loss following traumatic brain injury. Exp Neurol 250:353–365
Vizza D, Perri A, Toteda G, Lupinacci S, Leone F, Gigliotti P, Lofaro D, La Russa A, Bonofiglio R (2015) Nerve growth factor exposure promotes tubular epithelial–mesenchymal transitionviaTGF-β1 signaling activation. Growth Factors 33(3):169–180
Yin J, Chang HM, Yi Y, Yao Y, Leung PCK (2020) TGF-β1 increases GDNF production by upregulating the expression of GDNF and furin in human granulosa-lutein cells. Cells. https://doi.org/10.3390/cells9010185
Harvey BK, Hoffer BJ, Wang Y (2005) Stroke and TGF-β proteins: glial cell line-derived neurotrophic factor and bone morphogenetic protein. Pharmacol Ther 105(2):113–125
Shen WX, Chen JH, Lu JH, Peng YP, Qiu YH (2014) TGF-β1 protection against Aβ1–42-induced neuroinflammation and neurodegeneration in rats. Int J Mol Sci 15(12):22092–22108
Krieglstein K, Strelau J, Schober A, Sullivan A, Unsicker K (2002) TGF-beta and the regulation of neuron survival and death. J Physiol Paris 96(1–2):25–30
Naik AS, Lin JM, Taroc EZM, Katreddi RR, Frias JA, Lemus AA, Sammons MA, Forni PE (2020) Smad4-dependent morphogenic signals control the maturation and axonal targeting of basal vomeronasal sensory neurons to the accessory olfactory bulb. Development. https://doi.org/10.1242/dev.184036
Yu AL, Fuchshofer R, Birke M, Priglinger SG, Eibl KH, Kampik A, Bloemendal H, Welge-Lussen U (2007) Hypoxia/reoxygenation and TGF-β increase αB-crystallin expression in human optic nerve head astrocytes. Exp Eye Res 84(4):694–706
Wu Q, Miao X, Zhang J, Xiang L, Li X, Bao X, Du S, Wang M, Miao S, Fan Y, Wang W, Xu X, Shen X, Yang D, Wang X, Fang Y, Hu L, Pan X, Dong H, Wang H, Wang Y, Li J, Huang Z (2021) Astrocytic YAP protects the optic nerve and retina in an experimental autoimmune encephalomyelitis model through TGF-β signaling. Theranostics 11(17):8480–8499
Cekanaviciute E, Dietrich HK, Axtell RC, Williams AM, Egusquiza R, Wai KM, Koshy AA, Buckwalter MS (2014) Astrocytic TGF-β signaling limits inflammation and reduces neuronal damage during central nervous system toxoplasma infection. J Immunol 193(1):139–149
Gugala Z, Olmsted-Davis EA, Xiong Y, Davis EL, Davis AR (2018) Trauma-induced heterotopic ossification regulates the blood-nerve barrier. Front Neurol 9:408
Ding W, Cai C, Zhu X, Wang J, Jiang Q (2022) Parthenolide ameliorates neurological deficits and neuroinflammation in mice with traumatic brain injury by suppressing STAT3/NF-kappaB and inflammasome activation. Int Immunopharmacol 108:108913
Sun X, Li X, Zhou Y, Wang Y, Liu X (2022) Exogenous TIPE2 inhibit TAK1 to improve inflammation and neuropathic pain induced by sciatic nerve injury through inactivating NF-kappaB and JNK. Neurochem Res 47(10):3167–3177
Genêt F, Kulina I, Vaquette C, Torossian F, Millard S, Pettit AR, Sims NA, Anginot A, Guerton B, Winkler IG, Barbier V, Lataillade JJ, Le Bousse-Kerdilès MC, Hutmacher DW, Levesque JP (2015) Neurological heterotopic ossification following spinal cord injury is triggered by macrophage-mediated inflammation in muscle. J Pathol 236(2):229–240
Brady RD, Shultz SR, McDonald SJ, O’Brien TJ (2018) Neurological heterotopic ossification: current understanding and future directions. Bone 109:35–42
Huang Y, Wang X, Zhou D, Zhou W, Dai F, Lin H (2021) Macrophages in heterotopic ossification: from mechanisms to therapy. Npj Regen Med. https://doi.org/10.1038/s41536-021-00178-4
Tirone M, Giovenzana A, Vallone A, Zordan P, Sormani M, Nicolosi PA, Meneveri R, Gigliotti CR, Spinelli AE, Bocciardi R, Ravazzolo R, Cifola I, Brunelli S (2019) Severe heterotopic ossification in the skeletal muscle and endothelial cells recruitment to chondrogenesis are enhanced by monocyte/macrophage depletion. Front Immunol. https://doi.org/10.3389/fimmu.2019.01640
Sorkin M, Huber AK, Hwang C, Carson WF, Menon R, Li J, Vasquez K, Pagani C, Patel N, Li S, Visser ND, Niknafs Y, Loder S, Scola M, Nycz D, Gallagher K, McCauley LK, Xu J, James AW, Agarwal S, Kunkel S, Mishina Y, Levi B (2020) Regulation of heterotopic ossification by monocytes in a mouse model of aberrant wound healing. Nat Commun. https://doi.org/10.1038/s41467-019-14172-4
Cutolo M, Campitiello R, Gotelli E, Soldano S (2022) The role of M1/M2 macrophage polarization in rheumatoid arthritis synovitis. Front Immunol. https://doi.org/10.3389/fimmu.2022.867260
Torossian F, Guerton B, Anginot A, Alexander KA, Desterke C, Soave S, Tseng HW, Arouche N, Boutin L, Kulina I, Salga M, Jose B, Pettit AR, Clay D, Rochet N, Vlachos E, Genet G, Debaud C, Denormandie P, Genet F, Sims NA, Banzet S, Levesque JP, Lataillade JJ, Le Bousse-Kerdilès M-C (2017) Macrophage-derived oncostatin M contributes to human and mouse neurogenic heterotopic ossifications. JCI Insight. https://doi.org/10.1172/jci.insight.96034
Wang L, Zhao R, Shi X, Wei T, Halloran BP, Clark DJ, Jacobs CR, Kingery WS (2009) Substance P stimulates bone marrow stromal cell osteogenic activity, osteoclast differentiation, and resorption activity in vitro. Bone 45(2):309–320
Xie K, Chen L, Yang J (2021) RNA sequencing evidences the prevention of oxidative stress is effective in injury-induced heterotopic ossification treatment. J Biomed Nanotechnol 17(2):196–204
Stegen S, Laperre K, Eelen G, Rinaldi G, Fraisl P, Torrekens S, Van Looveren R, Loopmans S, Bultynck G, Vinckier S, Meersman F, Maxwell PH, Rai J, Weis M, Eyre DR, Ghesquière B, Fendt SM, Carmeliet P, Carmeliet G (2019) HIF-1α metabolically controls collagen synthesis and modification in chondrocytes. Nature 565(7740):511–515
Fang CN, Tan HQ, Song AB, Jiang N, Liu QR, Song T (2022) NGF/TrkA promotes the vitality, migration and adhesion of bone marrow stromal cells in hypoxia by regulating the Nrf2 pathway. Metab Brain Dis 37(6):2017–2026
Li Z, Wu F, Xu D, Zhi Z, Xu G (2019) Inhibition of TREM1 reduces inflammation and oxidative stress after spinal cord injury (SCI) associated with HO-1 expressions. Biomed Pharmacother 109:2014–2021
Zheng G, Peng X, Zhang Y, Wang P, Xie Z, Li J, Liu W, Ye G, Lin Y, Li G, Liu H, Zeng C, Li L, Wu Y, Shen H (2023) A novel Anti-ROS osteoblast-specific delivery system for ankylosing spondylitis treatment via suppression of both inflammation and pathological new bone formation. J Nanobiotechnol 21(1):168
Li G, Deng Y, Li K, Liu Y, Wang L, Wu Z, Chen C, Zhang K, Yu B (2022) Hedgehog signalling contributes to trauma-induced tendon heterotopic ossification and regulates osteogenesis through antioxidant pathway in tendon-derived stem cells. Antioxidants (Basel) 11(11):2265
Yang J, Zhang X, Lu B, Mei J, Xu L, Zhang X, Su Z, Xu W, Fang S, Zhu C, Xu D, Zhu W (2023) Inflammation-responsive hydrogel spray for synergistic prevention of traumatic heterotopic ossification via dual-homeostatic modulation strategy. Adv Sci (Weinh). https://doi.org/10.1002/advs.202302905
Wang H, Lindborg C, Lounev V, Kim JH, McCarrick-Walmsley R, Xu M, Mangiavini L, Groppe JC, Shore EM, Schipani E, Kaplan FS, Pignolo RJ (2016) Cellular hypoxia promotes heterotopic ossification by amplifying BMP signaling. J Bone Miner Res 31(9):1652–1665
Agarwal S, Loder S, Brownley C, Cholok D, Mangiavini L, Li J, Breuler C, Sung HH, Li S, Ranganathan K, Peterson J, Tompkins R, Herndon D, Xiao W, Jumlongras D, Olsen BR, Davis TA, Mishina Y, Schipani E, Levi B (2015) Inhibition of Hif1α prevents both trauma-induced and genetic heterotopic ossification. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.1515397113
Sang X, Wang Z, Shi P, Li Y, Cheng L (2019) CGRP accelerates the pathogenesis of neurological heterotopic ossification following spinal cord injury. Artif Cells Nanomed Biotechnol 47(1):2569–2574
Acknowledgements
Draft of Fig. 1 was created with BioRender.com.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 82102600 and 82272485).
Author information
Authors and Affiliations
Contributions
DL mainly contributed to the topic determination, literature selection, and draft written, CL, HW, YL and YW screened detailed information from the literature and helped in the manuscript discussion. SS and SA approved the direction of the topic, revised the manuscript, and supervised the work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, D., Liu, C., Wang, H. et al. The Role of Neuromodulation and Potential Mechanism in Regulating Heterotopic Ossification. Neurochem Res 49, 1628–1642 (2024). https://doi.org/10.1007/s11064-024-04118-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-024-04118-8