Abstract
Objectives
A systematic review and meta-analysis were performed to answer this research question: “Does combined in-office (IO) and at-home (AH) bleaching produce improved color change and lower tooth sensitivity (TS) better than solely AH or IO bleaching in adults?”
Material and methods
Randomized controlled trials in adults that compared combined versus sole application bleaching were included. The risk of bias (RoB) was evaluated using the Cochrane Collaboration tool. Meta-analyses were conducted for color change in shade guide units (∆SGU) and with a spectrophotometer (∆E*), risk, and intensity of TS, using the random effects model. Heterogeneity was assessed with Cochran’s Q test and I2 statistics. GRADE assessed the quality of the evidence. PubMed, Scopus, Web of Science, LILACS, BBO, Cochrane Library, SIGLE, IADR abstracts, unpublished, ongoing trial registries, dissertations, and theses were searched on August 28, 2017 (updated on January 29, 2019).
Results
Twelve studies remained. Two were considered to have low RoB. For combined vs. IO bleaching, no significant difference for ∆E*, ∆SGU, and risk of TS were observed; data were not available to analyze the intensity of TS. For combined vs. AH bleaching, no significant difference for ∆E*, ∆SGU, but lower TS to risk (RR 1.40, 95% 1.10 to 1.80) and intensity (MD 1.40, 95% CI 0.18 to 2.63) were detected for AH bleaching. Quality of evidence was graded as low or very low in all meta-analyses.
Conclusion
Lower risk and intensity of TS was observed for the solely AH group without jeopardizing color change. However, more studies are still encouraged due to the low quality of evidence for most of the outcomes.
Clinical relevance
If clinicians are to choose between combined or sole AH bleaching, the solely AH may be preferable; combined bleaching may potentiate the risk of TS without benefits in color change. For combined or sole IO bleaching, no important clinical difference in color change and risk of TS were detected; however, intensity of TS could not be compared due to lack of data. Further studies should be conducted due to the low/very low quality of the evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental bleaching is the most popular cosmetic procedure because it is a conservative method for treating dental discoloration [1, 2] and it meets the needs of an increasing number of patients who request treatment for esthetic discoloration [3,4,5]. Furthermore, dental bleaching is technically easier and lower-cost than any other type of cosmetic treatment, such as veneers.
Dentist-supervised dental bleaching can be performed in-office by the dentist, using high-concentrate hydrogen peroxide (HP), or it can be done at-home by the patient, using low-concentrate carbamide peroxide (CP) or low-concentrate HP [6]. Although at-home bleaching is frequently used, some patients do not adapt to the daily use of a tray for several weeks, so they request a tray-free and faster bleaching option [7, 8]. In-office bleaching is a good alternative for such patients. It can be performed in one to four clinical appointments, with applications lasting from 15 to 60 min [9,10,11]. This technique, however, has the disadvantage of producing a higher intensity of tooth sensitivity (TS) during and after bleaching due to the inflammatory reaction produced by HP and free radicals when they contact the dental pulp [12,13,14,15].
A common clinical practice is to combine at-home and in-office bleaching techniques [16,17,18] to obtain faster bleaching effects [18], improved color stability [17, 19], and reduced levels of TS. Within this context, a single in-office bleaching session is usually performed first to start the bleaching effects quickly [20, 21]. Then, the patient continues the protocol at-home with a custom-made bleaching tray, using low-concentrate products until the desired shade is obtained [17, 18, 22].
Some randomized controlled trials (RCTs) have already compared the combined bleaching technique with the sole use of at-home or in-office protocols [17, 20, 23, 24]; however, conflicting results in terms of risk and intensity of tooth sensitivity [25] and color change and stability [17, 18, 20, 22] have been reported.
Perhaps, such differences can be attributed to differences in protocols and deserve a deeper systematic revision to reach more reliable conclusions and allow for clinical recommendations. Therefore, the aim of the present systematic review of the literature was to evaluate whether there are evidence-based differences in color change, risk, and intensity of tooth sensitivity of combined bleaching versus the sole use of at-home or in-office bleaching protocols.
Materials and methods
Protocol and registration
This systematic review was registered at the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42016036555. The present study was reported, following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [26].
Information sources and search strategy
The controlled vocabulary (MeSH terms) and free keyword in the search strategy were defined based on the following PICOS question (P: participant, I: intervention, C: comparator, O: outcome, and S: study design):
-
1.
Participant (P): adult patients that underwent vital tooth bleaching;
-
2.
Intervention (I): combined in-office and at-home bleaching;
-
3.
Comparison (C): solely in-office or at-home bleaching;
-
4.
Outcome (O): color change in shade guide units (∆SGU) and with a spectrophotometer (∆E*); risk and intensity of TS taken after dental bleaching;
-
5.
Study design (S): randomized controlled trials.
The search strategy was first defined for the MEDLINE database by PubMed, based on using controlled vocabulary (MeSH terms) and free keywords for each concept of the PICO question was searched.
The MEDLINE search strategy was adapted to other electronic databases (Cochrane Library, Brazilian Library in Dentistry, Latin American and Caribbean Health Sciences Literature [LILACS] database) and citation databases (Scopus and Web of Science) (Table 1). In addition, gray literature was investigated by searching the abstracts of the annual conference of the International Association for Dental Research (IADR) and its regional divisions (1990–2018), the System for Information on Gray Literature in Europe database, and dissertations and theses, using the ProQuest Dissertations and Theses full-text database as well as the Periódicos Capes Theses database.
Ongoing studies were searched in the following clinical trial registries: Current Controlled Trials (www.controlled-trials.com), International Clinical Trials registry platform (http://apps.who.int/trialsearch/), ClinicalTrials.gov (http://www.clinicaltrials.gov), Rebec (www.rebec.gov.br), and EU Clinical Trials Register (https://www.clinicaltrialsregister.eu).
In addition, the reference lists of all primary and eligible studies of this systematic review for additional relevant publications were hand-searched. The first two pages of the related-articles link of each primary study in the PubMed database were also searched. In the whole search process, no restriction was placed on publication date and/or language.
Eligibility criteria
Parallel and split-mouth randomized controlled trials conducted with adult patients of any age group that answered the PICO question described at the end of the introduction section were included. RCTs were excluded if the studies compared only different combined bleaching treatments.
Study selection and data collection process
The articles retrieved by the literature search were revised in three phases. All studies were initially scanned for relevance by title, and the abstracts of those that were not excluded at this stage were appraised. The next step included the abstract reading, and the full text of the studies that could not be excluded according to our eligibility criteria in the abstract review was retrieved for further evaluation. Three reviewers then read the full texts to see whether they met the inclusion criteria. Finally, the eligible articles received a study identification (ID), combining first author and year of publication.
Two reviewers independently abstracted data from included articles, such as study design, participants, interventions, and outcomes. In cases of disagreement, a decision was reached by consulting a third reviewer. If there were multiple reports of the same study (i.e., reports with different follow-ups), data from all reports were extracted directly into a single data collection form to avoid overlapping data.
Data from color change after the end of the bleaching treatment was collected with periods ranging from immediately to 2-week post-bleaching (Table 2). This variation was due to the differences in the assessment period reported in the studies; from the 7 studies included [11, 16, 21, 27,28,29,30], 4 provided data for 1-week post-bleaching [11, 16, 27, 30], the reason of why we selected this time period for meta-analysis. When this period was not reported, we chose the closest period to 1-week post-bleaching, which was between immediately after [21, 28, 29] 2-week post-bleaching [21]. Preference was given for 2-week post-bleaching when the two options were available [21], since the teeth tend to appear whiter immediately after bleaching due to dental dehydration by teeth isolation and demineralization caused by the acidity of the bleaching agent [31]. Regarding TS, the worst mean value of TS reported for the group was collected.
Risk of bias in individual studies
Quality assessments of the selected trials were carried out by three independent reviewers, using the Cochrane Collaboration tool for assessing the risk of bias in RCTs [32]. The assessment criteria contained six items: sequence generation, allocation concealment, blinding of the outcome assessors, incomplete outcome data, selective outcome reporting, and other possible sources of bias. Disagreements among the reviewers were solved through discussion and, if needed, by consulting a fourth reviewer (A.R.).
For each aspect of the quality assessment, the risk of bias was scored, following the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions 5.02 (http://handbook.cochrane.org). Each domain level was judged as having low, high, or unclear risk of bias. At the study level, the study was at low risk of bias if all key domains (see below) for each outcome were at low risk of bias. If one or more key domains were judged as having unclear risk, the study was at unclear risk, and if at least one key domain was considered at high risk of bias, the study was considered at high risk of bias.
For the patient-centered outcomes such as the risk and intensity of TS, the key domains were adequate sequence generation and allocation concealment. Patient blinding was not considered a key domain because patients could easily identify the different bleaching protocols. For color change in ∆SGU, three items of the Cochrane Collaboration tool were considered key domains: adequate sequence generation, allocation concealment, and examiner blinding. However, for ∆E*, examiner blinding was not considered a key domain, because the previous knowledge of the treatment would not affect the results produced by an objective tool for color assessment such as spectrophotometers or colorimeters.
Data synthesis and statistical analysis
Data were analyzed using Revman 5.3 (Review Manager, version 5.3, the Cochrane Collaboration, Copenhagen, Denmark). Meta-analyses were performed in studies classified as low or unclear risk of bias. Studies judged to have high risk of bias were not included in the meta-analyses. Data from eligible studies were summarized by calculating the risk ratio (risk of TS) and the mean difference (intensity of TS and ∆E*). For the ∆SGU, mean difference was calculated when studies used the same shade guide or standardized mean difference were employed when at least one study used a different shade guide tool. For all meta-analyses, random effects model was chosen to summarize a mean effect size of the primary studies. Heterogeneity was assessed using Cochran’s Q test and I2 statistics. According to the Cochrane Handbook for Systematic Reviews of Interventions, the heterogeneity was classified as follows: < 40% may be low; 30–60% may be moderate; 50–90% may be substantial; 75–100% may be considerable.
When a study used a split-mouth design, data was merged keeping the same number of patients used in the comparison, and if the study reported two or more groups with the same intervention, we merged the data using the following below where N1 and N2 is the number of participants from groups 1 and 2; SD1 e SD2 is the standard deviation of groups 1 and 2, and M1 and M2 is the mean of groups 1 and 2.
Sensitivity analyses were also conducted to investigate the reasons for high heterogeneity, whenever detected, and also to assess the impact of imputations required for meta-analysis. Individual meta-analysis for studies that compared combined bleaching vs. in-office bleaching and those that compared combined bleaching vs. at-home bleaching was performed, because both types of comparison were identified in the systematic review.
Assessment of the quality of the evidence, using GRADE
The quality of the evidence for each outcome across the studies (body of evidence) was graded by using the Grading of Recommendations: Assessment, Development, and Evaluation (GRADE) (http://www.gradeworkinggroup.org/) system to determine the overall strength of the evidence for each meta-analysis. The GRADE pro Guideline Development Tool (available online at www.gradepro.org) was used to create a summary-of-findings table, as suggested in the Cochrane Handbook for Systematic Reviews of Interventions 5.2.0 (http://handbook.cochrane.org).
The GRADE approach for RCTs addresses five possible reasons (risk of bias, imprecision, inconsistency, indirectness of evidence, and publication bias) to downgrade the quality of the evidence (1 or 2 levels). Each of these topics was assessed as having no limitations, serious limitations, or very serious limitations to categorize the quality of the evidence into high, moderate, low, and very low.
Results
Study selection
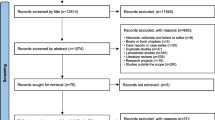
The search strategy was conducted initially on August 28, 2017, and it was updated on April 25, 2018, and January 29, 2019. After database screening and duplicate removal, 2466 studies were identified, after title screening, 331 studies remained, and this number was reduced to 12 after careful examination of the abstracts (Fig. 1).
Characteristics of included articles
Nine studies were published [10, 11, 16, 18, 21, 22, 28, 29, 33], being one of them an IADR abstract [27] and one was in a thesis format not published yet in a peer reviewed journal [30], and the same study is an IADR abstract [34] and a thesis format not published yet in a peer reviewed journal [35].
The characteristics of the 12 eligible studies are listed in Table 3. Nine studies used parallel design [10, 11, 16, 22, 27, 29, 30, 33, 34], and three studies used the split-mouth design [18, 21, 28] (Table 3).
Eight studies used the Vita Classical Shade guide (Vita Zahnfabrik, BadSäckingen, Germany) [11, 16, 18, 21, 22, 28,29,30], and three studies used the Vita Bleached guide 3D-Mastershade guide (Vita Zahnfabrik, Bad Säckingen, Germany) [29, 30, 34]. Seven studies used an objective instrument for color assessment (spectrophotometer or colorimeter) [10, 18, 21, 27,28,29,30]. Photography was used in four studies [18, 21, 22, 34]. One study did not evaluate color change [33] (Table 3).
The intensity of TS was evaluated using the visual analog scale (VAS) [16, 18, 21, 28, 30]. This outcome was not evaluated in three studies [22, 27, 33]. Four studies evaluated the risk of TS [10, 11, 29, 30, 34] (Table 3).
Age of participants in the primary RCTs and gender
The patients ranged from 18 to 78 years of age. The mean age of all participants that reported this information was approximately 29.7 years (Table 3). In the studies that reported the gender of the sample, females were more prevalent [10, 18, 28,29,30, 34].
Four studies evaluated combined bleaching (in-office plus at-home bleaching) vs. sole in-office bleaching [11, 18, 22, 29], whereas four studies evaluated combined bleaching (in-office plus at-home bleaching) vs. sole at-home bleaching [10, 16, 28, 30]. Three studies included both comparisons [27, 33, 34]. For this reason, individual meta-analyses for each one of these comparisons were performed as it would not be reasonable to merge these data.
In the sole in-office bleaching, the product employed was high-concentrate hydrogen peroxide (35% or 38%). In each clinical session, the product remained in contact with the dental structure from 15 to 60 min and, in total, one to four clinical appointments were performed 6 to 15 days apart (Table 3).
In the sole at-home bleaching, carbamide peroxide (10% or 16%) or hydrogen peroxide (4%HP) was employed. The bleaching trays were used from 7 to 21 days with a daily use that varied from 1 to 8 h (Table 3).
In the combined bleaching, the HP concentration varied from 9 to 38% when used in the in-office protocol. In each clinical session, the product remained in contact with the dental structure from 15 to 60 min. In some studies, the bleaching product was applied only once at the beginning of the treatment, whereas in others, more than one in-office bleaching was applied with an at-home session in between. For the at-home bleaching in the combined protocol, CP (10% or 16%) or HP (4% or 6%) was used in bleaching trays for 5 to 28 days, with daily use of 1 to 8 h (Table 3).
Assessment of the risk of bias
The risk of bias in the eligible studies is presented in Fig. 2. Few full-text studies reported the method of randomization, allocation concealment, and whether the examiner was blinded during color assessment in shade guide units (SGU). In summary, from the 12 studies, only two were considered to have a low risk of bias [29, 30], and the remaining were considered to have an unclear risk of bias.
Meta-analysis
Meta-analyses were performed on all studies from which information about the outcome was reported and could be extracted (Fig. 1). Some studies could not be included in the meta-analysis. One study [33] was not included in none of meta-analyses because the main objective of the study was to evaluate the buccal microbiota after bleaching; therefore, the outcomes of color change and TS were not reported. The study of Wetter [10] was not included in the meta-analysis of color change because they did not report color change in ∆E*, but as change in chroma, lightness, and hue, mainly focusing in interdental difference of color change during different bleaching protocols. The study of Matis [18] and Kugel [22] were not included in the meta-analyses as they did not have comparable groups. Matis [18] performed the in-office bleaching with very shorter application time, i.e., only a single session of 45 min. Kugel performed two clinical sessions, but each one with 15 min contact (total contact time of 30 min). All other studies performed at least two in-office bleaching sessions (30 to 60 min application per session) (at least) 1 week apart resulting in a total contact time of 90 to 120 min. Comparison of these shorter application protocols with a combined technique that associates to it 1 week of at-home bleaching is not a fair comparison.
The study by Dawson [16] had two groups of combined bleaching using two HP concentrations (9% and 27%). Only data from the highest concentration (27%) was used in the meta-analysis to be consistent with the other protocols that compared high-concentrate products in the combined group.
Color change in ∆E*
Combined vs. in-office bleaching
A total of two studies were included in this meta-analysis [27, 29]. The mean difference was − 0.63 (95% CI − 3.40 to 2.13) with no significant difference between groups (p = 0.65). Data showed considerable heterogeneity (p = 0.07; I2 = 69%) (Fig. 3a). The study by Bernardon [21] was removed from the meta-analysis of color change in Delta E because no direct comparison of the combined groups with the in-office groups was made.
Combined vs. at-home bleaching
Four studies were included in this meta-analysis [21, 27, 28, 30]. Imputation of the SD was done in the Machado [28] study based on the coefficient of variation of the other studies. The mean difference was 0.19 (95% CI − 0.57 to 0.95) with no significant difference between groups (p = 0.62). Data were not heterogeneous (p = 0.66; I2 = 0%) (Fig. 3b).
Color change in ∆SGU
Combined vs. in-office bleaching
The study of Rezende [11] reported the final SGU color, while the other two [29, 34] reported the change from baseline. The comparison of the final measurements in RCT, in theory, estimates the same quantity as the comparison of changes from baseline; in these cases, outcome can only be summarized in the meta-analysis as mean difference. For this reason, the study of Dias [34] had to be removed from the meta-analysis, as the authors employed a different shade guide unit for color assessment (Bleachedguide) and its inclusion could only be done using the standardized mean difference (not possible in this case, as the meta-analysis mixed final SGU measurements with change from baseline values). One study [29] reported the interquartile range; then, an estimate of the standard deviation (SD) was calculated based on these values, being the SD approximately equal to 1.35 times the range of the interquartile range. The study by Bernardon [21] was removed from the meta-analysis of color change in Delta SGU because no direct comparison of the combined groups with the in-office groups was made.
Then, two studies were included in this meta-analysis [11, 29] resulting in a mean difference of − 0.49 (95% CI − 0.87 to − 0.10), with a significant difference between groups (p = 0.01) favoring the in-office protocol. Heterogeneity of the data was not detected (p = 0.77; I2 = 0%) (Fig. 4a).
Combined vs. at-home bleaching
A total of four studies were included in this meta-analysis [16, 21, 28, 30] The studies by Bernardon [21], Dawson [16], and Machado [28] reported the final SGU color, while the study Vochikovski [30] reported the change from baseline. Mean difference was used to summarize data from this meta-analysis and for this reason, the study of Dias [34] had to be removed (as explained above). Imputation of the SD, following the mean coefficient of variation of the other studies that reported final SGU measurements, was done for the study of Machado [28]. A mean difference was − 0.10 (95% CI − 0.54 to 0.33), and it was not statistically different (p = 0.64). A moderate heterogeneity of the data was detected (p = 0.11; I2 = 51%) (Fig. 4b).
Risk of tooth sensitivity
Combined vs. in-office bleaching
Three studies were included in this meta-analysis [11, 29, 34] The risk ratio was 0.98 (95% CI 0.80 to 1.22), showing no significant differences between the groups (p = 0.89). No heterogeneity of the data was detected (p = 0.86; I2 = 0%) (Fig. 5a).
Combined vs. at-home bleaching
Three studies were included in this meta-analysis [10, 30, 34]. The risk ratio was 1.40 (95% CI 1.10 to 1.80), showing significant differences between the groups (p = 0.007). No heterogeneity of the data was detected (p = 0.80; I2 = 0%) (Fig. 5b).
Intensity of tooth sensitivity
Combined vs. in-office bleaching
Only one study could be included in this meta-analysis [21]; therefore, this meta-analysis was not run.
Combined vs. at-home bleaching
Two studies did not report the SD of TS intensity [21, 28] and was imputed a SD based on the mean coefficient of variation of the two other studies [16, 30]. A total of four studies were included in this meta-analysis [16, 21, 28, 30]. The mean difference was 1.40 (95% CI 0.18 to 2.63), and it was significantly different (p = 0.02). Considerable heterogeneity of the data was detected (p < 0.0001; I2 = 87%) (Fig. 6).
Narrative description of studies not included in the meta-analysis
The study of Matis [18] and Kugel [22] reported a significant and clinically important difference between color change in the combined group in comparison with the sole in-office bleaching protocol. A mean difference of 3.15 (95% CI 2.82 to 3.48) and 3.30 (95% CI 1.46 to 5.14) was observed in these studies, respectively, in favor of the combined group. Wetter [10] study mainly focused on interdental differences rather than bleaching protocols. However, by the data described it seems no significant difference was observed between the combined and at-home bleaching protocol. The study of Dias [34] compared in-office vs. combined bleaching (mean difference in ΔSGU of 1.14; 95% CI – 0.49 to 2.77) and at-home vs. combined bleaching (mean difference − 0.57; 95% CI – 2.33 to 1.19), with no difference among the protocols.
Sensitivity analysis
A standard deviation was imputed in the studies that did not report it. The value imputed was based on the average of the coefficient of variation of the other studies that reported the same finding [36]. More extreme imputations, such as a value that corresponded to the lowest coefficient of variation of the primary studies and a value that was as high as the reported mean, was evaluated and no differences in the results therein reported were detected.
Assessment of the quality of evidence
The body of evidence produced by all meta-analyses was very low or low due to unclear risk of bias in most RCTs and the high confidence interval that does not exclude great benefit or great harm. Additionally, three meta-analysis (ΔE combined bleaching vs. in-office; ΔSGU combined bleaching vs. at-home and intensity of TS combined bleaching vs. at-home) also presented inconsistency in the data due to high and non-explained heterogeneity and therefore were graded as very low quality of evidence (Table 4).
Discussion
Systematic reviews and meta-analyses are important in resolving the problem of controversies between clinical trials. In addition, systematic reviews and meta-analyses can provide a critical evaluation of the body of evidence and summarize it for development of recommendations for clinical implementation [37].
The search strategy of any systematic review usually has high sensitivity (number of relevant reports divided by the total number of existing reports). In a search with high sensitivity, the accuracy of the search (number of relevant documents divided by the total number of articles retrieved) is reduced, explaining why a huge number of retrieved articles were obtained and why few articles remained for evaluation [37, 38].
Among the factors that affect the risk of bias in primary studies, correct randomization is essential in an RCT. It ensures that the chances of a patient being allocated in the test or control group are the same for all participants, which means that known and unknown prognostic factors are balanced among groups [32]. However, the random sequence should be protected until implementation [32] in a process called allocation concealment. Most of the eligible studies from this systematic review were classified as having unclear risk of bias. This judgment was based on the lack of clear description of the randomization and allocation concealment process. This is in accordance with what was recently published by Loguercio et al. 2017 [39], who reported that more than 50% of RCTs about bleaching had a high or unclear risk of bias for randomization and allocation concealment. Unfortunately, effect sizes from studies with inappropriate random sequences and/or allocation concealment favor the experimental group [40], producing biased conclusions.
The combined bleaching technique was suggested to potentiate the bleaching effect and improve color stability [17]. However, neither of the two comparisons performed in this study (combined bleaching vs. solely in-office bleaching and combined bleaching vs. solely at-home bleaching) exhibited a higher degree of color change in 1 to 2 weeks after the end of the bleaching protocol. This belief is probably the result of earlier studies that were used to compare a single in-office bleaching with a 2- or 3-week, at-home protocol [18, 41,42,43,44]. A single in-office bleaching session is usually not enough to achieve the same degree of whitening that an extended at-home bleaching protocol would achieve.
This explains the removal of study by Matis [18] in meta-analysis of ∆E* that compared one in-office bleaching session to a combined bleaching that consisted of one in-office bleaching session plus 1 week of an at-home protocol. In such a study, a high effect size was observed in favor of the combined bleaching, a finding not observed in the other studies that performed two [21, 29] or three [27] in-office bleaching sessions. In the same trend, the meta-analysis of color change in ΔSGU for the same comparison (combined vs. in-office bleaching) did not include the study of Matis [18], and the study of Kugel [22] who left the gel in contact with the dental structure for a very short period of only 15 min in two clinical sessions. A previous RCT reported that a single 15-min application per session, even when applied in two clinical sessions, does not produce the same color change as two or three 15-min applications per clinical appointment [45], because it yields a lower whitening degree than two or three-min applications.
While the color change in ΔE for the comparison combined vs. in-office bleaching was not significant, color change in ΔSGU for the same comparison was significant different. While this could be seen as a controversy among the outcomes, one should consider that a statistically significant finding may not report a significant clinical outcome. In this case, the mean difference between groups was approximate half of a color tab unit in the Classical Vita shade guide, not easily detectable by untrained eyes [46].
For the other comparison (combined vs. at-home bleaching), no difference in color change in ∆E* was observed. The at-home protocol of all studies included in this meta-analysis consisted of a 14-day or 21-day regimen, and the combined bleaching consisted of a single 30-min or 45-min application plus a 14-day or 21-day regimen of at-home bleaching. As shown by Kihn [47] the difference of color change was not noticeable until the full 2-week regimen was completed. Thus, a 14-day or 21-day regimen should be performed for an effective tooth bleaching with the at-home protocol without the need of an in-office bleaching session [48,49,50]. This may justify the heterogeneity of the meta-analysis of color change in ∆E* (combined vs. in-office bleaching) being caused by the study by Rodrigues [29]. These authors only associated a single in-office bleaching with a 7-day at-home protocol in the combined group resulting in an effect size that favored the in-office bleaching. This was not reflected in the meta-analysis of color change in ∆SGU as this scale does not allow detection of subtle differences.
Regarding color change in ∆SGU for this comparison (combined vs. at-home bleaching), heterogeneity was observed to be different from the other primary studies in this comparison; Vochikovski [30] reported higher whitening efficacy for the combined bleaching group. This was the single study that used a low HP concentration (4%) compared to other studies that used 10 to 16% carbamide peroxide. An earlier systematic review of the literature that compared at-home bleaching with carbamide peroxide or low-concentrate HP showed that bleaching with carbamide peroxide yields higher bleaching efficacy in terms of color change [51]. Although both carbamide peroxide and HP are used for whitening, their properties are quite different, and this may play a role in the difference observed. HP-based products are very unstable and release all of their active hydrogen peroxide in 30 to 60 min [52, 53], whereas HP release from carbamide peroxide gels is slower than in HP-based products with a release of about 50% in the first 2 to 4 h and then the remainder over the next 2 to 6 h [52, 54].
The other outcome evaluated in this study was tooth sensitivity, which is the most common side effect after vital tooth bleaching [3, 7]. TS probably arises from the diffusion of HP into the dental structure and then the pulp chamber. In the pulp, HP induces the release of cell-derived factors such as adenosine triphosphate (ATP) and prostaglandins, which can excite or sensitize nociceptors [55, 56]. One of the factors that affect the intensity of TS is the concentration of the bleaching agent. In-office bleaching was associated with a higher intensity of TS than at-home bleaching [57]. This is the reason why a high intensity and risk of TS was observed in the combined bleaching in the comparison combined vs. at-home bleaching. This was expected due to the use of bleaching agents in concentrations much higher in the combined bleaching than those used in the solely at-home protocol [58,59,60].
The meta-analysis of intensity of TS was heterogeneous, probably due to the study by Dawson [16]. This was the single study that performed at-home bleaching before the in-office protocol. Perhaps such approach prepared the pulp tissue by the presence or even faster release of catalases to decompose hydrogen peroxide into water and oxygen.
In the meta-analysis of the risk of combined vs. in-office bleaching, no difference in the comparison was found. Indeed, this was observed in an earlier study that merged the results of several RCTs about at-home and in-office bleaching [57]. Unfortunately, the intensity of TS of combined bleaching vs. solely in-office bleaching could not be compared due to the lack of data availability. This should encourage further studies for this comparison.
Some decisions had to be made during data collection and deserve some discussion. The choice to collect the worst TS mean value presented in the study was performed to allow a fair comparison between the protocols. Because TS is lower in the at-home bleaching, if the data was collected only at the end of each treatment (after in-office, or after at-home bleaching or after combined bleaching), the TS of the combined group would be similar to the at-home protocol, because the at-home protocol was usually performed after the initial in-office start. Apart from that, the peak of pain varied among techniques. For in-office bleaching, it was reported to start within 1 h after the beginning of the treatment, with a pain peak within 1 and 6-h post-treatment [61]. For at-home bleaching, most patients usually reported TS in the first days of gel application, and the sensitivity tended to disappear after 4 days for most patients [62].
Another decision was the choice of effect size for color change in ΔSGU. The choice of standardized mean difference would allow the inclusion of one study that employed a different shade guide unit but not data from two studies that only reported final SGU values. The choice of the mean difference makes possible mixing data from final SGU measurements and change from baseline (ΔSGU), but it does not allow inclusion of studies that employed different scales for the outcome measurement. The selected outcome was the one that allowed the inclusion of more studies; however, unfortunately, the summary outcomes were sensitive to these changes.
Finally, the limitations of this study should be reported. EMBASE database was not directly inspected in the search process. However, we believe this limitation is of very low impact in the study results due to the fact that 65% of the journals indexed in EMBASE are also indexed in PUBMED. Additionally, EMBASE content also appears in CENTRAL, Scopus, and Web of Science, being these ones included in the search strategy.
Because few studies remained in this systematic review and the quality of evidence was graded as very low and low, due to unclear risk of bias of most studies, imprecision, and inconsistency (high heterogeneity), more randomized controlled trials with a sound methodology, reporting data in change from baseline, should be conducted to compare both techniques and to allow for a more comprehensive evaluation of protocols. The results reported herein should be interpreted with caution because they represent an overall comparison without taking into consideration variations in the protocols (daily usage time, number of bleaching sessions, product concentration, and days of home use) of the bleaching techniques.
Conclusions
In a comprehensive analysis, without considering other variables but the protocol, we may conclude that there is no benefit in color change was observed when combined bleaching was either compared with sole at-home bleaching or sole in-office bleaching. These findings should be interpreted with caution due to the low quality of evidence of all meta-analysis herein reported.
References
Sarrett DC (2002) Tooth whitening today. J Am Dent Assoc 133:1535–1538 quiz 1541
Joiner A (2006) The bleaching of teeth: a review of the literature. J Dent 34:412–419. https://doi.org/10.1016/j.jdent.2006.02.002
Auschill TM, Hellwig E, Schmidale S, Sculean A, Arweiler NB (2005) Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper Dent 30(2):156–163. https://doi.org/10.2341/1559-2863-30-2-1
Meireles SS, Goettems ML, Dantas RV, Bona ÁD, Santos IS, Demarco FF (2014) Changes in oral health related quality of life after dental bleaching in a double-blind randomized clinical trial. J Dent 42(2):114–121. https://doi.org/10.1016/j.jdent.2013.11.022
Samorodnitzky-Naveh GR, Grossmann Y, Bachner YG, Levin L (2010) Patients’ self-perception of tooth shade in relation to professionally objective evaluation. Quintessence Int 41:E80–E83
Haywood VB, Leonard RH, Nelson CF, Brunson WD (1994) Effectiveness, side effects and long-term status of nightguard vital bleaching. J Am Dent Assoc 125:1219–1226
Dahl JE, Pallesen U (2003) Tooth bleaching - a critical review of the biological aspects. Crit Rev Oral Biol Med 14:292–304
Gallagher A, Maggio B, Bowman J, Borden L, Mason S, Felix H (2002) Clinical study to compare two in-office (chairside) whitening systems. J Clin Dent 13:219–224
Gurgan S, Cakir FY, Yazici E (2010) Different light-activated in-office bleaching systems: a clinical evaluation. Lasers Med Sci 25:817–822. https://doi.org/10.1007/s10103-009-0688-x
Wetter NU, Branco EP, Deana AM, Pelino JE (2009) Color differences of canines and incisors in a comparative long-term clinical trial of three bleaching systems. Lasers Med Sci 24:941–947
Rezende M, Siqueira SH, Kossatz S (2014) Clareamento dental - efeito da técnica sobre a sensibilidade dental e efetividade (Dental bleaching - technique effect on dental sensivity and effectiveness). Rev Assoc Paul Cir Dent 68:208–212
Mena-Serrano AP, Parreiras SO, do Nascimento EM, Borges CP, Berger SB, Loguercio AD, Reis A (2015) Effects of the concentration and composition of in-office bleaching gels on hydrogen peroxide penetration into the pulp chamber. Oper Dent 40:E76–E82. https://doi.org/10.2341/13-352-L
Soares DG, Basso FG, Hebling J, de Souza Costa CA (2015) Immediate and late analysis of dental pulp stem cells viability after indirect exposition to alternative in-office bleaching strategies. Clin Oral Investig 19:1013–1020. https://doi.org/10.1007/s00784-014-1321-3
de Almeida LC, Soares DG, Gallinari MO, de Souza Costa CA, Dos Santos PH, Briso AL (2015) Color alteration, hydrogen peroxide diffusion, and cytotoxicity caused by in-office bleaching protocols. Clin Oral Investig 19:673–680. https://doi.org/10.1007/s00784-014-1285-3
Rezende M, Chemin K, Vaez SC, Peixoto AC, de Freitas RJ, Braga SSL, Faria-e-Silva AL, da Silva GR, Soares CJ, Loguercio AD (2018) Effect of topical application of dipyrone on dental sensitivity reduction after in-office dental bleaching: a randomized, triple-blind multicenter clinical trial. J Am Dent Assoc 149(5):363–371. https://doi.org/10.1016/j.adaj.2017.11.003
Dawson PF, Sharif MO, Smith AB, Brunton PA (2011) A clinical study comparing the efficacy and sensitivity of home vs combined whitening. Oper Dent 36(5):460–466. https://doi.org/10.2341/10-159-C
Deliperi S, Bardwell DN, Papathanasiou A (2004) Clinical evaluation of a combined in-office and take-home bleaching system. J Am Dent Assoc 135:628–634
Matis BA, Cochran MA, Wang G, Eckert GJ (2009) A clinical evaluation of two in-office bleaching regimens with and without tray bleaching. Oper Dent 34:142–149. https://doi.org/10.2341/08-64
Buchalla W, Attin T (2007) External bleaching therapy with activation by heat, light or laser--a systematic review. Dent Mater 23:586–596. https://doi.org/10.1016/j.dental.2006.03.018
Rezende M, Ferri L, Kossatz S, Loguercio AD, Reis A (2016) Combined bleaching technique using low and high hydrogen peroxide in-office bleaching gel. Oper Dent 41:388–396. https://doi.org/10.2341/15-266-c
Bernardon JK, Sartori N, Ballarin A, Perdigao J, Lopes G, Baratieri LN (2010) Clinical performance of vital bleaching techniques. Oper Dent 35:3–10. https://doi.org/10.2341/09-008cr
Kugel G, Perry RD, Hoang E, Scherer W (1997) Effective tooth bleaching in 5 days: using a combined in-office and at-home bleaching system. Compend Contin Educ Dent 18(378):380–373
Zhao K, Zong L, Zhang Q, Att W (2013) Clinical comparison between two bleaching techniques: a 180-day follow-up study. Quintessence Int 44(8):601–607. https://doi.org/10.3290/j.qi.a29702
Radz G (2014) Effectiveness of a combined in-office and take-home whitening system for teeth shades A3. 5 to A4. Compend Contin Educ Dent 35:696–700
Paula E, Kossatz S, Fernandes D, Loguercio A, Reis A (2013) The effect of perioperative ibuprofen use on tooth sensitivity caused by in-office bleaching. Oper Dent 38:601–608. https://doi.org/10.2341/12-107-c
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Coban A, Can E, Soyman M (2011) Clinical evaluation of in office at home and combined bleaching. Paper presented at the IADR/AADR/CADR 89th General Session, San Diego, California
Machado LS, Anchieta RB, dos Santos PH, Briso AL, Tovar N, Janal MN, Coelho PG, Sundfeld RH (2016) Clinical comparison of at-home and in-office dental bleaching procedures: a randomized trial of a split-mouth design. Int J Periodontics Restorative Dent 36:251–260. https://doi.org/10.11607/prd.2383
Rodrigues JL, Rocha PS, Pardim SLS, Machado ACV, Faria-e-Silva AL, Seraidarian PI (2018) Association between in-office and at-home tooth bleaching: a single blind randomized clinical trial. Braz Dent J 29:133–139
Vochikovski L (2018) Sensibilidade dental e efetividade de um novo protocolo de aplicação da técnica de clareamento associado com aplicação de dessensibilizante. Dissertation, State University of Ponta Grossa, Ponta Grossa
de Souza Costa CA, Riehl H, Kina JF, Sacono NT, Hebling J (2010) Human pulp responses to in-office tooth bleaching. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e59–e64
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Franz-Montan M, Ramacciato JC, Rodrigues JA, Marchi GM, Rosalen PL, Groppo FC (2009) The effect of combined bleaching techniques on oral microbiota. Indian J Dent Res 20:304–307. https://doi.org/10.4103/0970-9290.57367
Dias KRHC, Lima JP, Silva TM, Monte Alto RV, Oliveira Jr OB (2012) Evaluation of efficacy of three tooth bleaching technique. Paper presented at the IADR/AADR/CADR 89th General Session, San Diego, California
Lima JP (2012) Avaliação clínico visual de três técnicas de clareamento dental. Universidade do Estado do Rio de Janeiro
Ma J, Liu W, Hunter A, Zhang W (2008) Performing meta-analysis with incomplete statistical information in clinical trials. BMC 8:56. https://doi.org/10.1186/1471-2288-8-56
Higgins J, Green S (2010) Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration. http://handbook.cochrane.org/. Accessed June 2019
Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC (2014) How to write a systematic review. Am J Sports Med 42:2761–2768. https://doi.org/10.1177/0363546513497567
Loguercio AD, Maran BM, Hanzen TA, Paula AMd, Perdigão J, Reis A (2017) Randomized clinical trials of dental bleaching – compliance with the CONSORT Statement: a systematic review. Braz Oral Res 31. https://doi.org/10.1590/1807-3107bor-2017.vol31.0060
Schulz KF, Chalmers I, Hayes RJ, Altman DG (1995) Empirical evidence of bias. dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 273:408–412
da Costa JB, McPharlin R, Paravina RD, Ferracane JL (2010) Comparison of at-home and in-office tooth whitening using a novel shade guide. Oper Dent 35:381–388. https://doi.org/10.2341/09-344-C
Giachetti L, Bertini F, Bambi C, Nieri M, Scaminaci Russo D (2010) A randomized clinical trial comparing at-home and in-office tooth whitening techniques: a nine-month follow-up. J Am Dent Assoc 141:1357–1364
Moghadam FV, Majidinia S, Chasteen J, Ghavamnasiri M (2013) The degree of color change, rebound effect and sensitivity of bleached teeth associated with at-home and power bleaching techniques: a randomized clinical trial. Eur J Dent 7:405–411. https://doi.org/10.4103/1305-7456.120655
Pintado-Palomino K, Peitl Filho O, Zanotto ED, Tirapelli C (2015) A clinical, randomized, controlled study on the use of desensitizing agents during tooth bleaching. J Dent 43:1099–1105. https://doi.org/10.1016/j.jdent.2015.07.002
Kose C, Calixto AL, Bauer JR, Reis A, Loguercio AD (2016) Comparison of the effects of in-office bleaching times on whitening and tooth sensitivity: a single blind, randomized clinical trial. Oper Dent 41:138–145. https://doi.org/10.2341/15-085-C
Browning WD (2003) Use of shade guides for color measurement in tooth-bleaching studies. J Esthet Restor Dent 15:S13–S20
Kihn PW, Barnes DM, Romberg E, Peterson K (2000) A clinical evaluation of 10 percent vs. 15 percent carbamide peroxide tooth-whitening agents. J Am Dent Assoc 131:1478–1484
Chemin K, Rezende M, Loguercio AD, Reis A, Kossatz S (2018) Effectiveness of and dental sensitivity to at-home bleaching with 4% and 10% hydrogen peroxide: a randomized, triple-blind clinical trial. Oper Dent 43:232–240. https://doi.org/10.2341/16-260-C
Leonard RH Jr, Garland GE, Eagle JC, Caplan DJ (2002) Safety issues when using a 16% carbamide peroxide whitening solution. J Esthet Restor Dent 14:358–367
Matis BA, Mousa HN, Cochran MA, Eckert GJ (2000) Clinical evaluation of bleaching agents of different concentrations. Quintessence Int 31:303–310
Luque-Martinez I, Reis A, Schroeder M, Munoz MA, Loguercio AD, Masterson D, Maia LC (2016) Comparison of efficacy of tray-delivered carbamide and hydrogen peroxide for at-home bleaching: a systematic review and meta-analysis. Clin Oral Investig 20:1419–1433. https://doi.org/10.1007/s00784-016-1863-7
Matis B (2000) Degradation of gel in tray whitening. Compend Contin Educ Dent Suppl S28:S31–S25 quiz S49
Al-Qunaian T, Matis B, Cochran M (2003) In vivo kinetics of bleaching gel with three-percent hydrogen peroxide within the first hour. Oper Dent 28:236–241. https://doi.org/10.2341/1559-2863-28-3-1
Matis B, Yousef M, Cochran M, Eckert G (2002) Degradation of bleaching gels in vivo as a function of tray design and carbamide peroxide concentration. Oper Dent 27:12–18. https://doi.org/10.2341/1559-2863-27-1-1
Wang Y, Gao J, Jiang T, Liang S, Zhou Y, Matis BA (2015) Evaluation of the efficacy of potassium nitrate and sodium fluoride as desensitizing agents during tooth bleaching treatment - a systematic review and meta-analysis. J Dent 43:913–923. https://doi.org/10.1016/j.jdent.2015.03.015
Cook S, McCleskey E (2002) Cell damage excites nociceptors through release of cytosolic ATP. Pain 95:41–47
Rezende M, Loguercio AD, Kossatz S, Reis A (2016) Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: a multi regression and logistic analysis. J Dent 45:1–6. https://doi.org/10.1016/j.jdent.2015.11.003
Krause F, Jepsen S, Braun A (2008) Subjective intensities of pain and contentment with treatment outcomes during tray bleaching of vital teeth employing different carbamide peroxide concentrations. Quintessence Int 39:203–209
Kose C, Reis A, Baratieri LN, Loguercio AD (2011) Clinical effects of at-home bleaching along with desensitizing agent application. Am J Dent 24(6):379–382
Meireles SS, Heckmann SS, Santos IS, Della Bona A, Demarco FF (2008) A double blind randomized clinical trial of at-home tooth bleaching using two carbamide peroxide concentrations: 6-month follow-up. J Dent 36:878–884. https://doi.org/10.1016/j.jdent.2008.07.002
Charakorn P, Cabanilla L, Wagner W, Foong W, Shaheen J, Pregitzer R, Schneider D (2009) The effect of preoperative ibuprofen on tooth sensitivity caused by in-office bleaching. Oper Dent 34:131–135. https://doi.org/10.2341/08-33
Marson FC, Sensi LG, Vieira LCC, Araujo E (2008) Clinical evaluation of in-off ice dental bleaching treatments with and without the use of light-activation sources. Oper Dent 33:15–22. https://doi.org/10.2341/07-57
Acknowledgments
This study was developed by Andres Felipe Millan Cardenas, Bianca Medeiros Maran, Lucila Cristina Rodrigues Araújo, Fabiana Suelen Figuerêdo de Siqueira, Letícia Maíra Wambier, and Carla Castiglia Gonzaga under the supervision of Profs. Alessandro Loguercio and Alessandra Reis. The authors would like to thank Prof. Ana Armas-Vega during the review process of meta-analysis.
Funding
This study was partially supported by National Council for Scientific and Technological Development from the Brazilian Government, under grants 303332/2017-4 and 305588/2014-1 and the Coordination of Improvement of Higher Level Personnel (CAPES) from the Brazilian Ministry of Education.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cardenas, A.F.M., Maran, B.M., Araújo, L.C.R. et al. Are combined bleaching techniques better than their sole application? A systematic review and meta-analysis. Clin Oral Invest 23, 3673–3689 (2019). https://doi.org/10.1007/s00784-019-03042-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03042-4