Abstract
Background
Heterotopic ossification (HO) is the process of bone formation at a nonskeletal site. Recently, we showed that the earliest steps occur in sensory nerves. We now extend these studies by identifying unique osteogenic progenitors within the endoneurial compartment of sensory nerves.
Questions/purposes
We asked: (1) What is the nature of the osteoprogenitor in the endoneurium of peripheral nerves? (2) How do osteoprogenitors travel from the nerve to the site of new bone formation?
Methods
HO was induced by intramuscular injection of Ad5BMP-2-transduced cells in mice. Osteoprogenitors were identified through immunohistochemistry and then quantified and further characterized by fluorescence-activated cell sorting and immunocytochemistry. The kinetics of the appearance of markers of extravasation was determined by quantitative reverse transcription-polymerase chain reaction. In each experiment mice were injected with bone morphogenetic protein-2 (BMP-2)-producing cells (experimental) or with cells transduced with empty vector or, in some cases, a group receiving no injection (control).
Results
Induction of HO leads to the expression, within 24 hours, of osteoblast-specific transcription factors in cells in the endoneurium followed by their coordinate disappearance from the nerve at 48 hours. They reappear in blood also at 48 hours after induction. During vessel entrance they begin to express the tight junction molecule, claudin 5. The cells expressing both the osteoblast-specific transcription factor, osterix, as well as claudin 5, then disappear from circulation at approximately 3 to 4 days by extravasation into the site of new bone formation. These endoneurial osteoprogenitors express neural markers PDGFRα, musashi-1, and the low-affinity nerve growth factor receptor p75(NTR) as well as the endothelial marker Tie-2. In a key experiment, cells that were obtained from mice that were injected with cells transduced with an empty vector, at 2 days after injection, contained 0.83% (SD, 0.07; 95% confidence interval [CI], 0.59–1.05) cells expressing claudin 5. However, cells that were obtained from mice 2 days after injection of BMP-2-producing cells contained 4.5% cells expressing claudin 5 (SD, 0.72%; 95% CI, 2.01–6.94; p < 0.0015). Further analysis revealed that all of the cells expressing claudin 5 were found to be positive for osteoblast-specific markers, whereas cells not expressing claudin 5 were negative for these same markers.
Conclusions
The findings suggest that the endoneurial progenitors are the major osteogenic precursors that are used for HO. They exit the nerve through the endoneurial vessels, flow through vessels to the site of new bone formation, and then extravasate out of the vessels into this site.
Clinical Relevance
The biogenesis of osteoblasts in HO is very different than expected and shows that HO is, at least in part, a neurological disorder. This could result in a major shift in orthopaedic methodologies to prevent or treat this disease. The fact that nerves are intimately involved in the process may also provide clues that will lead to an explanation of the clinical fact that HO often occurs as a result of traumatic brain injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterotopic ossification (HO) is the formation of bone at nonskeletal sites as a result of a variety of causes including traumatic injury, orthopaedic surgical procedures (eg, hip replacement), joint disease, and burns. We previously demonstrated a link between peripheral nerves and HO in a murine model, which relies on sustained delivery of bone morphogenetic protein-2 (BMP-2) through injection of AdBMP-2-transduced cells into muscle [33]. Salisbury et al. [33] identified the immediate expression of the pain mediators, substance P and CGRP (calcitonin gene-related peptide), on delivery of the BMP-2, which leads to neural inflammation with resultant degranulation of local mast cells and remodeling of the epineurium of sensory nerves in the muscle near the injection site. Removal of the epineurium was correlated with migration of progenitors that reside in the perineurium that undergo brown adipogenesis [34], presumably for the purpose of patterning the new bone [27]. Blocking this process either through delivery of inhibitors of mast cell degranulation [33] or inhibitors of the binding of pain mediators to their receptor [13] resulted in a significant decrease in HO. Blocking nerve remodeling led to the accumulation within the endoneurium of nanog+ Klf-4+ osterix+ progenitors [33]. Osterix+ cells express the osteoblast-specific marker osterix [37] and therefore allow characterization of osteoprogenitors. The endoneurium contains the axons and their supporting glial cells, called Schwann cells, embedded in loose collagen fibrils within unique fascicles surrounded by multiple layers of perineurial cells [21, 44]. The endoneurium possesses a tight junction forming a microvascular barrier similar to that found in the brain that is identified by CD31 expression. CD31 is a predominant marker for the endothelial cells in the vessel. The blood-nerve barrier that is formed by endoneurial endothelial cells is critical in the control of the endoneurial microenvironment needed to maintain normal axonal signal transduction and is known as the blood-nerve barrier (BNB) [46]. An important protein, claudin 5, has been shown to be an essential component of restrictive microvascular barriers [3]. This protein is expressed at sites of cell-to-cell contact on human endoneurial endothelial cells in vitro [47]. Mice lacking expression of claudin 5 lack a functional blood-brain barrier (BBB) and die immediately after birth [24].
There has been a great deal of controversy regarding the exact nature of progenitors for the osteoblast during HO and the mechanism they use to travel to the site of bone formation. There have been publications suggesting that osteoprogenitors are derived from either mesenchymal stem cells in the bone marrow [29] or from the interstitial cells between the muscle fibers [45] or from fully differentiated endothelial cells [19], which then undergo an endothelial to mesenchymal transition [18]. It has also been suggested that the osteoprogenitors can be found in the circulation [39].
In this article we have therefore characterized the cells expressing osterix that reside in the nerve to determine the answers to two questions: (1) What is the nature of the osteoprogenitor in the endoneurium of peripheral nerves? (2) How do osteoprogenitors travel from the nerve to the site of new bone formation?
Materials and Methods
Study Design and Analysis
In this manuscript, studies were designed to evaluate in vivo the biogenesis of the osteoblasts used for HO. Because we are evaluating the formation of osteoprogenitors in response to BMP-2, analysis was mostly performed early (1–2 days) after induction. To accomplish this, studies were performed using groups of eight to 16 6-month-old, male C57BL/6 mice in which HO was induced by intramuscular injection of cells releasing physiological levels of BMP-2. Numbers of mice were determined by power analysis to be the minimal number for determining statistical significance between groups. Other groups of the same mice were used as controls and consisted of injection of cells transduced with a vector not containing BMP-2 cDNA (Ad Empty) as well as mice that were not injected. The analyses were conducted for all eight to 16 biological samples and the average and SDs calculated. For comparison of results between various groups, to determine their significance, analysis of variance (ANOVA) with Bonferroni-Holm post hoc correction for multiple comparisons was used. For all analysis, control groups were analyzed in parallel with experimental samples. For immunohistochemical and immunocytochemical analysis, antibody specificity was assessed by comparing the staining pattern of antibody with that of DAPI (4′,6-diamidino-2-phenylindole) at the optimal dilutions of primary and secondary antibodies. In all cases antibody specificity was judged excellent by these criteria.
Heterotopic Bone Formation
Replication defective adenovirus was used that contains cDNA for BMP-2 [28]. As a control we used Ad Empty that did not contain cDNA encoding BMP-2. The cells were transduced and 5 × 106 cells delivered by intramuscular injection into the hindlimb quadriceps muscle of C57BL/6 mice. Heterotopic bone is consistently observed near the injection site in approximately 7 days using this procedure.
Immunohistological and Immunocytochemical Analysis
Immunohistochemistry, immunocytochemistry, and cytospin analysis of cells isolated by fluorescence-activated cell sorting (FACS) was all performed as previously described [33]. For paraffin sections the entire hindlimb including the skeletal bone was harvested, the skin was removed, then the tissue was decalcified and paraffin-embedded. For frozen sections the soft tissue encompassing the site of the new bone formation was isolated from the rear hindlimbs and flash frozen. Serial sections (3–4 µm) were prepared with approximately 50 sections per tissue specimen. Hematoxylin and eosin staining was performed on every tenth slide to locate the region containing delivery cells or the newly forming bone. Serial unstained slides were used for immunohistochemical staining with either single or double antibody labeling. Primary antibodies were used at a dilution of 1:100 to 1:200 with overnight incubation, washed, and incubated with respective secondary antibodies of Alexa Fluor 488, 594, or 647 (Invitrogen Life Technologies, Bethesda, MD, USA) at a 1:500 dilution. Primary antibodies used were as follows: Claudin 5 (Novus Biological, Littleton, CO, USA), CD31 (Becton Dickson and Company, Franklin Lakes, NJ, USA), Neurofilament (NF) (Sigma-Aldrich, St Louis, MO, USA), osterix (OSX) (R & D Systems, Minneapolis, MN, USA), Tie-2 (Merck Millipore, Billerica, MA, USA), dlx 5 (Santa Cruz, Santa Cruz, CA, USA), CD44, E-selectin (CD62), myelin protein zero (MPZ), Musashi 1 (NRP-1), and nerve growth factor receptor (NGF [p75]; Abcam, Cambridge, MA, USA). Primary and secondary antibodies were diluted in 2% bovine serum albumin. When necessary, the mouse on mouse, MOM kit (Vector Laboratories, Burlingame, CA, USA), was used according to the manufacturer’s protocol for mouse antibodies. Tissues were counterstained and covered with Vectashield mounting medium containing DAPI (Vector Laboratories).
Cytospin slide preparations of FACS-isolated cells were produced by centrifugation of approximately 40,000 cells at 500 rpm using a Cytopro 7620 cytocentrifuge (Wescor, Logan, UT, USA) for 5 minutes. The slides were subsequently immunostained following similar methods as previously stated. Briefly, cells were fixed with 4% paraformaldehyde, washed with phosphate-buffered saline (PBS), treated with 0.3% Triton X-100 in Tris-buffered saline, blocked with 2% bovine serum albumin, and incubated in primary antibody overnight. After further PBS washing, samples were incubated in the appropriate secondary antibody and counterstained with DAPI. Stained cells were examined by confocal microscopy (LSM 510 META; Zeiss, Inc, Thornwood, NY, USA). Although immunohistochemistry results do not provide definitive proof that a single cell expresses two proteins, the cytospin method described does provide such proof. Dlx5 is an osteogenic factor that is expressed during development in the perichondrial region of both the embryonic axial and appendicular skeleton [31] and is thought to be upstream of osterix. It is activated by BMP-2 and upregulates both osterix [42] and osteocalcin [11] expression during osteogenesis.
Flow Cytometry and Fluorescence-activated Cell Sorting
Cells were isolated from the hindlimb soft tissues after removal of the skeletal bone and skin. Briefly, soft tissues were isolated from three mice (both legs pooled as one replicate), minced with scissors, and then subjected to 0.2% collagenase type II digestion at 37° C for 45 minutes. The digestion was stopped by adding an equal volume of DMEM (Dulbecco’s modified Eagle’s medium) containing 10% fetal bovine serum and cells collected by centrifugation at 400 × g for 5 minutes. Debris was removed by filtration through a 70-μm filter. Because claudin 5 is not only an important tight junction protein, but also has been found in blood after barrier disruption [14], mononuclear cells from blood were isolated and tested for the presence of claudin 5+ cells at various times after BMP-2 induction. For isolation of cells from peripheral blood, whole blood was layered onto Ficoll-Paque™ Plus (GE Healthcare, Princeton, NJ, USA) and spun according to the manufacturer’s instructions. The mononuclear cell band was removed and washed with PBS. Immunostaining was performed by incubating cells with claudin 5 antibody (Novus Biological, Littleton, CO, USA; 1:200 dilution) and/or PDGFRα antibody (Santa Cruz; 1:200 dilution) for 45 minutes on ice. Cells were washed with PBS and then incubated with antigoat Alexa Fluor 488 (Invitrogen; 1:500 dilution) for 30 minutes on ice. Cells were again washed with PBS and stained cells were analyzed on a FACSAria II (BD, Becton Dickinson, Franklin Lakes, NJ, USA) flow cytometer and BD FACSDiva software. For cell sorting, labeled cells were separated based on their fluorescence intensity and the claudin 5-negative and -positive populations were collected with > 95% purity. In this article, the populations are referred to as claudin 5+, meaning that claudin 5 is present in all cells, and claudin 5−, meaning that claudin 5 is absent in all cells. For experiments in which the percentage of positive cells was calculated versus time after BMP-2 induction, the FACS results from each time point were averaged, the SEM calculated, and statistical significance determined by ANOVA with Bonferroni-Holm post hoc correction for multiple comparisons.
Quantitative Reverse Transcription-Polymerase Chain Reaction (Real-Time Polymerase Chain Reaction)
To determine the concentration of factors known to be involved in extravasation, Ct values, which are directly related to the relative concentration of a specific RNA in the tissue, were collected. The Ct values were normalized to both internal 18S ribosomal RNA used in multiplexing and to each other to remove changes in gene expression common to both the control and BMP-2 tissues by using the method of ΔΔ Ct along with SYBR Green probes and quantitative polymerase chain reaction (PCR) primers. The analyses were conducted in triplicate for eight biological samples at each time point and were reported as the mean and SD of the fraction of RNA that was attributed to target cDNA. Significance for a change in the level of target RNA relative to the control was determined by the Student’s t-test comparing the control values with the values obtained in samples from mice injected with BMP-2-producing cells.
Results
Osteoblast Formation Begins in Nerves
BMP-2 Induces the Appearance of Osterix in p75+ Cells in the Endoneurium of Peripheral Nerves
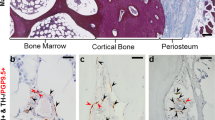
Previous studies [33] suggested that cells present in the endoneurial compartment of peripheral nerves express the osteogenic factor osterix after delivery of AdBMP-2-transduced cells. Therefore, tissues were isolated and immunostained on Days 1, 2, 4, and 7 after induction of HO through delivery of AdBMP-2-transduced cells. Surprisingly, there was osterix expression in cells in the endoneurium at 24 hours, but this rapidly disappeared within 24 hours as seen on tissues isolated 2 days after induction of HO (Fig. 1A). Two different primary antibodies represented by two different secondary antibodies were used to confirm this phenomenon and patterns of osterix expression appeared to be similar, independent of the antibody (Fig. 1A). To confirm the nerve structure, tissues were also immunostained for neurofilament H chain (NF). Two cell types are common within the endoneurial compartment of peripheral nerves, specialized vascular endothelial cells, and Schwann cells necessary for myelination of axons. Claudin 5 is a marker for the specialized endoneurial endothelial cells [41, 47]. Therefore, tissues were costained for osterix and claudin 5 (Fig. 1). Claudin 5 appears to be associated with vessels and the CD31+ vasculature is shown on a serial section (Fig. 1A). CD31 is a major component of vascular endothelial cells. Interestingly, the majority of the osterix+ cells did not appear to also express claudin 5 on Day 1, particularly those in the endoneurium. However, on both the first and second days after induction, some of the vessels within the endoneurium expressed both osterix and CD31 (yellow arrows, Fig. 1A), although it is not clear whether osteoprogenitors in these vessels coexpress these proteins. Examination of tissues isolated 4 and 7 days after BMP-2 induction (Fig. 1B) shows coexpression of osterix and claudin 5 in many cells throughout the muscle (eg, yellow arrow). Additionally, substantial vessel networks, as assessed by CD31 staining (CD31, red; original magnification, × 20, Fig. 1B), were observed in the region where the claudin 5+ osterix+ cells were localized, and these regions were found by Day 7 to be associated with bone matrix (Fig. 1B, red arrows).
(A) Osterix expression begins in the endoneurium of peripheral nerves. C57BL/6 mice (n = 8) were injected with BMP-2- producing cells and four mice each were euthanized on Days 1 and 2. Frozen sections were prepared and immunostained for neurofilament heavy chain (NF), CD31, or osterix. DAPI is blue. H and E sections were stained with hematoxylin and eosin (Stain, NF; original magnification, × 20; CD31; original magnification, × 20; osterix, original magnification, × 20). Some of the vessels within the endoneurium expressed both osterix and CD31 (yellow arrows). (B) Expression of osterix, claudin 5, and CD31 at later times after BMP-2 induction (Stain, osterix; original magnification, × 20; claudin 5; original magnification, × 20; CD31, original magnification, × 20). C57BL/6 mice (n = 16) were injected with BMP-2-producing cells and eight mice each were euthanized at either Day 4 or 7. Frozen sections were prepared and immunostained for CD31, claudin 5, or osterix (Stain, osterix; original magnification, × 20; claudin 5; original magnification, × 20; CD31, original magnification, × 20). Some of the vessels within the endoneurium expressed both osterix and CD31 (yellow arrows). Some of the vessels within the endoneurium expressed both osterix and CD31 (yellow arrows). H&E = hematoxylin and eosin.
Claudin 5+ Cells Express Osteogenic Markers After BMP-2 Induction
The majority of the claudin 5+ population first isolated by FACS followed by staining after centrifugation of these cells onto microscope slides also stained positively for not only claudin 5 (Fig. 2A), but also osterix (Fig. 2B). A merger of these two figures is also shown (Fig. 2C). In the claudin 5− population, cells were neither positive for claudin 5 (Fig. 2D) nor osterix (Fig. 2E), although there were many cells present (Fig. 2F). We next performed immunostaining to detect the expression of dlx5 on the claudin 5+ and − cell populations. Most cells positive for claudin 5 (Fig. 2G) also expressed dlx5 (Fig. 2H) although some of the cells were not positive for this factor (Fig. 2I); the claudin 5− population was completely negative for claudin 5 expression (Fig. 2J) as well as dlx5 expression (Fig. 2K), although there were many cells present (Fig. 2L).
Claudin 5-positive cells express osteogenic markers. The claudin 5+ population (green) was isolated from a FACS of cells isolated from muscle 4 days after BMP-2 induction. These isolated cells were subjected to cytospin and the slides were then probed with antibodies for claudin 5 (green) and osterix (red). (A–C) One field obtained from the claudin 5+ population with C being the merger of A and B; (D–F) one field of the cytospin of a claudin 5− population obtained from the same mouse that was stained with antibodies against claudin 5 (green) and osterix (red) as well as DAPI (F). In the claudin 5+ cell population, osterix-positive cells were found to be 75% ± 3%. In G-I and J-L, respectively, we show the cytospin patterns of the claudin 5-positive and -negative populations of another mouse after staining for claudin 5 (green) and dlx 5 (red).
Claudin 5+ Cells Express Factors Associated With Nerve Stem/Progenitor Cells
Claudin 5+ cells were further characterized for the expression of two additional neural stem or progenitor cell markers, PDGFRα and musashi. Both PDGFRα, a factor associated with perivascular astrocytes [38] and shown to be involved in glial-endothelial cell interactions and critical for maintenance of the BBB [38], and musashi, which is an RNA-binding protein that is highly specific for neural stem cells [23] and is not expressed in fully differentiated cells [26], were assessed in the claudin 5+ cells. FACS analysis showed that PDGFRα was expressed on these cells (Fig. 3A). Analysis of the cells showed the absence of a claudin 5+ PDGFRα− population, although we did observe a small PDGFRα+ claudin 5− population (Fig. 3A) that may represent Schwann cells, which previously have been shown to be positive for this receptor [8].
(A) Analysis of the expression of PDGFRα in claudin 5-positive cells. C57BL/6 mice (n = 8) were injected with BMP-2-producing cells or cells transduced with empty vector (n = 8, control). After 4 days the mice were euthanized and cells from the muscle around the site of injection were isolated, reacted with an antibody against claudin 5 tagged with Alexa fluor 488 (green), mixed with an antibody against PDGFRα tagged with Alexa fluor 595 (red), and the cells subjected to FACS analysis. The percentage of the total cells in each gate (PDGFRα expression only, claudin 5 expression only, and both PDGFRα and claudin 5 expression) was determined. The mean is plotted on the chart and error bars are the SD. (B) Expression of musashi 1 in claudin 5-positive cells. C57BL/6 mice (n = 8) were either injected in the quadriceps with BMP-2-producing cells. The results for two of these mice are shown in B. After 4 days mice were euthanized, the cells isolated from muscle, reacted with an antibody against claudin 5 tagged with Alexa fluor 488 (green), and subjected to FACS. The claudin 5-positive (A-C and G-I) and claudin 5-negative (D-F and J-L) populations were isolated from both mice, subjected to cytospin, and the resultant slides stained with DAPI (blue) and tagged antibodies to claudin 5 (green) and to musashi 1 (red).
Again claudin 5+ and − populations isolated from tissues 2 days after delivery of the AdBMP-2-transduced cells were isolated and immunostained for musashi. The results from two mice injected with BMP-2-producing cells are shown (Fig. 3B; panels A-F showing results from the first and panels G-L showing results from the second animal). The claudin 5+ populations (Fig. 3B, panels A and G) stained positively for claudin 5 (Fig. 3B, panels B and H) and most of those cells were also positive for musashi (Fig. 3B, panels C and I). However, although there was an approximately equal number of cells present in the claudin 5− populations (Fig. 3B, panels D and J), these cells did not stain positively for neither claudin 5 (Fig. 3B, panels E and K) or musashi (Fig. 3B, panels F and L), with the exception of a few cells staining positively for musashi in the first mouse (Fig. 3B, panel F).
Claudin 5+ Cells Express the Endothelial Marker Tie-2
Because others have reported the presence of PDGFRα on the surface of an osteoprogenitor expressing Tie-2 [45], the claudin 5+ and − populations were immunostained for Tie-2 (Fig. 4A). Almost all of the claudin 5+ cells were found to express Tie-2, but there appeared to be a wide variation in its expression level, whereas only a few cells in the claudin 5− population were positive for either claudin 5 or Tie-2. We noted asymmetric localization of Tie-2 within the cell (Fig. 4B).
(A) Osteoprogenitors express the endothelial marker Tie-2. C57/BL6 mice were injected with BMP-2-producing cells (n = 4) and 4 days after induction, the mice were euthanized and the cells harvested from the muscle around the site of injection were separated by FACS into claudin 5-positive and -negative populations. The populations were subjected to cytospin and the slides were assessed for expression of Tie-2 (red). Claudin 5 = green; DAPI = blue. Arrows indicate cells that co-express Claudin 5 (green arrows) and Tie 2 (red arrows). Yellow arrows are shown in the merger. (B) This is a photomicrograph × 40 magnification showing an asymmetric distribution of Tie-2 (red) in some of the cells.
Osteoprogenitors Do Not Express Markers of Differentiated Schwann Cells
Schwann cells express elevated levels of p75 (NTR) during peripheral nerve regeneration and myelination [4], but neural crest stem cells also express p75 (NTR) [22]. To distinguish Schwann cells from neural progenitors, tissues isolated 2 and 6 days after induction of HO were coimmunostained with osterix and either p75 (NTR) or MPZ (Fig. 5). Osterix and p75 were coexpressed within the endoneurium (Fig. 5). MPZ+ cells were also observed in this region of the nerve; however, these cells did not express osterix (Fig. 5).
Osteoprogenitors for HO are not derived from dedifferentiating Schwann cells. Osteoprogenitors in peripheral nerves were assessed at early (1 day) and late (6 days) times after BMP-2 induction by analyzing frozen serial sections of C57BL/6 mice (n = 4 per group) euthanized either 1 or 6 days after BMP-2 induction. Sections were analyzed by immunohistochemistry simultaneously for either p75 (NTR) and osterix or MPZ and osterix (Stain, p75 [NTR]; original magnification, × 20; osterix; original magnification, × 20; MPZ, original magnification, × 20). The second panel of the osterix and MPZ stain on Day 1 is at an original magnification of × 40. The yellow arrow in the panel showing a merger of p75NTR (red) and osterix (green) on the first day after BMP2 induction indicates cells co-expressing these two markers.
Osteoblast Precursors Migrate Through Vessels
Claudin 5+ Osteoprogenitors Enter the General Circulation Shortly After BMP-2 Induction
Osterix expression was present on the endoneurial cells for only 24 hours after which time we did not observe expression in the nerve (Fig. 1A). This suggests that either expression is downregulated or that these cells immediately exit the nerve. One of the only ways for cells to exit the endoneurium of the nerve is through the highly regulated BNB formed by tight and adheren junctions between endoneurial endothelial cells lining the endoneurial vessels. The actual FACS data on Day 2 for mice injected with Ad Empty-transduced cells is shown (Fig. 6A); on Day 2 for uninjected mice (Fig. 6B); and on days 1 (Fig. 6C), 2 (Fig. 6D), and 4 (Fig. 6E) for mice injected with BMP-2-producing cells. The overall results obtained using mononuclear cells isolated from blood, as described in the Materials and Methods, show that 1.37% (range, 1.1%-2.14%; 95% confidence interval [CI], -0.25 to 2.99) of the cells were positive for claudin 5 1 day after induction of bone formation (Fig. 6A). This percentage was not different from the control value of 0.83 % (SD, 0.07; 95% CI, 0.59–1.05) when injected cells were transduced with Ad Empty. Interestingly, the percentage of claudin 5+ cells increased dramatically 2 days after the induction with 4.48% of the cells (SD, 0.72%; 95% CI, 2.01–6.94; p < 0.0015) now positive for this marker (Fig. 6A, panel E). However, the increase in cells expressing claudin 5 in blood was short-lived and returned to background levels with a value of 1.39% of positive cells (SD, 0.20%; 95% CI, 0.7–2.08) 4 days after BMP-2 induction (Fig. 6A, panel E).
(A) Cells expressing claudin 5 increase in blood after BMP-2 induction. C57/BL6 mice (n = 4 per group) were injected either with cells transduced with Ad Empty (control) or were injected with BMP-2-producing cells. Another group of mice (n = 4) remained uninjected. Mice were bled by cardiac puncture at 0 (untreated), 1, 2, and 4 days after induction. Mononuclear cells were collected, reacted with an antibody to claudin 5, and subjected to FACS analysis. (Panel A) FACS analysis of blood taken at Day 2 from mice injected with cells transduced with empty vector (Q2 is the gate for claudin 5-positive cells); (Panel B) FACS analysis of blood taken from uninjected mice; (Panel C) FACS analysis of blood taken at Day 1 from mice injected with BMP-2-producing cells; (Panel D) FACS analysis of blood taken at Day 2 from mice injected with BMP-2-producing cells; (Panel E) FACS analysis of blood taken at Day 4 from mice injected with BMP-2-producing cells. (Panel F) Bar chart of the overall results. The values on the chart are the mean of the percentage of claudin 5-positive cells present in blood at the respective days. The error bars are the SD. Descriptive statistics were used to analyze the study results with the control being injection of cells transduced with Ad Empty. The sample size in the groups was n = 3. The ANOVA with Bonferroni-Holm post hoc correction for multiple comparisons was used to detect statistically significant differences between the number of claudin 5+ cells present in the circulation at given time points after intramuscular injection of BMP-2-producing cells. (B) Claudin 5-positive cells isolated from blood cells express osteogenic markers. The claudin 5+ population (green) was isolated from a FACS of cells isolated from muscle 4 days after BMP-2 induction. These isolated cells were subjected to cytospin and the slides were stained with DAPI (A) and then probed with antibodies for osterix (red, B) and claudin 5 (green, C). A cytospin analysis of a claudin 5− population obtained from the same mouse showing DAPI (D) and after staining with antibodies against osterix (red, E) claudin 5 (green, F).
To confirm that these circulating claudin 5+ cells were expressing osterix, both positive and negative populations were isolated by FACS followed by cytospin and immunostaining for osterix. All of the osterix expression was found to be in the claudin 5+ cells (Fig. 6B).
Osteoprogenitors Extravasate Across the Vessel Wall When They Reach the Area of Bone Formation
To determine if the process of extravasation [30] is involved in the migration of the claudin 5+ osterix+ cells through the vessel wall and to the site of bone formation, RNA was isolated from muscle at daily intervals for 7 days after BMP-2 induction and the levels of RNA specific for known extravasation factors (CXCR4, CD44, SDF, and P and E-selectin) were quantified through quantitative reverse transcription-PCR (Fig. 7A). The results show an increase in E-selectin (Fig. 7A, panel A), CXCR4 (Fig. 7A, panel B), and CD44 (Fig. 7A, panel C) RNAs starting 4 days after induction of HO that was maintained for the remainder of bone formation (Fig. 7A), whereas SDF and P-selectin did not show a change (data not shown). As confirmation, claudin 5+ and − cells were isolated from the tissues, spun onto slides that were then immunostained for a factor present on the endothelial cells (E-selectin) as well as factors present on the extravasating cell (CD44 and CXCR4). As expected, the claudin 5+ population expressed CD44 and CXCR4, whereas the negative population expressed E-selectin (Fig. 7B).
(A) CD44, CXCR4, and E-selectin are expressed on BMP-2 induction. C57/BL6 mice were injected with BMP-2-producing cells (n = 8 per group) and at the times indicated mice were euthanized, RNA extracted from muscle around the site of injection, and the relative amounts of RNA encoding E-selectin at the times indicated are shown in A, CXCR4 is shown in B, and CD44 is shown in C. The actual data for each sample are adjacent to each panel including the mean, SD, mean difference with 95% CIs. The p values for significant differences are shown in the graph and the error bars in the graphs are the SD. The thresholds for statistically significant differences were set at p < 0.05. (B) Claudin 5+ cells express CD44 and CXCR4, whereas claudin 5− cells express E-selectin. C57BL/6 mice (n = 4 per group) were injected with BMP-2-producing cells and mice were euthanized 4 days later. Claudin 5+ and claudin 5− cells were isolated by preparative FACS, subjected to cytospin, and the resulting slides analyzed for staining for CD44, E-selectin, and CXCR4.
Discussion
The studies described in this article were designed to address the controversy surrounding the origin of osteoprogenitors during HO. It has been published previously that they may arise from bone marrow cells [12], endothelial cells [19], or muscle stem cells [45]. In answer to the questions posed by us in these studies: (1) yes, osteoprogenitors are derived from progenitors in the endoneurium of peripheral nerves. Osteoprogenitors most likely do not arise from Schwann cells, despite publications that Schwann cells dedifferentiate [35]. The results suggest that the progenitor is either a nonmyelinating Schwann cell or a neural crest stem cell as was previously suggested by Morrison et al. [22]. Although the progenitor cells bear an endothelial marker (Tie-2), they also simultaneously express several neural markers and are therefore not endothelial cells. (2) Finally, as to how the osteoprogenitors migrate from the nerve to the site of new bone formation, the data collectively suggest that neural progenitors within the endoneurium of peripheral nerves can cross into the endoneurial vessels and enter the circulation to the site of new bone formation undergoing at least partial osteogenic differentiation during this transit. Many recent studies suggest that osteoprogenitors are local progenitors, either recruited from vasculature or from interstitial spaces between muscle fibers [19]. Our data actually support not only a circulating progenitor, but also a local progenitor, because the cells engraft several days before the appearance of cartilage or bone. Therefore, these fibroblast-like cells deposited from the circulation between the muscle fibers would appear to be local cells.
There are several limitations in the current studies. First, the results suggest that osteoprogenitors outside the nerve express claudin 5; however, the osterix+ cells in the endoneurium 24 hours after delivery of BMP-2 do not appear to express claudin 5. The reason for expression of claudin 5 by these osteoprogenitors is not clear. It has been shown that cells expressing claudin 5 have not only increased adherence, but also increased motility [9] consistent with the ability of these osteoprogenitors to circulate. Interestingly, endothelial progenitors have previously been shown to leave the vessel wall and circulate [2] suggesting that the osterix+ claudin 5+ p75+ cells may function similarly to these endothelial progenitors.
The second limitation of this study is that, although consistent with the presence of a neural stem cell that resides in adult peripheral nerves, it does not prove this point. We speculate that in the adult nerve, as has been shown for other tissues, regeneration of tissue does not solely depend on a pluripotent stem cell, but rather on progenitor cells stored, often in discrete depots, at various stages of differentiation. Also it is possible that BMP-2 induction of bone formation in the adult is, at least in part, a recapitulation of embryonic bone formation. The formation of craniofacial bone and cartilage in the embryo begins with neural crest stem cell migration from the neural tube [20]. One of the key factors that indicates the start of osteogenesis in these cells is the expression of dlx5 and osterix, similar to the early osteogenic factors on the osterix+ claudin 5+ p75+ progenitors. The synthesis of osteoblasts from neural crest stem cells uses a combination of Wnt and BMP signaling. Although Wnt 1 is the major inducer of neural crest [10], when it is unopposed, Wnt 1 signaling leads to the production of sensory nerves from neural stem cells [17]. However, when opposed by BMP-2, Wnt 1 signaling in neural crest stem cells leads to other cell types including osteoprogenitors [15]. Thus, the biogenesis of osteoprogenitors in the adult may ultimately originate from neural stem cells housed in the endoneurium. It is conceivable that these cells may have been deposited within the endoneurium during neural crest migration and formation of sensory nerves. Perhaps neural crest stem cells are deposited in all neural crest tissues, because several reports suggest a Wnt1+ neural crest stem cell in the head [16]. Alternatively, these cells may simply persist in the endoneurium because it is an immune privileged location, because it is behind the BNB. Such a mechanism would also allow tissue regeneration using a recapitulation of an embryonic process although early embryonic antigens may not be recognized as self by the adult immune system.
Our results suggest that osteoprogenitors are osterix-expressing cells residing in the endoneurium and are not Schwann cells; further phenotypic characterization of the osteoprogenitors shows expression of Tie-2, a marker of endothelial cells. The presence of endothelial markers on osteoprogenitors has also recently been described by others [5]. Additionally, we noted that in some cases, Tie-2 had a surprisingly asymmetric localization on cells, which may indicate a migrating rather than matrix-bound cell, as described by Saharinen et al. [32]. Additionally, these cells express musashi and p75 that are phenotypic markers of neural crest stem cells [23]. In addition to these neural crest markers, the cells also express PDGFRα, a factor involved in glial-endothelial cell interactions and critical for maintenance of the BBB, suggesting that endothelial-neural cell interaction may play a key role in transition of these progenitors from a neural to mesodermal fate.
The results described in this article also answer the question of the mechanism by which osteoprogenitors exit the nerve and migrate to the site of bone formation. They show the presence of osterix+ cells in the endoneurium of peripheral nerves immediately after HO induction through delivery of AdBMP-2-transduced cells; however, these cells then disappear at the same time as the appearance of osterix+ claudin 5+ cells in the circulation. Within 4 days after induction of HO, they disappear from the bloodstream with a simultaneous increase in expression of factors involved in cell extravasation and the appearance of the osterix+ claudin 5+ cells in muscle at the site of HO. The data suggest that these osteoprogenitors exit the nerve through the BNB, enter the circulation, and home to the site of HO. However, how these cells cross the BNB and whether the barrier is compromised during their transit is unknown and is a shortcoming of these studies.
New vessels appear to be formed to carry these osteoprogenitors. We previously showed the rapid expansion of new vessels after delivery of the AdBMP-2-transduced cells [7] and in the current study, an extensive vascular plexus can be seen surrounding the claudin 5+ osterix+ cells. Furthermore, at the same time, extravasation factors (CXCR4, CD44, and E-selectin) were significantly elevated in these tissues consistent with the appearance, through the circulation, of the cells at this site. It has been previously shown that CD44 is a key mediator of the transendothelial migration of many cell types and mediates the binding of CD44 to hyaluronic acid on the endothelial cell [6]. Therefore, CD44, which is expressed on the surface of the osteoprogenitor, likely binds to the E-selectin on the surface of the endothelial cells. This is the first step of extravasation. Additionally, the cells appear to express CXCR4, which is also significantly elevated in the tissues at this time; CXCR4 has been shown to bind SDF 1 on endothelial cells, as the second step in extravasation, which allows for tighter binding and eventually migration through pores between the endothelial cells [25]. SDF 1 RNA within the tissues did not change significantly during HO; however, it was present in the tissues (data not shown). Additionally, the new vessels that are rapidly forming at this site are tiny, with significant branches, suggesting lower flow, necessary for depositing cells. Finally, new vessels or venules must undergo remodeling to organize the structure and support greater blood flow without leaking [43]. Thus, it is highly likely at this stage for cells to traverse the vessel wall more easily than in mature vessels. We therefore propose that the exact location of extravasation of the osteoprogenitors is determined by induction of HIF1 in tBAT [27] because of the ability of UCP1 to rapidly generate a hypoxic microenvironment [27]. This process induces vascular endothelial growth factor [7], which then induces new vessel formation. These new vessels are actually the small venules that are required for extravasation [43].
The current study also underscores the importance of barriers or interfaces between blood and nerves in HO and perhaps begins to explain some of the surprising clinical data in HO. Two molecules that show a dramatic increase on BMP-2 induction of HO, claudin 5 and PDGFRα, are either a key component or regulator, respectively, of these barriers. Recently it has become very obvious that there is a relationship between traumatic brain injury and HO [1, 40]. One possible reason that HO is associated with traumatic brain injury, which causes a breakdown in the BBB [36, 40], could be that changes in this barrier lead to the exit of these neural progenitors that can engraft and become osteoblasts, particularly at sites where BMP-2 may be present such as those that have also sustained an injury to bone, thus releasing BMP-2.
Furthermore, if this is a recapitulation of neural crest formation of the bones and cartilage of the head, then presumably this is not endochondral bone formation but rather two independent processes. Thus, it may not be surprising that these osteogenic cells appear in a location distinct from the cartilage and arrive before its formation. In conclusion, these studies are the first to demonstrate the presence of a progenitor within peripheral nerves that responds to BMP-2 by undergoing both osteogenic differentiation and homing to the location of bone formation through vessels. The conclusions are clinically relevant because the mechanism is very different than that predicted from the current thinking about the formation of bone. Future studies on this mechanism are already underway and include the use of tracking mice based on an inducible early neural promoter (Wnt 1) driving Cre recombinase, enabling expression of a permanent fluorescent marker in each cell derived from the neural stem cell. Preliminary data from these experiments confirm the results reported here and show dramatically fluorescent peripheral nerves at early times after BMP-2 induction as well as the accumulation of equally dramatic fluorescent osteoblasts on the bone surface at later times after induction.
References
Alfieri KA, Forsberg JA, Potter BK. Blast injuries and heterotopic ossification. Bone Joint Res. 2012;1:192–197.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967.
Campbell M, Hanrahan F, Gobbo OL, Kelly ME, Kiang AS, Humphries MM, Nguyen AT, Ozaki E, Keaney J, Blau CW, Kerskens CM, Cahalan SD, Callanan JJ, Wallace E, Grant GA, Doherty CP, Humphries P. Targeted suppression of claudin-5 decreases cerebral oedema and improves cognitive outcome following traumatic brain injury. Nat Commun. 2012;3:849.
Cosgaya JM, Chan JR, Shooter EM. The neurotrophin receptor p75NTR as a positive modulator of myelination. Science. 2002;298:1245–1248.
Decker B, Bartels H, Decker S. Relationships between endothelial cells, pericytes, and osteoblasts during bone formation in the sheep femur following implantation of tricalciumphosphate-ceramic. Anat Rec. 1995;242:310–320.
DeGrendele HC, Estess P, Picker LJ, Siegelman MH. CD44 and its ligand hyaluronate mediate rolling under physiologic flow: a novel lymphocyte-endothelial cell primary adhesion pathway. J Exp Med. 1996;183:1119–1130.
Dilling CF, Wada AM, Lazard ZW, Salisbury EA, Gannon FH, Vadakkan TJ, Gao L, Hirschi K, Dickinson ME, Davis AR, Olmsted-Davis EA. Vessel formation is induced prior to the appearance of cartilage in BMP-2-mediated heterotopic ossification. J Bone Miner Res. 2010;25:1147–1156.
Eccleston PA, Funa K, Heldin CH. Expression of platelet-derived growth factor (PDGF) and PDGF alpha- and beta-receptors in the peripheral nervous system: an analysis of sciatic nerve and dorsal root ganglia. Dev Biol. 1993;155:459–470.
Escudero-Esparza A, Jiang WG, Martin TA. Claudin-5 is involved in breast cancer cell motility through the N-WASP and ROCK signalling pathways. J Exp Clin Cancer Res. 2012;31:43.
Garcia-Castro MI, Marcelle C, Bronner-Fraser M. Ectodermal Wnt function as a neural crest inducer. Science. 2002;297:848–851.
Hassan MQ, Javed A, Morasso MI, Karlin J, Montecino M, van Wijnen AJ, Stein GS, Stein JL, Lian JB. Dlx3 transcriptional regulation of osteoblast differentiation: temporal recruitment of Msx2, Dlx3, and Dlx5 homeodomain proteins to chromatin of the osteocalcin gene. Mol Cell Biol. 2004;24:9248–9261.
Jung Y, Song J, Shiozawa Y, Wang J, Wang Z, Williams B, Havens A, Schneider A, Ge C, Franceschi RT, McCauley LK, Krebsbach PH, Taichman RS. Hematopoietic stem cells regulate mesenchymal stromal cell induction into osteoblasts thereby participating in the formation of the stem cell niche. Stem Cells. 2008;26:2042–2051.
Kan L, Lounev VY, Pignolo RJ, Duan L, Liu Y, Stock SR, McGuire TL, Lu B, Gerard NP, Shore EM, Kaplan FS, Kessler JA. Substance P signaling mediates BMP-dependent heterotopic ossification. J Cell Biochem. 2011;112:2759–2772.
Kazmierski R, Michalak S, Wencel-Warot A, Nowinski WL. Serum tight-junction proteins predict hemorrhagic transformation in ischemic stroke patients. Neurology. 2012;79:1677–1685.
Kleber M, Lee HY, Wurdak H, Buchstaller J, Riccomagno MM, Ittner LM, Suter U, Epstein DJ, Sommer L. Neural crest stem cell maintenance by combinatorial Wnt and BMP signaling. J Cell Biol. 2005;169:309–320.
Kurosaka S, Leu NA, Zhang F, Bunte R, Saha S, Wang J, Guo C, He W, Kashina A. Arginylation-dependent neural crest cell migration is essential for mouse development. PLoS Genet. 2010;6:e1000878.
Lee HY, Kleber M, Hari L, Brault V, Suter U, Taketo MM, Kemler R, Sommer L. Instructive role of Wnt/beta-catenin in sensory fate specification in neural crest stem cells. Science. 2004;303:1020–1023.
Medici D, Olsen BR. The role of endothelial-mesenchymal transition in heterotopic ossification. J Bone Miner Res. 2012;27:1619–1622.
Medici D, Shore EM, Lounev VY, Kaplan FS, Kalluri R, Olsen BR. Conversion of vascular endothelial cells into multipotent stem-like cells. Nat Med. 2010;16:1400–1406.
Mishina Y, Snider TN. Neural crest cell signaling pathways critical to cranial bone development and pathology. Exp Cell Res. 2014;325:138–147.
Mizisin AP, Weerasuriya A. Homeostatic regulation of the endoneurial microenvironment during development, aging and in response to trauma, disease and toxic insult. Acta Neuropathol. 2011;121:291–312.
Morrison SJ, White PM, Zock C, Anderson DJ. Prospective identification, isolation by flow cytometry, and in vivo self-renewal of multipotent mammalian neural crest stem cells. Cell. 1999;96:737–749.
Nakamura M, Okano H, Blendy JA, Montell C. Musashi, a neural RNA-binding protein required for Drosophila adult external sensory organ development. Neuron. 1994;13:67–81.
Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N, Furuse M, Tsukita S. Size-selective loosening of the blood-brain barrier in claudin-5-deficient mice. J Cell Biol. 2003;161:653–660.
Oberlin E, Amara A, Bachelerie F, Bessia C, Virelizier JL, Arenzana-Seisdedos F, Schwartz O, Heard JM, Clark-Lewis I, Legler DF, Loetscher M, Baggiolini M, Moser B. The CXC chemokine SDF-1 is the ligand for LESTR/fusin and prevents infection by T-cell-line-adapted HIV-1. Nature. 1996;382:833–835.
Okano H, Kawahara H, Toriya M, Nakao K, Shibata S, Imai T. Function of RNA-binding protein Musashi-1 in stem cells. Exp Cell Res. 2005;306:349–356.
Olmsted-Davis E, Gannon FH, Ozen M, Ittmann MM, Gugala Z, Hipp JA, Moran KM, Fouletier-Dilling CM, Schumara-Martin S, Lindsey RW, Heggeness MH, Brenner MK, Davis AR. Hypoxic adipocytes pattern early heterotopic bone formation. Am J Pathol. 2007;170:620–632.
Olmsted-Davis EA, Gugala Z, Gannon FH, Yotnda P, McAlhany RE, Lindsey RW, Davis AR. Use of a chimeric adenovirus vector enhances BMP2 production and bone formation. Hum Gene Ther. 2002;13:1337–1347.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147.
Rampon C, Weiss N, Deboux C, Chaverot N, Miller F, Buchet D, Tricoire-Leignel H, Cazaubon S, Baron-Van Evercooren A, Couraud PO. Molecular mechanism of systemic delivery of neural precursor cells to the brain: assembly of brain endothelial apical cups and control of transmigration by CD44. Stem Cells. 2008;26:1673–1682.
Robledo RF, Rajan L, Li X, Lufkin T. The Dlx5 and Dlx6 homeobox genes are essential for craniofacial, axial, and appendicular skeletal development. Genes Dev. 2002;16:1089–1101.
Saharinen P, Eklund L, Miettinen J, Wirkkala R, Anisimov A, Winderlich M, Nottebaum A, Vestweber D, Deutsch U, Koh GY, Olsen BR, Alitalo K. Angiopoietins assemble distinct Tie2 signalling complexes in endothelial cell-cell and cell-matrix contacts. Nat Cell Biol. 2008;10:527–537.
Salisbury E, Rodenberg E, Sonnet C, Hipp J, Gannon FH, Vadakkan TJ, Dickinson ME, Olmsted-Davis EA, Davis AR. Sensory nerve induced inflammation contributes to heterotopic ossification. J Cell Biochem. 2011;112:2748–2758.
Salisbury EA, Lazard ZW, Ubogu EE, Davis AR, Olmsted-Davis EA. Transient brown adipocyte-like cells derive from peripheral nerve progenitors in response to bone morphogenetic protein 2. Stem Cells Transl Med. 2012;1:874–885.
Salzer JL. Switching myelination on and off. J Cell Biol. 2008;181:575–577.
Shlosberg D, Benifla M, Kaufer D, Friedman A. Blood-brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol. 2010;6:393–403.
Sinha KM, Zhou X. Genetic and molecular control of osterix in skeletal formation. J Cell Biochem. 2013;114:975–984.
Su EJ, Fredriksson L, Geyer M, Folestad E, Cale J, Andrae J, Gao Y, Pietras K, Mann K, Yepes M, Strickland DK, Betsholtz C, Eriksson U, Lawrence DA. Activation of PDGF-CC by tissue plasminogen activator impairs blood-brain barrier integrity during ischemic stroke. Nat Med. 2008;14:731–737.
Suda RK, Billings PC, Egan KP, Kim JH, McCarrick-Walmsley R, Glaser DL, Porter DL, Shore EM, Pignolo RJ. Circulating osteogenic precursor cells in heterotopic bone formation. Stem Cells. 2009;27:2209–2219.
Sullivan MP, Torres SJ, Mehta S, Ahn J. Heterotopic ossification after central nervous system trauma: a current review. Bone Joint Res. 2013;2:51–57.
Ubogu EE. The molecular and biophysical characterization of the human blood-nerve barrier: current concepts. J Vasc Res. 2013;50:289–303.
Ulsamer A, Ortuno MJ, Ruiz S, Susperregui AR, Osses N, Rosa JL, Ventura F. BMP-2 induces osterix expression through up-regulation of Dlx5 and its phosphorylation by p38. J Biol Chem. 2008;283:3816–3826.
Wagner DD, Frenette PS. The vessel wall and its interactions. Blood. 2008;111:5271–5281.
Weerasuriya A, Mizisin AP. The blood-nerve barrier: structure and functional significance. Methods Mol Biol. 2011;686:149–173.
Wosczyna MN, Biswas AA, Cogswell CA, Goldhamer DJ. Multipotent progenitors resident in the skeletal muscle interstitium exhibit robust BMP-dependent osteogenic activity and mediate heterotopic ossification. J Bone Miner Res. 2012;27:1004–1017.
Yosef N, Ubogu EE. An immortalized human blood-nerve barrier endothelial cell line for in vitro permeability studies. Cell Mol Neurobiol. 2013;33:175–186.
Yosef N, Xia RH, Ubogu EE. Development and characterization of a novel human in vitro blood-nerve barrier model using primary endoneurial endothelial cells. J Neuropathol Exp Neurol. 2010;69:82–97.
Acknowledgments
We thank Rita Nistal for preparation of tissues for histology and Joel Sederstrom of the Baylor College of Medicine Flow Cytometry and Cell Sorting Core for assistance with FACS.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by grants from the Department of Defense (DAMD W81XWH-12-1-0274, “Diagnosis and Treatment of Heterotopic Ossification”) and the National Institutes of Health (NIH), National Institute of Arthritis and Musculoskeletal and Skin Diseases (R21AR061638, “Heterotopic Bone from Stem Cells in Nerve”; R21AR063779, “Function of Brown Adipose in Bone Formation”; R01AR066556, “Neural Mechanisms in Heterotopic Ossification”). One of the authors (EAS) was supported by a postdoctoral fellowship (NIH NIGMS K12 GM084897). The institutions of one or more of the authors (EAO-D, EEU, ARD) have received, during the study period, funding from the NIH and the Department of Defense.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution, with the exception of The University of Alabama at Birmingham and the University of Texas Medical Branch in which no animal experiments were performed, approved the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Baylor College of Medicine, Houston, TX, USA.
About this article
Cite this article
Lazard, Z.W., Olmsted-Davis, E.A., Salisbury, E.A. et al. Osteoblasts Have a Neural Origin in Heterotopic Ossification. Clin Orthop Relat Res 473, 2790–2806 (2015). https://doi.org/10.1007/s11999-015-4323-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4323-9