Abstract
This manuscript aspires to portray a review of the current literature focusing on manifest peritoneal metastasis (PM) derived from gastric cancer and its treatment options. Despite the development of chemotherapy and multimodal treatment options during the last decades, mortality remains high worldwide. After refreshing important epidemiological considerations, the molecular mechanisms currently accepted through which PM occurs are revised. Palliative chemotherapy is the only recommended treatment option for patients with PM of gastric cancer according to the National Comprehensive Cancer Network guidelines, although cytoreductive surgery in combination with hyperthermic intraperitoneal chemotherapy demonstrated promising results in selected patients with regional PM and localized intraabdominal tumor spread. A novel treatment named pressurized intraperitoneal aerosol chemotherapy may have a promising future in improving overall survival with an acceptable postoperative complication rate and stabilizing quality of life during treatment. Additionally, the procedure has been proved to be safe for the patient and medical personnel and a feasible, repeatable method to deter metastatic proliferation. This overview comprehensively addresses this novel and promising treatment in the context of a scientifically and clinically challenging disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer currently holds one of the highest mortality rates among neoplasms. This fact is explained by its aggressive behavior through a high metastatic rate and rapid progression time. Despite many theories behind metastasis migration in the peritoneal cavity, theories regarding particular chemokines and their ligands and peritoneal milky spots seem to lead fittingly. A plethora of molecular mechanisms occur in each of the processes leading to peritoneal dissemination to confide free gastric cancer cells with the vital instruments to survive in a hostile intraabdominal microenvironment. The presence of PM translates in an appalling prognosis for gastric cancer patients with a median survival of approximately 4 months [1, 2]. Thus, new and effective intraperitoneal chemotherapy strategies are needed to mitigate the progression of the disease. For the past two decades, great advances have been made in the diagnosis and treatment of end-stage cancers. The peritoneum tends to be an ideal spreading ground for distant metastasis caused by epithelial cancers. These include various types such as ovarian, colon, pancreatic and gastric carcinomas [3]. Although, there are increasingly more studies demonstrating the adhesion mechanisms of the carcinoma cells to the peritoneum, it is yet unclear under which exact mechanisms this adhesion occurs, thus making it a challenge for both scientists and clinicians to ascertain effective strategies to prevent and treat peritoneal metastasis hence ensuing dismal prognosis and limited treatment options for the patients. This overview aims to present and analyze the currently available scientific literature regarding a novel intraperitoneal chemotherapeutic therapy and its effect on synchronous and metachronous metastasis from gastric cancer.
Epidemiology
Gastric cancer is the fourth most common cancer in the world and leads as the third and fifth cancer-related cause of death in men and women respectively [4]. Prognosis of gastric cancer is dismal and 5-year-survival barely reaches 30%. However, the incidence of gastric cancer has shown a significant decline over the past half century. This reduction in gastric cancer incidence is largely related to the economic improvements leading to improved sanitation, better food hygiene, and a reduction in the prevalence of Helicobacter pylori infection. Still, gastric cancer continues to be a major health care problem in East Asia, Eastern Europe, Latin America, and certain areas in the United States of America [5]. Though the incidence of gastric cancer is showing a declining trend, the percentage of its aggressive variant ‘signet ring cell cancer’ is reported to be increasing in recent years [6].
Gastric cancer is considered an aggressive malignancy due to its metastasizing capabilities through the bloodstream to the liver, through lymphatics to the regional lymph nodes, or by the penetration of the peritoneal lining of the stomach to its immediate surroundings including the peritoneum [7]. Thus, PM is a common finding, observed in almost 20% patients at the time of planned curative surgery [8, 9].
Pathophysiology of peritoneal metastasis
Albeit the notable differences in the mechanisms through which cancer cells reach the peritoneum depending upon the primary tumor, it is still a frequent homing site for metastasis from ovarian, colorectal, gastric and pancreatic tumors. In this section, we will elucidate the mechanisms known to date, by which the implantation of metastasis derived from gastric carcinomas in the peritoneal cavity is accomplished. The anatomy and physiology of the peritoneum make it an ideal location for the formation of these metastases, specifically its extensive area and the presence and hydrodynamics of the peritoneal fluid throughout the entire surface area.
Molecular mechanisms of gastric cancer derived peritoneal metastasis
In 2011 Valastyan et al. [10] proposed a revised conceptual approach entailing a six-step hematogenous metastasizing process from primary local tumor to distant metastasis: (1) local invasion, (2) intravasation, (3) survival in the circulation, (4) arrest at distant organ site and extravasation, (5) micro-metastasis formation and (6) metastatic colonization. Pachmayr et al. [11] highlighted an explanation of the events and mechanisms involved in each one of the steps. The first event of cancer cell metastasis is detachment of the free cancer cell from the primary tumor. For this to happen, a disruption in the union between the epithelial cell and the matrix must occur. The unstable cell–cell unions that explain cancer cell detachment are a byproduct of aberrant cadherin activity, thus allowing the epithelium to be more permeable [12]. This is an important part of a process named epithelial-mesenchymal transition (EMT). Essentially, EMT is the transformation of epithelial cells into mesenchymal cells, through which cells acquire important migratory and invasive properties. Mechanisms also attributed to EMT, specifically in gastric cancer, include preventing apoptosis and cellular senescence, and contributing to immunosuppression [13]. Following intravasation, accomplished mainly by the secretion of vascular endothelial growth factor (VEGF) and proteases by the detached tumor cells, these must survive in the circulation to reach the distant organ site. Through tumor cell-induced platelet aggregation and secretion of various factors, tumor cells enhance their capability to adhere to capillary endothelial walls, permeate through the vascular wall and promote growth, survival and motility in the distant organ [14].
Pertaining to the peritoneal dissemination of gastric cancer, several steps are involved: (1) detachment of cancer cells from the primary tumor, (2) survival in the microenvironment of the abdominal cavity, (3) attachment of free tumor cells to peritoneal mesothelial cells and invasion of the basement membrane, and (4) tumor growth with the onset of angiogenesis [15, 16]. The most frequent detachment mechanism is the spontaneous exfoliation of tumor cells after having invading the serosa. Dysregulation of the calcium-dependent cell–cell adhesion molecule E-cadherin (CDH1) produces important changes in the epithelial architecture and cell polarity, which contribute to the invasion of the gastric wall and subsequent migration into the abdominal cavity. Also, the phosphorylation activation of the ERK pathway, the anti-inflammatory protein Annexin 1 (ANXA1) and the neutrophin receptor-interacting melanoma antigen-encoding gene homolog (NRAGE) are involved in this pathological process [16,17,18].
In order for free gastric cancer cells to grow and form solid metastases, they must survive in the hostile, hypoxic, and nutrient-poor intraabdominal environment. Until they can attach to the mesothelium, tumor preservation mechanisms come in play. Serving as a rich immune (macrophages, T-lymphocytes and B-lymphocytes) pro-inflammatory microenvironment, milky spots (MS), which are minute cribriform stomatas located on the peritoneal surfaces mainly in the omentum and subdiaphragmatic areas, harbor free cancer cells and form metastatic foci. Within this hypoxic niche provided by the MS, tumor associated macrophages (TAMs) participate in the promotion of cancer cell motility and metastasis in stromal and perivascular areas [19]. Microscopically, MS contain a capillary network of blood vessels which enables them to communicate, through pores or stomata, to the peritoneal cavity, blood stream and surrounding omentum [19, 20]. MS express a key transcription factor involved in the cellular response to hypoxic conditions, as well as angiogenesis and glycolysis: hypoxia-inducible factor-1α (HIF-1α). Through it, the EGFR/STAT and TGF-β/Smad signaling pathways are activated and a set of adaptive transcriptional responses that regulate tumor stem cell differentiation and self-renewal are triggered. Subsequently, the ability of the cell to differentiate is reduced whilst the self-renewal rate is enhanced, ensuing a more aggressive tumor [19, 21]. Also, EMT is induced by down-regulation of CDH1 and up-regulation of alpha-smooth muscle actin (α-SMA), enhancing the PM recurrence ratio as demonstrated by Miao et al. [21]. It has been suggested that throughout the EMT, cancer associated fibroblasts (CAFs) are generated from mesenchymal cells with multiple-differentiation potential [22]. CAFs are associated with migration, invasion and progression of disease by means of a wide range of factors (cytokines, growth factors and chemokines). A pool of microRNAs (miRNAs), specifically miRNA-200b, miRNA-106b, mi RNA-143 and miRNA-145, have been linked to CAFs. The last two are known to be under-expressed in gastric cancer cell lines. When miRNA-143 expression is increased, it can induce apoptosis by targeting COX-2. miRNA-143 also regulates the expression of collagen type III in CAFs, a protein that significantly increases tumor cell migration and invasion [23].
Migrating molecular mechanisms are not completely clear, nevertheless recent research has demonstrated certain pathways and mechanisms are present in cancer cell dissemination in the peritoneal cavity. Chemokines (CXC/CC) are thought to be involved as small secretory proteins that control migration and activation of leukocytes and other types of cells through interaction with a group of seven transmembrane G protein-coupled chemokine receptors (CCR). It is believed that the axis between CCL12-22/CCR4, the first being a ligand expressed by the free gastric cancer cell and the second being the receptor of the ligand, in combination with the pro immune macrophage reactions of the peritoneum serve as the “seed and soil” for the settlement of gastric cancer derived PM via the PI3K/mTOR pathway [24,25,26]. Intriguingly, CCR4 ligands can be found in higher concentrations in the omentum and in the diaphragm underlining [25]. Zhang et al. [27] demonstrated that the down-regulation of phosphatase and tensin homolog (PTEN), and consequent up-regulation of the PI3K/NF-κB/FAK pathway play a role in dissemination of gastric cancer cells.
Adhesion to the peritoneal surface is achieved on account of specific molecules promoting invasion of the peritoneum and mesothelium. The submesothelial basement membrane penetration mechanism could be explained by the production of growth factors and matrix metalloproteinases by the free cells that contribute to the contraction of the mesothelial cells, thus exposing the membrane and allowing it to be breached. Integrins (α1, α3β1, α6) are overexpressed, intermediating the initial attachment of gastric cancer cells to extracellular matrix (ECM) proteins [28, 29]. Matrix metalloproteinase 7 (MMP7) has been demonstrated to play a central role in stromal invasion via degradation of most components of the ECM and activating other MMP family members [30]. Chen et al. concluded in a translational study, that patients expressing low connective tissue growth factor (CTGF), a secretory protein known to be involved in cell adhesion and chemotaxis, among other processes, had a significantly higher prevalence of PM and the corresponding lower probability of survival after surgery [31]. They concluded that CTFG acted through binding to integrin α3β1 and preventing it from binding to laminin [31, 32].
Finally, angiogenesis must be achieved for the new-formed metastasis to receive vital substrate from the main circulation. This new vessel formation is mainly driven by VEGF, which provides the metastasis with the crucial microvascular density (MVD) to survive. A study by Li et al. [33] demonstrated the relationship between integrin β3, VEGF protein expression, MVD, survival period and 5-year survival rate of gastric cancer patients.
Provided that ascites is present, data suggests that cancer cells within a mucinous fluid are redistributed on the abdomino-pelvic surfaces. In the model presented by Carmignani et al. [34], free “cancer cells do not immediately adhere to a peritoneal surface after detachment from the primary malignancy” rather, owing to physical forces such as intraperitoneal fluid hydrodynamics and gravity in conjunction with the anatomical attributes of the peritoneum, the cells move with the peritoneal fluid to distant sites, resulting in a wider distribution of cancer cells both in the abdomen and pelvis [34].
Another potential risk factor for the development of PM is the presence of free cancer cells which are exfoliated from the tumors reaching the serosal surface during surgery. In almost 60% of post-gastrectomy cases, peritoneal washings may show the presence of CEA or CK20 mRNA that did not have CEA or CK20 mRNA amplification in peritoneal washings immediately prior to surgery. This may result in poor peritoneal recurrence free-survival [35].
Treatment
Traditionally, PM is managed with therapeutic nihilism because of the associated dismal prognosis. The last two decades have witnessed a paradigm shift in the management of PM due to various studies confirming the benefit of various peritonectomy procedures, hyperthermic intraperitoneal chemotherapy (HIPEC), and pressurized intraperitoneal chemotherapy (PIPAC).
Advantages of intraperitoneal chemotherapy application
It is known that only a small portion of the systemically applied chemotherapy is delivered to the peritoneum. Hence, it seems appealing to approach peritoneal metastasis directly with the usage of intraperitoneal (IP) chemotherapy, which lowers systemic side effects and is potentially more effective. A meta-analysis by Yang et al. [36] demonstrated a survival benefit for patients treated with intraperitoneal combined with intravenous chemotherapy compared to patients with intravenous chemotherapy only.
The largest evidence and experience of IP chemotherapy application derives from Japan. In contrast to Western centers, which usually provide IP chemotherapy through HIPEC after (semi-) curative cytoreductions, the Japanese centers mainly provide IP chemotherapy through IP palliative or neo-adjuvant treatment options. The recently published PHOENIX-GC trial: “A phase III trial comparing intraperitoneal and intravenous paclitaxel plus S-1 vs. cisplatin plus S-1 in patients with GC with PM” showed in 164 patients an overall survival benefit for patients treated with combined IP and IV chemotherapy (17.7 vs. 15.2 months; p = 0.08) and an increased 3 years overall survival rate (21.9% vs. 6.0%) compared to IV chemotherapy only, but failed the level of significance. According to this study the IP regimen compromised intraperitoneal paclitaxel 20 mg/m2 and IV paclitaxel 50 mg/m2 on days 1 and 8 plus oral S-1 80 mg/m2 per day on days 1 to 14 of every 3 weeks cycle. The IV regimen compromised intravenous cisplatin 60 mg/m2 on day 8 plus oral S-1 80 mg/m2 per day on days 1 to 21 of every 5 weeks cycle [37].
More evidence for neoadjuvant IP chemotherapy (docetaxel and cisplatin) followed by four cycles of oral S-1 is provided by Canbay et al.. The largest single center study included 194 patients with GC and either PM or positive cytology. In total, 152 patients (78.3%) showed negative results in peritoneal cytology after combined neoadjuvant IP and IV regimen and were treated with CRS & HIPEC. Multivariate analysis revealed PCI ≤ 6, pathologic response to neoadjuvant IP chemotherapy, and completeness of cytoreduction as significant factors for overall survival [38]. Patients tolerated in general the combined or so call bidirectional intraperitoneal and systemic induction chemotherapy well. Five patients developed hematologic complications, eight gastrointestinal, 25 nausea/vomiting and 18 patients developed fatigue. No chemotherapeutic associated death was observed. Postoperative complications after CRS & HIPEC occurred in 36 patients (23.6%) with an overall operative mortality rate of 3.9% (6/152) [38]. However, another important aspect despite the therapeutic substance is the way of application. Table 1 summarizes the adverse events published in some of the previously mentioned studies after CRS and HIPEC.
Intratumoral fluid pressure and drug penetration
After the intraperitoneal instillation of the chemotherapeutic agents, two mechanisms that drive the tissue transport of the drugs are diffusion and convection. Convection occurs due to the pressure gradient between the tumor tissue and the intraperitoneal fluid column. On the other hand, drug diffusion is the result of a concentration gradient. The rate of diffusion is determined by the temperature, the physicochemical drug properties, and the stromal architecture [44]. As the intra-tumoral interstitial fluid pressure is considerably higher compared to normal tissue due to rapid tumor cell proliferation, contraction of the interstitial stroma by activated fibroblasts, hyper-permeable microvessels, and deficient lymphatic drainage, drug transport within the tumor tissue is largely dependent upon the diffusion [45]. A number of physical (raising the intraperitoneal pressure, prolonging the exposure time, higher temperature, hyperbaric oxygen, photodynamic therapy, radiation therapy, ultrasound) and pharmacological interventions (drugs targeting the tumor vessels, stromal components, tumor cell density, or tumor pH) may result in better tumor tissue penetration of the drugs [44].
There is evidence, that increased intraperitoneal pressure of 10, 20, and 30 mmHg or 25 cm H2O leads to an increased tissue uptake of doxorubicin, cisplatin and oxaliplatin in animal models applying IP chemotherapy similar to HIPEC [46,47,48]. Just recently, Kusamura et al. published preliminary results of the first human trial focusing on different levels of abdominal pressure during HIPEC (NCT02949791). The preliminary results favor an intraabdominal pressure of 18 mmHg compared to 11 mmHg in the aim of a higher cisplatin tissue concentration [49].
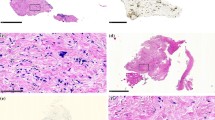
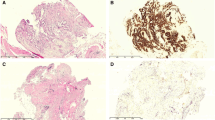
There is a difference in drug tissue penetration between the soluble application of intraperitoneal chemotherapy (NIPS or HIPEC) and the pressurized aerosol application (PIPAC). In a HIPEC model, the expectable ratio of cisplatin tissue concentration is 30–50%, whereas in PIPAC models, using pressure and repeated application, an expected uptake ratio of + 200% can be reached [50, 51]. The drug penetration depth of cisplatin could be measured in an animal model as 349 ± 65 µm, as reported by Khosrawipour et al. [52]. Unfortunately, there is no such data in HIPEC models for cisplatin, only paclitaxel. Coccolini et al. demonstrated a penetration depth of 630 µm for nab-paclitaxel, whereas CremophorEL-paclitaxel was not detectable in peritoneal tissue of rabbits [53]. These findings support further studies in the usage of intraperitoneal nanoparticles. To combine the effect of hyperthermia with the increased tissue penetration of PIPAC, Do Hyun Jung et al. developed a first porcine model for hyperthermic pressurized intraperitoneal chemotherapy (H-PAC) [54].
Cytotoxic effects of intraperitoneal application
Cisplatin
The most commonly used drug is cisplatin (CDDP), which forms covalent binds with endogenous nucleophiles after replacing its own cis chloro groups with water molecules. This interaction leads to two different consequences: (1) promoting oxidative stress which may have a direct cytotoxic effect or induce DNA damage, and (2) operating as a cytoprotective buffer by inactivating chemically reactive cisplatin. CDDP binds with high affinity to mitochondrial and nuclear DNA and induces DNA damage, which leads to either a permanent cell cycle arrest or mitochondrial apoptosis [55].
Doxorubicin
In 1995, the liposomal doxorubicin (DoxilⓇ) was approved for the treatment of numerous types of cancer and also the first nanodrug [56]. Doxorubicin passively diffuses into the cytoplasm of the cancer cell, where it is converted into a semiquinone and generates reactive oxygen species (ROS). In the cytosol, doxorubicin enters the mitochondria causing DNA damage and energetic stress. Hence, the cytochrome C peptide is released by the mitochondria triggering the caspase cascade leading to cell death [57].
Paclitaxel
Paclitaxel is one of several cytoskeletal drugs that target tubulin, which results in defects in mitotic spindle assembly, chromosome segregation, and cell division. Paclitaxel stabilizes the microtubule polymer and protects it from disassembly. Chromosomes are thus unable to achieve a metaphase spindle configuration. This blocks the progression of mitosis and prolonged activation of the mitotic checkpoint triggers apoptosis or revision to the G0-phase without cell division [58, 59].
PIPAC as a strategy against gastric cancer derived peritoneal metastasis
In 2011, Solass et al. [60] corroborated direct penetration of methylene blue in normal peritoneum and confirmed that peritoneal nebulization allowed for a better distribution of this substance throughout the porcine abdominal cavity in comparison with peritoneal lavage (i.e. HIPEC). Recently, the same group described a novel method that involved the use of an innovative intraperitoneal chemotherapy named pressurized intraperitoneal aerosol chemotherapy (PIPAC) [61] applicable to the human patient. This method combines the benefits of an aerosol (i.e. dispersion), with those of higher-than-normal intraabdominal pressure provided by the laparoscopy technique and proved to be well tolerated. Within these benefits is the capacity of the chemotherapeutic agent to reach the complete area of the targeted tissue, in this case, the metastasis. This translates in better distribution and penetration of the drug by counterbalancing intrametastatic interstitial fluid pressure, which in turn yields higher intrametastatic concentrations and less systemic toxicity, comprising clear pharmacokinetic advantages when chemotherapeutic drugs that target metastasis are delivered intraperitoneally rather than intravenously [60].
Surgical procedure
The procedure begins with a diagnostic laparoscopy under general anesthesia. A two-trocar method is used, placing a 12 mm trocar in the middle of the lower abdomen and a second 5–12 mm trocar in the lower lateral abdomen. Capnoperitoneum is achieved via CO2-insufflation, reaching an intraabdominal pressure of 14 mmHg at 37 °C. The extent of peritoneal involvement is assessed using PCI [62]. Peritoneal biopsies are taken in different locations for histopathological examination. Afterwards, both doxorubicin (suggested dosage: 1.5 mg/m2 body surface) and CPPD (7.5 mg/m2 body surface), dissolved in NaCl 0.9% are applied through an injector at a 0.3 ml/s flow rate and pressure of 1380 kPa over 30 min in aerosol form. The toxic remnant is disposed of through a closed aerosol waste system (CAWS) before removing the trocars. Several studies have demonstrated that this procedure does not expose health providers to an occupational hazard [63, 64].
Cytotoxic agents used for PIPAC
In contrast to the broad evidence for (the combination of) intravenous chemotherapeutic substances, there is only little evidence about the intraperitoneal usage of these substances. Mostly, the therapeutic regimens were chosen in analogy to intravenous evidence, which is one of the major problems regarding the level of evidence of chemotherapeutic drugs for HIPEC or PIPAC. Most recently, Weinreich et al. provided the first attempt of evidence for chemosensitivity in gastric cancer cell lines (MKN45, 23132/87) using a combination of cisplatin and doxorubicin at same concentrations as used in clinical approach (cisplatin 24 µg/ml; doxorubicin 5 µg/ml) provided with HIPEC and PIPAC [65].
Further clinical studies were performed in order to evaluate the ideal intraperitoneal dose of cisplatin and doxorubicin in patients with ovarian cancer. Tempfer et al. demonstrated the safe use and low systemic toxicity of 10.5 mg/m2 cisplatin and 2.1 mg/m2 doxorubicin in 15 patients treated with PIPAC, while the maximum tolerable dose was not reached [66].
Benefits of PIPAC
To date, there are no well-defined indications for PIPAC, which translates into few clinical studies specific to stomach neoplasms. Nevertheless, PIPAC shows a promising future accredited to its benefits in treating metastatic disease indistinctively of its origin [67]. Momentarily, phase II studies that aim to investigate, among other aspects, long term survival, are being carried out. The latest trial available, published in an abstract form, enrolled 25 patients in an open-label, single-arm phase II clinical trial, in which ten of the 25 patients had an objective tumor response. Nine of the 12 (75%) patients who underwent a minimum of two PIPAC procedures had a complete or major histological tumor regression. Furthermore, there were no treatment-related deaths and four patients with grade three toxicities (Common Terminology Criteria for Adverse Events—CTCAE v3) reported. The mean OS was 8.4 months, higher (13.1 months) in patients with a PCI under 12 [68]. A study by Nadiradze et al. [69] demonstrated histopathological regression in 50% of the gastric cancer patients submitted to PIPAC, half of which showed complete histological remission and the other half partial regression. Furthermore, stable disease was documented in 12.5% (3/24) of the cases. However, patients with synchronous malignant pleural effusion did not benefit from PIPAC. In a retrospective series published by Alyami et al. [70], the PCI improved in 64.5% of the patients treated with PIPAC, as did the symptoms related to PM. A fourth study worth mentioning is that of Odendahl et al. [71], which remains self-critic due to some described bias, but still reported stabilization of QoL during PIPAC, demonstrated by non-deteriorating gastrointestinal symptoms and stable functional scores, ultimately concluding that PIPAC does not deteriorate QoL in the patients with peritoneal metastasis in a salvage situation. Moreover, Girshally et al. [72] proposed that PIPAC could be used as neoadjuvant therapy before CRS with HIPEC and showed interesting preliminary data. Table 2 illustrates the documented complications in various studies also including other tumor entities. Nowacki et al. reported the first case of neoadjuvant PIPAC in a patient with PM of GC (PCI 19) and a singular liver metastasis. Eight weeks after receiving PIPAC, the patient, showing a complete peritoneal response, underwent gastrectomy, D2-lymphadenectomy, and atypical liver resection. Postoperatively the patient received Capecitabine as recommended [73]. To note, PIPAC can be offered as an earlier therapeutic option to patients who are not eligible for peritonectomy. After histological regression of the metastasis (response to the treatment), a complete cytoreduction surgery could potentially be proposed to these patients. Presently, phase II trials aiming to study the oncological benefit of PIPAC are in progress. The results of which will hopefully inspire confidence in clinicians. Median overall survival results of several studies of patients with PM of gastric cancer are illustrated according to their therapeutic regimen (chemotherapy, CRS & HIPEC, PIPAC) in Fig. 1 [39, 41, 68, 74,75,76,77].
Safety and adverse events after PIPAC
It has been demonstrated that patients who have undergone the procedure have not shown evidence of postoperative hepatic or renal toxicities [80]. Moreover, the aerosol properties coalesce with the benefits of a minimally invasive procedure, such as lower postoperative morbidity, better QoL and the possibility of effortlessly repeating the method. Nevertheless, as with any medical intervention, complications may arise. There are several publications focusing on patient (morbidity and mortality) and staff safety analyzing platin remains in swipe samples of several locations as well as biomonitoring in urine samples. Despite the fact that platinum concentration after PIPAC is increased on the gloves of the surgeon, the floor, and the PIPAC device, biomonitoring remained negative and therefore staff contamination can be excluded as long as the proposed safety guidelines are followed [81, 82]. Regarding morbidity, PIPAC using low dose cisplatin (7.5 mg/m2) and doxorubicin (1.5 mg/m2) is considered to be a safe technique, which is supported by several publications. Contrarily, the usage of oxaliplatin led in two out of 24 patients to severe peritoneal sclerosis and has to be followed-up carefully. Patient one had a mucinous adenocarcinoma of the appendix and patient two was treated due to a goblet cell carcinoid [83]. The latest trial on methodological and technical analysis available, published a retrospective multicenter experience of 832 PIPAC procedures in 349 patients with PM of different tumor origin demonstrating the homogenously performed and standardized procedure in 34 PIPAC centers [84] setting up the field for further multicenter trials.
Ongoing trials and new endeavors
Numerous Phase I and Phase II trials are currently ongoing and recruiting. Table 3 gives an overview about registered and ongoing PIPAC trials for cancer patients with PM of GC [85,86,87]. PIPAC has opened a new world of therapeutic opportunities for cancer patients with PM through the use of cancer chemotherapeutic drugs as aerosols. Nevertheless, Minnaert et al. [88] reported the use of aerosolized nucleic acid (small interfering RNAs, siRNAs) to downregulate cancer-associated genes, opening a new field of research for future cancer treatment options.
Conclusion and suggestions for further research
Metastasizing tumors, notably gastric neoplasms, continue to be responsible for a significant number of deaths yearly all around the world, despite significant advances in the research and understanding of these. Poor therapeutic response of the primary tumor, resistance of PM to intravenous chemotherapy and a fraught general health could be the explanation. After reviewing current literature, there is definitely a sense of hope for patients with advanced gastric cancer. Through CRS with HIPEC, carefully selected patients have longer survival times, notably when carried out in specialized high-volume centers that can provide quality perioperative care. With the introduction of PIPAC, a novel treatment option can now be offered to patients who are potential candidates for CRS with HIPEC, but do not yet meet the criteria to be subjected to surgery. Documented adverse events are significantly reduced, histological regression is often evidenced and the patient’s QoL is stabilized. There is a growing amount of clinical evidence regarding PIPAC and HIPEC, nevertheless further research is warranted to determine the underlying molecular mechanisms being affected by intraperitoneal chemotherapeutics within the metastasis itself to comprehend and target oncogenic promotion factors, consequently reducing therapy related toxicity and helping devise better strategies to treat therapy responders and non-responders. Well-designed multicenter randomized control trials are needed to compare the benefit of sequential PIPAC procedures with systemic chemotherapy to chemotherapy alone in patients with unresectable gastric cancer derived PM. Finally, researchers and clinicians alike must strive towards the creation and implementation of comprehensive guidelines regarding PIPAC after efficacy is thoroughly demonstrated.
Abbreviations
- ANXA1:
-
Anti-inflammatory protein Annexin 1
- CAFs:
-
Cancer associated fibroblasts
- CAWS:
-
Closed aerosol waste system
- CCR:
-
Transmembrane G protein-coupled chemokine receptors
- CDH1:
-
Calcium-dependent cell–cell adhesion molecule E-cadherin
- CRS:
-
Cytoreductive surgery
- CTGF:
-
Connective tissue growth factor
- CXC/CC:
-
Chemokines
- ECM:
-
Extracellular matrix
- EMT:
-
Epithelial-mesenchymal transition
- HIF-1α:
-
Hypoxia-inducible factor-1α
- HIPEC:
-
Hyperthermic intraperitoneal chemotherapy
- miRNA:
-
MicroRNAs
- MMP:
-
Matrix metalloproteinase
- MS:
-
Milky spots
- MVD:
-
Microvascular density
- NCCN:
-
National comprehensive cancer network
- NIPS:
-
Neoadjuvant intraperitoneal-systemic chemotherapy protocol
- NRAGE:
-
Neutrophin receptor-interacting melanoma antigen-encoding gene homolog
- PCI:
-
Peritoneal cancer index
- PIPAC:
-
Pressurized intraperitoneal aerosol chemotherapy
- PM:
-
Peritoneal metastasis
- PTEN:
-
Phosphatase and tensin homolog
- S-1:
-
Tegafur, 5-chloro-2-4-dihydroxypyridine and oxonic acid
- TAMs:
-
Tumor associated macrophages
- VEGF:
-
Vascular endothelial growth factor
- α-SMA:
-
Alpha-smooth muscle actin
References
Thomassen I, Van Gestel YR, Van Ramshorst B et al (2013) Peritoneal carcinomatosis of gastric origin: a population-based study on incidence, survival and risk factors. Int J Cancer 134:622–628. https://doi.org/10.1002/ijc.28373
Yang D, Hendifar A, Lenz C et al (2011) Survival of metastatic gastric cancer: significance of age, sex and race/ethnicity. J Gastrointest Oncol 2:77–84. https://doi.org/10.3978/j.issn.2078-6891.2010.025
van Baal JOAM, Van de Vijver KK, Nieuwland R et al (2017) The histophysiology and pathophysiology of the peritoneum. Tissue Cell 49:95–105. https://doi.org/10.1016/j.tice.2016.11.004
American Cancer Society (2015) Global cancer facts & figs, 3rd edn. American Cancer Society, Atlanta
Balakrishnan M, George R, Sharma A, Graham DY (2017) Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep 19:36. https://doi.org/10.1007/s11894-017-0575-8
Lu M, Yang Z, Feng Q et al (2016) The characteristics and prognostic value of signet ring cell histology in gastric cancer: a retrospective cohort study of 2199 consecutive patients. Medicine 95(27):e4052. https://doi.org/10.1097/MD.0000000000004052
Sugarbaker PH (2018) Gastric cancer: prevention and treatment of peritoneal metastases. J Cancer Metastasis Treat 4:7. https://doi.org/10.20517/2394-4722.2017.67
Sugarbaker PH, Yonemura Y (2000) Clinical pathway for the management of resectable gastric cancer with peritoneal seeding: best palliation with a ray of hope for cure. Oncology 58(2):96–107
Gretschel S, Siegel R, Estévez-Schwarz L et al (2006) Surgical strategies for gastric cancer with synchronous peritoneal carcinomatosis. Br J Surg 93:1530–1535. https://doi.org/10.1002/bjs.5513
Valastyan S, Weinberg RA (2011) Review tumor metastasis: molecular insights and evolving paradigms. Cell 147:275–292. https://doi.org/10.1016/j.cell.2011.09.024
Pachmayr E, Treese C, Stein U (2017) Underlying mechanisms for distant metastasis-molecular biology. Visc Med 33(1):11–20. https://doi.org/10.1159/000454696
Takeichi M (1993) Cadherins in cancer: implications for invasion and metastasis. Curr Opin Cell Biol 5:806–811. https://doi.org/10.1016/0955-0674(93)90029-P
Peng Z, Wang C, Fang E et al (2014) Role of epithelial-mesenchymal transition in gastric cancer initiation and progression. World J Gastroenterol 20:5403–5410. https://doi.org/10.3748/wjg.v20.i18.5403
Chang M-C, Jeng J-H (2011) Tumor Cell-Induced Platelet Aggregation. In: Schwab M (ed) Encyclopedia of cancer. Springer, Berlin, p 3793–3795
Yutaka Y, Yoshio E, Tohru O, Takuma S (2006) Recent advances in the treatment of peritoneal dissemination of gastrointestinal cancers by nucleoside antimetabolites. Cancer Sci 98:11–18. https://doi.org/10.1111/j.1349-7006.2006.00350.x
Kanda M, Kodera Y (2016) Molecular mechanisms of peritoneal dissemination in gastric cancer. 22:6829–6840. https://doi.org/10.3748/wjg.v22.i30.6829
Cheng T, Wu M, Lin J, Lin M (2012) Annexin A1 is associated with gastric cancer survival and promotes gastric cancer cell invasiveness through the formyl peptide receptor/extracellular signal-regulated kinase/integrin beta-1-binding protein 1 pathway. Cancer 118(23):5757–5767. https://doi.org/10.1002/cncr.27565
Singh J, Sharma A, Ahuja N (2017) Genomics of peritoneal surface malignancies. J Perit. https://doi.org/10.4081/joper.2017.62
Liu J, Geng X, Li Y (2016) Milky spots: omental functional units and hotbeds for peritoneal cancer metastasis. Tumor Biol 5715–5726. https://doi.org/10.1007/s13277-016-4887-3
Liebermann-Meffert D, White H, Vaubel E (1983) The greater OMENTUM. Springer, Berlin
Miao ZF, Wang ZN, Zhao TT et al (2014) Peritoneal milky spots serve as a hypoxic niche and favor gastric cancer stem/progenitor cell peritoneal dissemination through hypoxia-inducible factor 1α. Stem Cells 32:3062–3074. https://doi.org/10.1002/stem.1816
Quail DF, Joyce JA (2013) Microenvironmental regulation of tumor progression and metastasis. Nat Med 19:1423–1437. https://doi.org/10.1038/nm.3394
Yan Y, Wang L-F, Wang R-F (2015) Role of cancer-associated fibroblasts in invasion and metastasis of gastric cancer. World J Gastroenterol 21:9717. https://doi.org/10.3748/wjg.v21.i33.9717
Mura G, Verdelli B (2016) The features of peritoneal metastases from gastric cancer. J Cancer Metastasis Treat 2:365. https://doi.org/10.20517/2394-4722.2016.19
Cao L, Hu X, Zhang J et al (2014) The role of the CCL22-CCR4 axis in the metastasis of gastric cancer cells into omental milky spots. J Transl Med 12:267. https://doi.org/10.1186/s12967-014-0267-1
Chen G, Chen SM, Wang X et al (2012) Inhibition of chemokine (CXC motif) ligand 12/chemokine (CXC motif) receptor 4 axis (CXCL12/CXCR4)-mediated cell migration by targeting mammalian target of rapamycin (mTOR) pathway in human gastric carcinoma cells. J Biol Chem 287:12132–12141. https://doi.org/10.1074/jbc.M111.302299
Zhang LL, Liu J, Lei S et al (2014) PTEN inhibits the invasion and metastasis of gastric cancer via downregulation of FAK expression. Cell Signal 26:1011–1020. https://doi.org/10.1016/j.cellsig.2014.01.025
Takatsuki H, Komatsu S, Sano R et al (2004) Adhesion of gastric carcinoma cells to peritoneum mediated by α3β1 integrin (VLA-3). Cancer Res 64:6065–6070. https://doi.org/10.1158/0008-5472.CAN-04-0321
Nishimori H, Yasoshima T, Denno R et al (2000) A novel experimental mouse model of peritoneal dissemination of human gastric cancer cells: different mechanisms in peritoneal dissemination and hematogenous metastasis. Jpn J Cancer Res 91:715–722. https://doi.org/10.1111/j.1349-7006.2000.tb01004.x
Yonemura Y, Endou Y, Fujita H et al (2000) Role of MMP-7 in the formation of peritoneal dissemination in gastric cancer. Gastric Cancer 3:63–70
Chen C-N, Chang C-C, Lai H-S et al (2015) Connective tissue growth factor inhibits gastric cancer peritoneal metastasis by blocking integrin α3β1-dependent adhesion. Gastric Cancer 18:504–515. https://doi.org/10.1007/s10120-014-0400-0
Saito Y, Sekine W, Sano R et al (2010) Potentiation of cell invasion and matrix metalloproteinase production by alpha3beta1 integrin-mediated adhesion of gastric carcinoma cells to laminin-5. Clin Exp Metastasis 27:197–205. https://doi.org/10.1007/s10585-010-9314-3
Li S-G, Ye Z-Y, Zhao Z-S et al (2008) Correlation of integrin β3 mRNA and vascular endothelial growth factor protein expression profiles with the clinicopathological features and prognosis of gastric carcinoma. World J Gastroenterol 14:421. https://doi.org/10.3748/wjg.14.421
Carmignani CP, Sugarbaker TA, Bromley CM, Sugarbaker PH (2003) Intraperitoneal cancer dissemination: Mechanisms of the patterns of spread. Cancer Metastasis Rev 22:465–472. https://doi.org/10.1023/A:1023791229361
Takebayashi K, Murata S, Yamamoto H et al (2014) Surgery-induced peritoneal cancer cells in patients who have undergone curative gastrectomy for gastric cancer. Ann Surg Oncol 21:1991–1997. https://doi.org/10.1245/s10434-014-3525-9
Yang S, Feng R, Pan ZC et al (2015) A comparison of intravenous plus intraperitoneal chemotherapy with intravenous chemotherapy alone for the treatment of gastric cancer: a meta-analysis. Sci Rep 5:1–12. https://doi.org/10.1038/srep12538
Ishigami H, Fujiwara Y, Fukushima R et al (2018) Phase III trial comparing intraperitoneal and intravenous paclitaxel plus S-1 versus cisplatin plus S-1 in patients with gastric cancer with peritoneal metastasis: PHOENIX-GC trial. J Clin Oncol 36:1922–1929. https://doi.org/10.1200/JCO.2018.77.8613
Canbay E, Mizumoto A, Ichinose M et al (2014) Outcome data of patients with peritoneal carcinomatosis from gastric origin treated by a strategy of bidirectional chemotherapy prior to cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in a single specialized center in Japan. Ann Surg Oncol 21:1147–1152. https://doi.org/10.1245/s10434-013-3443-2
Yang X-J, Huang C-Q, Suo T et al (2011) Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol 18:1575–1581. https://doi.org/10.1245/s10434-011-1631-5
Rudloff UDO, Langan RC, Mullinax JE et al (2014) Impact of maximal cytoreductive surgery plus regional heated intraperitoneal chemotherapy (HIPEC) on outcome of patients with peritoneal carcinomatosis of gastric origin: results of the GYMSSA trial. J Surg Oncol, 110(3):275–284. https://doi.org/10.1002/jso.23633
Glehen O, Gilly FN, Arvieux C et al (2010) Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Ann Surg Oncol 17:2370–2377. https://doi.org/10.1245/s10434-010-1039-7
Magge D, Zenati M, Mavanur A et al (2014) Aggressive locoregional surgical therapy for gastric peritoneal carcinomatosis. Ann Surg Oncol 21:1448–1455. https://doi.org/10.1245/s10434-013-3327-5
Harmon RL, Sugarbaker PH (2005) Prognostic indicators in peritoneal carcinomatosis from gastrointestinal cancer. Int Semin Surg Oncol 2:3. https://doi.org/10.1186/1477-7800-2-3
Lagast N, Carlier C, Ceelen WP (2018) Pharmacokinetics and tissue transport of intraperitoneal chemotherapy. Surg Oncol Clin N Am 27:477–494. https://doi.org/10.1016/j.soc.2018.02.003
Carlier C, Mathys A, De Jaeghere E et al (2017) Tumour tissue transport after intraperitoneal anticancer drug delivery. Int J Hyperth 33:534–542. https://doi.org/10.1080/02656736.2017.1312563
Jacquet P, Stuart OA, Chang D, Sugarbaker PH (1996) Effects of intra-abdominal pressure on pharmacokinetics and tissue distribution of doxorubicin after intraperitoneal administration. Anticancer Drugs 7:596–603
Esquis P, Consolo D, Magnin G et al (2006) High intra-abdominal pressure enhances the penetration and antitumor effect of intraperitoneal cisplatin on experimental peritoneal carcinomatosis. Ann Surg 244:106–112. https://doi.org/10.1097/01.sla.0000218089.61635.5f
Facy O, Al Samman S, Magnin G et al (2012) High pressure enhances the effect of hyperthermia in intraperitoneal chemotherapy with oxaliplatin: an experimental study. Ann Surg 256:1084–1088. https://doi.org/10.1097/SLA.0b013e3182582b38
Kusamura S, Luca F, Baratti D et al (2018) Phase II randomized study on tissue distribution of cisplatin according to different levels of intra abdominal pressure during HIPEC: preliminary results. NCT02949791. Eur J Surg Oncol 44:e7. https://doi.org/10.1016/j.ejso.2018.07.029
Tempfer CB, Hilal Z, Dogan A et al (2018) Concentrations of cisplatin and doxorubicin in ascites and peritoneal tumor nodules before and after pressurized intraperitoneal aerosol chemotherapy (PIPAC) in patients with peritoneal metastasis. Eur J Surg Oncol 44:1112–1117. https://doi.org/10.1016/j.ejso.2018.04.020
Cho H-K, Lush RM, Bartlett DL et al (1999) Pharmacokinetics of cisplatin administered by continuous hyperthermic peritoneal perfusion (CHPP) to patients with peritoneal carcinomatosis. J Clin Pharmacol 39:394–401. https://doi.org/10.1177/00912709922007967
Khosrawipour V, Khosrawipour T, Kern AJP et al (2016) Distribution pattern and penetration depth of doxorubicin after pressurized intraperitoneal aerosol chemotherapy (PIPAC) in a postmortem swine model. J Cancer Res Clin Oncol 142:2275–2280. https://doi.org/10.1007/s00432-016-2234-0
Coccolini F, Acocella F, Morosi L et al (2017) High penetration of paclitaxel in abdominal wall of rabbits after hyperthermic intraperitoneal administration of Nab-Paclitaxel compared to standard paclitaxel formulation. Pharm Res 34:1180–1186. https://doi.org/10.1007/s11095-017-2132-4
Jung DH, Son SY, Oo AM et al (2016) Feasibility of hyperthermic pressurized intraperitoneal aerosol chemotherapy in a porcine model. Surg Endosc 30:4258–4264. https://doi.org/10.1007/s00464-015-4738-0
Galluzzi L, Vitale I, Michels J et al (2014) Systems biology of cisplatin resistance: past, present and future. Cell Death Dis 5:e1257–e1218. https://doi.org/10.1038/cddis.2013.428
Barenholz Y (2012) Doxil®—the first FDA-approved nano-drug: lessons learned. J Control Release 160:117–134. https://doi.org/10.1016/j.jconrel.2012.03.020
Franco Y, Vaidya T, Ait-Oudhia S (2018) Anticancer and cardio-protective effects of liposomal doxorubicin in the treatment of breast cancer. Breast Cancer Targets Ther 10:131–141. https://doi.org/10.2147/BCTT.S170239
Bharadwaj R, Yu H (2004) The spindle checkpoint, aneuploidy, and cancer. Oncogene 23:2016
Brito DA, Yang Z, Rieder CL (2008) Microtubules do not promote mitotic slippage when the spindle assembly checkpoint cannot be satisfied. J Cell Biol 182:623 LP–L629
Solaß W, Hetzel A, Nadiradze G et al (2012) Description of a novel approach for intraperitoneal drug delivery and the related device. Surg Endosc 26:1849–1855. https://doi.org/10.1007/s00464-012-2148-0
Solass W, Kerb R, Mürdter T et al (2014) Intraperitoneal chemotherapy of peritoneal carcinomatosis using pressurized aerosol as an alternative to liquid solution: first evidence for efficacy. Ann Surg Oncol 21:553–559. https://doi.org/10.1245/s10434-013-3213-1
Jacquet P, Sugarbaker PH (1996) Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res 82:359–374
Ametsbichler P, Böhlandt A, Nowak D, Schierl R (2018) Occupational exposure to cisplatin/oxaliplatin during pressurized intraperitoneal aerosol chemotherapy (PIPAC)?. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2018.05.020
Solaß W, Giger-Pabst U, Zieren J, Reymond MA (2013) Pressurized intraperitoneal aerosol chemotherapy (PIPAC): occupational health and safety aspects. Ann Surg Oncol 20:3504–3511. https://doi.org/10.1245/s10434-013-3039-x
Weinreich J, Struller F, Sautkin I et al (2018) Chemosensitivity of various peritoneal cancer cell lines to HIPEC and PIPAC: comparison of an experimental duplex drug to standard drug regimens in vitro. Investig New Drugs. https://doi.org/10.1007/s10637-018-0641-6
Tempfer CB, Giger-Pabst U, Seebacher V et al (2018) A phase I, single-arm, open-label, dose escalation study of intraperitoneal cisplatin and doxorubicin in patients with recurrent ovarian cancer and peritoneal carcinomatosis. Gynecol Oncol 150:23–30. https://doi.org/10.1016/j.ygyno.2018.05.001
Sleeman JP (2017) PIPAC puts pressure on peritoneal metastases from pancreatic cancer. Clin Exp Metastasis 34:291–293. https://doi.org/10.1007/s10585-017-9851-0
Struller F, Horvath P, Solass W et al (2017) Pressurized intraperitoneal aerosol chemotherapy with low-dose cisplatin and doxorubicin (PIPAC C/D) in patients with gastric cancer and peritoneal metastasis (PIPAC-GA1). J Clin Oncol 35:99. https://doi.org/10.1200/JCO.2017.35.4_suppl.99
Nadiradze G, Giger-Pabst U, Zieren J et al (2016) Pressurized intraperitoneal aerosol chemotherapy (PIPAC) with low-dose cisplatin and doxorubicin in gastric peritoneal metastasis. J Gastrointest Surg 20:367–373. https://doi.org/10.1007/s11605-015-2995-9
Alyami M, Gagniere J, Sgarbura O et al (2017) Multicentric initial experience with the use of the pressurized intraperitoneal aerosol chemotherapy (PIPAC) in the management of unresectable peritoneal carcinomatosis. Eur J Surg Oncol 43:2178–2183. https://doi.org/10.1016/j.ejso.2017.09.010
Odendahl K, Solass W, Demtröder C et al (2015) Quality of life of patients with end-stage peritoneal metastasis treated with pressurized intraperitoneal aerosol chemotherapy (PIPAC). Eur J Surg Oncol 41:1379–1385. https://doi.org/10.1016/j.ejso.2015.06.001
Girshally R, Demtröder C, Albayrak N et al (2016) Pressurized intraperitoneal aerosol chemotherapy (PIPAC) as a neoadjuvant therapy before cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. World J Surg Oncol 14:253. https://doi.org/10.1186/s12957-016-1008-0
Nowacki M, Grzanka D, Zegarski W (2018) Pressurized intraperitoneal aerosol chemotheprapy after misdiagnosed gastric cancer: case report and review of the literature. World J Gastroenterol 24:2130–2136. https://doi.org/10.3748/wjg.v24.i19.2130
Chan DL, Sjoquist KM, Goldstein D et al (2017) The effect of anti-angiogenic agents on overall survival in metastatic oesophago-gastric cancer: a systematic review and meta-analysis. PLoS ONE 12:e0172307. https://doi.org/10.1371/journal.pone.0172307
Thuss-Patience PC, Kretzschmar A, Dogan Y et al (2011) Docetaxel and capecitabine for advanced gastric cancer: investigating dose-dependent efficacy in two patient cohorts. Br J Cancer 105:505–512. https://doi.org/10.1038/bjc.2011.278
Khomiakov V, Ryabov A, Bolotina LV et al (2017) Bidirectional chemotherapy in gastric cancer (GC) with peritoneal carcinomatosis (PC) combining intravenous chemotherapy with intraperitoneal chemotherapy with low-dose cisplatin and doxorubicin administered as a pressurized aerosol: an open-label, phase. J Clin Oncol 35:e15532–e15532. https://doi.org/10.1200/JCO.2017.35.15_suppl.e15532
Alyami M, Bonnot PE, Villeneuve L et al (2018) Pressurized intraperitoneal aerosol chemotherapy (PIPAC) for nonresectable peritoneal carcinomatosis from gastric cancer. J Clin Oncol 36:149. https://doi.org/10.1200/JCO.2018.36.4_suppl.149
Tempfer CB, Rezniczek GA, Ende P (2015) Pressurized intraperitoneal aerosol chemotherapy with cisplatin and doxorubicin in women with peritoneal carcinomatosis: a cohort study. Anticancer Res 35:6723–6730
Khomyakov V, Ryabov A, Ivanov A et al (2016) Bidirectional chemotherapy in gastric cancer with peritoneal metastasis combining intravenous XELOX with intraperitoneal chemotherapy with low-dose cisplatis and Doxorubicin administered as a pressurized aerosol: an open-label, phase-2 study (PIPAC-GA2). 1:159–166. https://doi.org/10.1515/pap-2016-0017
Blanco A, Giger-Pabst U, Solass W et al (2013) Renal and hepatic toxicities after pressurized intraperitoneal aerosol chemotherapy (PIPAC). Ann Surg Oncol 20:2311–2316. https://doi.org/10.1245/s10434-012-2840-2
Ndaw S, Hanser O, Kenepekian V et al (2018) Occupational exposure to platinum drugs during intraperitoneal chemotherapy. Biomonitoring and surface contamination. Toxicol Lett. https://doi.org/10.1016/j.toxlet.2018.05.031
Jansen-Winkeln B, Thieme R, Haase L et al (2018) Perioperative sicherheit der intraperitonealen aerosolchemotherapie. Der Chir. https://doi.org/10.1007/s00104-018-0667-5
Graversen M, Detlefsen S, Pfeiffer P et al (2018) Severe peritoneal sclerosis after repeated pressurized intraperitoneal aerosol chemotherapy with oxaliplatin (PIPAC OX): report of two cases and literature survey. Clin Exp Metastasis 35:103–108. https://doi.org/10.1007/s10585-018-9895-9
Nowacki M, Alyami M, Villeneuve L et al (2018) Multicenter comprehensive methodological and technical analysis of 832 pressurized intraperitoneal aerosol chemotherapy (PIPAC) interventions performed in 349 patients for peritoneal carcinomatosis treatment: an international survey study. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2018.02.014
Dumont F, Senellart H, Pein F et al (2018) Phase I/II study of oxaliplatin dose escalation via a laparoscopic approach using pressurized aerosol intraperitoneal chemotherapy (PIPOX trial) for nonresectable peritoneal metastases of digestive cancers (stomach, small bowel and colorectal): rationale and design. Pleura Perit. https://doi.org/10.1515/pp-2018-0120
Goetze TO, Al-Batran SE, Pabst U et al (2018) Pressurized intraperitoneal aerosol chemotherapy (PIPAC) in combination with standard of care chemotherapy in primarily untreated chemo naive upper gi-adenocarcinomas with peritoneal seeding—A phase II/III trial of the AIO/CAOGI/ACO. Pleura Perit. https://doi.org/10.1515/pp-2018-0113
Eveno C, Jouvin I, Pocard M (2018) PIPAC EstoK 01: pressurized intraperitoneal aerosol chemotherapy with cisplatin and doxorubicin (PIPAC C/D) in gastric peritoneal metastasis : a randomized and multicenter phase II study. Pleura Perit 1–7. https://doi.org/10.1515/pap-2018-0116
Minnaert A-K, Dakwar GR, Benito JM et al (2017) High-pressure nebulization as application route for the peritoneal administration of sirna complexes. Macromol Biosci 17:1700024. https://doi.org/10.1002/mabi.201700024
Ceelen WP, Van de Sande L (2018) PIPAC Nab-pac for stomach, pancreas, breast and ovarian cancer (PIPAC-nabpac). https://clinicaltrials.gov/ct2/show/NCT03304210
Mortensen MB (2017) Treatment of Peritoneal carcinomatosis with pressurized intraperitoneal aerosol chemotherapy—(PIPAC-OPC2). https://clinicaltrials.gov/ct2/show/NCT03287375
So J, Guowei K (2017) Pressurized Intraperitoneal aerosol chemotherapy (PIPAC) with oxaliplatin in patients with peritoneal carcinomatosis (PIPAC). https://clinicaltrials.gov/ct2/show/NCT03172416
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alberto, M., Brandl, A., Garg, P.K. et al. Pressurized intraperitoneal aerosol chemotherapy and its effect on gastric-cancer-derived peritoneal metastases: an overview. Clin Exp Metastasis 36, 1–14 (2019). https://doi.org/10.1007/s10585-019-09955-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-019-09955-4