Abstract
Purpose
Annually, over 20 million patients worldwide undergo inguinal hernia repair procedures. Surgery stands as the recommended treatment, however, a consensus on the optimal method is lacking. This study aims to conduct an updated systematic review and meta-analysis to compare the risk of chronic inguinal pain and recurrence between laparo-endoscopic mesh repair (TAPP and TEP) versus Lichtenstein repair for inguinal hernia.
Methods
Searches were conducted in Ovid MEDLINE, PubMed, EBSCO, Cochrane, and Google Scholar. Inclusion criteria encompassed randomized controlled trials (RCTs) involving adults, published in English and Spanish, comparing surgical outcomes among the Lichtenstein open technique, TAPP, and/or TEP. Adherence to the PRISMA guidelines was maintained in the methodology, and the CASP tool was employed to assess the quality of the articles. Statistical analysis involved mean [± standard deviation (SD)], Odds Ratio (OR), and Confidence Interval (CI).
Results
Eight RCTs encompassing 1,469 patients randomized to Lichtenstein repair (n = 755) and laparo-endoscopic repair (n = 714) were included. Laparo-endoscopic repair was associated with a lower likelihood of chronic inguinal pain compared to Lichtenstein repair (OR = 0.28, 95% CI [0.30–0.56], p = 0.0001). There were no significant differences in recurrence rates between the laparo-endoscopic and the Lichtenstein group (OR = 1.03, 95% CI [0.57–1.86], p = 0.92).
Conclusions
This systematic review and meta-analysis demonstrate that laparo-endoscopic hernia surgery leads to a lower incidence of chronic inguinal pain compared to Lichtenstein repair, while maintaining similar rates of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia constitutes 75% of all abdominal wall hernias, with an incidence of 27% in males and 3% in females. These hernias typically manifest with symptoms, and surgical intervention represents the sole curative option thus far [1, 2]. The high prevalence rate of 20 million patients per year result in inguinal hernia repairs to be one of the most common surgical procedures globally [1].
The surgical procedure, hernioplasty, presents substantial challenges, both in economic terms, with costs varying between 126 and 4116 USD per patient [1], and from a societal perspective due to work absenteeism and the emergence of complications.
Common primary complications [1]
-
Recurrence: Notably, some series report recurrence rates as high as 15% [1].
-
Wound infection following surgery.
-
Chronic postoperative inguinal pain (CPIP): CPIP, lacks a universally agreed-upon definition concerning its duration, spanning from 3 months to one year [1]. Nevertheless, certain authors have utilized a criterion of pain persisting for six months or more in their systematic reviews concerning mesh-based hernia repairs [1]. This condition is estimated to afflict 10–12% of patients following surgery, with 1–3% of cases experiencing incapacitating pain [1].
The Lichtenstein technique is universally recognized as the gold standard for open repair of primary inguinal hernias, primarily owning to its minimal recurrence rates, which fall below 1% [3, 4]. Nevertheless, its limitations are manifested in the risk of chronic pain development, which can ascend to 63% in certain series, with moderate to severe pain manifesting in 5–10% of cases [1].
Laparo-endoscopic approaches have garnered increased favor in recent years, with certain surgeons reporting a markedly lower incidence of long-term postoperative pain, ranging between 0% and 3% for severe pain [1, 2, 5, 6]. However, select publications have reported that the extraperitoneal or endoscopic approach (TEP) associates with a heightened risk of recurrence compared to open surgery, particularly when the follow-up data exceeded the three-year mark [4]. Conversely, the laparoscopic approach (TAPP) appears to entail a heightened risk of perioperative complications, including some of a more severe nature, when contrasted to open surgery. Recent studies have illuminated equivalent recurrence rates [4, 7].
Considering the substantial volume of patients undergoing inguinal hernia repair annually, potentially elevating this procedure to one of the most frequently performed interventions in the realm of general surgery, and the potential for postoperative complications, inclusive of CPIP which could afflict one in ten patients [1], becomes imperative to conduct a contemporary systematic review and meta-analysis. The objective is to discern, within the ambit of commonly employed surgical techniques, the method that yields the least CPIP and fewest recurrence during the course of follow-up.
Objectives
-
Primary objective: To assess the risk of chronic inguinal pain in laparo-endoscopic repair (TEP or TAPP) versus the Lichtenstein repair for inguinal hernia.
-
Secondary objective: To evaluate the recurrence rates of inguinal hernia according to the different techniques.
Methodology
This systematic review and meta-analysis follows the preferred reporting items for systematic reviews and meta-analyses (PRISMA) protocol [8].
PICO question
Detailed in Table 1.
Eligibility criteria
The studies analyzed consisted of randomized controlled trials (RCTs) providing the highest level of scientific evidence.
Inclusion criteria
-
a)
Patients aged 18 and above.
-
b)
Studies written in English and Spanish published between 2017 and May 8, 2023.
-
c)
Studies comparing surgical outcomes in Lichtenstein repair, TAPP and/ or TEP techniques for inguinal hernia repair.
-
d)
Inclusion of chronic inguinal pain as a variable in the study.
Exclusion criteria
-
a)
Studies analyzing herniorrhaphies or repairs without mesh.
-
b)
Robotic approaches.
-
c)
Open hernioplasties other than the Lichtenstein technique.
-
d)
Patients undergoing emergency surgery due to incarceration or strangulation.
-
e)
Femoral hernias.
Eligibility assessment was performed by two authors in an unblinded manner. Disagreements were resolved by consensus.
Sources of information
The searched was conducted in electronic databases including Ovid MEDLINE, PubMed, EBSCO, Cochrane and Google Scholar, with the latest search date being May 8, 2023.
Search strategy
A combination of the following Medical Subject Headings (MeSH) terms, using Boolean operators ‘AND’ and ‘OR’ was employed as keywords: “inguinal hernia”, “Lichtenstein”, “open repair techniques”, “laparoscopy”, “TEP”, “TAPP”, “inguinal hernia repair” and “chronic pain”.
Selection process
Two researchers searched independently the reviews based on the pre-specified criteria in the research protocol, placing any screened citations into a database. Initially, the researchers screened the titles and abstracts identified by the search strategy. Any screening-related disagreement was resolved by a third author.
Data collection process
Two authors extracted and examined the data independently. A third author eventually reviewed the database. Discrepancies were clarified by consensus. If an RCT had been reported in more than one publication, the most recent publication that reported the trial was used as the reference article.
Data items
The following data was retrieved from main text, tables and graphs and was recorded in an Excel: author, year of publication, country, study design, number of patients, sex, age, surgical approach, material mesh, weight of mesh, mesh fixation and type of mesh fixation, pubis fixation and type of pubis fixation, neurectomy, chronic inguinal pain and hernia recurrence.
Quality and study risk of bias assessment
To evaluate the methodological quality and conduct a quality analysis of the information within the studies included in this systematic review, the CASP [9] (Critical Appraisal Skills Program) scale was employed. The risk of bias in the included studies was assessed using the Cochrane Collaboration tool [10] and the Cochrane Handbook for Systematic Reviews of Interventions [11]. All included RCTs were evaluated by two reviewers who individually evaluated the quality and the bias of RCTs. Any disagreements were discussed with and resolved by a third author.
Effect measures
A statistical analysis was performed for continuous variables, presenting results as mean [± standard deviation (SD)] or median [interquartile range (IQR)], as appropriate. Categorical variables are expressed as percentages.
Meta-analysis statistical analysis was conducted using RevMan version 5.4 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen) [12]. Clinical outcomes were analyzed using a random-effects model following DerSimonian and Laird. Pooled odds ratios (OR) with a 95% confidence interval (CI) were calculated to measure the effect of each type of procedure, Lichtenstein repair and laparo-endoscopic surgery (TEP and TAPP), for dichotomous variables.
Heterogeneity was assessed by calculating I2 values and Cochrane’s Q test. Regarding the I2 value heterogeneity was classified as low (25%) moderate (50%) or high (75%) and considered significant when p < 0.1 [13].
Publication bias was evaluated visually be assessing funnel plot symmetry and numerically using Rosenthal’s Fail-Safe N or Rosenthal’s Tolerance Index.
Results
Study selection
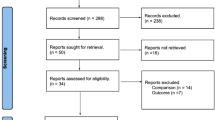
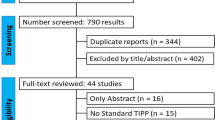
A flow chart (Fig. 1) outlining the study selection process in this systematic review and meta-analysis is presented in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews) [8]. Initially, a search strategy was conducted in electronic databases including PubMed, Cochrane, EBSCO, Ovid, and Google Scholar, resulting in the identification of 252 records. After removing duplicated, 201 titles and abstracts were reviewed for eligibility. Of these, 64 articles were selected for full-text review. After a thorough examination of the remaining 64 articles, 56 did not meet inclusion criteria were excluded.
PRISMA 2020 [8] flow diagram. n = number
Ultimately, a total of 8 articles reporting on randomized controlled trials (RCTs) met the eligibility criteria and were included in the review [14,15,16,17,18,19,20,21].
Study characteristics
The articles incorporated into this systematic review were published between 2017 and 2022, and all of them were randomized clinical trials (RCTs). The overall sample size comprised 1,469 patients who were randomly assigned to two treatment groups: Lichtenstein repair with 51.4% (n = 755) and laparo-endoscopic repair (TAPP or TEP) with 48.6% (n = 714). The mean age of the participants was 54.52 years with a standard deviation of 3.54.
Only five articles considered the participation of women, resulting in a total of 92% (n = 1357) men and 5.4% (n = 79) women (Table 2).
Regarding the type of anesthesia used (Table 3), it is noteworthy that in the 714 patients who underwent laparo-endoscopic procedures, general anesthesia was employed. Of the total cases where the type of anesthesia in Lichtenstein surgery was recorded (n = 680), 1.03% of the surgeries were performed under local anesthesia, 57.5% under regional anesthesia and 41.47% under general anesthesia.
Concerning the type of mesh and techniques performed during open surgery, as depicted in Table 4, studies recording mesh material predominantly opted for polypropylene. Only one article described the weight of the mesh, which was of low weight [17]. In all instances where the open (Lichtenstein) surgical procedure was described, mesh fixation to the pubis was achieves through sutures. The prophylactic neurectomy is only mentioned in the work of Shah MY et al. [18], while in the rest of the articles, either it is not described [14, 19], or the approach of identifying and preserving the nerves has been chosen [15, 17, 20, 21] (Table 4). Similarly, the type of mesh and techniques performed during laparo-endoscopic surgery are detailed in Table 5. It is notable that studies recording mesh material also opted for polypropylene. Mesh weight was only described in the study by Gutlic et al. [17], and it was of high weight. In contrast to Lichtenstein repair, mesh fixation to the pubis was achieved with staples in only one study [21]. Neurectomy was not performed in laparo-endoscopic surgery.
According to the term “recurrence,” only one study, Yang B et al. [14], defines recurrence as a palpable bulge on examination on the same side as the repair; the remaining articles do not. As for CPIP, four studies [17,18,19,20] define it as No pain, Mild, Moderate, and Severe.
Methodological quality and risk of Bias
The methodological quality of the included studies is depicted in Table 6. The included trials can be regarded as high-quality (Fig. 2: a and b). Concealment of allocation is well described in 5 out of 8 studies. Except for one study, the remaining studies had issues with blinding of personnel but not patients. Moreover, 2 articles achieved the blinding of the assessor.
Pain results
The definition of chronic pain varied across the studies, with some defining it starting at three months, others at six months and others at the first year. A total of 1,469 patients were followed to assess chronic pain. Regarding open surgery (Lichtenstein), CPIP was observed in 21.1% (n = 159) of patients. On the other hand, in laparo-endoscopic surgery, pain was reported in 8.1% (n = 58) of patients undergoing this intervention, as shown on Table 7.
In the random-effects analysis, laparo-endoscopic repair was associated with reduced odds of chronic pain compared to Lichtenstein repair (M-H OR = 0.28, 95% CI [0.30–0.56], p = 0.0001). There was some heterogeneity among the studies, with an I2 = 63% and a p-value of 0.009 for the Cochrane Q test (Fig. 3). Upon visual analysis of the funnel plot no evidence of publication bias was found (Fig. 4), a finding supported by Rosenthal’s tolerance test with a value of n = 106.
Recurrence results
Recurrence rates were reported in the eight trials with varying follow-up periods. Some studies followed up for the first year, while others extended follow-up to two years. In total, 1,469 patients were analyzed. Concerning Lichtenstein surgery, a recurrence rate of 3% (n = 23) was observed in patients, while in laparo-endoscopic surgery, a 3.1% (n = 22) recurrence rate was reported (Table 8).
After applying the fixed-effects model, no significant differences were found when comparing laparo-endoscopic repair with Lichtenstein repair (M-H OR = 1.03; 95% CI [0.57–1.86], p = 0.92) (Fig. 5). There was no heterogeneity among the studies, with an I2 value of 0% and a p-value > 0.1 in the Cochrane Q test. Upon visual analysis of the funnel plot, no evidence of publication bias was found (Fig. 6).
Discussion
This systematic review and meta-analysis of RCTs provides updated evidence on the comparative effect of chronic inguinal pain following hernioplasty in patients undergoing laparoendoscopic repair compared to open surgery (Lichtenstein). It included 8 studies and 1469 patients demonstrating lower rates of CPIP in laparoendoscopic surgery. However, recurrence rates were the same.
The results of this study can be significant when the surgical community contemplates current guidelines and their implementation in practice, as both the Lichtenstein procedure and minimally invasive techniques (laparo-endoscopic) are currently recommended as the best evidence-based options, particularly in the hands of experts [1].
Although this systematic review and meta-analysis differ from previous works published on this topic, primarily because it also focus solely on unilateral primary inguinal hernia, and the definition of chronic pain varies in the literature, the results are in line with those of studies that did focus exclusively on it [3, 4, 6, 22] except for one study that conducted a Bayesian network meta-analysis, which did not find differences in CPIP [5]. This result may be due to the lower validity of indirect comparisons employed by this statistical method. In addition, this review and meta-analysis provides five RCTs not mentioned in previous meta-analyses [14, 17]- [20]. Consistent with the mentioned studies, a statistically significant difference is observed when comparing the risk of CPIP following laparo-endoscopic surgery versus open surgery. One possible explanation is the greater tissue damage and dissection of the spermatic cord and cremaster muscle in open surgery [7], while the risk of recurrence did not show statistical significance.
However, CPIP has also been associated with other perioperative factors besides surgical technique, such as the type of anesthesia. Chinchilla-Hermida et al. [23]. and Zwaan et al. [24]. demonstrated that general anesthesia is a risk factor for the development of CPIP, although this result may be biased as general anesthesia is often reserved for more complex patients with greater comorbidity, etc. Furthermore, in the same study by Chinchilla-Hermida et al. and the work of Crompton J et al. [25]. , it is reported that local trans-fascial infiltration of local anesthetics during open surgery is a factor that prevents the development of chronic pain in this type of surgery.
Postoperative chronic pain has been shown to be associated with injury or entrapment of the ilioinguinal, iliohypogastric, and genitofemoral nerves, as they can become entrapped in a mesh or undergo peri-prosthetic inflammatory processes [26]. These nerves can be damaged during open surgery, unlike in laparo-endoscopic surgery, where there is less risk, provided careful dissection is performed without placing staples [27] in the pain triangle, where the nerves of the area are in the lateral preperitoneal space of Bogros. The management of these nerves in open surgery varies according to the studies. The European Hernia Society (EHS) guideline [1] recommends identifying and preserving the nerves to reduce chronic pain. In cases of nerve injury, suspicion, or difficulty placing the mesh, pragmatic resection is recommended. The EHS [1] rejects prophylactic neurectomy; however, recent series have demonstrated that prophylactic neurectomy of the ilioinguinal nerve decreases pain at six months (not at one year), increasing paresthesia in the first six months in the study by Charalambous MP et al. [27]. and without increasing them in the studies by Cirocchi R et al. [28]. and Xu Z et al. [29]. .
In this review, only one study conducted prophylactic neurectomy [18], demonstrating a higher rate of chronic pain following Lichtenstein repair; these results are in contrast to the previously mentioned articles. The remaining articles of the review which described the process, identified and preserved the nerves.
Other influential factors for postoperative chronic pain include mesh weight and the fixation method.
Regarding mesh weight, a recent study by Bakker WJ et al. [30]. showed differences favoring lightweight mesh for chronic pain, but the rates were similar for severe chronic pain, and there were no differences in the recurrence rate. In contrast, for laparo-endoscopic surgery, Xu M et al. [31]. , Bakker WJ et al. [30]. , and Hu D et al. [32]. reported no differences in pain when comparing low-weight to high-weight meshes, but they did observe an increase in the recurrence rate with low-weight meshes.
Although there are multiple fixation methods, there is no consensus on which is the “best,” so the methods used are based on surgeons’ preferences. Trauma-free fixation with adhesives appears to reduce acute postoperative pain [1]. Regarding chronic pain, a review by de Sun P et al. [33]. found significant differences when comparing adhesive fixation to suture fixation (OR 0.63, 95% CI 0.44–0.91), with a lower incidence of chronic pain in the adhesive group and the same recurrence rate. However, most recent series did not find differences in either the rate of chronic pain or recurrences when comparing adhesives to sutures and self-adhesive meshes [34, 35], or when comparing sutures to self-adhesive meshes [36,37,38].
It is important to mention the fixation of the mesh to the pubis, which the EHS [1] discourages, as it can increase the incidence of chronic pain, due to the highly innervated periosteum of the pubic bone. If damaged by sutures or staples, it is likely to result in intense and long-lasting pain [1].
Although the aim of this study is not to compare mesh fixation versus non-fixation, it is worth mentioning that in the Lichtenstein repair, the articles describing the surgical procedure fix the mesh with sutures or staples, and those mentioning the fixation of the mesh to the pubis do so with sutures. Only Yang B et al. [14]. reports less chronic pain in laparo-endoscopic surgery, while the remaining articles [17, 20, 21] do not show differences between fixing or not the mesh. Among these, the study by Sawarkar P et al. [20]. stands out, being the only one that secures the mesh to the pubis in laparo-endoscopic surgery, resulting in the RCT with the highest percentage of cases of CPIP in this technique.
In the laparo-endoscopic repair of inguinal hernia, the EHS [1] finds significant differences regarding chronic pain when not fixing the mesh or fixing it in a trauma-free manner (with adhesives/self-adhering) or mechanically (with sutures/staples). However, it recommends not fixing the mesh in most types of hernias, except in large medial defects (EHS M3 classification), where mesh fixation is recommended to decrease recurrence [1].
The literature shows variability in results regarding fixation in laparo-endoscopic surgery. In the Swedish study by Gutlic N et al. [39]. , no differences were found in postoperative chronic pain and recurrence between non-fixation, trauma-free fixation (adhesive), and mechanical fixation in TEP.
However, in the work of Habib Bedwani NaR et al. [40]. , it is reported that there are differences in favor of trauma-free fixation (adhesive) over mechanical fixation in both TEP and TAP (RR = 0.43, 95% CI [0.27–0.86]). Additionally, the review by Wang D et al. [41] describes a lower incidence of chronic pain with self-adhesive meshes (trauma-free) compared to conventional ones (mechanical) (OR 0.43, 95% CI 0.20–0.93, P = 0.03). Both studies demonstrated that there were no differences in terms of the risk of recurrence.
In this review, all of the studies examined opted to fix the mesh in laparo-endoscopic surgery with staples [14,15,16, 19, 20], except for two which did not do so [17, 18]. It is worth noting that the study by Yang B et al. [14]. , which used adhesive in cases of defects smaller than 3 centimeters. It is difficult to know the relevance of these techniques. The current trend is only to fix the mesh in M3 hernias [1].
Finally, it is relevant to note that this systematic review and meta-analysis grouped both the TEP and TAPP techniques because the literature shows that both have similar risks in terms of complications, incidence of acute and chronic postoperative pain, as well as recurrence rates.
There are several limitations that could influence the results. These limitations include the exclusion of articles in languages other than English and Spanish, what could cause the omission of important articles, the absence of multicenter studies, the specific characteristics and practices of a particular center (such as mesh fixation technique and its location, the point of fixation in Lichtenstein repair to the pubic tubercle, and the material used, as well as the type of mesh employed), the lack of blinding for surgeons and evaluators, and different methods of random assignment. All of these factors contribute to a high level of heterogeneity among the studies. Moreover, the studies obtained do not follow up beyond 5 years to adequately assess recurrence.
Two studies analyzed (Ielpo B et al. [18] and Elmessiry M.M et al. [19]) only include patients operated on for bilateral inguinal hernia and analyze patients presenting with CPIP without differentiating whether it is unilateral or bilateral pain, which implies it is a confounding variable.
In conclusion, the laparo-endoscopic techniques (TAPP and TEP) present a lower risk of CPIP compared to Lichtenstein repair. This study did not find differences in the recurrence rates between laparo-endoscopic repair (TAPP and TEP) and open repair (Lichtenstein).
References
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Haladu N, Alabi A, Brazzelli M et al (2022) Open versus laparoscopic repair of inguinal hernia: an overview of systematic reviews of randomised controlled trials. Surg Endosc 36:4685–4700. https://doi.org/10.1007/s00464-022-09161-6
Guillaumes S, Hoyuela C, Hidalgo NJ et al (2021) Inguinal hernia repair in Spain. A population-based study of 263,283 patients: factors associated with the choice of laparoscopic approach. Hernia 25:1345–1354. https://doi.org/10.1007/s10029-021-02402-y
Bullen NL, Massey LH, Antoniou SA et al (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23:461–472. https://doi.org/10.1007/s10029-019-01989-7
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23:473–484. https://doi.org/10.1007/s10029-019-01964-2
Wu JJ, Way JA, Eslick GD, Cox MR (2018) Transabdominal Pre-peritoneal Versus Open Repair for primary unilateral inguinal hernia: a Meta-analysis. World J Surg 42:1304–1311. https://doi.org/10.1007/s00268-017-4288-9
Scheuermann U, Niebisch S, Lyros O et al (2017) Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair - A systematic review and meta-analysis of randomized controlled trials. BMC Surg 17:55. https://doi.org/10.1186/s12893-017-0253-7
Page MJ, Mckenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:71. https://doi.org/10.1136/bmj.n71
Critical Appraisal Skills Programme (2023) CASP (Randomised Controlled Trial) Checklist. https://casp-uk.net/checklists/casp-rct-randomised-controlled-trial-checklist.pdf. Accessed 18 April 2023
Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC (2023) Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (ed). Cochrane Handbook for Systematic Reviews of Interventions version 6.4. Cochrane
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2023) Cochrane Handbook for Systematic Reviews of Interventions version 6.4. Cochrane
Cochrane.org RevMan [Internet] https://training.cochrane.org/online-learning/core-software/revman. Accessed 8 Mar 2023
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Yang B, Zhou S, Li Y et al (2018) A comparison of outcomes between Lichtenstein and Laparoscopic Transabdominal Preperitoneal Hernioplasty for recurrent inguinal hernia. Am Surg 84:1774–1780. https://doi.org/10.1177/000313481808401134
Ielpo B, Duran H, Diaz E et al (2018) A prospective randomized study comparing laparoscopic transabdominal preperitoneal (TAPP) versus Lichtenstein repair for bilateral inguinal hernias. Am J Surg 216:78–83. https://doi.org/10.1016/j.amjsurg.2017.07.016
Sevinç B, Damburacı N, Güner M, Karahan Ö (2019) Comparison of early and long term outcomes of open Lichtenstein repair and totally extraperitoneal herniorrhaphy for primary inguinal hernias. Turk J Med Sci 49:38–41. https://doi.org/10.3906/sag-1803-94
Gutlic N, Gutlic A, Petersson U et al (2019) Randomized clinical trial comparing total extraperitoneal with Lichtenstein inguinal hernia repair (TEPLICH trial). Br J Surg 106:845–855. https://doi.org/10.1002/bjs.11230
Shah MY, Raut P, Wilkinson TRV, Agrawal V (2022) Surgical outcomes of laparoscopic total extraperitoneal (TEP) inguinal hernia repair compared with Lichtenstein tension-free open mesh inguinal hernia repair: a prospective randomized study. Med (Baltimore 101:e29746. https://doi.org/10.1097/MD.0000000000029746
Elmessiry MM, Gebaly AA (2020) Laparoscopic versus open mesh repair of bilateral primary inguinal hernia: a three-armed Randomized controlled trial. Annals Med Surg 59:145–150. https://doi.org/10.1016/j.amsu.2020.08.055
Sawarkar P, Agrawal A, Zade R et al (2017) Lichtenstein hernia repair versus totally extraperitoneal hernia repair: randomized control study in rural area. J Mahatma Gandhi Inst Med Sci 22:93–98. https://doi.org/10.4103/jmgims.jmgims_47_15
Yen FV, Sani I, Md Hashim MN et al (2017) Laparoscopic total extraperitoneal approach versus open lichtenstein repair of primary unilateral uncomplicated inguinal hernia : a single centre experience in Malaysia. Surg Chronicles 22:54–58
Patterson TJ, Beck J, Currie PJ et al (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg 106:824–836. https://doi.org/10.1002/bjs.11139
Chinchilla-Hermida PA, Baquero-Zamarra DR, Guerrero-Nope C, Bayter-Mendoza EF (2017) Incidence of chronic post-surgical pain and its associated factors in patients taken to inguinal hernia repair. Colombian J Anesthesiology 45:291–299. https://doi.org/10.1016/j.rcae.2017.07.002
Zwaans WAR, Verhagen T, Roumen RMH, Scheltinga MRM (2015) Factors determining outcome after surgery for Chronic Groin Pain following a Lichtenstein Hernia Repair. World J Surg 39:2652–2662. https://doi.org/10.1007/s00268-015-3183-5
Crompton JG, Dawes AJ, Donald GW et al (2016) Perineural bupivacaine injection reduces inguinodynia after inguinal hernia repair. Surgery 160:1528–1532. https://doi.org/10.1016/j.surg.2016.07.016
Charalambous MP, Charalambous CP (2018) Incidence of chronic groin pain following open mesh inguinal hernia repair, and effect of elective division of the ilioinguinal nerve: meta-analysis of randomized controlled trials. Hernia 22:401–409. https://doi.org/10.1007/s10029-018-1753-9
Cirocchi R, Sutera M, Fedeli P et al (2021) Ilioinguinal nerve neurectomy is better than preservation in Lichtenstein Hernia Repair: a systematic literature review and Meta-analysis. World J Surg 45:1750–1760. https://doi.org/10.1007/s00268-021-05968-x
Xu Z, Qu H, Kanani G et al (2020) The short outcome of the routine ilioinguinal neurectomy in the treatment of chronic pain during herniorrhaphy: a meta-analysis of randomized-controlled trials. Asian J Surg 44:431–439. https://doi.org/10.1016/j.asjsur.2020.10.022
Bakker WJ, Aufenacker TJ, Boschman JS, Burgmans JPJ (2020) Lightweight mesh is recommended in open inguinal (Lichtenstein) hernia repair: a systematic review and meta-analysis. Surgery 167:581–589. https://doi.org/10.1016/j.surg.2019.08.021
Xu M, Xu S (2019) Meta-analysis of randomized controlled trials comparing lightweight and heavyweight mesh for laparoscopic total extraperitoneal inguinal hernia repair. Am Surg 85:620–624. https://doi.org/10.1177/000313481908500626
Hu D, Huang B, Gao L (2019) Lightweight Versus Heavyweight Mesh in laparoscopic inguinal hernia repair: an updated systematic review and Meta-analysis of Randomized trials. J Laparoendosc Adv Surg Tech A 29:1152–1162. https://doi.org/10.1089/lap.2019.0363
Sun P, Cheng X, Deng S et al (2017) Mesh fixation with glue versus suture for chronic pain and recurrence in Lichtenstein inguinal hernioplasty. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010814.pub2
Rausa E, Asti E, Kelly ME et al (2019) Open Inguinal Hernia Repair: A Network Meta-analysis comparing self-gripping mesh, suture fixation, and glue fixation. World J Surg 43:447–456. https://doi.org/10.1007/s00268-018-4807-3
Hoyuela C, Juvany M, Carvajal F et al (2017) Randomized clinical trial of mesh fixation with glue or sutures for Lichtenstein hernia repair. Br J Surg 104:688–694. https://doi.org/10.1002/bjs.10488
Bullen NL, Hajibandeh S, Hajibandeh S et al (2021) Suture fixation versus self-gripping mesh for open inguinal hernia repair: a systematic review with meta-analysis and trial sequential analysis. Surg Endosc 35:2480–2492. https://doi.org/10.1007/s00464-020-07658-6
van Steensel S, van Vugt LK, Al Omar AK et al (2019) Meta-analysis of postoperative pain using non-sutured or sutured single-layer open mesh repair for inguinal hernia. BJS Open 3:260–273. https://doi.org/10.1002/bjs5.50139
Ismail A, Abushouk AI, Elmaraezy A et al (2017) Self-gripping versus sutured mesh fixation methods for open inguinal hernia repair: a systematic review of clinical trials and observational studies. Surgery 162:18–36. https://doi.org/10.1016/j.surg.2016.12.028
Gutlic N, Rogmark P, Nordin P et al (2016) Impact of mesh fixation on Chronic Pain in total extraperitoneal inguinal hernia repair (TEP): a Nationwide Register-based study. Ann Surg 263:1199–1206. https://doi.org/10.1097/SLA.0000000000001306
Habib Bedwani N, a. R, Kelada M, Smart N et al (2021) Glue versus mechanical mesh fixation in laparoscopic inguinal hernia repair: meta-analysis and trial sequential analysis of randomized clinical trials. Br J Surg 108:14–23. https://doi.org/10.1093/bjs/znaa002
Wang D, Jiang J, Fu Y, Qu P (2022) The comparison of self-gripping mesh and conventional mesh in laparoscopic inguinal hernia repair: the results of meta-analysis. Updates Surg 74:857–863. https://doi.org/10.1007/s13304-021-01218-w
Acknowledgment
Acknowledgment to Sofia Khan Saiz de Omeñaca for the translation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guillermo Lillo-Albert, Elvira Buch Villa, Andrea Boscà-Robledo, Omar Carreño-Sáenz, José Bueno-Lledó, Jesús Martínez-Hoed, Salvador Pous-Serrano declare that they have no conflict of interest.
There is not conflict of interest, including but not limited to direct, indirect financial or personal relationships.
Approval from the institutional review board was not required for this study.
This article is a systematic review and meta-analysis contains data collected through literature review. It does not include research directly involving human or animal participation.
For this literature review, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lillo-Albert, G., Villa, E.B., Boscà-Robledo, A. et al. Chronic inguinal pain post-hernioplasty. Laparo-endoscopic surgery vs lichtenstein repair: systematic review and meta-analysis. Hernia 28, 1427–1439 (2024). https://doi.org/10.1007/s10029-024-03077-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-024-03077-x