Abstract
Background
Atypical meningioma differs from Grade I meningioma in terms of high recurrence rate and short life expectancy. We evaluated the clinical course of atypical meningioma and investigated prognostic factors affecting its outcomes.
Method
We reviewed 45 patients with atypical meningioma who underwent surgical intervention between January 2000 and December 2013. The mean age of the patients and mean follow-up period was 58.7 years and 81.0 months, respectively. Analyses included factors such as patient age, gender, location and size of tumor, extent of surgical resection (Simpson Grading System), and MIB-1 labeling index (LI). Univariate analysis was used to detect prognostic factors associated with recurrence and survival.
Results
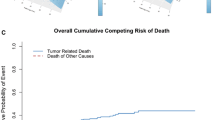
The 5-year recurrence-free rate for all 45 patients was 58.4 %; 5- and 10-year survival rates were 83.2 % and 79.9 %, respectively. In univariate analyses, age >60 years, and MIB-1 LI correlated with disease recurrence, whereas age >60 years, subtotal surgical resection, MIB-1 LI, and indication for radiotherapy correlated with death. MIB-1 LI levels higher than 12.8 % and 19.7 % predicted recurrence and death, respectively. In our cohort, 26 patients received postoperative radiotherapy including conventional radiation (n = 21) or gamma knife radiosurgery (n = 5). Postoperative radiotherapy did not decrease recurrence rates in our cohort (p = 0.63). Six and two patients who died during the study period underwent conventional radiation and radiosurgery, respectively.
Conclusions
Age, male gender, extent of surgical resection, and higher MIB-1 LI influenced the outcome of atypical meningioma. In our cohort, postoperative radiotherapy failed to provide long-term tumor control. Following incomplete surgical resection of atypical meningioma in elderly patients, adjuvant postoperative radiotherapy may not be an ideal treatment option, particularly when MIB-1 LI is higher than 19.7 %.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meningioma is a type of tumor that arises from the meninges of the brain and spinal cord. It is the most common of all central nervous system (CNS) tumors, representing approximately 30 % of the CNS neoplasms [11, 24, 32]. Subgroups of meningioma with aggressive and malignant behaviors have long been recognized [12]. The term “atypical grade II meningioma” was first coined in 1985 [20]. Based on histopathological criteria, the World Health Organization (WHO) further classified meningioma into atypical (Grade II) and anaplastic (Grade III) subtypes in its recent classification schemes [26, 37]. Following the induction of the 2000 and 2007 WHO classifications, the proportion of atypical meningioma has increased [35, 44]. According to recent reports, atypical meningioma now accounts for approximately 20–30 % of meningioma cases [6, 34, 35].
Previous literature suggests an increased risk of recurrence and shorter lengths of overall survival in atypical meningioma than that of its benign counterparts [22, 28, 36]. Atypical meningioma carries a sevenfold to eightfold increased risk of recurrence, and an approximate twofold increased risk of death 3–5 years post-diagnosis [36]. Moreover, previous studies have reported possible prognostic factors of atypical meningioma recurrence as cellular proliferating index [5, 9, 33, 34, 43], age [13, 14, 34, 45], tumor location [43], preoperative tumor size [13], degree of surgical resection [13–16, 22, 27, 33, 45], and early postoperative radiotherapy [1, 22, 23, 33]. However, these reports are controversial, and the optimum treatment strategy for atypical meningioma remains to be elucidated.
In the present study, we retrospectively reviewed the medical records of 45 patients with atypical meningioma who underwent surgical treatment at our institute. We intended to identify risk factors for the poor prognosis of this clinical entity.
Materials and methods
Patients
We reviewed the medical records of all patients who underwent surgical resection of intracranial meningioma at the Tohoku University Hospital between January 2000 and December 2013; we identified 45 patients with atypical meningioma from a total of 398 patients with WHO Grade I, II, or III meningioma according to the criteria as described below (see “Tumor histology”). We excluded patients who underwent primary surgery at another institution and were subsequently referred to our hospital. Furthermore, patients with a history of any other intracranial tumor or neurofibromatosis type 2 were excluded.
This study was approved by the Internal Review Board of the Ethical Committee at the Tohoku University Hospital. Our Institutional Review Board did not require informed consent from patients due to the retrospective nature of this study.
Tumor histology
Histological subtypes were determined according to the WHO 2007 criteria [37]. Atypical meningioma was defined as WHO-II (2007) meningioma. Tumor occurrences before 2007 were re-evaluated by a senior neuropathologist (M.W.) to confirm the diagnosis. A Grade II meningioma was diagnosed as the presence of four or more mitoses per ten high-power fields or three or more of the following features: increased cellularity, high nuclear/cytoplasm ratio, prominent nucleoli, sheet-like growth and/or geographic necrosis as well as clear cell and chordoid histologies. Consequently, 45 patients were diagnosed as atypical meningioma and included in this study. The MIB-1 labeling index (LI) was used to assess cellular proliferation. For quantification, the most densely stained areas were selected [38]. Overall, the number of stained tumor cells was counted among 1,000 tumor cells. MIB-1 LI was available for 42 of the 45 patients, and further analyses regarding MIB-1 LI were performed in these 42 patients.
Clinical and radiological data
Demographic data including patient age and gender were collected. Tumor size was evaluated using contrast-enhanced magnetic resonance imaging (MRI); when MRI was not available, computed tomography (CT) was used. The size was measured as the longest tumor length in any dimension on preoperative imaging. Tumor location was determined using the images and/or surgeon’s operative notes. According to previous meningioma criteria [39], those arising from the olfactory groove, sphenoid wing, tuberculum sellae, cerebellopontine angle, foramen magnum, anterior clinoid, cavernous sinus, petroclival region, tentorium, middle fossa, or posterior fossa (non-convexity) were classified as cranial base lesions; those located in the convexity, falcine, parasagittal, or interventricular regions were classified as non-cranial base lesions.
Treatment
The extent of resection was determined based on the operative notes and postoperative imaging. The Simpson Grading system was used for analyses [41]. Patients in whom Simpson Grade I–II resection was achieved were defined as gross total resection (GTR). When tumors were not completely resected, either conventional radiation or gamma knife radiosurgery was indicated for all patients with atypical meningioma. Following complete resection of the tumor, decision for radiotherapy was made by consensus among neurosurgeons (T.E., K.M., M.F., Y.S., H.J., and T.T.) and radiation oncologists. If indicated, conventional radiation or gamma knife radiosurgery was offered immediately following the surgical treatment. Radiation modalities and doses varied according to the location of the tumor.
Patients were followed-up in the outpatient clinic using successive MRI. In case of emergence of new enhanced areas or regrowth of residual tumors, indication and timing for further treatment were discussed. In the present paper, we defined the date of recurrence as when the second surgery was performed or when radiotherapy was applied after the aforementioned radiographic changes. In addition to the surgical intervention, either conventional radiation or gamma knife radiosurgery was indicated at the time of recurrence.
Statistical analysis
Overall and recurrence-free survivals were calculated from the date of surgery. The probability of death or recurrence was estimated using the Cox proportional hazards model. Univariate analysis was performed to determine associations between recurrence or death and other factors. The following variables were analyzed: age, gender, location and size of the tumor, extent of surgical resection, MIB-1 LI, and immediate postoperative radiotherapy. In order to estimate the most discriminatory cut-off for MIB-1 LI with respect to tumor recurrence and survival, receiver-operated characteristics (ROC) were used. Statistical analyses were performed using JMP version 11 (SAS Institute., Cary, NC, USA) and data represented as mean ± standard deviation (SD). Differences were deemed significant at p < 0.05.
Results
In this study, we included 45 patients [20 women (44.4 %) and 25 men (55.6 %)] with atypical meningioma. Clinical characteristics of the patients are summarized in Table 1. Patient age ranged from 5 to 82 years (mean, 58.7 years). The mean follow-up period was 81.0 months (range, 5–187 months). In 17 (37.8 %) and 28 (62.2 %) patients, meningioma was located in the cranial and non-cranial base regions, respectively. Simpson Grade I and Grade II resection was achieved in 12 and 19 patients, respectively. These 31 patients were classified as GTR, and the remaining patients were judged to undergo Simpson Grade III (3 patients) and Grade IV (11 patients) resection. Following non-GTR resections (n = 14), 10 and 4 patients received postoperative conventional radiation and radiosurgery, respectively. Following GTR (n = 31), 11 and 1 patients received postoperative conventional radiation and radiosurgery, respectively. Overall, 21 patients received conventional radiation with a dose of 50 Gy (n = 12) and 54–60 Gy (n = 9). Among the 12 patients who underwent GTR and received postoperative either conventional radiation (n = 11) or radiosurgery (n = 1), recurrence was observed in 4 patients during the follow-up period (33.3 %), whereas 8 patients suffered recurrence (42.1 %) among those who did not receive radiotherapy after GTR (n = 19). This difference did not reach statistical significance.
Prognostic factors
The 5-year recurrence-free rate for all 45 patients was 58.4 %; 5- and 10-year survival rates were 83.2 % and 79.9 %, respectively. Risk factors for recurrence and death as indicated by univariate analysis are shown in Table 2. Age >60 years (p < 0.001), and higher MIB-1 LI (p < 0.007) were associated with a high recurrence rate. Furthermore, age >60 years (p = 0.016), subtotal resection (p = 0.003), higher MIB-1 LI (p = 0.004), and indication for radiotherapy (p = 0.007) were associated with death. Using a ROC analysis, 12.8 % of MIB-1 LI predicted recurrence with an 83.3 % sensitivity and 62.5 % specificity. Regarding survival, an MIB-1 LI of 19.7 % was the best predictive value, yielding 75.0 % sensitivity and 88.3 % specificity.
Discussion
In this study, we retrospectively reviewed 45 patients with atypical meningioma, with a mean follow-up period of 81.0 months. Regarding clinical outcomes including recurrence-free and overall survivals at 5 years, our results are comparable to other studies, as summarized in Table 3 [1, 14–16, 27, 33, 34, 43, 45, 46]. Notably, our cohort predominantly included male patients (55.6 %), which is in accordance with previous studies indicating different gender predominance in benign and non-benign meningioma [7, 34]. Furthermore, our analyses suggested the male gender as a risk for recurrence, although the difference was not statistically significant (p = 0.051, Table 2). One study actually indicated the male gender as a risk for shorter survival in atypical meningioma [43], while another study reported that the female gender would predict recurrences [46] (Table 3). Considering the inconsistency regarding the gender as a risk factor, our result could be due to the small sample size of our cohort. Our analyses also found an older age as a significant prognostic factor; this finding is concomitant with those of other studies reporting older age as a significant risk for recurrence and shorter survival (Table 3) [14, 15, 33, 34, 45].
MIB1-LI
In the present study, higher MIB-1 LI was the strongest indicator of a poor outcome in atypical meningioma, as suggested in previous literature [33, 34, 43]. A recent meta-analysis suggested that MIB-1 LI for atypical meningioma was between 2 and 20 %, with an average value of 8 % [3]. Several studies have suggested an MIB-1 LI of 10 % as a meaningful criterion to predict the clinical course of the disease [18, 42]. In a study including 16 patients with atypical meningioma [9], an MIB-1 LI <9.9 % was associated with longer overall survival. In our cohort, ROC analyses indicate that an MIB-1 LI >12.8 % predicts recurrence with the best combination of sensitivity and specificity. For prediction of death in patients with atypical meningioma, 19.7 % was considered as an appropriate cut-off value. However, it was concerning that MIB-1 LI data in our study were relatively higher than those reported in previous studies. This was probably because we calculated MIB-1 LI by adopting the highest labeling method [2]. Counting methods in MIB-1-positive cells may also have influenced the results [30]. Since several authors have preferred to count randomly selected fields or evenly distributed fields [40], care must be taken when comparing MIB-1 LI values between different studies.
Surgical resection
The degree of surgical resection also influenced clinical courses in our case series. Regarding surgical resection, our findings corroborate with those of other studies that complete surgical resection of a tumor is an important factor in reducing recurrence and expecting longer overall survival (Table 3) [1, 14–16, 27, 33, 45, 46]. Vranic et al. [43] found that a parasagittal–falcine location led to a higher recurrence rate in their series of 76 cases of atypical meningioma. Although the degree of surgical resection was not a significant prognostic factor in their study, the authors speculated that residual tumors along the superior sagittal sinus contributed to the higher recurrence rate of atypical meningioma in this location. Our findings highlight the fact that achieving complete resection should be important in risk stratification of atypical meningioma.
Postoperative radiotherapy
In benign grade I meningioma, postoperative radiation usually provides long-term tumor control even after subtotal resection. In a series of 300 benign meningioma cases, the recurrence rates improved in patients who underwent subtotal resection and postoperative radiotherapy; these rates became comparable to the rates of those who underwent total resection [31]. However, for atypical meningioma, the situation can be different. The role of postoperative radiotherapy remains controversial, as Hardesty et al. [17] implied that radiotherapy could not offer good tumor control in atypical meningioma following subtotal removal. In a study analyzing 166 atypical meningioma patients, postoperative radiotherapy was not beneficial, but associated with a poorer prognosis [14].
In the present study, all patients underwent immediate postoperative radiotherapy after incomplete resection, referring to studies that advocated early adjuvant radiotherapy for atypical meningioma [1, 4, 22, 23, 25, 33]. Nonetheless, radiotherapy failed to provide long-term control in our cohort, because all eight patients who died during the study period had undergone postoperative radiotherapy. This result must be read with caution, since it could be related to a major limitation of the current study, that is, indication, modalities, and doses of radiotherapy were not consistent throughout the patients. Our study included 12 patients (38.7 %) who underwent postoperative radiotherapy, even though they had achieved complete resection. This shows that indications for postoperative radiotherapy fluctuated, particularly for completely resected atypical meningioma, in our treatment protocol. Furthermore, among 24 patients who underwent immediate postoperative radiotherapy in our cohort, 12 underwent conventional radiation with a dose of 50 Gy. Although 50 Gy was the minimum irradiation dose required for atypical meningioma [29, 34], higher doses of radiation may have improved clinical results in our patients [7, 19, 21]. While there has also been a report that recommends radiosurgery as a treatment of choice [27], our study included only five patients for whom radiosurgery was prescribed. Further studies with a larger number of patients and a standard protocol are necessary to determine the appropriate dose and modality regarding postoperative radiotherapy.
Limitations
The present study had limitations due to its retrospective design and small number of patients; another limitation is that our analyses solely relied on clinical data of the patients and the histological appearance of the tumors. Recently, gene sequence analyses have revealed different genetic backgrounds of meningioma at various locations [8, 10]. For instance, medial and lateral meningioma had different genetic backgrounds, although they were histologically indistinguishable. Having recognized the important role of genetic alterations in the generation and progression of meningioma [37], future studies should include genetic backgrounds in their analyses.
Conclusion
Even with multimodal treatments, the prognosis of atypical meningioma remains poor. Based on our analyses, atypical meningioma with a higher MIB-1 LI recurred more frequently in elderly patients following surgical intervention. Postoperative radiotherapy could not provide long-term tumor control in patients with incompletely resected atypical meningioma, particularly in those harboring an MIB-1 LI higher >19.7 %. Our results emphasize the importance of pursuing complete surgical removal of atypical meningioma.
Reference
Aboukais R, Baroncini M, Zairi F, Reyns N, Lejeune JP (2013) Early postoperative radiotherapy improves progression free survival in patients with grade 2 meningioma. Acta Neurochir (Wien) 155:1385–1390
Abramovich CM, Prayson RA (1999) Histopathologic features and MIB-1 labeling indices in recurrent and nonrecurrent meningiomas. Arch Pathol Lab Med 123:793–800
Abry E, Thomassen IO, Salvesen OO, Torp SH (2010) The significance of Ki-67/MIB-1 labeling index in human meningiomas: a literature study. Pathol Res Pract 206:810–815
Adeberg S, Hartmann C, Welzel T, Rieken S, Habermehl D, von Deimling A, Debus J, Combs SE (2012) Long-term outcome after radiotherapy in patients with atypical and malignant meningiomas--clinical results in 85 patients treated in a single institution leading to optimized guidelines for early radiation therapy. Int J Radiat Oncol Biol Phys 83:859–864
Aghi MK, Carter BS, Cosgrove GR, Ojemann RG, Amin-Hanjani S, Martuza RL, Curry WT Jr, Barker FG 2nd (2009) Long-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiation. Neurosurgery 64:56–60
Backer-Grondahl T, Moen BH, Torp SH (2012) The histopathological spectrum of human meningiomas. Int J Clin Exp Pathol 5:231–242
Boskos C, Feuvret L, Noel G, Habrand JL, Pommier P, Alapetite C, Mammar H, Ferrand R, Boisserie G, Mazeron JJ (2009) Combined proton and photon conformal radiotherapy for intracranial atypical and malignant meningioma. Int J Radiat Oncol Biol Phys 75:399–406
Brastianos PK, Horowitz PM, Santagata S, Jones RT, McKenna A, Getz G, Ligon KL, Palescandolo E, Van Hummelen P, Ducar MD, Raza A, Sunkavalli A, Macconaill LE, Stemmer-Rachamimov AO, Louis DN, Hahn WC, Dunn IF, Beroukhim R (2013) Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat Genet 45:285–289
Bruna J, Brell M, Ferrer I, Gimenez-Bonafe P, Tortosa A (2007) Ki-67 proliferative index predicts clinical outcome in patients with atypical or anaplastic meningioma. Neuropathology 27:114–120
Clark VE, Erson-Omay EZ, Serin A, Yin J, Cotney J, Ozduman K, Avsar T, Li J, Murray PB, Henegariu O, Yilmaz S, Gunel JM, Carrion-Grant G, Yilmaz B, Grady C, Tanrikulu B, Bakircioglu M, Kaymakcalan H, Caglayan AO, Sencar L, Ceyhun E, Atik AF, Bayri Y, Bai H, Kolb LE, Hebert RM, Omay SB, Mishra-Gorur K, Choi M, Overton JD, Holland EC, Mane S, State MW, Bilguvar K, Baehring JM, Gutin PH, Piepmeier JM, Vortmeyer A, Brennan CW, Pamir MN, Kilic T, Lifton RP, Noonan JP, Yasuno K, Gunel M (2013) Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339:1077–1080
Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM (2005) Epidemiology of intracranial meningioma. Neurosurgery 57:1088–1095
Cushing H, Eisenhardt L (1938) Serial enumeraion of meningiomas. In: Charles CT (ed) Meningiomas. Their classification, regional behaviour, life history, and surgical end results. . Springfield, pp 56–73
Detti B, Scoccianti S, Di Cataldo V, Monteleone E, Cipressi S, Bordi L, Pellicano G, Gadda D, Saieva C, Greto D, Pecchioli G, Buccoliero A, Ceroti M, Ammannati F, Biti G (2013) Atypical and malignant meningioma: outcome and prognostic factors in 68 irradiated patients. J Neurooncol 115:421–427
Durand A, Labrousse F, Jouvet A, Bauchet L, Kalamarides M, Menei P, Deruty R, Moreau JJ, Fevre-Montange M, Guyotat J (2009) WHO grade II and III meningiomas: a study of prognostic factors. J Neurooncol 95:367–375
Gabeau-Lacet D, Aghi M, Betensky RA, Barker FG, Loeffler JS, Louis DN (2009) Bone involvement predicts poor outcome in atypical meningioma. J Neurosurg 111:464–471
Hammouche S, Clark S, Wong AH, Eldridge P, Farah JO (2014) Long-term survival analysis of atypical meningiomas: survival rates, prognostic factors, operative and radiotherapy treatment. Acta Neurochir (Wien) 156:1475–1481
Hardesty DA, Wolf AB, Brachman DG, McBride HL, Youssef E, Nakaji P, Porter RW, Smith KA, Spetzler RF, Sanai N (2013) The impact of adjuvant stereotactic radiosurgery on atypical meningioma recurrence following aggressive microsurgical resection. J Neurosurg 119:475–481
Ho DM, Hsu CY, Ting LT, Chiang H (2002) Histopathology and MIB-1 labeling index predicted recurrence of meningiomas: a proposal of diagnostic criteria for patients with atypical meningioma. Cancer 94:1538–1547
Hug EB, Devries A, Thornton AF, Munzenride JE, Pardo FS, Hedley-Whyte ET, Bussiere MR, Ojemann R (2000) Management of atypical and malignant meningiomas: role of high-dose, 3D-conformal radiation therapy. J Neurooncol 48:151–160
Jaaskelainen J, Haltia M, Laasonen E, Wahlstrom T, Valtonen S (1985) The growth rate of intracranial meningiomas and its relation to histology. An analysis of 43 patients. Surg Neurol 24:165–172
Kano H, Takahashi JA, Katsuki T, Araki N, Oya N, Hiraoka M, Hashimoto N (2007) Stereotactic radiosurgery for atypical and anaplastic meningiomas. J Neurooncol 84:41–47
Kaur G, Sayegh ET, Larson A, Bloch O, Madden M, Sun MZ, Barani IJ, James CD, Parsa AT (2014) Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Neuro Oncol 16:628–636
Komotar RJ, Iorgulescu JB, Raper DM, Holland EC, Beal K, Bilsky MH, Brennan CW, Tabar V, Sherman JH, Yamada Y, Gutin PH (2012) The role of radiotherapy following gross-total resection of atypical meningiomas. J Neurosurg 117:679–686
Kotecha RS, Pascoe EM, Rushing EJ, Rorke-Adams LB, Zwerdling T, Gao X, Li X, Greene S, Amirjamshidi A, Kim SK, Lima MA, Hung PC, Lakhdar F, Mehta N, Liu Y, Devi BI, Sudhir BJ, Lund-Johansen M, Gjerris F, Cole CH, Gottardo NG (2011) Meningiomas in children and adolescents: a meta-analysis of individual patient data. Lancet Oncol 12:1229–1239
Lee KD, DePowell JJ, Air EL, Dwivedi AK, Kendler A, McPherson CM (2013) Atypical meningiomas: is postoperative radiotherapy indicated? Neurosurg Focus 35:E15
Louis DN, Scheithauer BW, Budka H (2000) Meningiomas. In: Kleihues P, Cavanee WK (eds) World Health Organization classifications of tumours; pathology and genetics of tumours of the nervous system. . IARC Lyon, pp 176–184
Mair R, Morris K, Scott I, Carroll TA (2011) Radiotherapy for atypical meningiomas. J Neurosurg 115:811–819
McGovern SL, Aldape KD, Munsell MF, Mahajan A, DeMonte F, Woo SY (2010) A comparison of World Health Organization tumor grades at recurrence in patients with non-skull base and skull base meningiomas. J Neurosurg 112:925–933
Milosevic MF, Frost PJ, Laperriere NJ, Wong CS, Simpson WJ (1996) Radiotherapy for atypical or malignant intracranial meningioma. Int J Radiat Oncol Biol Phys 34:817–822
Nakasu S, Li DH, Okabe H, Nakajima M, Matsuda M (2001) Significance of MIB-1 staining indices in meningiomas: comparison of two counting methods. Am J Surg Pathol 25:472–478
Ohba S, Kobayashi M, Horiguchi T, Onozuka S, Yoshida K, Ohira T, Kawase T (2011) Long-term surgical outcome and biological prognostic factors in patients with skull base meningiomas. J Neurosurg 114:1278–1287
Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, Wolinsky Y, Stroup NE, Kruchko C, Barnholtz-Sloan JS (2013) CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro Oncol 15 Suppl 2:ii1-56
Park HJ, Kang HC, Kim IH, Park SH, Kim DG, Park CK, Paek SH, Jung HW (2013) The role of adjuvant radiotherapy in atypical meningioma. J Neurooncol 115:241–247
Pasquier D, Bijmolt S, Veninga T, Rezvoy N, Villa S, Krengli M, Weber DC, Baumert BG, Canyilmaz E, Yalman D, Szutowicz E, Tzuk-Shina T, Mirimanoff RO (2008) Atypical and malignant meningioma: outcome and prognostic factors in 119 irradiated patients. A multicenter, retrospective study of the Rare Cancer Network. Int J Radiat Oncol Biol Phys 71:1388–1393
Pearson BE, Markert JM, Fisher WS, Guthrie BL, Fiveash JB, Palmer CA, Riley K (2008) Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg Focus 24:E3
Perry A (2004) Unmasking the secrets of meningioma: a slow but rewarding journey. Surg Neurol 61:171–173
Perry A, Louis DN, Scheithauer BW, Budka H, von Deimling A (2007) Meningeal tumours. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the central nervous system. IARC Lyon, pp 164–172
Rezanko T, Akkalp AK, Tunakan M, Sari AA (2008) MIB-1 counting methods in meningiomas and agreement among pathologists. Anal Quant Cytol Histol 30:47–52
Sade B, Chahlavi A, Krishnaney A, Nagel S, Choi E, Lee JH (2007) World Health Organization Grades II and III meningiomas are rare in the cranial base and spine. Neurosurgery 61:1194–1198
Siegers HP, Zuber P, Hamou MF, van Melle GD, de Tribolet N (1989) The implications of the heterogeneous distribution of Ki-67 labelled cells in meningiomas. Br J Neurosurg 3:101–107
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Torp SH, Lindboe CF, Gronberg BH, Lydersen S, Sundstrom S (2005) Prognostic significance of Ki-67/MIB-1 proliferation index in meningiomas. Clin Neuropathol 24:170–174
Vranic A, Popovic M, Cor A, Prestor B, Pizem J (2010) Mitotic count, brain invasion, and location are independent predictors of recurrence-free survival in primary atypical and malignant meningiomas: a study of 86 patients. Neurosurgery 67:1124–1132
Willis J, Smith C, Ironside JW, Erridge S, Whittle IR, Everington D (2005) The accuracy of meningioma grading: a 10-year retrospective audit. Neuropathol Appl Neurobiol 31:141–149
Zaher A, Abdelbari Mattar M, Zayed DH, Ellatif RA, Ashamallah SA (2013) Atypical meningioma: a study of prognostic factors. World Neurosurg 80:549–553
Zhao P, Hu M, Zhao M, Ren X, Jiang Z (2015) Prognostic factors for patients with atypical or malignant meningiomas treated at a single center. Neurosurg Rev 38:101–107
Acknowledgments
We thank Enago (www.enago.jp) for English review.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
For this type of study formal consent is not required.
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Endo, T., Narisawa, A., Ali, H.S.M. et al. A study of prognostic factors in 45 cases of atypical meningioma. Acta Neurochir 158, 1661–1667 (2016). https://doi.org/10.1007/s00701-016-2900-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2900-7