Abstract
Introduction
Morbidity following open inguinal hernia repair is mainly related to chronic pain. ProGrip™ is a self-gripping mesh which aims to reduce rates of chronic pain. The aim of this study is to perform an update meta-analysis to consolidate the non-superiority hypothesis in terms of postoperative pain and recurrence and perform a trial sequential analysis.
Methods
Systematic review of randomised controlled trials performed according to PRISMA guidelines. Pooled odds ratios with 95% confidence intervals (CI) were calculated using the Mantel–Haenszel (M–H) method. The primary outcome measure was postoperative pain and secondary outcomes were recurrence, operative time, wound complications, length of stay, re-operation rate, and cost. Trial sequential analysis was performed.
Results
There were 14 studies included in the quantitative analysis with 3180 patients randomised to self-gripping mesh (1585) or standard mesh (1595). At all follow-up time points, there was no significant difference in the rates of chronic pain between the self-gripping and standard mesh (risk ratio, RR 1.10, 95% confidence interval, CI 0.83–1.46). There were no significant differences in recurrence rates (RR 1.13, CI 0.84–2.04). The mean operating time was significantly shorted in the ProGrip™ mesh group (MD − 7.32 min, CI − 10.21 to − 4.44). Trial sequential analysis suggests findings are conclusive.
Conclusion
This meta-analysis has confirmed no benefit of a ProGrip™ mesh when compared to a standard sutured mesh for open inguinal hernia repair in terms of chronic pain or recurrence. No further trials are required to address this clinical question.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recent hernia guidelines still consider the Lichtenstein technique to be the reference standard for open inguinal hernia repair [1]. Recurrence rates are reported to be less than 1% [1, 2]. Morbidity is primarily related to chronic pain, which can occur in up to 63% of patients and affects quality of life in 5–10% [3]. Several factors have been implicated in chronic postoperative pain, including recurrence, nociceptive problems (tissue inflammation, foreign material, meshoma [4]) and neuropathic causes (direct nerve injury or perineural scaring) [3, 5]. The causes of neuropathic pain are nerve entrapment by mesh or sutures and neuroma formation associated with complete or partial transection of the involved nerve [6]. Factors that may be responsible for chronic pain include taut fixation of the mesh, peri-ostial sutures into the pubic tubercle and herniotomy instead of repositioning of the hernia sac [7].
Self-gripping meshes have been developed, aiming at reducing short-term and long-term postoperative pain with comparable recurrence rates. This is purported to be due in part to a reduced inflammatory response and a less intense foreign body reaction [8]. In addition, by avoiding suture fixation it is thought to reduce the risk of suture-related neuropraxia, nerve entrapment, and nerve injury [9].
Early individual trials suggest a lower incidence of early postoperative pain with the use of self-gripping mesh compared to suture mesh fixation for open inguinal hernia repair [10, 11]. Four meta-analyses of randomised trials, however, have consistently demonstrated no significant difference in pain scores with comparable recurrence rates [8, 9, 12, 13]. The only reported benefit is a reduction in operation time with the self-gripping mesh [8, 9, 12, 13].
The objective of this study is to perform an update meta-analysis to consolidate the non-superiority hypothesis in terms of postoperative pain and recurrence when comparing self-gripping with suture mesh fixation for open inguinal hernia repair. Furthermore, to perform a trial sequential analysis and investigate whether the required information size has been reached and evidence is conclusive, or alternatively compute the number of patients required to be enrolled in further trials.
Methods
The protocol for this systematic review was established prior to initiation of the study and was registered under the number CRD42018069266 in the International Prospective Register of Systematic Reviews (PROSPERO) database [14]. The reporting methodology conforms to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [15].
Eligibility criteria, study selection and search strategy
Randomised controlled trials only were included comparing standard sutured mesh fixation with self-gripping mesh for open inguinal hernia repair. No other study design was considered. Studies enrolling patients aged over 16 years with primary unilateral or bilateral inguinal hernias repaired by the open approach were included. No other exclusion criteria were applied. The intervention was any technique of open inguinal hernia repair using a self-gripping mesh and no other method of invasive fixation (i.e. including penetration of musculature, muscle fascia, and/or the pubic bone). The control group was any technique of open inguinal hernia repair including mesh fixation onto the posterior wall of inguinal canal with any method of invasive fixation.
The electronic databases of Embase, Medline through PubMed, the Cochrane Central Register of Controlled Trials (CENTRAL, provider Wiley Online Library) and OpenGrey were searched from their inception until January 2018. A combination of the following MeSH terms (Medical Subject Headings) were used: “inguinal”, “groin”, “hernia”, “herniorrhaphy”, “Lichtenstein”, “mesh”, “prosthetic material”, “self-gripping”, “self-fixing”, “self-adhesive”, “Velcro effect” and “Progrip” (see Online Appendix 1 for search syntaxes). No language restrictions were applied. Eligibility assessment was performed independently in an unblinded standardised manner by two reviewers. Disagreements were resolved by consensus.
Data collection
Three independent reviewers were involved in study selection. Reviewers were blinded to studies selected for inclusion by the other reviewer. Discrepancies were resolved by a third party. Bibliographic references of published studies and reviews were also interrogated. Data were extracted using a standardised data collection form. One reviewer extracted the data and the second and third reviewers checked the extracted data. Attempts were made to contact authors of studies to verify extracted data and provide additional information.
The primary outcome measure was postoperative pain. Data related to the primary outcome measure were collected from the abstract, main text, tables or graphs. The time intervals for short-term assessment of postoperative pain were defined as 6 h, 12 h and 24 h. Longer term follow-up intervals were 1, 3, 6 and 12 months, 2 years and 3 years. If data on follow up were inadequate (less than 5 trials) then time intervals were merged to complete a set of 5 trials providing data. The longest duration of follow-up (minimum 1 year) was considered for trial sequential analysis (TSA). Most studies were expected to assess postoperative pain using the mean visual analogue scale (VAS) from 0 to 10. VAS scores ranging from 0 to 100 were converted to an 11-scale climax.
The secondary outcome measures were hernia recurrence; operative time; seroma/haematoma/soft tissue collection; wound infection; re-operation; hospital stay; and cost. The method of assessment of hernia recurrence was documented (clinical or radiological). Definitions of operative time, and descriptive data on seroma/haematoma/soft tissue collection (such as method of diagnosis) and on cost (hospitalisation, operative or material cost) were documented.
Synthesis of results
A fixed effect model was applied to synthesise data in the absence of statistical and conceptual heterogeneity. The presence of heterogeneity was evaluated by assessing the consistency of study population, intervention, perioperative care characteristics and method of outcome assessment, by inspecting the forest plots, and by computing the I2 values. If significant heterogeneity among the included studies was identified, random-effects analysis according to DerSimonian and Laird was used. Difference in means (MD) with 95% confidence intervals (CIs) were calculated to assess the size of the effect of the use of self-gripping or conventional meshes on continuous variables as appropriate. Where means and p values were given, we estimated the standard error and the standard deviation by calculating the standard error and t value using the given degrees of freedom. The standard error and standard deviation were obtained from confidence intervals using the formula suggested by the Cochrane Collaboration [16]. Pooled risk ratios (RRs) with 95% CIs were calculated to measure the effect of each type of procedure on dichotomous variables. Publication bias was assessed visually evaluating the symmetry of funnel plots if at least 10 trials were included in the meta-analysis. Statistical analysis was performed using RevMan 5.3 (Review Manger 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark).
Trial sequential analysis was performed to assess the possibility of type I error and to compute the information size. The Land and DeMets method was used to construct monitoring boundaries and set adjusted thresholds for statistical significance [17]. The information size was calculated at α = 0.05, β = 0.2, relative risk reduction of 50% and a cumulative incidence of chronic postoperative pain of 6.1% based on available trials. The Z value curve was constructed based on consecutive Z values calculated upon two-sided significant testing. Trial sequential monitoring boundaries were constructed using conventional testing and applying the O'Brien-Fleming α-spending function [18]. Futility testing was performed and the respective futility boundaries were constructed to assess whether the two interventions differ more than the anticipated intervention effect. Trial sequential analysis was performed using The Trial Sequential Analysis software 0.9.5.10 Beta (Copenhagen Trial Unit, Copenhagen, Denmark).
Sensitivity analyses of studies comparing self-gripping mesh versus (i) suture or (ii) tack fixation were planned, provided at least 3 studies would be available for each analysis. Post hoc subgroup analyses considered comparisons of Parietex ProGrip™ versus standard mesh and Parietene ProGrip™ versus standard mesh.
Methodological assessment
Risk of bias of the included studies was assessed using Cochrane Collaboration’s tool [19]. This tool considers random sequence generation, allocation concealment, blinding of participants, personnel and outcome assessors; incomplete outcome data, selective outcome reporting and other potential threats to validity.
IRB approval and written consent were not required for this study.
Results
Study selection and quality assessment
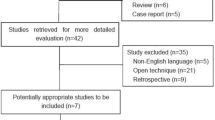
The searches of the electronic databases retrieved 176 records. After exclusion of duplicates, 103 titles and abstracts remained for screening. From these, 21 articles were selected for full-text review and 19 articles reporting on randomised controlled trials (RCTs) fulfilled the eligibility criteria and were included in the qualitative analysis. There were 5 trials that included two papers; short and long-term follow up so overall 14 studies were included in the quantitative analysis. There was excellent agreement between the reviews with only 2 articles causing conflict which were resolved by a third reviewer (SAA) and one of these was subsequently included. Literature search processes are summarised in Fig. 1. Search strategies can be found in Online Appendix 1.
Support was given to 2 studies by Covidien with one studies receiving a grant [20] and Jorgensen declared previous funding from Covidien for research support [21] but no conflicts of interest were declared. No other studies declared any conflicts of interest although this was not formally stated by 3 studies [21,22,23]. During the writing of the meta-analysis the long-term results of one of the studies already included was published and hence included in the analysis [20]. The risk of bias assessment of articles that were judged to be of acceptable or high quality is illustrated in Fig. 2A, B.
Study characteristics
The 14 included RCTs were published between 2010 and 2018 and all were written in the English language. A total of 3180 patients were included, randomised to ProGrip™/self-gripping mesh (n = 1585) or standard mesh (n = 1595). Study characteristics are summarised in Table 1.
Of the trials reporting sex of patients, 97% were male with two trials recruiting only male patients [24, 25]. The time period the studies were conducted over was from 2007 until 2013. Duration of follow up ranged from 6 months to 6 years.
Chronic groin pain was the primary outcome measure in ten trials. Two reported primarily operative time [23, 26] and one recurrence [22]. Further details are presented in Online Appendix 2. Half of the trials used ProGrip™ Parietene (polypropylene) and the other half Parietex (polyester). The control arm meshes were all made of polypropylene except for Molegraaf [27] who used a polyester mesh. The earlier seven trials had limited duration of follow up to one year whereas the later trials extended their follow up to up to six years. Most of the trials only included patients with primary inguinal hernia except the trial by Ronka [28] where both primary and recurrent hernias were included. All the studies reported data on unilateral hernia repairs alone except the trial by Perrero et al. [24]. Only four trials reported the use of the intention-to-treat principle [21, 27, 29,30,31].
Two studies, the FinnMesh trial [28] and Fernandez trial [22], were three arm RCTs comparing the self-gripping mesh, glue fixation and suture fixation of mesh. For the purpose of this meta-analysis the patients receiving glue fixation were excluded.
The trial by Kingsnorth/Sanders [11, 32] was the only one to perform a subgroup analysis. The self-gripping mesh group was divided into a subgroup without fixation and a group with a single suture fixation. There is a theory that even a single suture may lead to more postoperative pain. This study found that those without fixation had less pain at 1 and 3 months follow up.
Two studies were abstract publications, hence limited data were available. The authors were contacted but did not wish to release any further data prior to publication of their work. One of these was the follow up to an earlier included study by Chatzimavroudis [33]. The other by Fernandez [22] reported only recurrence data but as the follow up was two years it was eligible to be included in the analysis.
Data synthesis
Chronic pain
Chronic pain was reported in 13 trials. The definition of chronic pain was variable and five studies did not provide a definition (Online Appendix 2). Rates of chronic pain were analysed separately at different follow-up time periods (3–12 months, 2 years and 3 years). At all follow-up time points there was no significant difference in the rates of chronic pain between the self-gripping and standard mesh (RR 1.10, 95% CI 0.83–1.46) (Fig. 3). Between 3 and 12 months a total of 1784 patients were analysed and 7.3% (131) had chronic pain (69 self-adhering, 62 standard) (RR 1.13, CI 0.82–1.56). The frequency of chronic pain decreased over time for both groups but then reached a plateau. At 2 years 330 patients were analysed and 4.5% (15) had chronic pain (8 self-adhering and 7 standard) (RR 1.16, CI 0.43–3.12). Between 3 and 6 years postoperatively 500 patients were analysed and 5.4% (27) had chronic pain (13 self-adhering, 14 standard) (RR 0.93, CI 0.45–1.93). A fixed effect model was used as there was no evidence of conceptual or statistical between study heterogeneity. The funnel plot did not suggest presence of small study effects (Fig. 4).
VAS scores were reported by 13 trials but specifically mean VAS scores were only reported by 9 trials. Jorgensen [21] reported the percentage of patients with VAS scores > 30 and it was not clear if the data by Fan [26] and Zwaans [20] were means as there was no clear statement. When specifically comparing studies that reported data using mean VAS scores at multiple time points there is no statistically significant difference between the self-gripping and standard meshes (24 h MD 0.02, CI − 0.65 to 0.69; 7 days MD − 0.31, CI − 0.69 to 0.08; 1 month MD 0.02, CI − 0.2 to 0.24; 12 months MD 0.08, CI − 0.13 to 0.29), although the statistically significant difference at 2 and 3 years can be attributed to the relative weight of the RCTs by Molegraaf and Fan, respectively; (2 years MD 0.2, CI 0.19 to 0.21; 3 years MD 0.01, CI 0.01 to 0.01) (Fig. 5). These differences are however of no clinical significance. The funnel plot suggested some evidence of small study effects (Fig. 6).
Recurrence
Recurrence rates were reported in 12 trials over a range from 1 year to 6 years. Most trials assessed hernia recurrence by clinical examination. Three trials did not record the method of diagnosis of recurrence. Ronka et al. [28] assessed patients by clinical examination and ultrasound but only those that reported symptoms at a telephone follow up clinic. There were no significant differences in recurrence rates between the self-gripping and standard mesh. A total of 3203 patients were analysed with an overall 2.3% recurrence rate (73 patients—42 self-adhering and 31 standard mesh) (RR 1.31, CI 0.84–2.04) (Fig. 7). There was low evidence of between study heterogeneity (I2 = 18%). The funnel plot did suggest the presence of some small study effects (Fig. 8).
Sensitivity analysis for recurrence rates by calculation of the risk difference (RD) was performed and found similar results (RD 0.01, CI 0.00–0.02). This has allowed the inclusion of studies that reported a 0 recurrence rate [3, 5, 8, 9, 12, 16] hence providing a more accurate analysis (Fig. 9).
Operative time
Operative time was reported by 12 trials and nine trials reported the mean operating time. The mean operating time was significantly shorter in the self-gripping mesh group (MD − 7.32, CI − 10.21 to − 4.44) (Fig. 10). There was considerable between study heterogeneity (I2 = 92%). The funnel plot was not suggestive of small study effects (Fig. 11).
Other results
Results for wound complications, hospital stay, re-operation rates and cost are displayed in Online Appendix 3.
Subgroup analyses
Post hoc subgroup analyses of Parietex ProGrip™ vs. standard mesh and Parietene ProGrip™ vs. standard mesh did not suggest substantial differences in effect estimates between Parietex and Parietene, although only a few analyses were informed by at least 3 studies (Online Appendix 4).
Trial sequential analysis
The information size was calculated at 1417 patients. The Z-curve did not cross the O’Brien–Fleming α-spending boundaries and the evidence of non-superiority of the self-gripping mesh compared to the standard mesh can be considered to be conclusive (Fig. 12).
Discussion
This meta-analysis of randomised controlled trials provides robust evidence on the comparative effect of self-gripping and standard meshes for open inguinal hernia repair. It included 13 studies and 2786 patients. It shows no difference with respect to chronic pain or recurrence rates. The calculated information size suggests that the cumulative number of patients enrolled in published RCTs is large enough to draw solid conclusions on the non-superiority of the self-gripping mesh for inguinal hernia repair and further trials are highly unlikely to change this outcome.
One important issue regarding all the included trials is the definition of what material constituted the meshes used as both the ProGrip™ and the ‘standard’ mesh in the control arm were variable. This is an important source of heterogeneity. Half of the trials reported data on ProGrip™ Parietene (polypropylene) which has subsequently been discontinued and the more recent studies on ProGrip™ Parietex (polyester). All the trials except one used polypropylene mesh in the control arm, although of variable polymer fibre size; Molegraaf [27] used a polyester mesh. The trials that used different meshes were not just comparing method of fixation (self-gripping vs. suture) but are also comparing mesh material composition (which comprises polymer type, polymer fibre size, weave & porosity). For a true comparison of the effect of self-fixation in isolation meshes made of the same material should have been used, which was done by seven of the trials.
The main advantage of the ProGrip™ mesh lies in the reduction in operative time which has been shown to be significant in agreement with previous meta-analyses [8, 9, 12, 13]. This is due to the method of insertion i.e. placing the mesh onto the posterior inguinal wall rather than suturing to the inguinal ligament. Analysing the cost of the mesh in this review found on average that the ProGrip™ mesh was at least twice as expensive as the standard mesh. All health care services demand value which has been defined as outcomes related to costs and encompasses efficiency [34]. It is difficult to justify a more expensive mesh without proof of clinical effectiveness. Molegraaf et al. [8], however, suggested that the reduction in operation time and improved theatre efficiency would compensate for the higher cost of the mesh but no formal cost effectiveness analysis has been performed. Nevertheless, cumulative analysis suggests a mean difference of − 7 min in operative time, which would be probably of no significance.
Kingsnorth et al. [32] reported reduced infection rates with the ProGrip™ mesh (2 vs. 7%, p = 0.032) and this was supported by one previous meta-analysis which suggested a lower risk for wound infection with the ProGrip™ but this was not statistically significant [13]. The length of operation is proportional to the inoculation risk and it has been suggested that the reduced operating time with ProGrip™ reduces infection due to the reduced time the mesh is exposed to the open wound [33]. No evidence of significant difference in the risk of wound-related complications was found in this meta-analysis.
This meta-analysis was registered with the PROSPERO database prior to commencing the review hence minimising reporting bias. There were no deviations from the protocol. A formal assessment of publication bias has been done by way of funnel plots. Two abstract publications were included in the review [22, 33] and the authors were contacted for further information which they declined to provide prior to full publication of their results. Potential sources of bias include problems with the methodology of some of the trials. There were four studies that were not blinded introducing performance bias. The CONSORT statement recommends use of the intention-to-treat principle for all randomised controlled trials, however, only four papers reported on the intention-to-treat principle to analyse their data. It is however not likely that a significant proportion of patients in either group crossed over to the alternate intervention. Only three trials did not report pain as their primary outcome. This is particularly important as there is evidence that secondary outcomes are rarely reported as well as primary outcomes [35].
A limitation of this and previous meta-analyses are inconsistencies between trials regarding the definition of chronic pain between trials and how they report pain, e.g. VAS versus VRS (verbal rating scale) making it difficult to compare studies. Some authors regard all patients who report pain during different activities as patients with chronic pain, VAS > 0, VAS > 30, VAS > 40 (scale ranging from 0–10 or 0–100), or pain recorded by change in VAS scores compared with baseline (See Online Appendix 2). This high heterogeneity in part hinders the comparison of the outcomes of the trials. In contrast to previous meta-analyses, this review analysed both the number of patients with chronic pain and the mean VAS scores with the aim to give more accurate results. Ideally there would be a standardised format for reporting postoperative pain in inguinal hernia surgery. Bhangu et al. [36] have presented data showing that outcome reporting from RCTs concerning inguinal hernia repair is inconsistent and poorly defined. This consequently has limited meta-analyses. A core outcome dataset would standardise reporting and consequently improve quality of RCTs on inguinal hernias but as yet one does not exist.
Most trials reported only patients with primary inguinal hernias except for Ronka et al. [28] that included recurrent hernias. Recurrent hernias are associated with higher recurrence rates [37]. Perrero et al. [38] included only bilateral hernia repairs in their analysis which would no doubt have higher rates of early postoperative pain than the other trials reporting unilateral hernia repairs. The earlier meta-analyses reporting on self-gripping meshes included a short follow up of only 1 year [9, 12, 13]. The European Hernia society recommends a minimum 3 year follow-up for determining long-term outcome for pain [39]. Now several RCTs [26, 33] are available with follow up of up to 6 years allowing this analysis to draw more accurate conclusions.
In conclusion, this meta-analysis and trial sequential analysis report no benefit of the ProGrip™ mesh over the standard mesh. The evidence for non-superiority can be considered to be conclusive and no further trial data are required.
References
Simons MP, Aufenacker TJ, Berrevoet F, Bingener J, Bisgaard T, Bittner R, Bonjer HJ, Bury K, Campanelli G, Chen DC, Chowbey PK (2017) World guidelines for groin hernia management
Nordin P, Bartelmess P, Jansson C, Svensson C, Edlund G (2002) Randomized trial of Lichtenstein versus Shouldice hernia repair in general surgical practice. Br J Surg 89(1):45–49
Lange JFM, Kaufmann R, Wijsmuller AR, Pierie JPEN, Ploeg RJ, Chen DC, Amid PK (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19(1):33–43
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139(12):1297–1298
Wijsmuller AR, Van Veen RN, Bosch JL, Lange JFM, Kleinrensink GJ, Jeekel J, Lange JF (2007) Nerve management during open hernia repair. Br J Surg 94(1):17–22
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8(4):343–349
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8(1):1–7
Molegraaf M, Kaufmann R, Lange J (2018) Comparison of self-gripping mesh and sutured mesh in open inguinal hernia repair: a meta-analysis of long-term results. Surgery 163(2):351–360
Sajid MS, Farag S, Singh KK, Miles WF (2014) Systematic review and meta-analysis of published randomized controlled trials comparing the role of self-gripping mesh against suture mesh fixation in patients undergoing open inguinal hernia repair. Updates Surg 66(3):189–196
Verhagen T, Zwaans WAR, Loos MJA, Charbon JA, Scheltinga MRM, Roumen RMH (2016) Randomized clinical trial comparing self-gripping mesh with a standard polypropylene mesh for open inguinal hernia repair. Br J Surg 103(7):812–818
Sanders DL, Nienhuijs S, Ziprin P, Miserez M, Gingell-Littlejohn M, Smeds S (2014) Randomized clinical trial comparing self-gripping mesh with suture fixation of lightweight polypropylene mesh in open inguinal hernia repair. Br J Surg 101(11):1373–1382
Zhang C, Li F, Zhang H, Zhong W, Shi D, Zhao Y (2013) Self-gripping versus sutured mesh for inguinal hernia repair: a systematic review and meta-analysis of current literature. J Surg Res 185(2):653–660
Pandanaboyana S, Mittapalli D, Rao A, Prasad R, Ahmad N (2014) Meta-analysis of self-gripping mesh (Progrip) versus sutured mesh in open inguinal hernia repair. Surgeon 12(2):87–93
University of York, Centre for Reviews and Dissemination. PROSPERO; International Prospective Register of systematic reviews. https://www.crd.york.ac.uk/PROSPERO/
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Higgins JPT, Deeks JJ (2011) Obtaining standard deviations from standard errors, confidence intervals, t values and p values for differences in means. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. www.cochrane-handbook.org.
DeMets D, Lan KK (1994) Interim analysis: the alpha spending function approach. Stat Med 12:1341–1352
O'Brien PC, Fleming TR (1979) A multiple testing procedure for clinical trials. Biometrics 35:549–556
Higgins JP, Altman DG (2009) Assessing risk of bias in included studies. In: Higgins JP, Green S (eds) Cochrane handbook for systematic reviews of interventions. Wiley, West Sussex, pp 187–235
Zwaans WA, Verhagen T, Wouters L, Loos MJ, Roumen RM, Scheltinga MR (2018) Groin pain characteristics and recurrence rates: three-year results of a randomized controlled trial comparing self-gripping Progrip mesh and sutured polypropylene mesh for open inguinal hernia repair. Ann Surg 267(6):1028–1033
Jorgensen LN, Sommer T, Assaadzadeh S, Strand L, Dorfelt A, Hensler M, Rosenberg J, Danish Multicentre DANGRIP Study Group (2013) Randomized clinical trial of self-gripping mesh versus sutured mesh for Lichtenstein hernia repair. Br J Surg 100(4):474–481
Fernandez A, Pena Soria M, Jimenez-Valladolid D, Cabeza J, Perez Jimenez A, Florez Gamarra M, Estela L, del Pozo P, Garcia Galocha J, Romera Martinez J, Rojo Abecia M, Avellana R, Torres Garcia A (2017) Mesh fixation technique comparison in Lichtenstein hernioplasty, preliminary results of a prospective randomized study. Hernia 21(2):21–27
Suárez-Grau JM, Luque JB, Moreno JG, Menchero JG, Ferreras ID, Romero RM, Lupiañez ER, Jurado JG (2012) Postoperative pain and surgical time in Inguinal hernia repair with self-gripping mesh: experience in ambulatory surgery. Ambul Surg 18:18–20
Porrero JL, Castillo MJ, Pérez-Zapata A, Alonso MT, Cano-Valderrama O, Quirós E, Villar S, Ramos B, Sánchez-Cabezudo C, Bonachia O, Marcos A (2015) Randomised clinical trial: conventional Lichtenstein vs hernioplasty with self-adhesive mesh in bilateral inguinal hernia surgery. Hernia 19(5):765–770
Esteban MB, Pallarés MC, De Rojas EAS (2010) Use of adhesive mesh in hernioplasty compared to the conventional technique. Results of a randomised prospective study. Cirugía Española 88(4):253–258
Fan JKM, Yip J, Foo DCC, Lo OSH, Law WL (2017) Randomized trial comparing self gripping semi re-absorbable mesh (PROGRIP) with polypropylene mesh in open inguinal hernioplasty: the 6 years result. Hernia 21(1):9–16
Molegraaf MJ, Grotenhuis B, Torensma B, de Ridder V, Lange JF, Swank DJ (2017) The HIPPO Trial, a randomized double-blind trial comparing self-gripping Parietex Progrip mesh and sutured Parietex mesh in Lichtenstein hernioplasty: a long-term follow-up study. Ann Surg 266(6):939–945
Rönkä K, Vironen J, Kössi J, Hulmi T, Silvasti S, Hakala T, Ilves I, Song I, Hertsi M, Juvonen P, Paajanen H (2015) Randomized multicenter trial comparing glue fixation, self-gripping mesh, and suture fixation of mesh in Lichtenstein hernia repair (FinnMesh Study). Ann Surg 262(5):714–720
Nikkolo C, Vaasna T, Murruste M, Suumann J, Kirsimägi Ü, Seepter H, Tein A, Lepner U (2017) Three-year results of a randomized study comparing self-gripping mesh with sutured mesh in open inguinal hernia repair. J Surg Res 209:139–144
Nikkolo C, Vaasna T, Murruste M, Seepter H, Suumann J, Tein A, Kirsimägi Ü, Lepner U (2015) Single-center, single-blinded, randomized study of self-gripping versus sutured mesh in open inguinal hernia repair. J Surg Res 194(1):77–82
Kapischke M, Schulze H, Caliebe A (2010) Self-fixating mesh for the Lichtenstein procedure—a prestudy. Langenbeck's Arch Surg 395(4):317–322
Kingsnorth A, Gingell-Littlejohn M, Nienhuijs S, Schüle S, Appel P, Ziprin P, Eklund A, Miserez M, Smeds S (2012) Randomized controlled multicenter international clinical trial of self-gripping Parietex™ ProGrip™ polyester mesh versus lightweight polypropylene mesh in open inguinal hernia repair: interim results at 3 months. Hernia 16(3):287–294
Chatzimavroudis G, Papaziogas B, Koutelidakis I, Galanis I, Christopoulos P, Voloudkis N, Kotoreni G, Laskou S, Christofordis E (2014) Long-term follow-up of a prospective randomized study comparing polypropylene mesh fixed with sutures vs. self-fixating polypropylene mesh in inguinal hernia repair. Hernia 21(2):195–200
Porter ME (2010) What is value in health care? N Engl J Med 363(26):2477–2481
Matthews JH, Bhanderi S, Chapman SJ, Nepogodiev D, Pinkney T, Bhangu A (2016) Underreporting of secondary endpoints in randomized trials. Ann Surg 264(6):982–986
Bhangu A, Singh P, Pinkney T, Blazeby JM (2015) A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia 19(1):65–75
Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J (2015) Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov 22(3):303–317
Chatzimavroudis G, Papaziogas B, Koutelidakis I, Galanis I, Atmatzidis S, Christopoulos P, Doulias T, Atmatzidis K, Makris J (2014) Lichtenstein technique for inguinal hernia repair using polypropylene mesh fixed with sutures vs self-fixating polypropylene mesh: a prospective randomized comparative study. Hernia 18(2):93–198
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18(2):151–163
Esteban MB, Pallarés MC, de Rojas EAS, Vila MJ (2014) Prospective randomized trial of long-term results of inguinal hernia repair using autoadhesive mesh compared to classic Lichtenstein technique with sutures and polypropylene mesh. Cirugía Española 92(3):195–200
Pierides G, Scheinin T, Remes V, Hermunen K, Vironen J (2012) Randomized comparison of self-fixating and sutured mesh in open inguinal hernia repair. Br J Surg 99(5):630–636
Funding
There are no sources of funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Naomi L. Bullen, Shahin Hajibandeh, Shahab Hajibandeh, Neil J. Smart, Stavros A. Antoniou have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.


Rights and permissions
About this article
Cite this article
Bullen, N.L., Hajibandeh, S., Hajibandeh, S. et al. Suture fixation versus self-gripping mesh for open inguinal hernia repair: a systematic review with meta-analysis and trial sequential analysis. Surg Endosc 35, 2480–2492 (2021). https://doi.org/10.1007/s00464-020-07658-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07658-6